Abstract
Tissue-resident stem cells are surrounded by a microenvironment known as ‘stem cell niche’ which is specific for each stem cell type. This niche comprises of cell-intrinsic and -extrinsic factors like biochemical and biophysical signals, which regulate stem cell characteristics and differentiation. Biochemical signals have been thoroughly studied however, the effect of biophysical signals on stem cell regulation is yet to be completely understood. Biomaterials have aided in addressing this issue since they can provide a defined and tuneable microenvironment resembling in vivo conditions. We review various biomaterials used in many studies which have shown a connection between biomaterial-generated mechanical signals and alteration in stem cell behaviour. Researchers probed to understand the mechanism of mechanotransduction and reported that the signals from the extracellular matrix regulate a transcription factor yes-associated protein (YAP)/transcriptional coactivator with PDZ-binding motif (TAZ), which is a downstream-regulator of the Hippo pathway and it transduces the mechanical signals inside the nucleus. We highlight the role of the YAP/TAZ as mechanotransducers in stem cell self-renewal and differentiation in response to substrate stiffness, also the possibility of mechanobiology as the emerging field of regenerative medicines and three-dimensional tissue printing.
Keywords: Mechanobiology, Human pluripotent stem cells, YAP/TAZ, Biomaterials
Introduction
Stem cells are unique cells that can self-renew and differentiate into specialized cells. Stem cell research has opened a new field of regenerative medicine, it has modernized the fields of drug discovery and our understanding of the physiological processes associated with disease or injury [1, 2]. Even though adult human stem cells have been used in clinical settings, their use is impeded because of their limited expansion capabilities, differentiation potential, and availability [3–5]. Human pluripotent stem cells (hPSCs) on the other hand exhibit unlimited expansion potential and unique property to differentiate into three germ layer cells, which makes them an ideal cell source for basic and clinical research [6, 7]. The microenvironment surrounding the stem cells, also known as ‘niche’, maintains a balance between self-renewal and differentiation and is specific for each type of stem cell population. It is mainly composed of tissue-specific extracellular matrix (ECM) proteins, other cells, and soluble factors such as Wingless-Type MMTV integration site family member (WNT), bone morphogenetic proteins (BMPs), ACTIVIN/NODAL, fibroblast growth factor (FGF) among others, all of which regulate cellular functions [8–10].
Signalling pathways originating from soluble factors are well known in regulating stem cell proliferation and differentiation. A number of studies have demonstrated that the physical properties of ECM and the mechanical forces generated from the surrounding niche also play an integral part in defining the stem cell behaviour, inducing specific differentiation pathways. The mechanical forces such as stress, tension, pressure, and stretch can be generated internally or externally in response to fluid flow, substrate stiffness, gas partial pressures or from adjacent cells [11, 12]. The mechanism by which the mechanical signals originating from the ECM are transduced into biological signals is collectively known as mechanotransduction and has been of great interest to the researchers. The knowledge gained so far has been invaluable in understanding metastatic cancers, neuronal regeneration, wound healing, liver regeneration, bone repair, and several other cellular phenomena. Mechanotransduction involves sensing of mechanical signals by cell surface receptors and translating it into biochemical signals by initiating a signalling cascade and eventually regulate the activity of specific genes [13]. Among all the mechanical forces, the role of ECM has been extensively researched; as the ECM plays important role in determining cellular functions [12, 14].
There has been a lot of excitement around organoids, generated from pluripotent and adult stem cells. Advances in the field of organoid research have shown the significance of cell–matrix interactions on stem cell self-renewal and differentiation [15]. For organoid formation, stem cells are embedded in complex ECM matrix which creates small, three-dimensional (3D) and self-organized tissue-like cell clusters. Organoids resembling complex tissues of intestine [16], retina [17], thyroid [18], brain [19], inner ear [20], kidney [21], liver [22], lungs [23], gastrointestinal tract [24] and blood vessels [25] have been generated. Mechanobiology behind organoid formation can shed some light upon the self-organization behaviour of stem cells in organogenesis.
Fundamental understanding of mechanical forces on stem cell behaviour can provide insights for developing an artificial niche, to support stem cells for regenerative medicine as well as it will add to our knowledge of developmental biology. In this review, we have tried to give the reader comprehensive information about the studies that have demonstrated the effect of mechanical signals mediated through hydrogels and artificial substrates on stem cell behaviour. We focus particularly on transcriptional activators yes-associated protein (YAP)/transcriptional coactivator with PDZ-binding motif (TAZ), their regulation by mechanical signals and their critical role in stem cell proliferation and differentiation.
Extracellular matrix regulated stem cell differentiation
The extracellular matrix is an essential component of the stem cell microenvironment and is indispensable for proliferation and differentiation. Apart from providing physical support to the cells, ECM regulates cell proliferation, growth, differentiation, cell shape, and migration. It is a complex assembly of proteins (mainly composed of collagen, fibronectin, elastin, laminin, and vitronectin), proteoglycans and small integrin-binding glycoproteins secreted by the cells; however, the precise composition of the matrix is different between tissues [26]. For instance, the extracellular matrix of bone is composed of highly insoluble collagen type I fibres, with traces of collagen III, V, XI, and XIII, with many intra- and inter-molecular crosslinks. Based on the composition and structure of the collagen fibres, the estimated stiffness; represented as Young’s modulus (E) expressed in Pascals (Pa); for bone is approximately 100 kPa–1GPa [27]. Whereas, the brain extracellular matrix primarily consists of lecticans, a proteoglycans family, crosslinked by tenascin (a glycoprotein), and hyaluronic acid (a glycosaminoglycan). ECM of the brain has a low content of fibrous proteins such as collagen, fibronectin, and vitronectin, making it soft compared to bone ECM with E of approximately 1 kPa [28–30]. Several experimental studies have shown that changing the biochemical composition of ECM, changes the mechanical properties (stiffness and resulting stress) which in turn regulates cell morphology, growth, differentiation, migration, and gene expression [14, 31, 32].
The substrate stiffness has been shown to change cellular morphology that leads to the reorganization of the intracellular cytoskeletal network [14, 31]. Human mesenchymal stem cells (hMSCs) develop broader and flattened morphology on the stiff substrate (E ~ 25–40 kPa) and show high expression of osteoblast-specific genes such as SRY-box transcriptional factor 9 (SOX9) and core-binding factor subunit alpha-1 (CBFA1) [33, 34], whereas, on the softer substrate (E ~ 0.1–1 kPa) hMSCs have shown upregulation of neuronal-specific protein markers such as Nestin, Tubulin beta 3 (TUBB3), Neuro Filament Light (NFL) chain, and Neural Cell Adhesion Molecule (NCAM) [33]. Mouse primary spinal cord neural cells grow and extend to neurite on the soft substrate but not on the stiff substrates [35]. On the soft substrate, cells show reduced spreading, reduced organization of actin into stress fibres and morphologically they appear round [36, 37]. Moreover, muscle stem cells maintain stemness and self-renew when cultured on soft synthetic hydrogel which mimics the elasticity of muscle (E ~ 12 kPa) [38]. Such diverse responses of stem cells to substrate stiffness represent a fundamental role of matrix in regulating cell behaviour. This shows that actin filaments regulate cell morphology in response to matrix stiffness. These biosystems help us in understanding the basic principles of tissue and organ functions.
Tools to engineer stem cell niche ex vivo and study ECM-cell interactions
In vitro studies are the ideal way to investigate the ECM-cell interactions; however, the complexity of the niche and variations in ECM composition makes it challenging and difficult. Traditional in vitro culturing methods involves the use of glass and plastic culture dishes for cell culture with E ~ 1GPa, which is very stiff compared to in vivo conditions [39]. Researchers have been using various biocompatible materials to engineer stem cell niches in vitro which mimic the stiffness of biological tissues. Natural polymers such as collagen, agarose, collagen, chitin [40], alginate, and hyaluronic acid or its conjugated hydrogel [32] are used to synthesize scaffolds due to their similarity with native ECM. However, given their limited mechanical properties focus has now shifted to synthetic hydrogels such as polyacrylamide (PA) gels [37], poly-dimethyl-siloxane (PDMS) [41], polyethylene glycol hydrogel [38], polyvinyl alcohol [42] to name a few. These synthetic hydrogels provide a wide array of stiffness range similar to physiological tissue stiffness but synthetic polymers provide limited cellular interactions due to lack of functional group present. To overcome the disadvantage of natural and synthetic polymers, semi-synthetic hydrogels such as gelatin methyl acrylate (GelMa) [43] was synthesized which combines the biocompatibility of natural hydrogel polymer and mechanical properties of synthetic biomaterials. Other than the hydrogels, artificial micropatterned and nanopatterned substrates [44], flexible micropillars [45], and electrospun nanofiber [46] have also been used as scaffolds to understand the effect of different substrate and their stiffness on cell migration, growth, and differentiation. In the following section, we have briefly discussed few natural and synthetic substrates and their effect on stem cells. Table 1 gives an overview of the various biomaterials discussed below and their influence on cell behaviour.
Table 1.
