Abstract
Purpose:
Adolescent vaping has reached epidemic levels. Identifying factors associated with electronic (e-)cigarette use initiation could inform prevention programming. This study examined whether parental attitudes towards e-cigarettes impacted adolescent e-cigarette use intentions, positive expectancies of use, and actual use when accounting for adolescent attitudes and peer norms. Parents’ negative attitudes towards e-cigarettes were expected to reduce teen e-cigarette use intentions. Low e-cigarette use intentions were expected to mediate the association between parental attitudes and teen e-cigarette use. Peer norms were expected to be associated with positive expectancies. Positive expectancies were expected to mediate the association between peer norms and teen e-cigarette use.
Methods:
A sample of e-cigarette naïve adolescents (n = 176, 14–17 years old, 52% female, 82% Latinx/Hispanic) and their parents were assessed. Parents and adolescents rated harm associated with e-cigarette use. Adolescents reported their perceptions of peer e-cigarette norms, intentions, positive expectancies, and e-cigarette use. Cross-sectional models were estimated for e-cigarette use intentions and positive expectancies. Prospective mediation models (n = 142) characterized pathways to e-cigarette use.
Results:
Parents’ attitudes towards e-cigarettes were associated with weaker intentions. Intentions mediated the association between parental attitudes and e-cigarette use. Adolescents reporting favorable e-cigarette peer norms endorsed more positive expectancies. Positive expectancies did not mediate the association between peer norms and e-cigarette use.
Conclusions:
Parents actively shape adolescent e-cigarette use even when accounting for peer norms and adolescent attitudes. Involving parents in prevention programming may help reduce teen vaping. These associations should be examined with a larger and more diverse sample.
Keywords: e-cigarettes, adolescents, parents, peers
Introduction
Adolescent electronic (e-)cigarette use has reached epidemic levels despite evidence of its health dangers.1 In 2018, Monitoring the Future (MTF) estimated that 21% of 12th graders reported past month vaping, nearly double the rate from the previous year.2 This represented the largest single-year increase for any substance over the four decades of the annual survey. This is alarming because most e-cigarettes contain nicotine, which can have long-term negative impacts on brain development and behavior, including effects on cognition,3 attention,4 mood,5 and increased risk for drug dependence.6 Vaping also increases the risk of cigarette smoking7 and has been associated with negative cardiovascular effects,8 development of respiratory symptoms,9 and reduced pulmonary immune function.10 Thus, understanding factors relevant to early stages of e-cigarette use can help inform preventative interventions aimed at reducing e-cigarette use and improving health among adolescents.
Social Learning Theory (SLT)11 posits that adolescents use cognitive representations shaped by observing influential people’s attitudes and behavior to inform decisions on whether to engage in substance use behaviors. That is, if valued social referents hold favorable attitudes towards, or actually use substances, then an adolescent is more likely to mirror these attitudes and behaviors. A key socialization context during adolescence is peers.12 According to SLT11, adolescents do not need to directly observe peers engaging in substance use behavior. Rather, the mere perception that their peer group either approves of (i.e., injunctive norms) or engages in (i.e., descriptive norms) substance use behavior can promote experimentation.13 In fact, perceived peer approval and use of substances may be particularly influential on early stages of substance use, such as the formation of positive expectancies of use and substance use intentions, when direct peer pressure is rare.14 Although some have advocated that a parent’s influence on substance use behavior becomes negligible as peers’ influence becomes more salient during adolescence,12 others have refuted this perspective as adolescents remain connected to parents for guidance and support.15,16 Indeed, prior studies have highlighted that both peers17,18 and parents19 influence e-cigarette use. Yet, these investigations have been limited to cross-sectional designs, focused on current e-cigarette users, largely only involved self-reports, and considered parental and peer influences in separate models. The goal of the current study was to examine parental and peer influences on early stages of e-cigarette use (i.e., positive expectancies, intentions to use). Possible mechanisms linking socialization effects on actual e-cigarette use were also characterized using prospective data. Parents’ perceptions of the harms of e-cigarette use were expected to reduce teens’ e-cigarette use intentions. E-cigarette use intentions were expected to mediate the association between parental attitudes and later teen e-cigarette use. Peer norms were expected to be associated with positive expectancies. Positive expectancies were expected to mediate the association between peer norms and later teen e-cigarette use.
Methods
Study Sample
Adolescents (N = 264) were enrolled into an ongoing, multi-wave, study investigating e-cigarette initiation among at-risk youth. To be eligible, participants had to be freshmen or sophomores at a local area public high school, have no diagnosis of a learning, intellectual, or physical disability making it difficult to complete study procedures, have no diagnosis of a neurological disorder or disorder characterized by psychotic or paranoid symptoms, including severe forms of bipolar disorder, and be able to speak and understand English. Additionally, given that the larger study’s primary objective was to identify adolescents that were slightly more at-risk for engaging in substance use during the course of high school, adolescents had to endorse at least one of the following risk factors: a high score on impulsivity (>10) and/or sensation seeking (>14)20, endorse that a friend or sibling had tried a substance, or endorse intentions to use cigarettes and/or e-cigarettes. Yet, only 2.6% of participants that were screened did not meet a high-risk criterion, suggesting that this sample is likely representative of regional high school students.
