Abstract
The XEN Gel Stent offers a unique Ab-interno approach for managing glaucoma and has shown a favorable risk profile relative to traditional trabeculectomy. XEN implantation has almost exclusively been reported in patients with open angle glaucoma and data in patients with angle closure glaucoma is limited. We report a postoperative complication of the XEN Gel Stent in a patient with primary angle closure glaucoma. An 86-year-old man with primary angle closure glaucoma underwent combined phacoemulsification and XEN implantation. After approximately two months, intraocular pressure was elevated and the stent was occluded by iris pigmentary deposits, traversing from the proximal to the distal conjunctival ends of the stent. Using an Ab-interno approach, the implant was successfully explanted, and the patient’s intraocular pressure was notably lowered.
Keywords: XEN Gel Stent, minimally invasive glaucoma surgery, complications, stent dislocation, antimetabolites, antifibrotics
Introduction
Minimally invasive glaucoma surgery is an emerging treatment option for glaucoma given its improved safety profile relative to traditional glaucoma drainage surgery [1]. The XEN Gel Stent (Allergan Inc., Irvine, CA) is the first Ab-interno MIGS device that targets subconjunctival outflow while sparing the conjunctiva. Implantation is frequently combined with phacoemulsification and anti-fibrinolytic injection. Recent studies have shown a favorable risk profile and shorter surgical time of the XEN Gel Stent relative to traditional trabeculectomy [2]. Nevertheless, XEN implantation has largely been exploited in open angle glaucoma and postoperative complications have almost exclusively been reported in patients with open angle glaucoma. More recently, there has been rising interest in the utility of the XEN Gel Stent in angle closure glaucoma. Data on stent complications and management in angle closure glaucoma are limited. We present a postoperative complication involving iris pigmentary occlusion of the XEN Gel Stent in a patient with primary angle closure glaucoma and describe an Ab-interno approach to management.
Case description
The current study was exempted by the University of Maryland ethics committee as no personally identifiable patient information was used. Informed consent was acquired by the patient for publishing the content of this study. Our patient was an 86-year-old man suffering from chronic, severe stage primary angle closure glaucoma of both eyes. Past surgical history included laser peripheral iridotomy of both eyes and phacoemulsification of the left eye. On ophthalmologic examination, best corrected visual acuity measured 20/30 for both eyes. Slit lamp biomicroscopy revealed a dense nuclear sclerotic cataract of the right eye. Fundus examination showed optic disc cupping of 0.95 for the right eye and 0.99 for the left eye. Glaucoma medications included Bimatoprost 0.03% administered to both eyes nightly and Brinzolamide-Brimonidine 1-0.2% administered to both eyes three times daily. Intraocular pressure of the right eye remained elevated and surgical management was performed with combined phacoemulsification and XEN 45 Gel Stent implantation with mitomycin C (MMC) 0.4 mg/ml. At the time of stent implantation following phacoemulsification, the angle was confirmed to be open in the operating room under a gonioprism.
The stent was properly positioned in the immediate postoperative period and on follow up examination one-week after surgery. By six weeks, however, slit lamp biomicroscopy revealed obstruction of the stent lumen by the iris (Figure 1) along with iris pigment deposits traversing to the distal conjunctival end of the stent within the bleb (Figure 2). The intraocular pressure had notably increased to 24 mm Hg. The patient was restarted on medical therapy with intraocular pressure lowering medication and scheduled for surgical revision of the stent.
Figure 1.

Depicts curling of the stent against iris in the anterior segment (A) followed by iris pigmentary occlusion at the proximal end of the stent (B).
Figure 2.
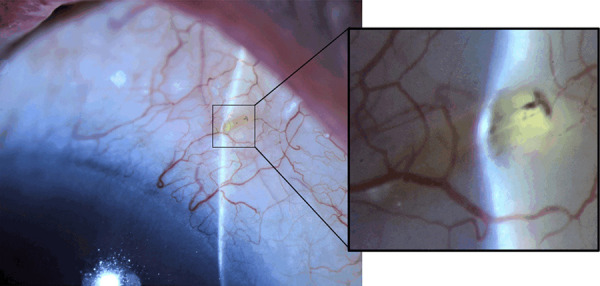
Illustrates iris pigmentary deposits traversed to the conjunctival end of the stent, occluding the distal internal ostium (magnified view).