Examples of various biomaterials and their influence on mammalian cell behaviour
| Biomaterial | Stiffness | Cell type cultured | Cell response | References |
|---|---|---|---|---|
| Natural polymer | ||||
| Matrigel (3D culture) |
34 Pa–480 Pa (of 3D Matrigel) |
Primary extravillous trophoblast | Cells showed migration towards stiff region and differentiated into endometrium and placental cells | [47] |
| Vitronectin | As coating on tissue culture plate | hESCs | Cell attachment, growth and proliferation | [48] |
| Synthetic substrates | ||||
| Polyacrylamide (PA) gel substrate | ||||
| PA gel substrate coupled with type I collagen |
10 Pa (soft) 90 Pa (stiff) |
Kidney epithelial cells and 3T3 fibroblasts |
Less spreading of cells on soft substrate compared to stiff substrate Cells migrate from soft substrate towards stiff substrate |
[14, 31] |
| PA gel substrate coupled with type I collagen |
0.1–1.0 kPa (soft) 8–17 kPa (intermediate stiff) 25–40 kPa (stiff) |
hMSCs |
Differentiated into neural lineage Differentiated into myogenic lineage Differentiated into osteogenic lineage |
[33] |
| PA gel functionalized with GAG peptides |
0.7 kPa (soft) 10 kPa (stiff) |
hESCs and hiPSCs |
Better attachment, self-renewal and maintains pluripotency Cells adopted neural morphology and after addition of neuronal maintaining media developed into mature neurons |
[49] [50] |
| PA gel substrate coupled with Matrigel |
3 kPa (soft) 165 kPa (stiff) |
hESCs and hiPSCs | On soft substrate which showed stiffness similar to liver tissue, the cells differentiated into endoderm lineage whereas not on stiff substrate | [51] |
| Poly (dimethyl siloxane) (PDMS) gel substrate | ||||
| PDMS coated with polydopamine | Not determined | Bone-marrow stromal cells | Promoted differentiation into osteogenic lineage in presence of osteogenic differentiation media | [52] |
| PDMS coupled with type I collagen | 1.9 MPa–2.7 MPa (stiff) | mESCs | Cells expressed pro-osteogenic gene markers | [53] |
| PDMS printed with Fibronectin or Laminin | 5 kPa (soft) |
PC12 (rat adrenal gland derived cell line), C2C12 (mouse muscle derived cell line) |
PC12 cells differentiated into neurons on soft substrate, whereas C2C12 formed myotubes when cultured stiff substrate | [54] |
| PDMS coated with type I collagen |
3 kPa (soft) 37 kPa (stiff) |
Cardiac fibroblasts, 3T3 fibroblast, hMSCs |
Cells of all three-cell line showed increased cell spreading on stiff substrate whereas on soft substrate these cells manifest small spread area Stiff substrate promoted myofibroblast activation of cardiac fibroblast |
[55] |
| Electrospun nanofibrous substrate | ||||
|
PCL fibrous substrate PET fibrous substrate PEKK fibrous substrate PCU fibrous substrate (all plasma treated or collagen-conjugated) |
19 kPa (softest) 39 kPa (soft) 74 kPa (stiff) 193 kPa (stiffest) |
hiPSCs |
hiPSCs exhibit round 3D colony morphology on softest/soft substrate, on stiff/stiffest substrate cells spread and have flattened morphology Long-term culture on soft(est) substrate led to ectodermal differentiation, no change in cells on other substrates After adding defined growth factors, stiff substrate promoted motor neurons and soft substrate enhanced posterior foregut specification |
[46] [56] [57] |
| Semi-synthetic substrates | ||||
| Gelatin methyl acrylate (GelMa) | ||||
|
5% GelMA 10% GelMA 20% GelMA 30% GelMA |
3.08 kPa (softest) 34.9 kPa (stiffer) ~75 kPa (data not provided, estimated from the graph) 184.52 kPa (stiffest) |
PC12 (rat adrenal gland derived cell line) |
Cells show highest adhesion rate on 5% GelMa compared to 20% and 30% Cells on 10% GelMA have optimum spreading rate and longest neurite length |
[58] |
|
5% GelMa, 10% Gelma |
Not determined | Rat MSCs | Cells differentiated into osteoblast when supplemented with osteogenic media | [59] |
|
3D GELMA-PEGDA 3D PEGDA-GELMA |
30 Pa–150 Pa (soft) 1 kPa–8 kPa (stiff) |
MDA-MB-231 (breast cancer cell line) |
Soft substrate support spindle-like morphology Stiff substrate showed tumor-like spheroidal morphology, cells from these spheroids showed epithelial to mesenchymal transition and drug resistance |
[60] [61] |
| Mineralised GelMa with functionalized PEGDA | Not determined | hiPSCs | Cells underwent osteogenic differentiation devoid of biochemical signals compared with non-mineralized GelMA | [62] |
Natural polymers
Conventional protocols for growing pluripotent stem cells use mouse embryonic fibroblast cells (MEFs) as a natural substrate. MEFs is known as ‘feeder cells’ are maintained in metabolically active but non-proliferating state, thus allowing them to express soluble, membrane-bound growth factors and extracellular matrix proteins, which controls cell growth and acts as a substrate [63, 64]. In 1998, the first derivation of human embryonic stem cells (hESC) line described the importance of inactivated MEFs feeder layer for maintaining their undifferentiated state [6]. However, owing to the risk of xeno-contamination and variability, a feeder-free culture system was introduced for the maintenance and proliferation of hESCs. The feeder-free culture system uses ECM protein namely laminin [65], collagen [66], fibronectin [67], vitronectin [48, 68], Matrigel [69–71].
Collagen is the abundant ECM protein, which is widely used as a natural substrate by many researchers. Since the majority of the native ECM is composed of collagen, collagen-based biomaterials are highly biocompatible and biodegradable. Collagen alone has very low mechanical property since the mechanical properties depend on the composition of the scaffold, collagen along with co-polymer has shown to support self-renewal and differentiation of hPSCs [66] and regeneration of various tissues [72–75] in several individual studies. Fibronectin is the second most abundant ECM protein after collagen and is often used for increasing cell adhesion [67]. Several studies have shown that fibronectin supports long-term self-renewal of hPSCs [76, 77]. Fibronectin along with another polymer, for example, silk fibroin, have been used to develop a hybrid fibre, which mimics the mechanical properties of desired tissue and sustains cell growth and proliferation [78].
Matrigel is a commercially available basement membrane-like protein matrix made up of laminin, collagen IV, heparan sulphate proteoglycan and a number of growth factors in a non-defined proportion and has been reported in several studies to support the growth of undifferentiated hESCs [79, 80]. By changing the composition of the biopolymer and protein growth factors, the elastic modulus of Matrigel varies from 34 Pa–480 Pa [81, 82]. Given such low elastic moduli, Matrigel has been an ideal substrate to study cell migration in 3D culture and for the generation of many 3D organoid culture models, for example, the organoid culture of endometrium and placenta has been well established [47]. Since Matrigel is not well-defined, it may not be suitable for large-scale manufacturing for therapeutic purposes. It is generated from mouse sarcoma cells and may contain carcinogenic or xenogenic factors; thus, it is not suitable for human clinical trials [83]. Alternatively, other ECM components have been coupled with synthetic polymer matrices with specific compositions. For example, hyaluronic acid (HA), glycosaminoglycans are critical in modulating neural and hematopoietic stem cell behaviour [84, 85]. Also, HA in conjugation with tyramine can form a tuneable 3D microenvironment that modulates chondrogenesis and may impact the spatial organization of cells [32].
Synthetic polymers
Synthetic substrates are promising alternative to natural substrates. Some advantages of synthetic polymers over natural polymers are their tuneable mechanical properties, ease of synthesis, available and low cost.
Polyacrylamide gel
Polyacrylamide gel consists of a linear monomer of acrylamide and a crosslinker bisacrylamide which links the linear acrylamide monomers. PA-gels have been used as a substrate for a diverse range of cell cultures for a long time because of its ideal physical and mechanical properties. By changing the ratio of acrylamide and bisacrylamide, PA-gel substrates can be generated having elastic modulus ranging from 0.1 kPa to 100 kPa, which is equivalent to the physiological elastic moduli of soft tissues namely adipose tissue, brain tissues, endothelial tissue or lung tissue [86–88]. Polyacrylamide is inert in nature, therefore, does not support cell growth and proliferation. For it to be used as a cell culture substrate, PA-gels are first treated with UV-activated cross-linker which couples’ extracellular matrix proteins to the substrate. A number of studies have reported that chemical and physical properties of the various PA substrates have a profound effect on cell locomotion, growth, and differentiation. Early studies with kidney epithelial cells and 3T3 fibroblasts on PA substrates reported that cells on flexible substrates with E between 10 Pa (soft)–90 Pa (stiff) displayed less spreading by limiting the amount of phosphotyrosine at adhesion sites, and more cell death [14]. A similar study with 3T3 fibroblast showed that cells migrate from the soft side towards the stiff side of the PA substrate [31]. Furthermore, PA substrate of varying stiffness has been shown to direct lineage specificity for human mesenchymal stem cells (hMSCs). hMSCs cultured on soft collagen-coated PA substrate (E ~ 0.1–1 kPa), the intermediate stiff substrate (E ~ 8.0–17 kPa) and stiff substrate (E ~ 25–40 kPa) differentiate into neural, myogenic and osteogenic lineages respectively [33]. Musah et al. [49] reported that stiff PA substrate (E ~ 10 kPa), when functionalized with glycosaminoglycans (GAG) peptides, offer better hESCs and human induced pluripotent stem cells (hiPSCs) attachment, self-renewal and promotes pluripotency evident from the expression of octamer binding transcriptional factor-4 (OCT4), stage-specific embryonic antigen-4 (SSEA4) and other pluripotency specific markers. In a different study, conducted by the same research group, they reported that PA substrate (E ~ 0.7 kPa) functionalized with GAG-binding peptide selectively differentiates hESCs. After several weeks of culture on these compliant substrates and in absence of neuronal inducing factors, hPSCs adopted neuronal morphology and expressed neuronal-specific tubulin beta 3 chain (TUJ1) protein. When the media was switched to neuronal maintaining media, cells showed expressions of microtubule-associated protein 2 (MAP2), a mature neuronal marker [50]. These results indicate that substrate alone can direct differentiation of hESCs, independent of soluble factors. A similar conclusion was drawn by Chen et al. [51], where they demonstrated that hPSCs cultured on soft PA-substrate with E ~ 3 kPa expresses high levels of the anterior primitive streak and definitive-endoderm-specific gene expression such as Eomesodermin (EOMES), Brachyury (T), Forkhead box protein A2 (FOXA2), and SRY-box transcription factor 17 (SOX17) compared to hPSCs on a stiff substrate with E ~ 165 kPa and tissue culture-treated plastic plates. Another study by Maldonado et al. [56] in hiPSCs cultured on electrospun nanofibrous scaffolds reported a similar observation, which we have discussed under subsection Electrospun Nanofibrous substrate.
Poly (dimethyl siloxane) (PDMS)
PDMS is a silicon-based flexible elastomer having a wide range of applications in medicine and cosmetics, soft lithography even as anti-foaming agents and surfactants [52]. PDMS has been extensively used to understand cell behaviour in the field of mechanobiology. These rubber-like elastomers have E up to 2 MPa [89], thus making them suitable for investigating cellular responses to changing substrate stiffness. Stiff PDMS substrate (E ~ 1.9 MPa-2.7 MPa) has been reported to support proliferation and cell spreading of mouse embryonic stem cells (mESCs). These cells showed significant upregulation of pro-osteogenic transcription factors runt-related transcription factor (Runx2) and secreted phosphoprotein 1 (Spp1), compared to mESCs cultured on soft PDMS [53]. PC12 (rat adrenal pheochromocytoma cell line) differentiate into neurons and develop longer neurites on soft PDMS substrate with elastic modulus similar to brain tissue (E ~ 5 kPa) compared to the cells on stiffer PDMS substrate. The same study also showed that C2C12 (mouse skeletal muscle cell line) when cultured and differentiated on stiff PDMS substrates formed longer myotubes compared to cells cultured on a soft substrate [54].
Many a time because of high surface hydrophobicity of PDMS cell attachment to the substrate is poor. For enhanced cell adhesion and proliferation bio-inspired polydopamine-coated PDMS was used instead of protein-coated PDMS. Polydopamine-coated PDMS promoted long term bone-marrow stromal cells culture while maintaining their multipotency [52]. In regard to cell spreading, 3T3 fibroblasts, cardiac fibroblasts and MSCs showed increased spreading on stiffer PDMS substrate coated with collagen compared to soft substrate, an observation similar to the PA substrate study. Interestingly, cells cultured on soft PDMS respond to secondary crosslinking-induced stiffness, representing similar spread area to the cells on stiff PDMS [55]. These reports indicate that PDMS hydrogels influences cell adhesion and spreading, potency and differentiation. It would be interesting to see whether PDMS modified to low stiffness help maintain the pluripotency of hPSCs or direct them towards differentiation.
Electrospun nanofibrous substrate
These substrates have been around for many years now and researchers have shown keen interest in using these substrates for as biological scaffolds in tissue engineering. They provide a porous mesh of nanoscale and microscale fibrous structures which highly resembles natural ECM [90]. A notable report by Maldonado et al. (2015 and 2016) [46, 56] studied the proliferation and differentiation of hiPSCs on various synthesized electrospun nanofiber substrates exhibiting different chemical and mechanical properties. These substrates were poly(ε-caprolactone) (PCL), polyethylene terephthalate (PET), polycarbonate-urethane (PCU), and poly(etherketoneketone) (PEKK). The measured Young’s modulus of these substrates ranged from ~ 19 kPa to ~ 313 kPa. Short- and long-term culture of hiPSCs showed characteristic pluripotent colony morphology and expressed pluripotency-associated markers OCT4, homeobox protein Nanog (NANOG) and DNA (cytosine-5-)-methyltransferase 3 beta (DNMT3B) on all the substrates. However, after 12 days in culture, cells on 19 kPa substrate highly expressed ectodermal markers PAX6 and NEUROD1, whereas these makers showed minimal expression on 193 kPa substrate and no expression on tissue culture-treated plastic dish.