For the cross-sectional models, the goal was to predict e-cigarette use intentions at time 1. Some data suggests that etiological processes are different for initiation, maintenance, and escalation of substance use.21 Accordingly, adolescents reporting lifetime e-cigarette use at time 1 were removed so that intentions to initiate could be unambiguously examined. This strategy has been used in previous research.22 Thus, 176 adolescents (Mage = 14.88, SD = 0.66) were included in cross-sectional models. The subsample was predominately female (52%), White (84%), and Latinx/Hispanic (82%), and did not differ demographically from the full sample. For the prospective mediation models, participants with available time 2 (approximately 15 months after time 1) data were examined, including those reporting lifetime e-cigarette use at time 1. Participants (n = 142; Mage = 14.99, SD = 0.72) were predominately female (62%), White (87%), and Latinx/Hispanic (82%). A higher percentage of females (χ2 [1, N = 264] = 15.46, p < .001) completed their time 2 assessment at the time of this study.
Procedures
Adolescents provided contact information for their parents during recruitment events. Parents were then contacted and provided with study information. Eligibility screens with adolescents and a parent were completed by phone. During study visits, staff obtained informed consent and assent from parents and adolescents, respectively. Adolescents and parents completed questionnaires on tablets separately in private testing rooms through REDCap.23 Families were compensated up to $75 for survey completion. The institutional review board at Florida International University approved the study.
Measures
Peer Norms.
At time 1, adolescents responded to items adapted from MTF2 that reflect perceived peer approval and peer use of e-cigarettes. Items included, “how much do your three closest friends approve/disapprove of vaping/use of e-cigarettes?” (1 = “strongly disapprove” to 7 = “strongly approve”) and “how often do your three closest friends vape/use e-cigarettes?” (1 = “never” to 7 = “daily”). These items were standardized and then averaged.
Perceived Harm of E-Cigarettes.
At time 1, parents and adolescents rated perceived harm of e-cigarette use (“In your opinion, how much do people harm themselves when they use e-cigarettes?”). Response options ranged from 0 = “No harm” to 3 = “A lot of harm.” This item was adapted from MTF.2
Positive E-Cigarette Use Expectancies.
The Electronic Cigarettes Attitudes Survey (ECAS24) was used to assess e-cigarette expectancies at time 1. Of particular interest, were three items that focused on flavoring (“the fruit and candy flavors available with e-cigarettes/ENDS is particularly appealing to kids my age”), social benefits (“smoking e-cigarettes/ENDS is cool and might make me more popular”), and individuality (“e-cigarettes/ENDs allows people to show their individuality and personality by customizing their product [e.g., vape pen]”) expectancies as prior work indicates that these are among the most salient reasons adolescents endorse for initiating e-cigarette use.17 Expectancy items were examined separately in order to identify possible nuances consistent with prior work.25 Items were rated from 1 = “strongly disagree” to 5 = “strongly agree.”
Intentions to Use.
At time 1, adolescents reported on the likelihood that they would use e-cigarettes within the next five years (1 = “I definitely will not” to 5 = “I definitely will”).
E-Cigarette Use.
At time 1, adolescents reported on lifetime e-cigarette use (yes/no). At time 2, adolescents reported e-cigarette use since the time 1 assessment (yes/no). Items assessing e-cigarette use were adapted from the Population Assessment of Tobacco and Health Study.26
Demographic Information.
Given prior work that e-cigarette use differs across demographic characteristics2, age, biological sex, and race were included as covariates across models.
Statistical Analysis
All study variables were normally distributed. Descriptive statistics and correlations were calculated for all variables. Ordinary least squares (OLS) regression was used to estimate the cross-sectional models using SAS v9.4.27 The unique effects of parental perceived harm of e-cigarettes, adolescent perceived harm of e-cigarettes, and peer norms on the three positive e-cigarette use expectancies and e-cigarette use intentions were analyzed in four separate models. Squared semipartial correlations (sr2) are presented to provide effect size estimates. Next, prospective path models in Mplus v7.428 were used to estimate the unique effects of parental perceived harm of e-cigarettes (time 1), adolescent perceived harm of e-cigarettes (time 1), peer norms (time 1), and lifetime e-cigarette use (time 1) on later (time 2) e-cigarette use via positive expectancies and intentions as mediators. Given the strong association between intentions and the three positive expectancy items (range of rs = 0.11–0.45), four separate models were estimated to minimize multicollinearity issues. All path models were just-identified. One advantage of a prospective design is that it establishes temporal precedence between the mediator and outcome, a key criterion for establishing mediation.29 Mediated effects were estimated by calculating bias-corrected bootstrap confidence intervals (BBCIs), which represent robust estimators of indirect effects.30
Results
Table 1 provides the descriptive statistics for all cross-sectional study variables among the subsample of e-cigarette use naïve adolescents. Noteworthy, although peer norms were not associated with adolescent perceived harm of e-cigarettes or intentions to use, peer norms were associated with two of the three positive e-cigarette use expectancies. Although parental perceived harm of e-cigarettes was not associated with adolescent perceived harm, both perceptions were negatively associated with e-cigarette use intentions. Only perceptions of e-cigarettes as showing one’s individuality were significantly associated with use intentions.
