Abstract
Objectives
Rates of maternal syphilis have increased five-fold in Brazil in the past decade. While penicillin remains the only appropriate treatment for maternal syphilis, we hypothesized that low non-treponemal titers (<1:16) may lead to reduced penicillin treatment in Brazil.
Methods
Using Brazilian Ministry of Health data on women diagnosed with maternal syphilis between January 1, 2010 and December 31, 2018, we conducted a random effects logistic regression model with a cluster correction at the state level to evaluate predictive factors of penicillin treatment.
Results
We observed yearly increases in cases of pregnant women with syphilis from 2010-2018. There was significant variation by state: 52,451 cases were reported in São Paulo, followed by 26,838 in Rio de Janeiro. Among 215,937 cases of maternal syphilis, 91·3% received penicillin. In the random effects model, a non-treponemal titer ≥1:16 was associated with 1·44 higher odds of receiving penicillin (95% confidence interval [CI]: 1·39,1·48), and pre-natal care was associated with a 2·12 increased odds of receiving penicillin (95% CI: 2·02,2·21). Although there is an association between absence of pre-natal care and inadequate treatment for syphilis, 83·2% of women in this cohort who did not receive penicillin were engaged in pre-natal care.
Conclusions
Providers may inappropriately exclude low non-treponemal titers and thereby fail to use penicillin treatment in maternal syphilis. While the cause of the maternal syphilis epidemic in Brazil is multifactorial, we believe our findings can be used to develop targeted interventions throughout Brazil as well as shape public health initiatives globally.
Keywords: Syphilis, Brazil, Pregnancy, Penicillin, Treatment, Health Policy
Introduction
Despite enhanced public health efforts to eradicate syphilis mother-to-child transmission (MTCT), maternal syphilis (diagnosed during pregnancy) remains a pressing global health concern. Nearly one third of untreated maternal syphilis cases will result in adverse pregnancy outcomes, including fetal or neonatal death (Newman et al., 2013). A 2008 analysis of multinational pre-natal clinics estimated 520,000 annual adverse pregnancy outcomes due to untreated syphilis, including 215,000 stillbirths, 90,000 neonatal deaths, and 65,000 preterm deliveries (Newman et al., 2013). In the surviving neonates, congenital syphilis may lead to permanent defects and lifelong health conditions, including renal failure and neurologic delay (Yeganeh et al., 2015). Congenital syphilis in neonates results from placental transfer of the bacteria Treponema pallidum from mothers with inadequately treated syphilis, and less frequently from direct inoculation from secondary syphilis lesions during vaginal delivery. Congenital syphilis is preventable with appropriate pre-natal testing and treatment. With the exception of prolonged treatment for tertiary syphilis, a single intramuscular injection of benzathine penicillin G (BPG) administered to the mother remains the only recommended treatment to prevent syphilis MTCT (Kwak, 2015). Alternative treatments do not effectively cross the placenta, or are contraindicated in pregnancy due to the risk of birth defects (Nurse-Findlay et al., 2017).
Although the World Health Organization (WHO) launched a global initiative to eliminate congenital syphilis as a public health concern in 2007, there is an ongoing syphilis epidemic throughout Brazil. Congenital syphilis rates increased five-fold in the past decade, last reported as 9·0 cases per one thousand live births in 2018 (Boletim Epidemiólogico Sífilis, 2019, Saúde 2020). This trend was further compounded by a penicillin shortage in Brazil from 2014 to 2016 due to drug-manufacturing market exits, which subsequently led to concerns regarding the quality of BPG preparations in Brazil (Nurse-Findlay et al., 2017).
Brazil relies on a non-treponemal titer followed by a confirmatory treponemal antibody to diagnose Syphilis. The main non-treponemal tests used worldwide are the Venereal Disease Research Laboratory (VDRL), Rapid Plasma Reagin (RPR) and Toluidine Red Unheated Serum Test (TRUST) quantitative titers.3 Multiple conditions, including lupus, certain medications, viral infections, and even pregnancy, may lead to false-positive or low non-treponemal titers (<1:16), raising questions as to whether these cases should be classified as true infections (Kwak, 2015). In addition, persistently low non-treponemal titers and confirmatory treponemal antibody assays will remain positive after adequate treatment in women with a history of prior syphilis. Several studies document an increased risk of syphilis MTCT and adverse pregnancy outcomes with titers ≥1:16 (Yeganeh et al., 2015, Wendel et al., 2002). In some settings, women with high non-treponemal titers (≥1:16) are more likely to receive penicillin compared to women with low titers (Yeganeh et al., 2015, Wendel et al., 2002).
While maternal syphilis cases are on the rise throughout Brazil, there is significant geographic variation at the state-level (Cambou, 2019). Although penicillin remains the only recommended treatment for maternal syphilis, there are no studies to our knowledge that have explored predictors of treatment assignment. Our study evaluates factors, including non-treponemal titers, associated with penicillin treatment in pregnant women diagnosed with syphilis in Brazil from 2010 to 2018.