Electrospun fibrous substrates induce substrate-dependent changes in colony morphology and gene expressions in hiPSCs. hiPSCs, when subjected to defined growth factors of specific lineages, tend to differentiate into motor neurons on a soft substrate during early differentiation, conversely, stiff substrates promoted motor neuron specification during late stages. In contrast, hiPSCs differentiated into the mesendodermal lineage on the stiff substrate, but soft substrate enhanced further their specification into the posterior foregut [57]. These observations are different from the studies that have used hydrogels as substrates, suggesting that differentiation is not restricted to single stiffness and dynamic changes in the mechanical microenvironment may help in enhancing the differentiation efficiency of hiPSCs.
Semi-synthetic polymers
Biohybrid or semi-synthetic polymers combine the best of both the natural and synthetic polymers. A number of scaffolds with at least one natural polymer such as collagen, fibrin, laminin in well-defined proportion with synthetic polymer namely polyethylene glycol (PEG), polyglycolic acid (PGA) or polycaprolactone (PCL) have been synthesized for 2D and 3D culture of many cell lines including stem cells [91]. Recently, GelMA has emerged as an attractive candidate for mimicking native ECM conditions in vitro.
Gelatin methyl acrylate (GelMa)
GelMa is a photo-reactive hydrogel made up of gelatin and methacrylic groups. First synthesized in 2000 by Van Den Bulcke et al. [92], GelMa is an inexpensive, natural polymer synthesized from hydrolysis and denaturation of collagen which makes it suitable biomaterial for in vitro studies. GelMa has proven to provide optimal conditions for cell culture due to the presence of arginine-glycine-aspartic acid (RGD) motifs for adhesions and matrix metalloproteinase (MMP) degradation motif for cellular enzymatic degradation. Depending upon the percentage of GelMa (w/v) or the concentration of the other polymers, such as alginate or hyaluronic acid, mixed with it, stiffness of GelMa can range from 1 kPa to 200 kPa [58, 93, 94]. Owing to such a large physiological stiffness range, GelMa hydrogels have been thoroughly investigated for its physical and biochemical properties as 2-D and 3-D scaffolds in tissue engineering [95]. Notable application of GelMa 3-D scaffolds for tissue engineering had been reported for bone [96], skin [97, 98], cardiac tissue [99], endochondral bone [100], skeletal muscles [101], and vascular networks [102].
To determine whether soft GelMa substrate supports neuronal development, PC12 cells were cultured on GelMa substrates having E ~ 3 kPa–184 kPa. The cells showed maximum adhesion on softest substrate of 3 kPa compared to other stiffness, however, the longest neurite length was observed on substrate with intermediate stiffness (E ~ 34.9 kPa) [58]. The authors, however, did not show the gene expression profile of the differentiated cells. It would be interesting to know whether these substrate support neurite maturation for a long duration and generate mature as well as functional neurons. In another study, rat bone-marrow derived MSCs were cultured on 5% (soft) and 10% (stiff) GelMa substrates and when they were supplemented with osteogenic media, MSCs differentiated into osteoblasts. The stiffness of these two GelMa substrates was not determined; hence which stiffness range of GelMa supports osteoblast differentiation still remains a question [59].
For 3D cell culture, a blend of GelMa and polyethylene (glycerol) diacrylate (PEGDA) was developed to study cell metastasis using cancer cells. By increasing the concentration of PEGDA, the elastic moduli of non-degradable 3D PEGDA-GELMA scaffold was between E ~ 1 kPa to 8 kPa whereas soft degradable 3D scaffolds were obtained by increasing GelMa concentration (E ~ 30 Pa to 150 Pa). Encapsulated MDA-MB-231 breast cancer cells in these substrates showed tumor-like spheroidal morphology in stiff PEGDA-GELMA substrate, while they showed spindle-like morphology in soft GELMA-PEGDA substrate. Invasion chick aorta arch assay showed that the softer GELMA-PEGDA substrate supports the invasion of both MDA-MB-231 and endothelial cells, along with sprouting of endothelial cells from chick aortic arches [60]. The gene expression profile of the spheroids derived cell from stiff PEGDA-GELMA showed epithelial-mediated transition (EMT) behaviour and drug resistance [61]. GelMa substrate mineralized with calcium and phosphate minerals induce osteogenic differentiation of hiPSCs in 2D and 3D, evident from gene expression study and immunofluorescent staining for osteogenic specific transcription factors RUNX2, OCN and SPP1. The hiPSCs were cultured devoid of growth factors and the differentiation was achieved through substrate-based biomechanical cues. However, non-mineralized GelMa or gelatin-coated dishes functionalized with PEGDA does not support the growth and differentiation of hiPSCs [62]. Though GelMa has shown great promise in tissue engineering, questions such as—whether GelMa directs differentiation into lineages other than osteogenic differentiation, is GelMa a better substrate than normal culture dishes or other substrates for differentiation, how stem cells differentiated on GelMa functionally differ from differentiated cells generated via the normal stiff culturing conditions, need to be addressed before GelMa could be routinely used for basic and possibly for translational purposes.
Mechanobiology: Intracellular sensory system
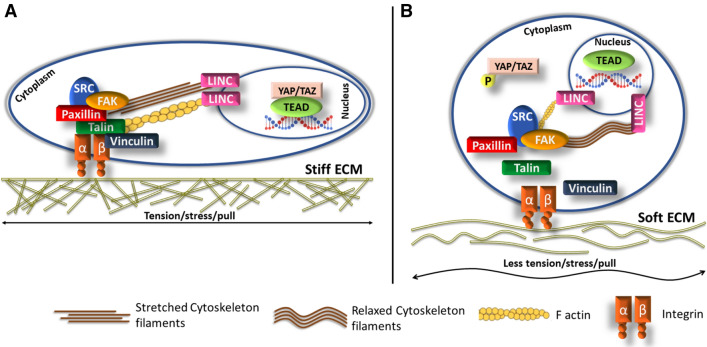
We have described the effect of various natural and synthetic biomaterials on cell proliferation and differentiation, this implies that cells have a mechanism to sense substrate stiffness and make modifications to generate specific proteins. In order to generate supportive biomaterial, it is essential to understand what changes occur to mechanosensing machinery inside the cells. Cell–matrix interactions are mediated by cell surface receptor integrins, focal adhesion kinases (FAK), and cytoskeletal filaments that connects the extracellular matrix to the intracellular environment. When cells come in contact with mechanical signals from the extracellular region, a multiprotein complex is formed near the cell surface receptor, known as focal adhesions (FA). FA comprises of talin, vinculin, paxillin, alpha-actinin, p-130cas, FAK, SRC, and FAs act as a mediator between integrins and actin filaments (Fig. 1). Other than FA, Rho family small GTPases, its downstream effectors Rho-associated kinases (ROCK), and myosin light chain kinases also relay the mechanical signals to cytoskeletal filaments [103–107]. The cytoskeletal components mainly actin filaments, microtubules, and non-muscle myosin undergo conformational changes (stretching or relaxing, shortening or elongating) [108, 109] which affects gene-specific transcription due to cytoplasmic or nuclear localization of gene-specific transcriptional factors. For example, the formation of stress fibres causes nuclear localization of transcriptional coactivators YAP and TAZ or cytoskeletal remodeling activates and translocates beta-catenin into the nucleus [110, 111], where these two proteins interact with their respective coactivators and activate specific gene expression.
Fig. 1.
The effect of substrate stiffness on YAP/TAZ. A Stiff substrate activates focal adhesion proteins—talin and vinculin, they bind to and activate integrin, resulting in cell adhesion and spreading. Formation of integrin-talin-vinculin phosphorylates FAK which forms a complex with Src and phosphorylates paxillin, contributing in mechanosignalling and cell spreading. This entire complex creates tension on actinomycin and cytoskeletal filaments which causes stretching of LINC; nuclear envelope protein; ensuring nuclear localization of YAP/TAZ and subsequent gene expression. B On the contrary cells on soft substrate experience less tension, forming an unstable integrin-talin-vinculin complex. Loosely formed FAK-SRC complex does not form tension-dependent stretching of actinomycin, cytoskeletal filaments, and LINC, causing cytoplasmic retention of YAP/TAZ
Apart from these, other transcriptional factors which have been reported to respond to different mechanical signals are tight junction protein ZO-1 [112], tyrosine kinase c-Abl [113], myocardial-related transcriptional factor (MRTF) [114], Nuclear Factor-kappa-B (NFκB) [115], nuclear factor erythroid-2-related factor 2 (NRF2) [116], epigenetic regulator HDAC3 in both mouse and human cell lines [117]. An important point to be noted here is that, these transcriptional factors have been known to be regulated by specific signalling pathways and do not solely function as mechanotransducers. The shuttling of these transcriptional factors between cytoplasm and nucleus is gated by linker of nucleoskeleton and cytoskeleton (LINC) complex present on the nucleus envelope. The tensed actin cytoskeleton causes stretching of actin binding LINC complex component Nesprin1, resulting in stiffening of nuclear envelope and localization of transcriptional factors [118, 119]. The mechanical signal-regulated signalling pathways are complex; numerous studies have identified YAP/TAZ proteins as mechano-transmitters that respond to signals from substrate stiffness, substrate topology, surface area, cell density, cell polarity, and cell geometry. Given such a vast array of regulators, YAP/TAZ has garnered the attention of many research groups. Here, we review the data highlighting the functions of YAP/TAZ as transcriptional co-activators and as mechanosensors.