Table 1.
Means, standard deviations, and correlations of study variables
| Mean | SD | Correlations | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | |||
| 1. Biological Sexa | 0.48 | 0.50 | |||||||||
| 2. Age | 14.88 | 0.66 | −0.01 | ||||||||
| 3. Raceb | 0.15 | 0.36 | 0.16 | −0.06 | |||||||
| 4. Parental Perceived Harm | 3.70 | 0.52 | 0.01 | 0.09 | −0.12 | ||||||
| 5. Adolescent Perceived Harm | 3.13 | 0.88 | −0.07 | −0.05 | −0.03 | −0.01 | |||||
| 6. Peer Norms | 2.33 | 1.58 | −0.03 | 0.06 | −0.07 | 0.10 | −0.10 | ||||
| 7. E-Cigarette Use Intentions | 1.53 | 0.85 | −0.12 | 0.03 | −0.02 | −0.21 | −0.37 | 0.09 | |||
| 8. Expectancy: Appealing Flavors | 4.03 | 0.88 | −0.07 | −0.06 | −0.05 | 0.09 | −0.09 | 0.25 | 0.08 | ||
| 9. Expectancy: E-Cigarettes Cool | 1.74 | 1.06 | 0.04 | 0.03 | 0.07 | −0.02 | −0.07 | 0.15 | 0.12 | 0.12 | |
| 10. Expectancy: Individuality | 2.25 | 1.20 | 0.12 | −0.05 | 0.13 | −0.07 | −0.01 | 0.16 | 0.15 | 0.14 | 0.44 |
Abbreviation: SD, standard deviation
Biological sex, 0 = female, 1 = male
Race, 0 = White, 1 = non-White
Bold values = significant Pearson correlations (p < .05)
Cross-Sectional E-Cigarette Use Expectancy Models
Cross-sectional models for positive e-cigarette use expectancies are presented in Table 2. The first model accounted for approximately 8% of the variance in perceptions of e-cigarette flavoring as appealing. Neither demographic characteristics nor perceived harm ratings were associated with perceptions of e-cigarette flavoring as appealing. Yet, as expected, peer norms were positively associated with perceptions of e-cigarette flavoring as appealing.
Table 2.
Cross-sectional Regression Models for Positive E-Cigarette Use Expectancies
| Expectancy: Appealing Flavors | Expectancy: E-Cigarettes Cool | Expectancy: Individuality | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Coefficient | SE | p-value | sr2 | Coefficient | SE | p-value | sr2 | Coefficient | SE | p-value | sr2 | |
| 5.34 | 1.54 | < 0.001 | 1.17 | 1.87 | 0.529 | 3.44 | 2.11 | 0.105 | ||||
| Biological Sexa | −0.13 | 0.13 | 0.345 | 0.005 | 0.09 | 0.16 | 0.580 | 0.002 | 0.25 | 0.18 | 0.163 | 0.011 |
| Age | −0.12 | 0.10 | 0.244 | 0.007 | 0.03 | 0.12 | 0.795 | 0.000 | −0.07 | 0.14 | 0.592 | 0.002 |
| Raceb | −0.06 | 0.18 | 0.746 | 0.001 | 0.24 | 0.22 | 0.284 | 0.007 | 0.39 | 0.25 | 0.126 | 0.013 |
| Parental Harm | 0.11 | 0.13 | 0.375 | 0.004 | −0.02 | 0.16 | 0.921 | 0.000 | −0.19 | 0.18 | 0.287 | 0.006 |
| Teen Harm | −0.08 | 0.07 | 0.279 | 0.006 | −0.06 | 0.09 | 0.535 | 0.002 | 0.02 | 0.10 | 0.816 | 0.000 |
| Peer Norms | 0.13 | 0.04 | 0.002 | 0.054 | 0.10 | 0.05 | 0.042 | 0.024 | 0.14 | 0.06 | 0.015 | 0.034 |
Biological sex, 0 = female, 1 = male
Race, 0 = White, 1 = non-White
Bold values = significant coefficients (p < .05)
The second model accounted for approximately 4% of the variance in perceptions of e-cigarettes as being cool. Again, neither demographic characteristics nor perceived harm ratings were associated with perceptions of e-cigarettes as being cool. Yet, as expected, peer norms were positively associated with adolescent perceptions of e-cigarettes as being cool.
The third model accounted for approximately 7% of the variance in perceptions of e-cigarettes as showing one’s individuality. Neither demographic characteristics nor perceived harm were associated with perceptions of e-cigarettes as showing one’s individuality. Yet, as expected, peer norms were positively associated with adolescent perceptions of e-cigarettes as showing one’s individuality.