Intraoperatively, the XEN Gel Stent was measured to be approximately 2.5 mm behind the limbus and positioned 1.5 mm within the anterior chamber. An Ab-externo approach was initially pursued repositioning the implant from the sclera, however, this resulted in stent decapitation. Following this failed attempt, an Ab-interno approach was subsequently pursued. Using a microforcep, the stent was successfully extracted from the anterior chamber. Remarkably, intraocular pressure was lowered to 10 mm Hg and remained adequately controlled off of medical therapy at 12 mm Hg on follow up one month after stent explantation. Aside from residual atrophy of the iris at the site of stent removal, the patient continued to have a low laying bleb that remained functionally intact without complications or changes in vision.
Discussion
We report a postoperative complication of the XEN Gel Stent in a patient with primary angle closure glaucoma. Implantation was complicated by iris pigmentary occlusion and managed by stent explantation using an Ab-interno approach.
Postoperative complications of XEN migration have been previously reported, albeit predominantly in open angle angle glaucoma (Table 1). In a patient with pseudoexfoliative glaucoma, Lapira et al. reported XEN stent extrusion and breakage leading to endophthalmitis three months after surgery [2]. Fea et al. described a case of XEN exposure two weeks after surgery in a primary open angle glaucoma patient having poor structural integrity of the conjunctiva [3]. Olate-Pérez and colleagues documented a case of stent exposure in a primary open angle glaucoma patient presenting with conjunctival perforation about two years after surgery [4]. In contradistinction to previous studies, stent migration in our case involved iris obstruction followed by pigmentary occlusion, despite proper stent implantation and positioning immediately postoperatively.
Table 1.
Lists the previously reported postoperative complications of stent migration following XEN implantation in patients with open angle glaucoma
| Study | Disease | Postoperative Complication |
|---|---|---|
| Fea et al. | Primary open angle glaucoma | Stent exposure |
| Olate-Pérez et al. | Primary open angle glaucoma | Stent exposure and conjunctival perforation |
| Lapira et al. | Pseudoexfoliative glaucoma | Stent extrusion and breakage |
| Karri et al. | Primary open angle glaucoma | Endophthalmitis |
| Salinas et al. | Pseudoexfoliative glaucoma | Leaking bleb |
| Santamaría-Álvarez et al. | Primary open angle glaucoma | Stent exposure and conjunctival perforation |
XEN Gel Stent insertion is commonly performed in combination with subconjunctival injection of antimetabolites including MMC. By reducing subconjunctival healing and delaying scarring at the filtration site, antimetabolites have been shown to enhance the success rate of surgical outcomes [5]. Nevertheless, antiproliferative medication has also been shown to cause thinning of the overlying conjunctiva and sclera, which may increase the probability of stent mobility. The combination of these factors has been suggested to increase the risk of XEN implant extrusion and may have similarly contributed to stent dislocation in our patient [2]. It should also be mentioned that stent migration in previous cases have predominantly involved corneal complications, whereas stent migration in our case was found curled against the iris without corneal touch.
The current case also differs from previous reports with respect to our patient’s surgical outcome and management following stent revision. Fea et al. described management of stent exposure by amniotic membrane suture with autologous conjunctival transplantation [3]. Salinas et al. reported a persistent bleb leak, which was managed by removal of the original stent and insertion of a new stent using the same incision port site [6]. Olate-Pérez et al. also attempted implant replacement and the stent similarly broke on two attempts when attempting removal at the distal conjunctival end. Since the stent was ultimately unable to be removed, the stent was cut to the scleral level and the conjunctiva subsequently sutured [4]. In our case, the original stent similarly broke upon initial repositioning performed at the conjunctival end. Notably, however, the implant was successfully removed Ab-interno from the anterior chamber.
The flexibility of the XEN Gel Stent has been shown to depend on its hydration status [7]. Composed of porcine gelatin cross-linked with glutaraldehyde, the dehydrated stent is a rigid tube that becomes soft and flexible upon hydration. Once this flexibility is acquired, the implant conforms to the tissue, which minimizes potential migration and erosion [8]. Previous studies have suggested that cessation of all topical therapy including steroids and glaucoma medications accelerates drying and renders the stent brittle and prone to breakage [7]. Notably, our patient had not been completely tapered off of topical medication, yet the stent dislocated after one month and then broke intraoperatively about two months after revision surgery. These findings suggest that the XEN Gel Stent may be more susceptible to drying than previously suspected. This loss of flexibility associated with dehydration may have contributed to stent dislocation in our patient’s postoperative course.