Methods
Data Collection
We requested de-identified data on all women diagnosed with maternal syphilis between January 1, 2010 and December 31, 2018 from the “Sistema de Informação de Agravos de Notificação” (http://portalsinan.saude.gov.br/), the infectious diseases surveillance branch of the Brazilian Ministry of Health. The data is publicly available by request.
Brazil has required mandatory notification for maternal syphilis since 2005, and requires a minimum of one-time syphilis screening during pregnancy in accordance with WHO guidelines (Bezerra et al., 2019, World Health Organization, 2019). The Ministry of Health requires notification of all reactive non-treponemal tests collected at clinics or hospitals from pregnant or post-partum women. The case-reporting form (CRF), to be completed by the healthcare facility, collects data on the following: age, trimester of pregnancy at diagnosis, self-identified race, educational level, population density, state of residence, year of diagnosis, non-treponemal titer at diagnosis (Brazil uses VDRL), confirmatory treponemal assay, treatment regimen, and history of HIV or syphilis.
After notification, the Ministry of Health reviews each case to determine if the woman was appropriately treated and whether additional antibiotics are required. For our study, we utilized the CDC definition of maternal syphilis: any reactive non-treponemal titer with a confirmatory treponemal antibody assay (Center for Disease Control, 2019).
Study Design
This was an observational, cross-sectional study of women diagnosed with maternal syphilis to examine whether non-treponemal titer thresholds and other factors are associated with appropriate treatment with penicillin. Each case represents a new case of maternal syphilis, as judged by the Ministry of Health. Although some women may have repeat measures (another syphilis infection during a subsequent pregnancy), this number was thought to be minimal, and would still represent a novel infection. This study used publicly available de-identified data, and was therefore IRB exempt.
Measures
The primary outcome was treatment with penicillin: answers were dichotomized as “yes” (any penicillin treatment) and “no” (other antibiotic treatment, or no treatment). Cases with unknown treatments were excluded from the final study population. The primary regressor was a VDRL titer ≥1:16: only titers 1:1, 1:2, 1:4, 1:8, 1:16, 1:32, 1:64, 1:128, 1:256, 1:512 and 1:1024 were treated as true titers. A confirmatory treponemal test (fluorescent Treponemal antibody-absorption, micro-hemagglutination Treponema pallidum assay, Treponema pallidum hemagglutination assay, enzyme-linked immunosorbent assay, or lateral flow assay) was required for inclusion in the final study population.
Age at the time of diagnosis was divided into three categories: <20 years, 20 to 29 years, and greater than or equal to 30 years. Self-identified race was categorized as White, Black, and Mixed/Indigenous/Other. Self-reported educational attainment was divided into three categories: some primary school (including illiterate), completed primary school or some secondary school, and high school graduate or higher. Population density was coded as urban or rural/periurban. Pre-natal care was divided into two categories: received pre-natal care, and did not receive pre-natal care. Access to pre-natal care was determined secondarily by the SINAN question “Município de realização do Pré-Natal” which provided the specific municipality of the hospital where the individual received pre-natal care: if the response was left blank, we assumed the patient did not receive pre-natal care. Trimester of pregnancy at diagnosis was divided into three categories: first trimester, second trimester, and third trimester or postnatal. Less than 0·10% of trimester answers were missing. The Ministry of Health did not grant us access to HIV history, including current CD4 count, viral load and treatment regimen. Years of diagnosis were stratified into three categories: before penicillin shortage (2010-2013), during shortage (2014-2016), and after shortage (2017-2018) (Nurse-Findlay et al., 2017). The 26 states and the Federal District were treated as categories for the cluster correction. Cases with missing states of residence were excluded from the final dataset.
Statistical Analysis
Descriptive statistics (frequency and percentage) of sociodemographic factors (age, self-identified race, educational attainment, population density, and state of residence) and clinical factors (trimester of pregnancy at diagnosis and syphilis non-treponemal titers) were stratified by penicillin treatment to characterize the study population. Age and trimester of pregnancy were divided into categories based on median and interquartile range (IQR); year of diagnosis in relation to the penicillin shortage was treated as a category. Pearson correlation values did not exceed 0·70, and there was low concern for multicollinearity as assessed by the variance inflation factor.
We used a random effects (RE) logistic regression model with a cluster correction at the state level of all pregnant women diagnosed with maternal syphilis reported to the Brazilian Ministry of Health to evaluate factors associated with penicillin treatment (Gardiner et al., 2009). Crude and adjusted odds ratios and 95% confidence intervals (CI) were estimated for our primary regressor and covariates. Statistical analysis was performed using Stata version 16, and all statistical significance tests relied on a two-sided α <0.05.
Results
The original dataset from the Ministry of Health included 225,451 women with maternal syphilis from 2010 to 2018, but 9,446 cases had no information on treatment (either unknown or missing) and therefore were excluded from the final sample. An additional 68 cases were excluded due to missing state of residence, for a total of 215,937 cases diagnosed from January 1, 2010 to December 31, 2018. The analysis of excluded data shown in Supplemental Tables 1 and 2 investigates demographic differences between included and excluded patient populations.