Positive Expectancies (Time 1) and Actual E-cigarette Use (Time 2)
Prospective associations examining the role of positive e-cigarette use expectancies (time 1) as possible mediators between peer norms (time 1) on e-cigarette use (time 2) accounted for approximately 17%−23% of the variance in e-cigarette use across models. In the model examining perceptions of e-cigarette flavoring as appealing as the mediator, there was support for the role of peer norms on e-cigarette use expectancies (estimate = 0.418, p < 0.001). However, perceptions of e-cigarette flavoring as appealing did not predict later e-cigarette use. In the model examining perceptions of e-cigarettes as being cool as the mediator, there was no support for the role of peer norms on e-cigarette use expectancies. However, perceptions of e-cigarettes as being cool did predict later e-cigarette use (estimate = 0.278, p = 0.006). Lastly, in the model examining perceptions of e-cigarettes as showing one’s individuality as the mediator, there was support for the role of peer norms on e-cigarette use expectancies (estimate = 0.198, p = 0.041). However, perceptions of e-cigarettes as showing one’s individuality did not predict later e-cigarette use. Taken together, there was no support for expectancies as a mediator between peer norms on later e-cigarette use.
Cross-Sectional E-Cigarette Use Intention Models
The model accounted for approximately 21% of the variance in e-cigarette use intentions. Neither demographic characteristics nor peer norms were significantly associated with e-cigarette use intentions (Table 3). Yet, as expected, parental and adolescent perceived harm of e-cigarettes were negatively associated with e-cigarette use intentions.
Table 3.
Cross-Sectional Regression Model for Future E-Cigarette Use Intentions
| E-Cigarette Intentions | ||||
|---|---|---|---|---|
| Coefficient | SE | p-value | sr2 | |
| 3.61 | 1.37 | 0.009 | ||
| Biological Sexa | −0.22 | 0.12 | 0.062 | 0.017 |
| Age | 0.02 | 0.09 | 0.793 | 0.000 |
| Raceb | −0.07 | 0.16 | 0.686 | 0.001 |
| Parental Harm | −0.34 | 0.11 | 0.003 | 0.043 |
| Adolescent Harm | −0.36 | 0.07 | < .001 | 0.140 |
| Peer Norms | 0.04 | 0.04 | 0.315 | 0.005 |
Biological sex, 0 = female, 1 = male
Race, 0 = White, 1 = non-White
Bold values = significant coefficients (p < .05)
Use Intentions (Time 1) and Actual E-cigarette Use (Time 2)
Prospective associations examining the role of e-cigarette use intentions as a possible mediator between parental perceived harm on e-cigarette use accounted for approximately 40% of the variance in intentions to use e-cigarettes at time 1 and 20% of the variance in actual e-cigarette use at time 2 (Figure 1). Specifically, parental perceived harm of e-cigarettes predicted lower e-cigarette use intentions and, in turn, lower e-cigarette use intentions predicted lower rates of actual e-cigarette use. Moreover, as expected, there was support for the role of e-cigarette use intentions as a mediator in the association between parental perceived harm on actual adolescent e-cigarette use (estimate = −0.087, 95% BCCI [−0.233 – −0.007]). Peer norms also predicted e-cigarette use intentions, but there was weak support for the role of e-cigarette use intentions as a mediator in the association between peer norms on actual e-cigarette use (estimate = 0.024, bias-corrected bootstrap 95% confidence interval [0.000 – 0.083]. These results offer support for the role that parents have on an adolescent’s decision to engage in e-cigarette use despite perceived peer norms and an adolescent’s own attitudes towards use.
Figure 1. Prospective Model for E-Cigarette Use.
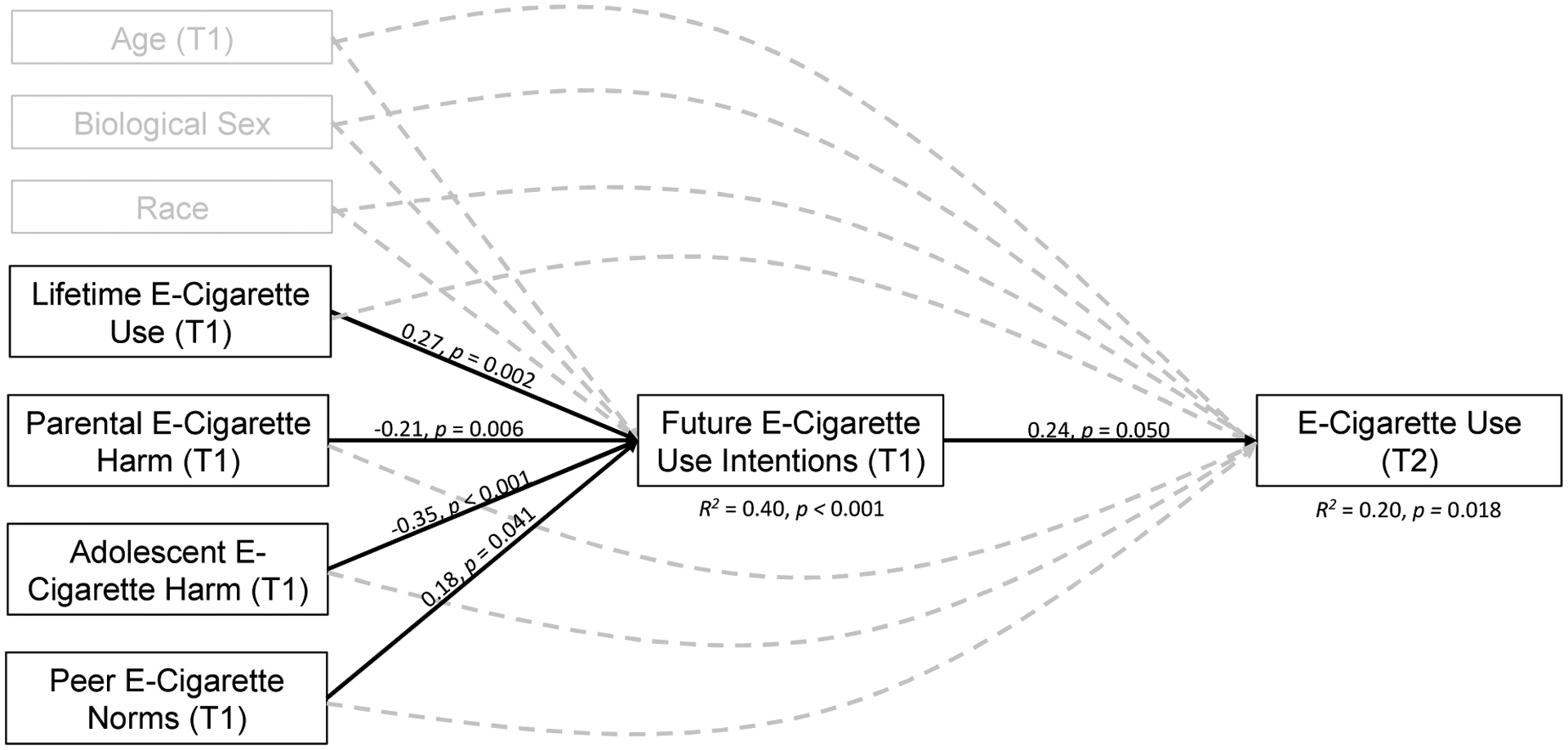
Values represent standardized path coefficients. Solid lines represent significant paths (p < .05). Dashed lines represent non-significant paths (p > .05). Covariances between exogenous variables (i.e., Time 1 lifetime e-cigarette use, parental e-cigarette harm, adolescent e-cigarette harm, peer e-cigarette norms, age, biological sex, and race) were estimated but not depicted to simplify visual presentation. The model is just-identified. T1 = Time 1 (i.e., baseline). T2 = Time 2 (i.e., approximately 15 months following baseline assessment).