Yes-associated protein (YAP) and transcriptional coactivator with PDZ-binding motif (TAZ)
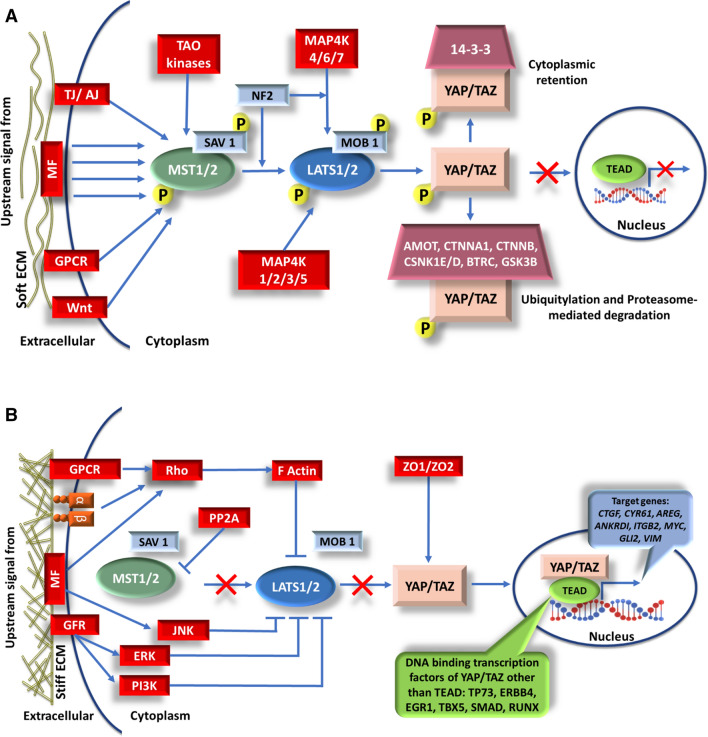
Yes-associated protein (YAP) was first discovered in Drosophila and was termed Yorkie due to its association with Src family kinase Yes [120] and transcriptional co-activator of PTZ binding motif (TAZ) was first identified as 14-3-3 binding protein as a paralog to YAP [121]. These transcriptional co-activators share 46% sequence homology and display a similar domain organization, except for a proline right domain, one WW domain and SH3 binding region [122]. YAP and TAZ are primary effectors of the Hippo pathway however; these coactivators also interact with TGF β, WNT, BMP, ERK and FGF signalling pathways [123, 124]. Figure 2 shows the core pathway consists of a cascade of kinase activations in which the upstream signals phosphorylates mammalian Ste20-like kinases 1/2 (MST 1/2; Drosophila homologous Hippo [Hpo]) which phosphorylates and binds to SAV1 (Drosophila homologous Salvador [Sav]). This complex then phosphorylates and activates large tumor suppressor kinase 1/2 (LATS1/2; Drosophila homologous Warts [Wts]) and monopolar spindle-one-binder proteins (MOB1; Drosophila homologous Mats) complex. LATS1/2 in turn activates YAP/TAZ by phosphorylating at specific serine residues, thereby causing it to localize in the cytoplasm. Besides LATS1/2 several other proteins—Angiomotin (AMOT), 14-3-3, SMADs, casein kinase 1 isoform epsilon and delta (CSNK1E/D), glycogen synthase kinase 3 beta (GSK3B), catenin beta (CTNNB), CAPZ and beta transducing repeat-containing protein (BTRC) also affect YAP/TAZ localization [121, 125–128] (Fig. 2A). Since YAP/TAZ does not have their own DNA binding motifs, unphosphorylated nuclear YAP/TAZ interacts with various DNA-binding transcription factors regulating targeted gene expression. The function of YAP/TAZ depends upon the upstream signal and its binding partner [129] (Fig. 2B). Their nuclear localization results in cell proliferation, differentiation, migration, epithelial-mediated transition (EMT), cancer development or suppression, and loss of contact inhibition [129–133].
Fig. 2.
The Mammalian Core Hippo Signaling pathway. A When Hippo pathway is ON, YAP and TAZ are cytoplasmic and do not bind to TEAD (DNA binding transcriptional factor). Upstream signals from various cell surface receptors such as GPCR, WNT, TAO Kinases, tight junction (TJ), adhesion junctions (AJ) or mechanical forces (soft substrate, high cell density, small surface area for adhesion etc.) initiates a cascade of phosphorylation reactions of core Hippo pathway proteins. These signals and scaffold protein SAV1 phosphorylate MST1/2. LATS1/2 is phosphorylated by MST1/2 and MAP4K, facilitated by MOB1 and NF2 (also known as Merlin), which subsequently phosphorylates YAP/TAZ at various serine residues (refer Fig. 3). After phosphorylation by LATS1/2-MOB1, YAP/TAZ either binds to 14-3-3 protein resulting in its cytoplasmic retention or binds to angiomotin (AMOT), casein kinase 1 isoform epsilon and delta (CSNK1E/D), β-transducing repeat-containing protein (BTRC), glycogen synthase kinase 3 Beta (GSK3B) or catenin beta (CTNNB) resulting in ubiquitylation and proteasomal-mediated degradation. YAP/TAZ cannot shuttle into the nucleus and bind to one of its DNA binding transcription factors such as TEAD when Hippo pathway is ON. B When Hippo pathway is OFF i.e. in absence of upstream signaling, MST1/2 and LATS1/2 are unphosphorylated and inactive. Unphosphorylated YAP/TAZ is active and is free to move into the nucleus, bind to transcriptional factors, such as TEAD, TP73, ERBB4, EGR1, TBX5, SMAD, or RUNX, and depending upon the binding partner promote specific gene expression
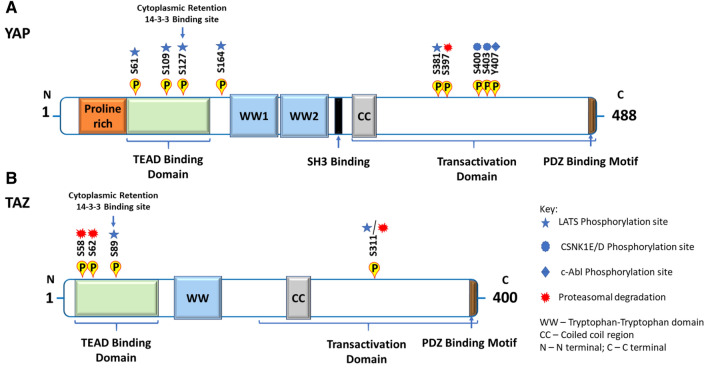
YAP and TAZ share high protein sequence similarity (Fig. 3) and thereby have similar functions. However, there are few structural differences that suggest non-overlapping functions of YAP and TAZ [134, 135]. YAP regulates TAZ cytoplasmic retention, but the exact mechanism is still not clear, although interestingly, the same cannot be said for TAZ because an increase in TAZ expression does not show any effect on YAP levels [136]. Transgenic expression of only YAP in mouse liver showed a dramatic increase in liver mass [137]. YAP and TAZ exhibit some physiological differences as well, and knockout studies have shown that YAP knockout mice embryo having normal TAZ develop severe developmental defects and subsequent embryonic lethality by embryonic day 8.5 [138]. Conversely, TAZ knockout embryos with normal YAP exhibit partial embryo lethality, where only half of the embryos survive while the other half die [139–141]. From these observations, it can be said that TAZ is unable to compensate for the loss of YAP.
Fig. 3.
Schematic representation of A YAP and B TAZ primary protein sequence: Phosphorylation sites on YAP and TAZ by LATS, CSNK1E/D, c-Abl and for proteasomal degradation are highlighted, including phosphorylation of YAP at S381 by LATS1/2 leads to SCF-βTRCP-mediated proteasomal degradation whereas phosphorylation of YAP at S58/62 causes GSK-3β mediated proteasomal degradation. Phosphorylation at Serine 127 (for YAP) and at Serine 89 (for TAZ) by LATS creates a binding site for 14-3-3 thereby retaining YAP/TAZ in the cytoplasm. YAP and TAZ both have a TEAD binding domain, WW domain, CC (coiled-coil region) domain, transactivation domain, and PDZ binding motif; with an additional proline-rich region, WW domain, and SH3 domain
The differentiation of MSCs into adipocytes, osteoblasts or myocytes has been shown to be regulated by YAP/TAZ activation [142, 143], whereas, YAP/TAZ has been associated in maintaining the pluripotent state and self-renewal in mESCs [137]. Qin et al. (2016) [144] reported that YAP overexpressing hPSCs cultured in DMEM F12 supplemented with bFGF, N2B27, ERK, GSK inhibitors, Forskolin and human LIF did not undergo differentiation as opposed to primed hESCs. Even in differentiating media these hESCs overexpressing YAP strongly expressed pluripotency markers such as OCT4, NANOG, SSEA3, SSEA4, alkaline phosphatase (AP), TRA-1-60 and TRA-1-81. The YAP overexpressing cells when cultured for more than 70 passages showed increased growth rate and dome-like colony morphology. They further proved the role of YAP in maintaining the naïve state by generating clustered regularly interspaced short palindromic repeats (CRISPR)/CRISPR associated protein 9 (Cas9)-generated YAP-/-cells. YAP knockout impairs hESCs ability to exhibit naïve-specific colony characteristics. Apart from this, YAP was shown to play a crucial role in anterior–posterior streak specification. YAP1-/- pluripotent stem cells specify into anterior–posterior streak progenitors in the presence of ACTIVIN which further differentiate into cardiac mesoderm and endoderm [145]. Other than stem cells, YAP/TAZ activation is well known in cancer cells where they function as an oncogene and play an important role in cancer initiation, progression, and metastasis [146]. Numerous knockouts, conditional knockout, deletion studies in various cancer models have revealed the potential role of YAP/TAZ in promoting tumorigeneses in skin, liver, breast and ovarian cancer. We would suggest the readers refer to other excellent reviews on the role of YAP/TAZ in cancer [147–150].
YAP and TAZ as mechanosensors in stem cells
Apart from acting as transcriptional activators, YAP/TAZ have emerged as key mechanotransducers, acting as nuclear relays in response to cell polarity, substrate stiffness, topology, surface area, and cell density [151–153]. YAP/TAZ activity as mechanosensors has been widely associated with the focal adhesion (FA) components namely integrins, talins, and FAKs. Indeed, on larger stiff substrates cells are well spread, in these conditions they exhibit high ROCK, non-muscle myosin II and F-actin levels, experience high contractile forces which activate YAP/TAZ. Conversely, cells on the soft or small substrates with reduced adhesive area display round morphology, low F-actin, low contractile forces causing cytoplasmic retention, and inactivation of YAP/TAZ [151, 154]. Additionally, the F-actin-capping and -severing proteins Cap Z, Cofilin and Gelsolin have shown to bind to YAP/TAZ thus, limiting YAP/TAZ nuclear localization in cells experiencing low mechanical stress [153]. hESCs on stiff PA-gel substrate (E ~ 10 kPa); showed high levels of nuclear YAP/TAZ, F-actin and OCT4 which is indicative of pluripotency [49]. Conversely, hESCs on soft PA-substrate (E ~ 0.7 kPa) showed more cytoplasmic YAP and differentiation into post-mitotic neurons [50]. These findings highlight that, substrate stiffness affects the formation of F-actin and further regulates YAP/TAZ activity. Interestingly, a recent study reported that by changing the stiffness of the PDMS substrate, the mesoderm differentiation kinetics of hiPSCs can be modulated and this mechanical change activates YAP during mesoderm induction [155]. This curious observation can be explored further by differentiating hiPSCs into other lineages on PDMS substrate of varying stiffness and studying the YAP/TAZ dynamics.
The nuclear translocation of YAP in response to mechanical stimuli has also been associated with the FAK activity. Computational model studies suggest that substrate rigidity affects the FAK activation levels which mediate YAP nuclear localization, and subsequent activations of downstream proteins and eventually gene regulation [119]. Among all the mechanosensing molecules, Talin directly links Integrins to Actin, thus the ECM-Integrin-Talin-Actin clutch is of particular interest in understanding mechanotransduction by matrix rigidity. Substrate stiffness above 5 kPa triggers conformational changes in Talin, it unfolds, binds to and activates vinculin, leading to an increase in focal adhesions and nuclear localization of YAP/TAZ as illustrated in Fig. 1. This role of Talin was demonstrated by culturing Talin-depleted cells on PA-gel, these cells showed normal spreading however they neither develop focal adhesions nor caused nuclear localization of YAP [153].