Table 1A shows general descriptive characteristics of our final study population stratified by penicillin use. The median age of the entire study population was 23 (IQR 19-28), and the greatest proportion of women that received penicillin treatment (52·2%) were aged 20 to 29. Nearly half (49·5%) of the study population identified as Mixed or Indigenous race, followed by 31·1% White, and 11·9% Black. The distribution across educational levels was fairly uniform, although there was a large percentage of unknowns (27·3%). Only 7·9% of the study population came from a rural area.
Table 1A:
General descriptive characteristics of women diagnosed with maternal syphilis in Brazil, 2010-2018A,B
| .. | Total | Did Not Receive Penicillin | Received Penicillin | |
|---|---|---|---|---|
| .. | n (%) | n (%) | n (%) | p-valueC |
| Outcome Total | 215,937 (100%) | 18,783 (8·7%) | 197,154 (91·3%) | .. |
| Age Median (IQR) | 23·0 (19·0, 28·0) | 24·0 (20·0, 30·0) | 23·0 (19·0, 28·0) | <0·001 |
| Under 20 | 58,759 (27·2%) | 4,199 (22·4%) | 54,560 (27·7%) | .. |
| 20-29 | 112,721 (52·2%) | 9,888 (52·6%) | 102,833 (52·2%) | .. |
| 30 or Older | 44,452 (20·6%) | 4,696 (25·0%) | 39,756 (20·2%) | .. |
| Unknown | 5 (<1%) | 0 (0%) | 5 (<1%) | .. |
| Self-Identified Race | .. | .. | .. | <0·001 |
| White | 67,076 (31·1%) | 5,608 (29·9%) | 61,468 (31·2%) | .. |
| Black | 25,731 (11·9%) | 2,030 (10·8%) | 23,701 (12·0%) | .. |
| Mixed or Indigenous | 106,860 (49·5%) | 9,197 (49·0%) | 96,663 (49·5%) | .. |
| Unknown | 16,270 (7·5%) | 1,948 (10·4%) | 14,322 (7·3%) | .. |
| Education | .. | .. | .. | <0·001 |
| Some Primary School | 66,053 (30·6%) | 5,612 (29·9%) | 60,441 (30·7%) | .. |
| Some Secondary School | 50,862 (23·6%) | 3,828 (20·4%) | 47,034 (23·9%) | .. |
| HS Graduate or Higher | 40,134 (18·6%) | 3,219 (17·1%) | 36,915 (18·7%) | .. |
| Unknown | 58,888 (27·3%) | 6,124 (32·6%) | 52,764 (26·8%) | .. |
| Population Density | .. | .. | .. | <0·001 |
| Urban | 192,370 (89·0%) | 16,721 (89·0%) | 175,649 (89·1%) | .. |
| Rural or Periurban | 17,032 (7·9%) | 1,398 (7·4%) | 15,634 (7·9%) | .. |
| Unknown | 6,535 (3·0%) | 664 (3·5%) | 5,871 (3·0%) | .. |
N=215,937. Data requested from SINAN, the national syphilis reporting system of the Ministry of Health, Brazil
Maternal syphilis was defined as a reactive VDRL titer with a confirmatory treponemal test (fluorescent Treponemal antibody-absorption, micro-hemagglutination Treponema pallidum assay, Treponema pallidum hemagglutination assay, enzyme-linked immunosorbent assay, or lateral flow assay)
p-value obtained from Kruskal-Wallis tests for continuous variables, and χ2 tests for categorical variables
The heat map of Brazil (Figure 1) demonstrates significant variation in maternal syphilis cases by state. The highest number of cases was observed in São Paulo (n=52,451, 24·3% of all cases), followed by Rio de Janeiro (n=26,838, 12·4% of all cases).
Figure 1: Reported cases of maternal syphilis by state, Brazil 2010 to 2018 (n=215,937).