Discussion
The introduction and rapid escalation of e-cigarette use has resulted in a new nicotine product landscape. There is concern that adolescents may initiate e-cigarettes without having a clear understanding of negative health effects, such as increased risk for combustible cigarette use and nicotine dependence.7 Perhaps the most effective way to counter the negative sequalae of e-cigarette use is to prevent initiation altogether. The objective of this study was to identify whether parental attitudes continue to have an impact on the early stages of e-cigarette use above and beyond adolescent attitudes and perceived peer norms. Limitations of prior work include reliance on adolescent-reports of parental attitudes, cross-sectional designs, and a sole focus on lifetime e-cigarette use. It is possible that perceived parental attitudes could be influenced by either the adolescent’s own attitudes or their own substance use behavior. The current study addressed these limitations by: 1) considering parent-reports of e-cigarette attitudes, 2) examining prospective effects on actual e-cigarette use, 3) delineating mechanisms linking parent and peer socialization effects on subsequent e-cigarette use, and 4) characterizing the influence of parental attitudes on adolescent use while accounting for adolescent attitudes and perceived peer norms.
Theoretical and empirical work have demonstrated that social contexts play a critical function in shaping substance use initiation.11,12 Peers are an especially salient influence in an adolescent’s social ecology and impact decisions to engage in substance use. However, less is known about social influences that impact e-cigarette attitudes and use. Preliminary work indicates that peer influence often operates indirectly to promote e-cigarette use. For example, the mere belief that peers either approve of or use e-cigarettes (i.e., perceived peer norms) can lead to e-cigarette use among college students.31 Peers also impact the formation of positive e-cigarette use expectancies, which typically precede use.17 Namely, prior work indicates that flavoring, social benefits, and individuality expectancies are widely reported retrospectively as reasons for initiating use among active e-cigarette users.32 Our study demonstrates that peer norms are associated with positive expectancies among e-cigarette naïve adolescents. Yet, a key finding is that positive expectancies did not mediate the association between peer norms and later e-cigarette use. This indicates that peer norms likely contribute to positive expectancies adolescents develop about e-cigarettes, but this may not suffice to influence actual e-cigarette use. That is, parental influence may ultimately buffer the effect of peer norms and positive expectancies on a teen’s decision to engage in e-cigarette use.
Although peers are primary influencers, parents continue to provide guidance and support to adolescents15,16, especially when making life decisions, such as initiating e-cigarette use. Few studies have examined the role of parents on early stages of adolescent e-cigarette use. A notable exception demonstrated that adolescents who perceived that their parents felt less negatively about e-cigarette use were more likely to use e-cigarettes.19 The current study advances the literature by demonstrating that parents’ perceptions of the harms of e-cigarette use not only influence adolescent e-cigarette use intentions (when controlling for adolescent attitudes and perceived peer norms), but also predict lower rates of e-cigarette use via e-cigarette use intentions. Interestingly, the effects of lifetime e-cigarette use did not predict later e-cigarette use. Potential explanations could be that some adolescents may have only experimented at time 1, some adolescents may have quit during the course of the study, or that intentions had a stronger impact on subsequent e-cigarette use. These findings support a critical role of parents as important socialization figures to target for e-cigarette prevention programming.