A common observation across current literature shows that hPSCs attach poorly on the soft substrate due to lack of binding sites on substrates, which directly affects their survival. To overcome this, a semi-interpenetrating matrix of PA gel and Matrigel was synthesized ranging from 150 to 12000 Pa in stiffness. hESCs on all the substrates maintain the expression of pluripotency markers even in small colonies. In response to the substrate stiffness, hESCs mimicked colony characteristics of epiblast, inner cell mass, and proamnion. hESCs on soft substrates with E < 450 Pa exhibit decreased nuclear YAP compared to cells on stiff substrates having E > 1000 Pa. Immunofluorescence probing of single cells grown on soft substrate showed a heterogeneous distribution of YAP in peripheral cells and nuclear localization in the colony interior, indicating a significant variation in YAP distribution within a single colony. When the substrate was switched from soft PA to glass coverslips, an increase in nuclear YAP was observed. Further analysis showed that YAP expression drastically decreased on soft substrate (E ~ 450 Pa and 150 Pa) whereas no significant changes in OCT4 expression were seen. This implies that on soft substrate, YAP expression in pluripotent stem cells is sufficient for proliferation and survival but it does not seem to play any role in maintaining pluripotency [156]. Substrate stiffness has a significant effect on cell migration, human adipose-derived stromal/stem cells, human hepatic stellate cells (HHSteC) and MSCs cultured on PA-gel substrate of stiffness spanning the in vivo physiological range, migrate towards the stiff region of the rigidity gradient substrate, a process known as durotaxis. To understand the mechanism behind migration, cells were treated with FAK inhibitor and siRNA YAP. Treated cells showed less motility compared to untreated cells indicating that the directed movement of cells from soft region towards stiff region is controlled by FAK and YAP [157–159].
To summarize, YAP/TAZ regulation is largely controlled by the integrity of the cytoskeleton mainly actin-myosin contractility [151]. Actin-severing proteins and unfolded Talin affects the YAP/TAZ nuclear localization [153, 154], while actin-capping proteins, impairment, and depletion of LINC or Nesprins, and finally stiffness of the substrates cause the cytoplasmic retention of YAP/TAZ in the cytoplasm [119, 154]. Elosegui-Artola et al. [107] have shown that by applying force to the nucleus, nuclear import of the YAP/TAZ and other proteins increases irrespective of their active or inactive state. Whether this passive transport initiates expressions of YAP/TAZ-regulated genes is yet to be shown.
Mechanobiology: future perspectives
Bone marrow transplantation or blood transfusions harbouring stem cells have been used for decades and have been reported to be very successful, however when isolated stem cells that are cultured on stiff substrates are transplanted, the results are variable. Sudden change in substrate stiffness may cause changes at gene-level leading to tumour formation or death of the injected cells. This might be the reason why many of the stem cell-based therapies have failed to show the desired effect. 3D bioprinting is a rapidly developing field, where cells are printed onto synthetic or natural biomaterials to generate tissues that closely resemble natural cell arrangement. Recently many newer biomaterials have been designed [160, 161], these biomaterials need to be stiff enough to support the growth of epithelial cells and pliable enough to support angiogenesis, to be clinically successful. Therefore, it is important that we understand the relationship between substrate stiffness and stem cells, so that cells can be cultured on substrate having similar physiological stiffness in order to achieve better results. We hope that with the knowledge about YAP/TAZ and the mechanism by which they regulate genes in response to varied substrate stiffness, would help us design functional 3D printed tissues. Most of the research work done to understand the effect of substrate stiffness on cell behaviour, has been carried out with MSCs, however not much data is available for primary tissues/cells or human pluripotent stem cells.
On a very fascinating note, researches have been focused on understanding the effect of microgravity on stem cell growth and differentiation, necessitated by the advances in space travel and challenges it poses to human physiology. Microgravity has a reversible effect on cell adhesion and microfilament rearrangements of MSCs as shown by the expression levels of vinculin, integrin, VCM1, and actin filaments [162]. Recently it has been demonstrated that the reduced gravity of the international space station (ISS) altered the functioning of neonatal and adult human cardiac progenitor cells [163]. These newer observations demonstrate that there is a lot to be uncovered about how living cells respond to external cues. Mechanobiology would be important discipline that should be studied if humans have to travel to distant planets or survive in low gravity environments of space stations.
Conclusion
Until recently, most of our understanding of molecular biology was from the cells cultured on very stiff tissue culture-treated plastic dishes. Cellular functions were defined by the signalling molecules used during culturing; however, the overarching function of mechanical signals suggests that mechanotransduction contributes to defining cellular activity. This raises profound questions such as- in the absence of signalling molecules are the external signals such as substrate stiffness or topology sufficient to direct the cellular fate of stem cells, the answers as and when are uncovered will have significant clinical impact.
Acknowledgements
We would to acknowledge Sunandan Divatia School of Science, NMIMS (deemed to-be University) and Symbiosis Centre for Stem Cell Research (SCSCR), Symbiosis International University, for providing the necessary resources and infrastructure. The work was funded by Department of Biotechnology (DBT), Govt of India, sanction order BT/PR28474/MED/31/393/2018. JKV was provided Senior Research Fellowship by Council of Scientific and Industrial Research (CSIR).
Compliance with ethical standards
Conflict of interest
The authors have no financial conflict of interest.
Ethical statement
There are no animal experiments carried out for this article.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Ranga A, Gjorevski N, Lutolf M. Drug discovery through stem cell-based organoid models. Adv Drug Deliv Rev. 2014;69:19–28. doi: 10.1016/j.addr.2014.02.006. [DOI] [PubMed] [Google Scholar]
- 2.Clevers H. Modeling development and disease with organoids. Cell. 2016;165:1586–1597. doi: 10.1016/j.cell.2016.05.082. [DOI] [PubMed] [Google Scholar]
- 3.Barkholt L, Flory E, Jekerle V, Lucas-Samuel S, Ahnert P, Bisset L, et al. Risk of tumorigenicity in mesenchymal stromal cell-based therapies bridging scientific observations and regulatory viewpoints. Cytotherapy. 2013;15:753–759. doi: 10.1016/j.jcyt.2013.03.005. [DOI] [PubMed] [Google Scholar]
- 4.Steinbeck JA, Studer L. Moving stem cells to the clinic: potential and limitations for brain repair. Neuron. 2015;86:187–206. doi: 10.1016/j.neuron.2015.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Caglayan S, Ahrens TD, Cieślar-Pobuda A, Staerk J. Modern ways of obtaining stem cells. In: Łos MJ, Hudecki A, Wiecheć E, editors. Stem cells and biomaterials for regenerative medicine. Cambridge: Academic Press; 2019. pp. 17–36. [Google Scholar]
- 6.Thomson JA, Itskovitz-Eldor J, Shapiro SS, Waknitz MA, Swiergiel JJ, Marshall VS, et al. Embryonic stem cell lines derived from human blastocysts. Science. 1998;282:1145–1147. doi: 10.1126/science.282.5391.1145. [DOI] [PubMed] [Google Scholar]
- 7.Yamanaka S. Patient-specific pluripotent stem cells become even more accessible. Cell Stem Cell. 2010;7:1–2. doi: 10.1016/j.stem.2010.06.009. [DOI] [PubMed] [Google Scholar]
- 8.Sato N, Meijer L, Skaltsounis L, Greengard P, Brivanlou AH. Maintenance of pluripotency in human and mouse embryonic stem cells through activation of Wnt signaling by a pharmacological GSK-3-specific inhibitor. Nat Med. 2004;10:55. doi: 10.1038/nm979. [DOI] [PubMed] [Google Scholar]
- 9.Zhang J, Li L. BMP signaling and stem cell regulation. Dev Biol. 2005;284:1–11. doi: 10.1016/j.ydbio.2005.05.009. [DOI] [PubMed] [Google Scholar]
- 10.Vallier L, Alexander M, Pedersen RA. Activin/Nodal and FGF pathways cooperate to maintain pluripotency of human embryonic stem cells. J Cell Sci. 2005;118:4495–4509. doi: 10.1242/jcs.02553. [DOI] [PubMed] [Google Scholar]
- 11.Kaverina I, Krylyshkina O, Beningo K, Anderson K, Wang YL, Small JV. Tensile stress stimulates microtubule outgrowth in living cells. J Cell Sci. 2002;115:2283–2291. doi: 10.1242/jcs.115.11.2283. [DOI] [PubMed] [Google Scholar]
- 12.Vining KH, Mooney DJ. Mechanical forces direct stem cell behaviour in development and regeneration. Nat Rev Mol Cell Biol. 2017;18:728–742. doi: 10.1038/nrm.2017.108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Eyckmans J, Boudou T, Yu X, Chen CS. A hitchhiker’s guide to mechanobiology. Dev Cell. 2011;21:35–47. doi: 10.1016/j.devcel.2011.06.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pelham RJ, Wang YL. Cell locomotion and focal adhesions are regulated by substrate flexibility. Proc Natl Acad Sci U S A. 1997;94:13661–13665. doi: 10.1073/pnas.94.25.13661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Huch M, Knoblich JA, Lutolf M, Martinez-Arias A. The hope and the hype of organoid research. Development. 2017;144:938–941. doi: 10.1242/dev.150201. [DOI] [PubMed] [Google Scholar]
- 16.Sato T, Vries RG, Snippert HJ, Van De Wetering M, Barker N, Stange DE, et al. Single Lgr5 stem cells build crypt–villus structures in vitro without a mesenchymal niche. Nature. 2009;459:262–265. doi: 10.1038/nature07935. [DOI] [PubMed] [Google Scholar]
- 17.Eiraku M, Takata N, Ishibashi H, Kawada M, Sakakura E, Okuda S, et al. Self-organizing optic-cup morphogenesis in three-dimensional culture. Nature. 2011;472:51–56. doi: 10.1038/nature09941. [DOI] [PubMed] [Google Scholar]