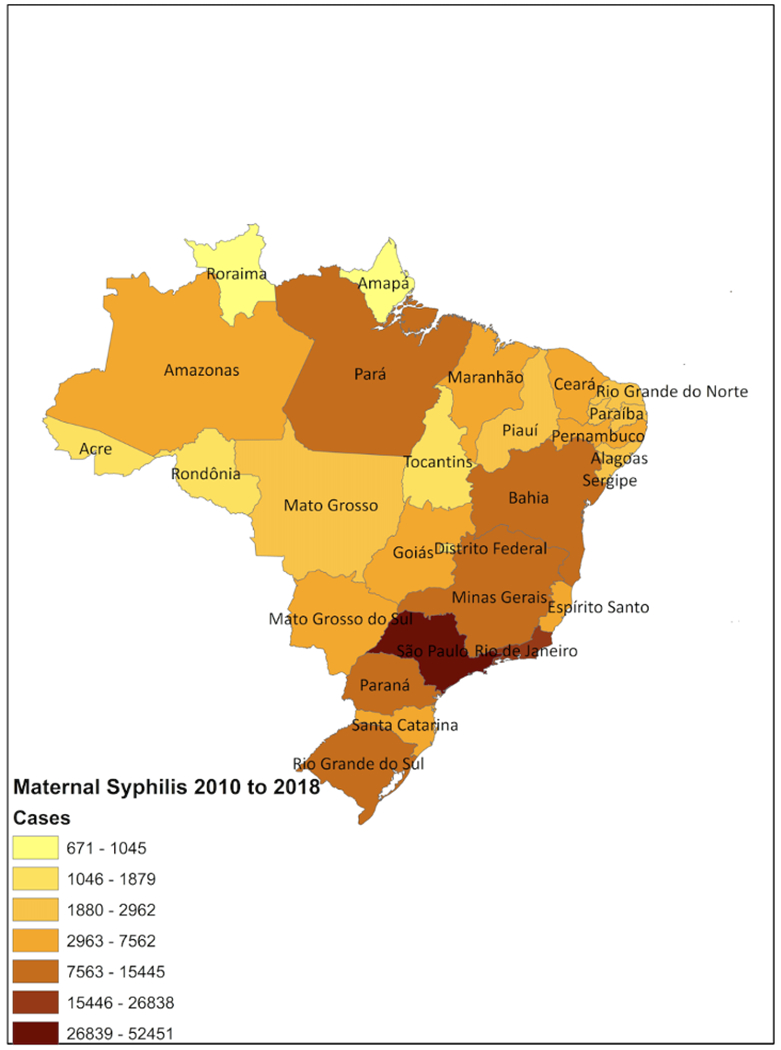
Heat map of maternal syphilis cases in Brazil from 2010 to 2018 as reported to SINAN (Sistema de Informação de Agravos de Notificação/ Brazilian Information System for Notifiable Diseases), the Brazilian Ministry of Health. Darker colors correspond with more case dense areas.
Figure 2 reveals an increase in cumulative maternal syphilis diagnoses in Brazil from 2010-2018. Only 8,704 cases of maternal syphilis were identified in 2010, compared to 46,340 cases in 2018. While the case load steadily increased annually, the number of maternal syphilis cases not treated with penicillin remained stable from 2010 to 2018.
Figure 2: Cumulative maternal syphilis detection in Brazil 2010–2018.
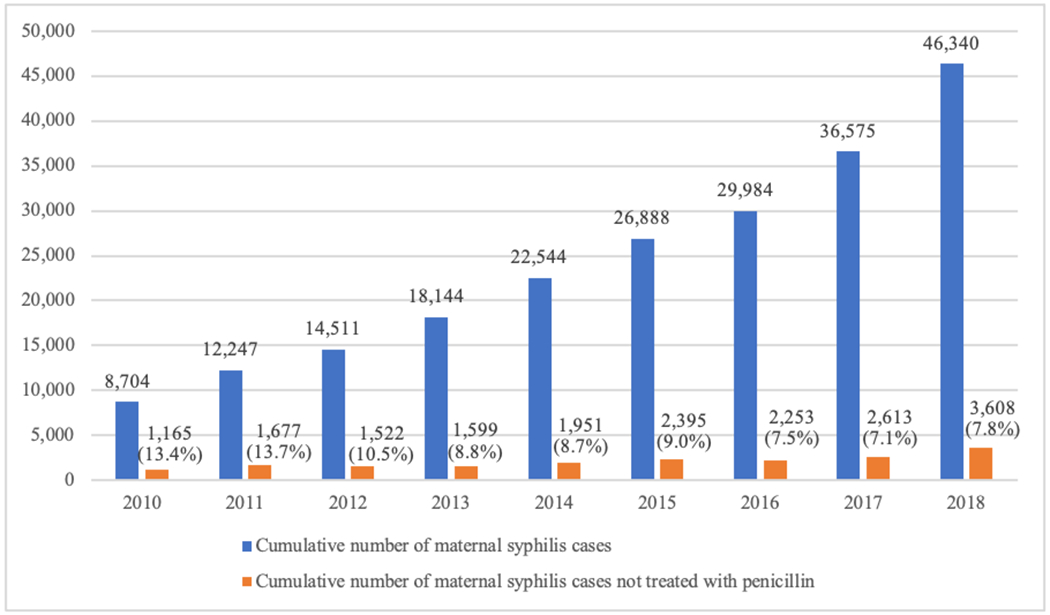
An annual display of the number of maternal syphilis cases and the number of cases not treated with penicillin as reported to SINAN, the national syphilis reporting system of the Ministry of Health, between 2010 and 2018. Maternal syphilis was defined as a reactive VDRL titer with a confirmatory treponemal test (fluorescent Treponemal antibody-absorption, micro-hemagglutination Treponema pallidum assay, Treponema pallidum hemagglutination assay, enzyme-linked immunosorbent assay, or lateral flow assay).
Table 1B shows clinically descriptive characteristics of our final study population stratified by penicillin use. The majority of women in the study population received pre-natal care (92·2%), and 83·2% of women that did not receive penicillin were engaged in pre-natal care, compared to the 93·0% of women that received penicillin (p<0·001). Despite the majority having access to pre-natal care, 61·7% of women who did not receive penicillin were diagnosed in the third trimester (p<0·001). Nearly two-thirds (63·3%) of women who did not receive penicillin had titers <1:16, compared to 53·2% of women who received penicillin (p-value <0·001).