Estimates indicate that less than half of middle and high school parents are able to correctly identify popular e-cigarette products, including JUULs.33 Parents rely heavily on schools and health professionals to educate them about emerging health issues, such as e-cigarettes.34,35 Yet, most parents report receiving little communication about e-cigarettes from their child’s school18 and a majority of healthcare providers indicate feeling uncomfortable talking to adolescent patients and their parents about e-cigarettes.35 A key barrier that parents report in terms of having conversations with their children about e-cigarettes is a lack of knowledge about these products and the risks associated with their usage.33 Moreover, although most parents acknowledge that adolescent e-cigarette use is a public health concern, a large majority indicate that their adolescent child is not at risk for initiating use.33 The current study indicates that parents still play an active role in influencing early stages of e-cigarette use among their adolescent children. Thus, promoting effective and frequent parental communication with youth regarding the harms, regulations, and marketing of e-cigarettes could have utility in shaping adolescent attitudes, and ultimately reducing e-cigarette use initiation. Prior work has demonstrated that school-based e-cigarette education programs, such as the Stanford Tobacco Prevention Toolkit, that consist of youth-, parent-, and teacher-modules, significantly increased the perceived harmfulness and addictiveness of e-cigarettes among youth and reduced e-cigarette use intentions.36 Similarly, some states explicitly targeting parents in anti-e-cigarette advertisements have demonstrated success in reducing e-cigarette use among youth.37 Namely, advertisements encouraging parents to have conversations with their children about e-cigarettes may also prevent e-cigarette use onset.38 Despite these efforts, additional work is needed to explore potential pathways linking the association between parental perception of e-cigarette harm and its impact on adolescent e-cigarette use outside of use intentions. For example, parents who perceive that e-cigarettes are harmful may engage in increased parental monitoring to ensure that their child is not engaging in e-cigarette use. Similarly, parents who use e-cigarettes may limit their own use if they believe that these products may be detrimental to their health, which may ultimately reduce the use of e-cigarettes among their children. Additional work is needed to identify specific treatment targets to inform existing programming.
Limitations
The sample was comprised of high school freshmen and sophomores. Thus, findings may not generalize to older adolescents where substance use is more normative and a developmental period when parents have a weaker influence. Similarly, future work should examine whether findings are consistent among middle school youth as parents are likely to have a stronger impact on during this developmental period where e-cigarette use is starting to gain popularity. Our sample was comprised largely of adolescents identifying as Latinx/Hispanic. Prior work indicates that Latinx/Hispanic youth may be at increased risk for using e-cigarettes,39 yet this demographic group is also more strongly influenced by positive parenting practices targeting youth substance use.40 Future studies should replicate this work with a more diverse sample. Only adolescent-reports of perceived peer norms were assessed. Although parent-report of attitudes were assessed, actual conversations were not assessed. Thus, parents could have held these beliefs without conveying them to their children. Lastly, the sample size was relatively small and prospective effects represent preliminary data. Future work should attempt to replicate these findings in a larger sample.
Conclusion
Rates of adolescent e-cigarette use have reached epidemic proportions. Parents can play an important role in shaping adolescent e-cigarette use behavior. Thus, increasing parental engagement in prevention programming through psychoeducation, as well as encouraging parents to have conversations with adolescents about e-cigarette use could help mitigate this public health crisis.
Implications and Contributions.
Findings indicate that parental electronic (e-)cigarette attitudes have a stronger impact on minimizing adolescent intentions to initiate e-cigarette use, and in turn, actual use than peer norms. Involving parents in prevention programming, especially as it relates to increasing effective communication with youth on e-cigarette use harms, could have utility.
Acknowledgements:
This research was supported by the National Institutes of Health [grant numbers U54 MD012393, Subproject ID:5378; K08 AA022390; T32 DA043449]. The contents are solely the responsibility of the authors and do not necessarily represent the views of the funder. We thank the families participating in the ACE Project, the ACE Program Coordinator, Nasreen Hidmi, and the ACE Project staff. Preliminary analyses were accepted as an oral presentation at the Society for Research on Adolescence’s Biennial Conference in March, 2020. All individuals who have contributed significantly to this work are listed.