The XEN Gel Stent creates a permanent channel through the sclera allowing aqueous humor to flow from the anterior chamber to the subconjunctival space posteriorly. Once in place, this outflow is regulated by the physics of the internal stent lumen [3]. To our surprise, no additional interventions were necessary for managing our patient’s glaucoma following stent explantation. In particular, our patient’s intraocular pressure was lowered to 10 mm Hg immediately after explantation and remained adequately controlled off of medical therapy one month after surgery. Given the antifibrotic properties of MMC, we postulate that the scleral tunnel at the stent insertion site may have likely maintained aqueous flow between the anterior chamber and subconjunctival space, enabling continued intraocular pressure lowering. Given the antifibrotic properties of MMC, we postulate that the scleral tunnel at the stent insertion site may have likely maintained aqueous flow between the anterior chamber and subconjunctival space, enabling continued pressure control post-explantation. Previous cases of stent migration have occurred concurrently with bleb-related complications including infection and leakage [9]. In our case, however, the filtering bleb remained functionally intact without complications, and may have further allowed for continued postoperative pressure control.
In conclusion, we report a postoperative complication of the XEN Gel Stent in primary angle closure glaucoma and management using an Ab-interno approach. Several practical implications can be deduced from this case. XEN implantation performed in combination with phacoemulsification may adequately lower intraocular pressure in primary angle closure glaucoma. In addition, careful examination of the stent at the scleral and conjunctival regions may be indicated early on, especially if antimetabolites have been used. Given stent migration in the setting of MMC, our case also suggests the need for additional studies to assess the effects of antifibrotic agents on stent fixation and to explore the hydrodynamics of stent displacement in the anterior chamber.
Disclosure of conflict of interest
None.
References
- 1.Lewis RA. Ab interno approach to the subconjunctival space using a collagen glaucoma stent. J Cataract Refract Surg. 2014;40:1301–1306. doi: 10.1016/j.jcrs.2014.01.032. [DOI] [PubMed] [Google Scholar]
- 2.Lapira M, Cronbach N, Shaikh A. Extrusion and breakage of XEN Gel Stent resulting in endophthalmitis. J Glaucoma. 2018;27:934–935. doi: 10.1097/IJG.0000000000001058. [DOI] [PubMed] [Google Scholar]
- 3.Fea A, Cannizzo PM, Consolandi G, Lavia CA, Pignata G, Grignolo FM. Managing drawbacks in unconventional successful glaucoma surgery: a case report of stent exposure. Case Rep Ophthalmol Med. 2015;2015:847439. doi: 10.1155/2015/847439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Olate-Pérez Á, Pérez-Torregrosa VT, Gargallo-Benedicto A, Escudero-Igualada R, Cerdà-Ibáñez M, Barreiro-Rego A, Duch-Samper A. Management of conjunctival perforation and late seidel after XEN surgery. Arch Soc Esp Oftalmol. 2018;93:93–96. doi: 10.1016/j.oftal.2017.10.002. [DOI] [PubMed] [Google Scholar]
- 5.Karri B, Gupta C, Mathews D. Endophthalmitis following XEN stent exposure. J Glaucoma. 2018;27:931–933. doi: 10.1097/IJG.0000000000001012. [DOI] [PubMed] [Google Scholar]
- 6.Salinas L, Chaudhary A, Guidotti J, Mermoud A, Mansouri K. Revision of leaking bleb with XEN Gel Stent replacement. J Glaucoma. 2018;2:e11–e13. doi: 10.1097/IJG.0000000000000811. [DOI] [PubMed] [Google Scholar]
- 7.Santamaría-Álvarez JF, Lillo-Sopena J, Sanz-Moreno S, Caminal-Mitjana JM. Management of conjunctival perforation and XEN Gel Stent exposure by stent repositioning through the anterior chamber. J Glaucoma. 2019;28:e24–e26. doi: 10.1097/IJG.0000000000001109. [DOI] [PubMed] [Google Scholar]
- 8.Reznik A, Varma R. Ab-Interno subconjunctival glaucoma implant for advanced open-angle glaucoma. In: Aref A, Varma R, editors. Advanced Glaucoma Surgery. Springer; 2016. pp. 51–56. [Google Scholar]
- 9.Tan SZ, Walkden A, Au L. One-year result of XEN45 implant for glaucoma: efficacy, safety, and postoperative management. Eye (Lond) 2018;32:324–332. doi: 10.1038/eye.2017.162. [DOI] [PMC free article] [PubMed] [Google Scholar]