Table 1B:
Clinical descriptive characteristics of women diagnosed with maternal syphilis in Brazil, 2010-2018A,B
| .. | Total | Did Not Receive Penicillin | Received Penicillin | .. |
|---|---|---|---|---|
| .. | n (%) | n (%) | n (%) | p-valueC |
| Outcome Total | 215,937 (100%) | 18,783 (8·7%) | 197,154 (91·3%) | .. |
| Prenatal Care | .. | .. | .. | <0·001 |
| No Prenatal Care | 16,899 (7·8%) | 3,147 (16·8%) | 13,752 (7·0%) | .. |
| Received Prenatal Care | 199,038 (92·2%) | 15,636 (83·2%) | 183,402 (93·0%) | .. |
| Syphilis Titer | .. | .. | .. | <0·001 |
| <1:16 | 116,782 (54·1%) | 11,885 (63·3%) | 104,897 (53·2%) | .. |
| ≥1:16 | 99,155 (46·0%) | 6,898 (36·7%) | 92,257 (46·8%) | .. |
| Trimester of Pregnancy at Diagnosis | .. | .. | .. | <0·001 |
| First | 68,836 (31·9%) | 3,751 (20·1:16 | 65,085 (33·0%) | .. |
| Second | 63, 079 (29·2%) | 3,448 (18·4%) | 59,631 (30·2%) | .. |
| Third or postnatal | 83,808 (38·8%) | 11,681 (61·7%) | 72,227 (36·6%) | .. |
| Unknown | 214 (0·10%) | 3 (<1%) | 211 (0·1%) | .. |
| Time related to Penicillin Shortage | .. | .. | .. | <0·001 |
| Before Penicillin Shortage (2010-2013) | 53,606 (24·8%) | 5,963 (31·7%) | 47,643 (24·2%) | .. |
| During Penicillin Shortage (2014-2016) | 79,416 (36·8%) | 6,599 (35·1%) | 72,817 (36·9%) | .. |
| After Penicillin Shortage (2017-2018) | 82,915 (38·4%) | 6,221 (33·1%) | 76,794 (38·9%) | .. |
N=215,937. Data requested from SINAN, the national syphilis reporting system of the Ministry of Health, Brazil
Maternal syphilis was defined as a reactive VDRL titer with a confirmatory treponemal test (fluorescent Treponemal antibody-absorption, micro-hemagglutination Treponema pallidum assay, Treponema pallidum hemagglutination assay, enzyme-linked immunosorbent assay, or lateral flow assay)
p-value obtained from Kruskal-Wallis tests for continuous variables, and χ2 tests for categorical variables
Table 2 shows the crude and adjusted odds ratios (AOR) of the random effects model. The odds of receiving penicillin treatment is 1·44 times higher among women with titers ≥1:16 compared to those with low titers (AOR 1·44, 95% CI: 1·39,1·48). The greatest predictor of penicillin treatment was pre-natal care (AOR 2·12, 95% CI: 2·02,2·21). Self-identified Black pregnant women had 16% increased odds of penicillin treatment (AOR 1·16, 95% CI: 1·10,1·22). The odds of receiving penicillin treatment also varied in relation to the penicillin shortage. During the penicillin shortage (2014-2016), women had a 1·34 increased odds of receiving penicillin compared to the years before the shortage (95% CI: 1·29,1·39). Similarly, after the penicillin shortage (2017-2018), women had 1·46 increased odds of receiving penicillin compared to before the shortage (95% CI: 1·41,1·52). Factors that demonstrated a negative relationship with penicillin treatment when controlling for patient level characteristics were age and trimester of diagnosis during pregnancy: age ≥ 30 was associated with a 0·74 reduced odds of penicillin treatment (AOR 0·74, 95% CI: 0·70,0·77), and diagnosis of syphilis in the third trimester was associated with 0·41 reduced odds of penicillin treatment (AOR 0·41, 95% CI: 0·39,0·43).