Abbreviations:
- e-cigarettes
Electronic cigarettes
- MTF
Monitoring the Future
- SLT
Social Learning Theory
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of Interest: None
References
- 1.Office of the Surgeon General. Surgeon General’s Advisory on E-cigarette Use Among Youth. 2018. [Google Scholar]
- 2.Johnston LD, Miech RA, O’Malley PM, Bachman JG, Schulenberg JE, Patrick ME. Monitoring the Future national survey results on drug use, 1975–2019: Overview, key findings on adolescent drug use. Ann Arbor, MI: Institute for Social Research, The University of Michigan.; 2020. [Google Scholar]
- 3.Squeglia LM, Gray KM. Alcohol and Drug Use and the Developing Brain. Curr Psychiatry Rep. 2016;18(5):46. DOI: 10.1007/s11920-016-0689-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Treur JL, Willemsen G, Bartels M, et al. Smoking During Adolescence as a Risk Factor for Attention Problems. Biol Psychiatry. 2015;78(9):656–663. DOI: 10.1016/j.biopsych.2014.06.019 [DOI] [PubMed] [Google Scholar]
- 5.Moylan S, Jacka FN, Pasco JA, Berk M. Cigarette smoking, nicotine dependence and anxiety disorders: a systematic review of population-based, epidemiological studies. BMC Medicine. 2012;10(1):123. DOI: 10.1186/1741-7015-10-123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lin F, Han X, Wang Y, et al. Sex-specific effects of cigarette smoking on caudate and amygdala volume and resting-state functional connectivity. Brain Imaging and Behav. 2020. DOI: 10.1007/s11682-019-00227-z [DOI] [PubMed] [Google Scholar]
- 7.Soneji S, Barrington-Trimis JL, Wills TA, et al. Association Between Initial Use of e-Cigarettes and Subsequent Cigarette Smoking Among Adolescents and Young Adults: A Systematic Review and Meta-analysis. JAMA Pediatr. 2017;171(8):788–797. DOI: 10.1001/jamapediatrics.2017.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yan XS, D’Ruiz C. Effects of using electronic cigarettes on nicotine delivery and cardiovascular function in comparison with regular cigarettes. Regul Toxicol Pharmacol. 2015;71(1):24–34. DOI: 10.1016/j.yrtph.2014.11.004 [DOI] [PubMed] [Google Scholar]
- 9.Cho JH, Paik SY. Association between Electronic Cigarette Use and Asthma among High School Students in South Korea. PLOS ONE. 2016;11(3):e0151022. DOI: 10.1371/journal.pone.0151022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hwang JH, Lyes M, Sladewski K, et al. Electronic cigarette inhalation alters innate immunity and airway cytokines while increasing the virulence of colonizing bacteria. J Mol Med. 2016;94(6):667–679. DOI: 10.1007/s00109-016-1378-3 [DOI] [PubMed] [Google Scholar]
- 11.Bandura A. Social Learning Theory. Englewood Cliffs, NJ: Prentice-Hill; 1977. [Google Scholar]
- 12.Leung RK, Toumbourou JW, Hemphill SA. The effect of peer influence and selection processes on adolescent alcohol use: a systematic review of longitudinal studies. Health Psychol Rev. 2014;8(4):426–457. DOI: 10.1080/17437199.2011.587961 [DOI] [PubMed] [Google Scholar]
- 13.Trucco EM. A review of psychosocial factors linked to adolescent substance use. Pharmacol Biochem Behav. 2020;196:172969. DOI: 10.1016/j.pbb.2020.172969 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bauman KE, Ennett ST. On the importance of peer influence for adolescent drug use: Commonly neglected considerations. Addiction. 1996;91(2):185–198. 10.1046/j.1360-0443.1996.9121852.x [DOI] [PubMed] [Google Scholar]
- 15.Cleveland MJ, Feinberg ME, Jones DE. Predicting alcohol use across adolescence: relative strength of individual, family, peer, and contextual risk and protective factors. Psychol Addict Behav. 2012;26(4):703–713. DOI: 10.1037/a0027583 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wood MD, Read JP, Mitchell RE, Brand NH. Do Parents Still Matter? Parent and Peer Influences on Alcohol Involvement Among Recent High School Graduates. Psychol Addict Behav. 2004;18(1):19–30. DOI: 10.1037/a0027583 [DOI] [PubMed] [Google Scholar]
- 17.Fadus MC, Smith TT, Squeglia LM. The rise of e-cigarettes, pod mod devices, and JUUL among youth: Factors influencing use, health implications, and downstream effects. Drug Alcohol Depend. 2019;201:85–93. DOI: 10.1016/j.drugalcdep.2019.04.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pentz MA, Shin H, Riggs N, Unger JB, Collison KL, Chou C-P. Parent, peer, and executive function relationships to early adolescent e-cigarette use: A substance use pathway? Addict Behav. 2015;42:73–78. DOI: 10.1016/j.addbeh.2014.10.040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Fite PJ, Cushing CC, Poquiz J, Frazer AL. Family influences on the use of e-cigarettes. J Subst Use. 2018;23(4):396–401. DOI: 10.1080/14659891.2018.1436601 [DOI] [Google Scholar]
- 20.Castellanos-Ryan N, O’Leary-Barrett M, Sully L, Conrod P. Sensitivity and Specificity of a Brief Personality Screening Instrument in Predicting Future Substance Use, Emotional, and Behavioral Problems: 18-Month Predictive Validity of the Substance Use Risk Profile Scale. Alcohol Clin Exp Res. 2013;37(s1):E281–E290. DOI: 10.1111/j.1530-0277.2012.01931.x. [DOI] [PubMed] [Google Scholar]