- 18.Antonica F, Kasprzyk DF, Opitz R, Iacovino M, Liao XH, Dumitrescu AM, et al. Generation of functional thyroid from embryonic stem cells. Nature. 2012;491:66–71. doi: 10.1038/nature11525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lancaster MA, Renner M, Martin CA, Wenzel D, Bicknell LS, Hurles ME, et al. Cerebral organoids model human brain development and microcephaly. Nature. 2013;501:373–379. doi: 10.1038/nature12517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Koehler KR, Mikosz AM, Molosh AI, Patel D, Hashino E. Generation of inner ear sensory epithelia from pluripotent stem cells in 3D culture. Nature. 2013;500:217–221. doi: 10.1038/nature12298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Xia Y, Nivet E, Sancho-Martinez I, Gallegos T, Suzuki K, Okamura D, et al. Directed differentiation of human pluripotent cells to ureteric bud kidney progenitor-like cells. Nat Cell Biol. 2013;15:1507–1515. doi: 10.1038/ncb2872. [DOI] [PubMed] [Google Scholar]
- 22.Huch M, Dorrell C, Boj SF, Van Es JH, Li VS, Van De Wetering M, et al. In vitro expansion of single Lgr5 + liver stem cells induced by Wnt-driven regeneration. Nature. 2013;494:247–250. doi: 10.1038/nature11826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Huang SX, Islam MN, O’Neill J, Hu Z, Yang YG, Chen YW, et al. Efficient generation of lung and airway epithelial cells from human pluripotent stem cells. Nat Biotechnol. 2014;32:84–91. doi: 10.1038/nbt.2754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Múnera JO, Wells JM. Generation of gastrointestinal organoids from human pluripotent stem cells. Organ Regen. 2017;1597:167–177. doi: 10.1007/978-1-4939-6949-4_12. [DOI] [PubMed] [Google Scholar]
- 25.Wimmer RA, Leopoldi A, Aichinger M, Kerjaschki D, Penninger JM. Generation of blood vessel organoids from human pluripotent stem cells. Nat Prot. 2019;14:3082–3100. doi: 10.1038/s41596-019-0213-z. [DOI] [PubMed] [Google Scholar]
- 26.Yue B. Biology of the extracellular matrix: an overview. J Glaucoma. 2014;23 Suppl 1:S20–S23. doi: 10.1097/IJG.0000000000000108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Cancedda R. Cartilage and bone extracellular matrix. Curr Pharma Design. 2009;15:1334–1348. doi: 10.2174/138161209787846739. [DOI] [PubMed] [Google Scholar]
- 28.Ruoslahti E. Brain extracellular matrix. Glycobiology. 1996;6:489–492. doi: 10.1093/glycob/6.5.489. [DOI] [PubMed] [Google Scholar]
- 29.Wells RG. The role of matrix stiffness in regulating cell behavior. Hepatology. 2008;47:1394–1400. doi: 10.1002/hep.22193. [DOI] [PubMed] [Google Scholar]
- 30.Budday S, Nay R, de Rooij R, Steinmann P, Wyrobek T, Ovaert TC, et al. Mechanical properties of gray and white matter brain tissue by indentation. J Mech Behav Biomed. 2015;46:318–330. doi: 10.1016/j.jmbbm.2015.02.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lo CM, Wang HB, Dembo M, Wang YL. Cell movement is guided by the rigidity of the substrate. Biophy J. 2000;79:144–152. doi: 10.1016/S0006-3495(00)76279-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Toh WS, Lim TC, Kurisawa M, Spector M. Modulation of mesenchymal stem cell chondrogenesis in a tuneable hyaluronic acid hydrogel microenvironment. Biomaterials. 2012;33:3835–3845. doi: 10.1016/j.biomaterials.2012.01.065. [DOI] [PubMed] [Google Scholar]
- 33.Engler AJ, Sen S, Sweeney HL, Discher DE. Matrix elasticity directs stem cell lineage specification. Cell. 2006;126:677–689. doi: 10.1016/j.cell.2006.06.044. [DOI] [PubMed] [Google Scholar]
- 34.García A, Reyes CD. Bio-adhesive surfaces to promote osteoblast differentiation and bone formation. J Dent Res. 2005;84:407–413. doi: 10.1177/154405910508400502. [DOI] [PubMed] [Google Scholar]
- 35.Flanagan LA, Ju YE, Marg B, Osterfield M, Janmey PA. Neurite branching on deformable substrates. NeuroReport. 2002;13:2411–2415. doi: 10.1097/01.wnr.0000048003.96487.97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Deroanne CF, Lapiere CM, Nusgens BV. In vitro tubulogenesis of endothelial cells by relaxation of the coupling extracellular matrix-cytoskeleton. Cardiovasc Res. 2001;49:647–658. doi: 10.1016/s0008-6363(00)00233-9. [DOI] [PubMed] [Google Scholar]
- 37.Engler AJ, Richert L, Wong JY, Picart C, Discher DE. Surface probe measurements of the elasticity of sectioned tissue, thin gels and polyelectrolyte multilayer films: correlations between substrate stiffness and cell adhesion. Surface Sci. 2004;570:142–154. [Google Scholar]
- 38.Gilbert M, Havenstrite KL, Magnusson KE, Sacco A, Leonardi NA, Kraft P, et al. Substrate elasticity regulates skeletal muscle stem cell self-renewal in culture. Science. 2010;329:1078–1081. doi: 10.1126/science.1191035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kolahi KS, Donjacour A, Liu X, Lin W, Simbulan RK, Bloise E, et al. Effect of substrate stiffness on early mouse embryo development. PLoS One. 2012;7:e41717. doi: 10.1371/journal.pone.0041717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Chevallay B, Herbage D. Collagen-based biomaterials as 3D scaffold for cell cultures: applications for tissue engineering and gene therapy. Med Biol Eng Comput. 2000;38:211–218. doi: 10.1007/BF02344779. [DOI] [PubMed] [Google Scholar]
- 41.Goffin JM, Pittet P, Csucs G, Lussi JW, Meister JJ, Hinz B. Focal adhesion size controls tension-dependent recruitment of α-smooth muscle actin to stress fibres. J Cell Biol. 2006;172:259–268. doi: 10.1083/jcb.200506179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Muduli S, Chen LH, Li M, Heish ZW, Liu CH, Kumar S, et al. Stem cell culture on polyvinyl alcohol hydrogels having different elasticity and immobilized with ECM-derived oligopeptides. J Polym Eng. 2017;37:647–660. [Google Scholar]
- 43.Guilak F, Cohen DM, Estes BT, Gimble JM, Liedtke W, Chen CS. Control of stem cell fate by physical interactions with the extracellular matrix. Cell Stem Cell. 2009;5:17–26. doi: 10.1016/j.stem.2009.06.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Théry M. Micropatterning as a tool to decipher cell morphogenesis and functions. J Cell Sci. 2010;123:4201–4213. doi: 10.1242/jcs.075150. [DOI] [PubMed] [Google Scholar]
- 45.Halder G, Dupont S, Piccolo S. Transduction of mechanical and cytoskeletal cues by YAP and TAZ. Nat Rev Mol Cell Biol. 2012;13:591–600. doi: 10.1038/nrm3416. [DOI] [PubMed] [Google Scholar]
- 46.Maldonado M, Wong LY, Echeverria C, Ico G, Low K, Fujimoto T, et al. The effects of electrospun substrate-mediated cell colony morphology on the self-renewal of human induced pluripotent stem cells. Biomaterials. 2015;50:10–19. doi: 10.1016/j.biomaterials.2015.01.037. [DOI] [PubMed] [Google Scholar]
- 47.Abbas Y, Carnicer-Lombarte A, Gardner L, Thomas J, Brosens JJ, Moffett A, et al. Tissue stiffness at the human maternal–fetal interface. Hum Reprod. 2019;34:1999–2008. doi: 10.1093/humrep/dez139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Braam SR, Zeinstra L, Litjens S, Ward-van Oostwaard D, van den Brink S, van Laake L, et al. Recombinant vitronectin is a functionally defined substrate that supports human embryonic stem cell self-renewal via αVβ5 integrin. Stem Cells. 2008;26:2257–2265. doi: 10.1634/stemcells.2008-0291. [DOI] [PubMed] [Google Scholar]
- 49.Musah S, Morin SA, Wrighton J, Zwick DB, Jin S, Kiessling LL. Glycosaminoglycan-binding hydrogels enable mechanical control of human pluripotent stem cell self-renewal. ACS Nano. 2012;6:10168–10177. doi: 10.1021/nn3039148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Musah S, Wrighton J, Zaltsman Y, Zhong X, Zorn S, Parlato MB, et al. Substratum-induced differentiation of human pluripotent stem cells reveals the coactivator YAP is a potent regulator of neuronal specification. Proc Natl Acad Sci U S A. 2014;111:13805–13810. doi: 10.1073/pnas.1415330111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Chen YF, Li Y, Chou CH, Chiew MY, Huang HD, Ho JHC, et al. Control of matrix stiffness promotes endodermal lineage specification by regulating SMAD2/3 via lncRNA LINC00458. Sci Adv. 2020;6:eaay0264. doi: 10.1126/sciadv.aay0264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Chuah YJ, Koh YT, Lim K, Menon NV, Wu Y, Kang Y. Simple surface engineering of polydimethylsiloxane with polydopamine for stabilized mesenchymal stem cell adhesion and multipotency. Sci Rep. 2015;5:18162. doi: 10.1038/srep18162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Evans ND, Minelli C, Gentleman E, LaPointe V, Patankar SN, Kallivretaki M, et al. Substrate stiffness affects early differentiation events in embryonic stem cells. Eur Cells Mater. 2009;18:1–13. doi: 10.22203/ecm.v018a01. [DOI] [PubMed] [Google Scholar]
- 54.Palchesko RN, Zhang L, Sun Y, Feinberg AW. Development of polydimethylsiloxane substrates with tunable elastic modulus to study cell mechanobiology in muscle and nerve. PLoS One. 2012;7:e51499. doi: 10.1371/journal.pone.0051499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Yeh YC, Corbin EA, Caliari SR, Ouyang L, Vega SL, Truitt R, et al. Mechanically dynamic PDMS substrates to investigate changing cell environments. Biomaterials. 2017;145:23–32. doi: 10.1016/j.biomaterials.2017.08.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Maldonado M, Ico G, Low K, Luu RJ, Nam J. Enhanced Lineage-Specific Differentiation Efficiency of Human Induced Pluripotent Stem Cells by Engineering Colony Dimensionality Using Electrospun Scaffolds. Adv Healthc Mater. 2016;5:1408–1412. doi: 10.1002/adhm.201600141. [DOI] [PubMed] [Google Scholar]
- 57.Maldonado M, Luu RJ, Ico G, Ospina A, Myung D, Shih H, et al. Lineage-and developmental stage-specific mechanomodulation of induced pluripotent stem cell differentiation. Stem Cell Res Ther. 2017;8:216. doi: 10.1186/s13287-017-0667-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Wu Y, Xiang Y, Fang J, Li X, Lin Z, Dai G, et al. The influence of the stiffness of GelMA substrate on the outgrowth of PC12 cells. Biosci Rep. 2019;39:BSR20181748. doi: 10.1042/BSR20181748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Celikkin N, Mastrogiacomo S, Jaroszewicz J, Walboomers XF, Swieszkowski W. Gelatin methacrylate scaffold for bone tissue engineering: the influence of polymer concentration. J Biomed Mater Res A. 2018;106:201–209. doi: 10.1002/jbm.a.36226. [DOI] [PubMed] [Google Scholar]
- 60.Peter M, Singh A, Mohankumar K, Jeenger R, Joge A, Gatne MM, et al. Gelatin-based matrices as a tunable platform to study in vitro and in vivo 3D cell invasion. ACS Appl Bio Mater. 2019;2:916–929. doi: 10.1021/acsabm.8b00767. [DOI] [PubMed] [Google Scholar]
- 61.Singh A, Tayalia P. Three-dimensional cryogel matrix for spheroid formation and anti-cancer drug screening. J Biomed Mater Res A. 2020;108:365–376. doi: 10.1002/jbm.a.36822. [DOI] [PubMed] [Google Scholar]