Table 2:
Crude and adjusted odds ratios (OR) for factors associated with penicillin treatment among women with maternal syphilis in Brazil, 2010 to 2018 (N=215,937)
| .. | Crude OR | Adjusted OR | ||||
|---|---|---|---|---|---|---|
| .. | Receive Penicillin Treatment | Receive Penicillin Treatment | ||||
| .. | OR | 95% CI | P Value | OR | 95% CI | P Value |
| Age (years) | .. | .. | .. | .. | .. | .. |
| <20 | 1·00 | Reference | Ref | 1·00 | Reference | Ref |
| 20-29 | 0·80 | 0·76-0·82 | <0·001 | 0·86 | 0·82-0·89 | <0·001 |
| ≥30 | 0·63 | 0·60-0·66 | <0·001 | 0·74 | 0·70-0·77 | <0·001 |
| Race | .. | .. | .. | .. | .. | .. |
| White | 1·00 | Reference | Ref | 1·00 | Reference | Ref |
| Black | 1·08 | 1·02-1·14 | <0·01 | 1·16 | 1·10-1·22 | <0·001 |
| Mixed or indigenous | 0·94 | 0·91-0·98 | <0·01 | 1·04 | 1·00-1·08 | <0·05 |
| Education | .. | .. | .. | .. | .. | .. |
| Some Primary School | 1·00 | Reference | Ref | 1·00 | Reference | Ref |
| Some Secondary School | 1·12 | 1·07-1·17 | <0·001 | 1·06 | 1·02-1·11 | <0·001 |
| HS Graduate or Higher | 1·02 | 0·98-1·07 | <0·30 | 1·00 | 0·96-1·04 | <0·90 |
| Population Density | .. | .. | .. | .. | .. | .. |
| Urban | 1·00 | Reference | Ref | 1·00 | Reference | Ref |
| Rural or Periurban | 1·12 | 1·06-1·19 | <0·001 | 1·07 | 1·00-1·13 | <0·05 |
| Prenatal Care | .. | .. | .. | .. | .. | .. |
| No Prenatal Care | 1·00 | Reference | Ref | 1·00 | Reference | Ref |
| Received Prenatal Care | 2·59 | 2·48-2·70 | <0·001 | 2·12 | 2·02-2·21 | <0·001 |
| Syphilis Titer | .. | .. | .. | .. | .. | .. |
| <1:16 | 1·00 | Reference | Ref | 1·00 | Reference | Ref |
| ≥1:16 | 1·54 | 1·49-1·58 | <0·001 | 1·44 | 1·39-1·48 | <0·001 |
| Trimester of Pregnancy at Diagnosis | .. | .. | .. | .. | .. | .. |
| First Trimester | 1·00 | Reference | Ref | 1·00 | Reference | Ref |
| Second Trimester | 0·99 | 0·94-1·04 | <0·70 | 1·00 | 0·96-1·05 | <0·90 |
| Third Trimester or Postnatal | 0·37 | 0·35-0·38 | <0·001 | 0·41 | 0·39-0·43 | <0·001 |
| Time related to Penicillin Shortage | .. | .. | .. | .. | .. | .. |
| Before Penicillin Shortage (2010-2013) | 1·00 | Reference | Ref | 1·00 | Reference | Ref |
| During Penicillin Shortage (2014-2016) | 1·43 | 1·38-1·48 | <0·001 | 1·34 | 1·29-1·39 | <0·001 |
| After Penicillin Shortage (2017-2018) | 1·61 | 1·55-1·68 | <0·001 | 1·46 | 1·41-1·52 | <0·001 |
Discussion
While the standard of care remains a penicillin-based regimen for all women with maternal syphilis, our study found that 8·7% of maternal syphilis cases diagnosed from 2010 to 2018 in Brazil were not treated with the recommended antibiotic. High non-treponemal titers were associated with a 44% increased odds of penicillin administration, suggesting providers may use a titer threshold of ≥1:16 in the decision process. The possibility of false positive results and questionable clinical relevance of low non-treponemal titers may be likely influencing penicillin treatment management. A study from Uganda of 215 sera from patients with reactive RPR found significant differences between RPR titers when evaluated at four additional reference laboratories (Wilcoxon rank p-value <0·001), with up to three-fold differences between facilities (Hamill et al., 2018). In addition to variability in titers, low non-treponemal titers are associated with a reduced risk of syphilis MTCT and adverse pregnancy outcomes (Yeganeh et al., 2015, Wendel et al., 2002). Consistent with studies on HIV and syphilis co-infection in southern Brazil, a large retrospective cohort study of 3,474 women with maternal syphilis in China from 2011 to 2018 found that TRUST titers ≥1:8 were independently associated with adverse pregnancy outcomes (Kwak, 2015, Hu et al., 2020). Low non-treponemal titers can be considered a “serological scar” resulting from a previously treated syphilis infection. As a result of high syphilis prevalence, it is common practice in Brazil for clinicians to interpret lower titers as remnants of an old infection that does not need treatment. In response to a similar drug shortage of generic injectables in 2012, Canadian hospitals developed a framework that called for optimization of therapeutic benefit through triage (Singleton et al., 2013). The clinical significance of low non-treponemal titers may have influenced providers in Brazil to opt for-non penicillin alternatives or no treatment as a form of triage during the penicillin shortage. As a large database study, we were unable to tease out clinical reasoning of low titer infections. Future studies including qualitative research are needed to investigate the role of low titers in clinician treatment decisions.
Our study showed that 83% of the pregnant women who did not receive penicillin had pre-natal care. While specific information regarding number of visits or details of visits were not available, our findings stand in stark contrast to the predominant narrative that women who do not receive adequate syphilis treatment are not engaged in pre-natal care. This exposes a major area for improvement at the public health and provider levels and shifts responsibility from the individual woman to the public health sector. While WHO guidelines strongly recommend that all pregnant women receive at least one-time syphilis screening during the first antenatal care visit, the CDC recommends triple testing in high-prevalence regions: once during the first pre-natal visit, again between 28-32 weeks, and last at delivery (World Health Organization, 2019, Center for Disease Control, 2019). This testing strategy would capture new infections that occur during pregnancy, presumably introduced by the partner.