- 21.Mayhew KP, Flay BR, Mott JA. Stages in the development of adolescent smoking. Drug Alcohol Depend. 2000;59:61–81. DOI: 10.1016/s0376-8716(99)00165-9 [DOI] [PubMed] [Google Scholar]
- 22.Trucco EM, Colder CR, Wieczorek WF. Vulnerability to peer influence: A moderated mediation study of early adolescent alcohol use initiation. Addict Behav. 2011;36(7):729–736. DOI: 10.1016/j.addbeh.2011.02.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Harris PA, Taylor R, Minor BL, et al. The REDCap consortium: Building an international community of software platform partners. J Biomed Inform. 2019;95. DOI: 10.1016/j.jbi.2019.103208 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Diez SL, Cristello JV, Dillon FR, De La Rosa M, Trucco EM. Validation of the electronic cigarette attitudes survey (ECAS) for youth. Addict Behav. 2019;91:216–221. DOI: 10.1016/j.addbeh.2018.11.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Adkison SE, O’Connor RJ, Bansal-Travers M, et al. Electronic nicotine delivery systems: international tobacco control four-country survey. Am. J. Prev. Med 2013;44(3):207–215. DOI: 10.1016/j.amepre.2012.10.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.U.S. Department of Health and Human Services. Population Assessment of Tobacco and Health (PATH) Study Wave 1 youth/parent Restricted Use File: Annotated Instruments. . Ann Arbor, MI: Inter-University Consortium for Political and Social Research; 2016. [Google Scholar]
- 27.SAS Institute (Version 9.4). Cary, NC, USA2002–2012. [Google Scholar]
- 28.Muthén LK, Muthén BO. Mplus user’s guide (7th ed). Los Angeles, CA: Muthén & Muthén; 1998–2017. [Google Scholar]
- 29.Kraemer HC, Kiernan M, Essex M, Kupfer DJ. How and why defining moderators and mediators differ between the Baron and Kenny and MacArthur approaches. Health Psychol. 2008;27(2 Suppl):S101–S108. DOI: 10.1037/0278-6133.27.2(Suppl.).S101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Preacher KJ, Hayes AF. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behav Res Methods. 2008;40:879–891. DOI: 10.3758/BRM.40.3.879 [DOI] [PubMed] [Google Scholar]
- 31.Noland M, Ickes MJ, Rayens MK, Butler K, Wiggins AT, Hahn EJ. Social influences on use of cigarettes, e-cigarettes, and hookah by college students. J Am Coll Health. 2016;64(4):319–328. DOI: 10.1080/07448481.2016.1138478 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Romijnders K, van Osch L, de Vries H, Talhout R. Perceptions and Reasons Regarding E-Cigarette Use among Users and Non-Users: A Narrative Literature Review. Int J Environ Res Public Health. 2018;15(6):1190. DOI: 10.3390/ijerph15061190 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Patel M, Czaplicki L, Perks SN, et al. Parents’ Awareness and Perceptions of JUUL and Other E-Cigarettes. Am J Prev Medicine. 2019;57(5):695–699. DOI: 10.1016/j.amepre.2019.06.012 [DOI] [PubMed] [Google Scholar]
- 34.Cohall AT, Cohall R, Dye B, Dini S, Vaughan RD. Parents of Urban Adolescents in Harlem, New York, and the Internet: A Cross-sectional Survey on Preferred Resources for Health Information. J Med Internet Res. 2004;6(4):e43. DOI: 10.2196/jmir.6.4.e43 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Pepper JK, McRee A-L, Gilkey MB. Healthcare Providers’ Beliefs and Attitudes About Electronic Cigarettes and Preventive Counseling for Adolescent Patients. J Adolescent Health. 2014;54(6):678–683. DOI: 10.1016/j.jadohealth.2013.10.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Gaiha SM, Duemler A, Silverwood L, Razo A, Halpern-Felsher B, Walley SC. School-based e-cigarette education in Alabama: Impact on knowledge of e-cigarettes, perceptions and intent to try. Addict Behav. 2021;112:106519. 10.1016/j.addbeh.2020.106519 [DOI] [PubMed] [Google Scholar]
- 37.California Department of Public Health. Flavors Hook Kids Campaign Retrieved from: https://www.cdph.ca.gov/Programs/CCDPHP/DCDIC/CTCB/Pages/FlavorsHookKidsCampaign.aspx 2020.
- 38.Carver H, Elliott L, Kennedy C, Hanley J. Parent-child connectedness and communication in relation to alcohol, tobacco and drug use in adolescence: An integrative review of the literature. Drugs (Abingdon Engl) 2017;24(2):119–133. DOI: 10.1080/09687637.2016.1221060 [DOI] [Google Scholar]
- 39.Lanza ST, Russell MA, Braymiller JL. Emergence of electronic cigarette use in US adolescents and the link to traditional cigarette use. Addict Behav. 2017;67:38–43. DOI: 10.1016/j.addbeh.2016.12.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Su J, Supple AJ. Parental, peer, school, and neighborhood influences on adolescent substance use: direct and indirect effects and ethnic variations. J Ethn Subst Abuse. 2014;13(3):227–246. DOI: 10.1080/15332640.2013.847393 [DOI] [PubMed] [Google Scholar]