- 62.Kang H, Shih YRV, Hwang Y, Wen C, Rao V, Seo T, et al. Mineralized gelatin methacrylate-based matrices induce osteogenic differentiation of human induced pluripotent stem cells. Acta Biomater. 2014;10:4961–4970. doi: 10.1016/j.actbio.2014.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Llames S, García-Pérez E, Meana Á, Larcher F, del Río M. Feeder layer cell actions and applications. Tissue Eng Part B Rev. 2015;21:345–353. doi: 10.1089/ten.teb.2014.0547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Puck TT, Marcus I. A rapid method for viable cell titration and clone production with HeLa cells in tissue culture: the use of X-irradiated cells to supply conditioning factors. PNAS USA. 1955;41:432. doi: 10.1073/pnas.41.7.432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Rodin S, Antonsson L, Hovatta O, Tryggvason K. Monolayer culturing and cloning of human pluripotent stem cells on laminin-521–based matrices under xeno-free and chemically defined conditions. Nat Protoc. 2014;9:2354–2368. doi: 10.1038/nprot.2014.159. [DOI] [PubMed] [Google Scholar]
- 66.Somaiah C, Kumar A, Mawrie D, Sharma A, Patil SD, Bhattacharyya J, et al. Collagen promotes higher adhesion, survival and proliferation of mesenchymal stem cells. PLoS One. 2015;10:e0145068. doi: 10.1371/journal.pone.0145068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Amit M, Shariki C, Margulets V, Itskovitz-Eldor J. Feeder layer-and serum-free culture of human embryonic stem cells. Biol Reprod. 2004;70:837–845. doi: 10.1095/biolreprod.103.021147. [DOI] [PubMed] [Google Scholar]
- 68.Chen G, Gulbranson DR, Hou Z, Bolin JM, Ruotti V, Probasco MD, et al. Chemically defined conditions for human iPSC derivation and culture. Nat Methods. 2011;8:424–429. doi: 10.1038/nmeth.1593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Philp D, Chen SS, Fitzgerald W, Orenstein J, Margolis L, Kleinman HK. Complex extracellular matrices promote tissue-specific stem cell differentiation. Stem Cells. 2005;23:288–296. doi: 10.1634/stemcells.2002-0109. [DOI] [PubMed] [Google Scholar]
- 70.Kleinman HK, Martin GR. Matrigel: basement membrane matrix with biological activity. Semin Cancer Biol. 2005;15:378–386. doi: 10.1016/j.semcancer.2005.05.004. [DOI] [PubMed] [Google Scholar]
- 71.Hughes CS, Postovit LM, Lajoie GA. Matrigel: a complex protein mixture required for optimal growth of cell culture. Proteomics. 2010;10:1886–1890. doi: 10.1002/pmic.200900758. [DOI] [PubMed] [Google Scholar]
- 72.Davidenko N, Campbell JJ, Thian ES, Watson CJ, Cameron RE. Collagen–hyaluronic acid scaffolds for adipose tissue engineering. Acta Biomater. 2010;6:3957–3968. doi: 10.1016/j.actbio.2010.05.005. [DOI] [PubMed] [Google Scholar]
- 73.Pawelec KM, Best SM, Cameron RE. Collagen: a network for regenerative medicine. J Mater Chem B. 2016;4:6484–6496. doi: 10.1039/c6tb00807k. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Chen C, Zhao ML, Zhang RK, Lu G, Zhao CY, Fu F, et al. Collagen/heparin sulfate scaffolds fabricated by a 3D bioprinter improved mechanical properties and neurological function after spinal cord injury in rats. J Biomed Mater Res A. 2017;105:1324–1332. doi: 10.1002/jbm.a.36011. [DOI] [PubMed] [Google Scholar]
- 75.Khatami N, Khoshfetrat AB, Khaksar M, Zamani ARN, Rahbarghazi R. Collagen-alginate-nano-silica microspheres improved the osteogenic potential of human osteoblast-like MG-63 cells. J Cell Biochem. 2019;120:15069–15082. doi: 10.1002/jcb.28768. [DOI] [PubMed] [Google Scholar]
- 76.Hughes CS, Radan L, Betts D, Postovit LM, Lajoie GA. Proteomic analysis of extracellular matrices used in stem cell culture. Proteomics. 2011;11:3983–3991. doi: 10.1002/pmic.201100030. [DOI] [PubMed] [Google Scholar]
- 77.Baxter MA, Camarasa MV, Bates N. Analysis of the distinct functions of growth factors and tissue culture substrates necessary for the long-term self-renewal of human embryonic stem cell lines. Stem Cell Res. 2009;3:28–38. doi: 10.1016/j.scr.2009.03.002. [DOI] [PubMed] [Google Scholar]
- 78.Jacobsen MM, Li D, Rim NG, Backman D, Smith ML, Wong JY. Silk-fibronectin protein alloy fibres support cell adhesion and viability as a high strength, matrix fibre analogue. Sci Rep. 2017;7:45653. doi: 10.1038/srep45653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Xu C, Inokuma MS, Denham J, Golds K, Kundu P, Gold JD, et al. Feeder-free growth of undifferentiated human embryonic stem cells. Nat Biotechnol. 2001;19:971–974. doi: 10.1038/nbt1001-971. [DOI] [PubMed] [Google Scholar]
- 80.Kohen NT, Little LE, Healy KE. Characterization of Matrigel interfaces during defined human embryonic stem cell culture. Biointerphases. 2009;4:69–79. doi: 10.1116/1.3274061. [DOI] [PubMed] [Google Scholar]
- 81.Semler EJ, Ranucci CS, Moghe V. Mechanochemical manipulation of hepatocyte aggregation can selectively induce or repress liver-specific function. Biotechnol Bioeng. 2000;69:359–369. doi: 10.1002/1097-0290(20000820)69:4<359::aid-bit2>3.0.co;2-q. [DOI] [PubMed] [Google Scholar]
- 82.Soofi SS, Last JA, Liliensiek SJ, Nealey F, Murphy CJ. The elastic modulus of Matrigel™ as determined by atomic force microscopy. J Struct Biol. 2009;167:216–219. doi: 10.1016/j.jsb.2009.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Takahashi Y, Sato S, Kurashima Y, Yamamoto T, Kurokawa S, Yuki Y, et al. A refined culture system for human induced pluripotent stem cell-derived intestinal epithelial organoids. Stem Cell Rep. 2018;10:314–328. doi: 10.1016/j.stemcr.2017.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Khaing ZZ, Seidlits SK. Hyaluronic acid and neural stem cells: implications for biomaterial design. J Mater Chem B. 2015;3:7850–7866. doi: 10.1039/c5tb00974j. [DOI] [PubMed] [Google Scholar]
- 85.Bierman R. Hyaluronic acid-based hydrogels as an in vitro approach to neural stem/progenitor cell differentiation [Doctoral dissertation]. Los Angeles: University of California, Los Angeles; 2018.
- 86.Wang HB, Dembo M, Wang YL. Substrate flexibility regulates growth and apoptosis of normal but not transformed cells. Am J Physiol Cell Physiol. 2000;279:C1345–C1350. doi: 10.1152/ajpcell.2000.279.5.C1345. [DOI] [PubMed] [Google Scholar]
- 87.Wong JY, Velasco A, Rajagopalan P, Pham Q. Directed movement of vascular smooth muscle cells on gradient-compliant hydrogels. Langmuir. 2003;19:1908–1913. [Google Scholar]
- 88.Sachot N, Engel E, Castaño O. Hybrid organic-inorganic scaffolding biomaterials for regenerative therapies. Curr Org Chem. 2014;18:2299–2314. [Google Scholar]
- 89.Brown XQ, Ookawa K, Wong JY. Evaluation of polydimethylsiloxane scaffolds with physiologically-relevant elastic moduli: interplay of substrate mechanics and surface chemistry effects on vascular smooth muscle cell response. Biomaterials. 2005;26:3123–3129. doi: 10.1016/j.biomaterials.2004.08.009. [DOI] [PubMed] [Google Scholar]
- 90.Jun I, Han HS, Edwards J, Jeon H. Electrospun fibrous scaffolds for tissue engineering: viewpoints on architecture and fabrication. Int J Mol Sci. 2018;19:745. doi: 10.3390/ijms19030745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Berkovitch Y, Seliktar D. Semi-synthetic hydrogel composition and stiffness regulate neuronal morphogenesis. Int J Pharm. 2017;523:545–555. doi: 10.1016/j.ijpharm.2016.11.032. [DOI] [PubMed] [Google Scholar]
- 92.Van Den Bulcke AI, Bogdanov B, De Rooze N, Schacht EH, Cornelissen M, Berghmans H. Structural and rheological properties of methacrylamide modified gelatin hydrogels. Biomacromol. 2000;1:31–38. doi: 10.1021/bm990017d. [DOI] [PubMed] [Google Scholar]
- 93.Wei D, Xiao W, Sun J, Zhong M, Guo L, Fan H, et al. A biocompatible hydrogel with improved stiffness and hydrophilicity for modular tissue engineering assembly. J Mater ChemB. 2015;3:2753–2763. doi: 10.1039/c5tb00129c. [DOI] [PubMed] [Google Scholar]
- 94.Costantini M, Testa S, Fornetti E, Barbetta A, Trombetta M, Cannata SM, et al. Engineering muscle networks in 3D gelatin methacryloyl hydrogels: influence of mechanical stiffness and geometrical confinement. Front Bioeng Biotechnol. 2017;5:22. doi: 10.3389/fbioe.2017.00022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Pepelanova I, Kruppa K, Scheper T, Lavrentieva A. Gelatin-Methacryloyl (GelMA) hydrogels with defined degree of functionalization as a versatile toolkit for 3D cell culture and extrusion bioprinting. Bioengineering (Basel) 2018;5:55. doi: 10.3390/bioengineering5030055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Zhao X, Liu S, Yildirimer L, Zhao H, Ding R, Wang H, et al. Injectable stem cell-laden photocrosslinkable microspheres fabricated using microfluidics for rapid generation of osteogenic tissue constructs. Adv Func Mater. 2016;26:2809–2819. [Google Scholar]
- 97.Eke G, Mangir N, Hasirci N, MacNeil S, Hasirci V. Development of a UV crosslinked biodegradable hydrogel containing adipose derived stem cells to promote vascularization for skin wounds and tissue engineering. Biomaterials. 2017;129:188–198. doi: 10.1016/j.biomaterials.2017.03.021. [DOI] [PubMed] [Google Scholar]
- 98.Zhang X, Li J, Ye P, Gao G, Hubbell K, Cui X. Coculture of mesenchymal stem cells and endothelial cells enhances host tissue integration and epidermis maturation through AKT activation in gelatin methacryloyl hydrogel-based skin model. Acta Biomater. 2017;59:317–326. doi: 10.1016/j.actbio.2017.07.001. [DOI] [PubMed] [Google Scholar]
- 99.Kerscher P, Kaczmarek JA, Head SE, Ellis ME, Seeto WJ, Kim J, et al. Direct production of human cardiac tissues by pluripotent stem cell encapsulation in gelatin methacryloyl. ACS Biomater Sci Eng. 2016;3:1499–1509. doi: 10.1021/acsbiomaterials.6b00226. [DOI] [PubMed] [Google Scholar]
- 100.Visser J, Gawlitta D, Benders KE, Toma SM, Pouran B, van Weeren R, et al. Endochondral bone formation in gelatin methacrylamide hydrogel with embedded cartilage-derived matrix particles. Biomaterials. 2015;37:174–182. doi: 10.1016/j.biomaterials.2014.10.020. [DOI] [PubMed] [Google Scholar]
- 101.Ebrahimi M, Ostrovidov S, Salehi S, Kim SB, Bae H, Khademhosseini A. Enhanced skeletal muscle formation on microfluidic spun gelatin methacryloyl (GelMA) fibres using surface patterning and agrin treatment. J Tissue Eng Regen Med. 2018;12:2151–2163. doi: 10.1002/term.2738. [DOI] [PubMed] [Google Scholar]