Starting in 2014, 39 out of 95 countries (41%), including Brazil, reported a BPG shortage (Nurse-Findlay et al., 2017). The severity of the penicillin shortage varied among Brazilian states and followed different timelines (Araujo et al., 2020). It is notable that in our analysis, women were more likely to receive penicillin during and after the penicillin shortage, compared to before the shortage. This may reflect the effect of Projeto Nascer, a nation-wide public health campaign to improve maternal and congenital syphilis testing and treatment (Projeto Nascer, 2020). Furthermore, due to market exits and quality disruptions of BPG in 2015, Brazil issued an official recommendation of alternate treatment regimens for non-pregnant women with syphilis, prioritizing pregnant women for penicillin treatment (Nurse-Findlay et al., 2017). BPG was scarce between 2014 and 2017 and those available in stock were intended for gestational and congenital syphilis (Araujo et al., 2020). Regardless of both yearly increases in pre-natal care and penicillin treatment, cases of maternal syphilis in Brazil continue to rise, suggesting there are other factors contributing to the epidemic not addressed by past and current health initiatives. Specific states may have responded differently to the epidemic due to differences in case load. On a global scale, adaptive changes made in the clinical diagnostic practice of countries that experienced a BPG shortage may be possible contributors to local syphilis epidemics.
Factors that showed an association with increased likelihood of receiving penicillin treatment in the RE model include self-identified race, education, and population density. Significance of these findings is likely a product of population size rather than true difference (Lantz et al., 2013). Alternatively, age ≥ 30 and syphilis diagnosis during the third trimester were associated with reduced odds of penicillin administration. We do not have access to previous history of syphilis, which may explain why providers would not treat older mothers with persistently positive titers. Reduced penicillin administration among women diagnosed in the third trimester may be the product of syphilis re-infection by untreated partners. The details of treatment for the partner were missing for 68·6% of the study population. A study from Peru of 144 seropositive pregnant women showed that only 33·7% of partners received a dose of penicillin (Garcia et al., 2015). In this study, women identified the provider as the main influence for partner notification and treatment, yet a minority of providers have received training for this type of counseling (Garcia et al., 2015).
Our study has several strengths and is the first to specifically examine the relationship between titers and treatment selection (Liu et al., 2019). The RE model allowed us to adjust for significant geographic variation to better characterize syphilis hot spots; information that can be used to build a global profile to identify areas at risk. Additionally, the vast nature of our study included a secular trend of increasing maternal syphilis cases, as well as a period of penicillin shortage that might not have been accurately captured in a smaller study.
While our model is based on previous literature, omitted variable bias in relation to nature of pre-natal care, penicillin treatment alternatives, and partner treatment specifics remains a possibility. Of note, Table 1A showed significant differences in age, race, education, and population density, possibly due to the large sample size (Greenland et al., 2016). Overall, the distributions between patients that received and did not receive penicillin treatment were similar, further supporting a lack of true significance.
In the largest cross-sectional study to-date to evaluate factors associated with penicillin treatment among women with maternal syphilis, we found that women with high non-treponemal titers (≥1:16) were more likely to receive penicillin. Providers may incorrectly use low titers as a way to ration treatment. Although it is unclear how these prescribing practices have contributed to the current maternal syphilis epidemic, states with high prevalence of syphilis in particular may benefit from targeted public health efforts. Regardless of adherence to the WHO guidelines, Brazil continues to experience a huge syphilis epidemic, exposing an implementation science conundrum. The yearly increases in cases of pregnant women with syphilis despite high rates of engagement in pre-natal care reflects the need for initiatives to address specific contributing factors. While high titer thresholds for penicillin treatment may be one contributor to the growing syphilis epidemic, other factors to investigate include the quality of pre-natal care, loss to follow up, treatment of partners, and co-infection with HIV. A multi-pronged approach is desperately needed to quell the maternal syphilis epidemic.
Supplementary Material
Highlights.
Rates of syphilis in pregnancy increased five-fold from 2010 to 2018 in Brazil
18,783 pregnant women with a positive syphilis titer did not receive penicillin treatment
Absence of pre-natal care was not the barrier to syphilis treatment
Women with a titer of <1:16 had reduced odds of receiving penicillin
Acknowledgements
Mary Catherine Cambou was supported by the UCLA Postdoctoral Fellowship Training Program in Global HIV Prevention Research (Currier and Gorbach, PIs). Emma Jane Swayze was supported by the UCLA South American Program in HIV Prevention Research Program, funded by the NIH/NIMH (PI: J Clark).
Funding
MCC and EJS were supported by the National Institute of Health and the National Institutes of Mental Health grants (T32MH080634) and (R25MH087222) respectively. Funding sources did not have a role in study design, collection, analysis and interpretation of data, in writing of the manuscript, or in decision to submit the manuscript for publication.
Footnotes
Publisher's Disclaimer: This is a PDF file of an article that has undergone enhancements after acceptance, such as the addition of a cover page and metadata, and formatting for readability, but it is not yet the definitive version of record. This version will undergo additional copyediting, typesetting and review before it is published in its final form, but we are providing this version to give early visibility of the article. Please note that, during the production process, errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosure of relationships and activities
All authors declare no competing interests.
Prior publications:
This research has not been published and is not currently submitted elsewhere as an abstract, presentation, or manuscript.
Ethics
This study used publicly available de-identified data, and was therefore IRB exempt.
References
- 1.Araujo S et al. Who was affected by the shortage of penicillin for syphilis in Rio de Janeiro, 2013–2017?. Revista de saude publica. 2020;54:109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bezerra M, Fernandes F, de Oliveira J, de Araujo S, Randau K. Congenital Syphilis as a Measure of Maternal and Child Healthcare, Brazil. Emerg Infect Dis. 2019;25:8:1469–1476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Boletim Epidemiológico Sífilis 2019. Departamento de Doenças de Condições Crônicas e Infecções Sexualmente Transmissíveis 2019. [Available from: http://www.aids.gov.br/pt-br/pub/2019/boletim-epidemiologico-sifilis-2019]. [Google Scholar]
- 4.Cambou M Are HIV and Syphilis Syndemic Among Pregnant Women in Brazil? Poster session presented at: 10th Annual IAS conference on HIV science; 2019. July 21–24; Mexico City, Mexico. [Google Scholar]
- 5.Centers for Diseae Control and Prevention. Screening Recommendations: Clinician Timeline for Screening Syphilis, HIV, HBV, HCV, Chlamydia, and Gonorrhea 2019. [Available from: https://www.cdc.gov/nchhstp/pregnancy/screening/clinician-timeline.html]. [Google Scholar]
- 6.Garcia P, Williams E, Cárcamo C, et al. Partner Notification Among Peruvian Pregnant Women With Syphilis. Sex Transm Dis. 2015;42(8):457–62. [DOI] [PubMed] [Google Scholar]
- 7.Gardiner J, Luo Z, Roman L. Fixed effects, random effects and GEE: what are the differences? Stat Med. 2009;28:2:221–39. [DOI] [PubMed] [Google Scholar]
- 8.Greenland S, Senn SJ, Rothman KJ, et al. Statistical tests, P values, confidence intervals, and power: a guide to misinterpretations. Eur J Epidemiol. 2016;31:4:337–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hamill M, Mbazira K, Kiragga A, et al. Challenges of Rapid Plasma Reagin Interpretation in Syphilis Screening in Uganda: Variability in Nontreponemal Results Between Different Laboratories. Sex Transm Dis. 2018;45:12:829–833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hu F, Guo S, Lu J, et al. The Effect of Different Treatment Regimens and Multiple Risk Factors on Adverse Pregnancy Outcomes among Syphilis-Seropositive Women in Guangzhou: A Retrospective Cohort Study. Biomed Res Int. 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kwak J, Lamprecht C. A review of the guidelines for the evaluation and treatment of congenital syphilis. Pediatr Ann. 2015;44:5. [DOI] [PubMed] [Google Scholar]
- 12.Lantz B The large sample size fallacy. Scand J Caring Sci. 2013;27:2:487–92. [DOI] [PubMed] [Google Scholar]
- 13.Liu H, Chen N, Yu J, et al. Syphilis-attributable adverse pregnancy outcomes in China: a retrospective cohort analysis of 1187 pregnant women with different syphilis treatment. BMC Infect Dis. 2019;19:1:292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Newman L, Kamb M, Hawkes S, et al. Global estimates of syphilis in pregnancy and associated adverse outcomes: analysis of multinational antenatal surveillance data. PLoS Med. 2013;10:2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Nurse-Findlay S, Taylor M, Savage M, Mello M, et al. Shortages of benzathine penicillin for prevention of mother to-child transmission of syphilis: An evaluation from multi-country surveys and stakeholder interviews. PLoS Med. 2017;14:12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Projeto Nascer Série F. Comunicação e Educação em Saúde. Projeto Nascer. MINISTÉRIO DA SAÚDE Secretaria-ExecutivaPrograma Nacional de DST e Aids [Available from: http://bvsms.saude.gov.br/bvs/publicacoes/projeto_nascer.pdf]. [Google Scholar]
- 17.Saúde M Indicadores e Dados Básicos da Sífilis nos Municípios Brasileiros. Available from: http://indicadoressifilis.aids.gov.br/. [Google Scholar]
- 18.Singleton R, Chubbs K, Flynn J, et al. From framework to the frontline: designing a structure and process for drug supply shortage planning. Healthc Manage Forum. 2013;1:41–45. [DOI] [PubMed] [Google Scholar]
- 19.Wendel G, Sheffield J, Hollier L, Ramsey P, Sánchez P. Treatment of syphilis in pregnancy and prevention of congenital syphilis. Clin Infect Dis. 2002;15:35. [DOI] [PubMed] [Google Scholar]
- 20.World Health Organization. WHO validation for the elimination of mother-to-child transmission of HIV and/or syphilis 2019. [Available from: https://www.who.int/reproductivehealth/congenital-syphilis/WHO-validation-EMTCT/en/]. [Google Scholar]
- 21.Yeganeh N, Watts HD, Camarca M, et al. Syphilis in HIV-infected mothers and infants: results from the NICHD/HPTN 040 study. Pediatr Infect Dis J. 2015;34:3. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