- 102.Lin RZ, Chen YC, Moreno-Luna R, Khademhosseini A, Melero-Martin JM. Transdermal regulation of vascular network bioengineering using a photopolymerizable methacrylated gelatin hydrogel. Biomaterials. 2013;34:6785–6796. doi: 10.1016/j.biomaterials.2013.05.060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Amano M, Nakayama M, Kaibuchi K. Rho-kinase/ROCK: a key regulator of the cytoskeleton and cell polarity. Cytoskeleton. 2010;67:545–554. doi: 10.1002/cm.20472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Donato DM, Ryzhova LM, Meenderink LM, Kaverina I, Hanks SK. Dynamics and mechanism of p130Cas localization to focal adhesions. J Biol Chem. 2010;285:20769–20779. doi: 10.1074/jbc.M109.091207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Ciobanasu C, Faivre B, Le Clainche C. Integrating actin dynamics, mechanotransduction and integrin activation: the multiple functions of actin binding proteins in focal adhesions. Eur J Cell Biol. 2013;92:339–348. doi: 10.1016/j.ejcb.2013.10.009. [DOI] [PubMed] [Google Scholar]
- 106.Janoštiak R, Pataki AC, Brábek J, Rösel D. Mechanosensors in integrin signaling: the emerging role of p130Cas. Eur J Cell Biol. 2014;93:445–454. doi: 10.1016/j.ejcb.2014.07.002. [DOI] [PubMed] [Google Scholar]
- 107.Elosegui-Artola A, Andreu I, Beedle AE, Lezamiz A, Uroz M, Kosmalska AJ, et al. Force triggers YAP nuclear entry by regulating transport across nuclear pores. Cell. 2017;171:1397–1410. doi: 10.1016/j.cell.2017.10.008. [DOI] [PubMed] [Google Scholar]
- 108.Bissell MJ, Aggeler J. Dynamic reciprocity: how do extracellular matrix and hormones direct gene expression? Prog Clin Biol Res. 1987;249:251–262. [PubMed] [Google Scholar]
- 109.Humphrey JD, Dufresne ER, Schwartz MA. Mechanotransduction and extracellular matrix homeostasis. Nat Rev Mol Cell Biol. 2014;15:802–812. doi: 10.1038/nrm3896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Gumbiner B. Signal transduction by B-catenin. Curr Opin Cell Biol. 1995;7:634–640. doi: 10.1016/0955-0674(95)80104-9. [DOI] [PubMed] [Google Scholar]
- 111.Huber O, Korn R, McLaughlin J, Ohsugi M, Herrmann BG, Kemler R. Nuclear localization of b-catenin by interaction with transcription factor LEF-1. Mech Dev. 1996;59:3–10. doi: 10.1016/0925-4773(96)00597-7. [DOI] [PubMed] [Google Scholar]
- 112.Spadaro D, Le S, Laroche T, Mean I, Jond L, Yan J, et al. Tension-dependent stretching activates ZO-1 to control the junctional localization of its interactors. Curr Biol. 2017;27:3783–3795. doi: 10.1016/j.cub.2017.11.014. [DOI] [PubMed] [Google Scholar]
- 113.Lewis JM, Baskaran R, Taagepera S, Schwartz MA, Wang JY. Integrin regulation of c-Abl tyrosine kinase activity and cytoplasmic-nuclear transport. Proc Natl Acad Sci U S A. 1996;93:15174–15179. doi: 10.1073/pnas.93.26.15174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Speight P, Kofler M, Szászi K, Kapus A. Context-dependent switch in chemo/mechanotransduction via multilevel crosstalk among cytoskeleton-regulated MRTF and TAZ and TGFβ-regulated Smad3. Nat Commun. 2016;7:1–17. doi: 10.1038/ncomms11642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Kumar A, Boriek AM. Mechanical stress activates the nuclear factor-kappaB pathway in skeletal muscle fibers: a possible role in Duchenne muscular dystrophy. The FASEB J. 2003;17:386–396. doi: 10.1096/fj.02-0542com. [DOI] [PubMed] [Google Scholar]
- 116.Escoll M, Lastra D, Pajares M, Robledinos-Antón N, Rojo AI, Fernández-Ginés R, et al. Transcription factor NRF2 uses the Hippo pathway effector TAZ to induce tumorigenesis in glioblastomas. Redox Biol. 2020;30:101425. doi: 10.1016/j.redox.2019.101425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Li Y, Chu JS, Kurpinski K, Li X, Bautista DM, Yang L, et al. Biophysical regulation of histone acetylation in mesenchymal stem cells. Biophys J. 2011;100:1902–1909. doi: 10.1016/j.bpj.2011.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Guilluy C, Osborne LD, Van Landeghem L, Sharek L, Superfine R, Garcia-Mata R. Isolated nuclei adapt to force and reveal a mechanotransduction pathway in the nucleus. Nat Cell Biol. 2014;16:376–381. doi: 10.1038/ncb2927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Driscoll T, Cosgrove BD, Heo SJ, Shurden ZE, Mauck RL. Cytoskeletal to nuclear strain transfer regulates YAP signaling in mesenchymal stem cells. Biophys J. 2015;108:2783–2793. doi: 10.1016/j.bpj.2015.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Sudol M, Bork P, Einbond A, Kastury K, Druck T, Negrini M, et al. Characterization of the mammalian YAP (Yes-associated protein) gene and its role in defining a novel protein module, the WW domain. J Biol Chem. 1995;270:14733–14741. doi: 10.1074/jbc.270.24.14733. [DOI] [PubMed] [Google Scholar]
- 121.Kanai F, Marignani A, Sarbassova D, Yagi R, Hall RA, Donowitz M, et al. TAZ: a novel transcriptional co-activator regulated by interactions with 14-3-3 and PDZ domain proteins. The EMBO J. 2000;19:6778–6791. doi: 10.1093/emboj/19.24.6778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Hong W, Guan KL. The YAP and TAZ transcription co-activators: key downstream effectors of the mammalian Hippo pathway. Semin Cell Dev Biol. 2012;23:785–793. doi: 10.1016/j.semcdb.2012.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Low BC, Pan CQ, Shivashankar GV, Bershadsky A, Sudol M, Sheetz M. YAP/TAZ as mechanosensors and mechanotransducers in regulating organ size and tumor growth. FEBS Lett. 2014;588:2663–2670. doi: 10.1016/j.febslet.2014.04.012. [DOI] [PubMed] [Google Scholar]
- 124.Hansen CG, Moroishi T, Guan KL. YAP and TAZ: a nexus for Hippo signaling and beyond. Trends Cell Biol. 2015;25:499–513. doi: 10.1016/j.tcb.2015.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Zhao B, Li L, Lu Q, Wang LH, Liu CY, Lei Q, et al. Angiomotin is a novel Hippo pathway component that inhibits YAP oncoprotein. Genes Dev. 2011;25:51–63. doi: 10.1101/gad.2000111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Azzolin L, Panciera T, Soligo S, Enzo E, Bicciato S, Dupont S, et al. YAP/TAZ incorporation in the β-catenin destruction complex orchestrates the Wnt response. Cell. 2014;158:157–170. doi: 10.1016/j.cell.2014.06.013. [DOI] [PubMed] [Google Scholar]
- 127.Shao Y, Sang J, Fu J. On human pluripotent stem cell control: the rise of 3D bioengineering and mechanobiology. Biomaterials. 2015;52:26–43. doi: 10.1016/j.biomaterials.2015.01.078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Szeto SG, Narimatsu M, Lu M, He X, Sidiqi AM, Tolosa MF, et al. YAP/TAZ are mechanoregulators of TGF-β-Smad signaling and renal fibrogenesis. J Am Soc Nephrol. 2016;27:3117–3128. doi: 10.1681/ASN.2015050499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Kim MK, Jang JW, Bae SC. DNA binding partners of YAP/TAZ. BMB Rep. 2018;51:126–133. doi: 10.5483/BMBRep.2018.51.3.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Huang J, Wu S, Barrera J, Matthews K, Pan D. The Hippo signaling pathway coordinately regulates Cell proliferation apoptosis by inactivating Yorkie, the Drosophila Homolog of YAP. Cell. 2005;122:421–434. doi: 10.1016/j.cell.2005.06.007. [DOI] [PubMed] [Google Scholar]
- 131.Zhao B, Wei X, Li W, Udan RS, Yang Q, Kim J, et al. Inactivation of YAP oncoprotein by the Hippo pathway is involved in cell contact inhibition and tissue growth control. Genes Dev. 2007;21:2747–2761. doi: 10.1101/gad.1602907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Zhang X, Milton CC, Humbert O, Harvey KF. Transcriptional output of the Salvador/warts/hippo pathway is controlled in distinct fashions in Drosophila melanogaster and mammalian cell lines. Cancer Res. 2009;69:6033–6041. doi: 10.1158/0008-5472.CAN-08-4592. [DOI] [PubMed] [Google Scholar]
- 133.Liu C, Huang W, Lei Q. Regulation and function of the TAZ transcription co-activator. Int J Biochem Mol Bio. 2011;2:247. [PMC free article] [PubMed] [Google Scholar]
- 134.Sun C, De Mello V, Mohamed A, Ortuste Quiroga HP, Garcia-Munoz A, Al Bloshi A, et al. Common and distinctive functions of the hippo effectors Taz and Yap in Skeletal Muscle stem cell function. Stem Cells. 2017;35:1958–1972. doi: 10.1002/stem.2652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Plouffe SW, Lin KC, Moore JL, 3rd, Tan FE, Ma S, Ye Z, et al. The Hippo pathway effector proteins YAP and TAZ have both distinct and overlapping functions in the cell. J Biol Chem. 2018;293:11230–11240. doi: 10.1074/jbc.RA118.002715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Finch-Edmondson ML, Strauss R, Passman AM, Sudol M, Yeoh GC, Callus BA. TAZ protein accumulation is negatively regulated by YAP abundance in mammalian cells. J Biol Chem. 2015;290:27928–27938. doi: 10.1074/jbc.M115.692285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Lian I, Kim J, Okazawa H, Zhao J, Zhao B, Yu J, et al. The role of YAP transcription coactivator in regulating stem cell self-renewal and differentiation. Genes Dev. 2010;24:1106–1118. doi: 10.1101/gad.1903310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Morin-Kensicki EM, Boone BN, Howell M, Stonebraker JR, Teed J, Alb JG, et al. Defects in yolk sac vasculogenesis, chorioallantoic fusion, and embryonic axis elongation in mice with targeted disruption of Yap65. Mol Cell Biol. 2006;26:77–87. doi: 10.1128/MCB.26.1.77-87.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Tian Y, Kolb R, Hong JH, Carroll J, Li D, You J, et al. TAZ promotes PC2 degradation through a SCFβ-Trcp E3 ligase complex. Mol Cell Biol. 2007;27:6383–6395. doi: 10.1128/MCB.00254-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Hossain Z, Ali SM, Ko HL, Xu J, Ng C, Guo K, et al. Glomerulocystic kidney disease in mice with a targeted inactivation of Wwtr1. Proc Natl Acad Sci U S A. 2007;104:1631–1636. doi: 10.1073/pnas.0605266104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Makita R, Uchijima Y, Nishiyama K, Amano T, Chen Q, Takeuchi T, et al. Multiple renal cysts, urinary concentration defects, and pulmonary emphysematous changes in mice lacking TAZ. Am J Physiol-Renal. 2008;294:F542–F553. doi: 10.1152/ajprenal.00201.2007. [DOI] [PubMed] [Google Scholar]
- 142.Brenan L. Elucidating the role of YAP in directing mesenchymal stem cell fate. Master of Arts thesis, Boston University. 2015.
- 143.Nie P, Li Y, Suo H, Jiang N, Yu D, Fang B. Dasatinib promotes chondrogenic differentiation of human mesenchymal stem cells via the Src/Hippo-YAP signaling pathway. ACS Biomater Sci Eng. 2019;5:5255–5265. doi: 10.1021/acsbiomaterials.9b00618. [DOI] [PubMed] [Google Scholar]
- 144.Qin H, Hejna M, Liu Y, Percharde M, Wossidlo M, Blouin L, et al. YAP induces human naive pluripotency. Cell Rep. 2016;14:2301–2312. doi: 10.1016/j.celrep.2016.02.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Hsu HT, Estarás C, Huang L, Jones KA. Specifying the anterior primitive streak by modulating YAP1 levels in human pluripotent stem cells. Stem cell Rep. 2018;11:1357–1364. doi: 10.1016/j.stemcr.2018.10.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Zanconato F, Cordenonsi M, Piccolo S. YAP/TAZ at the roots of cancer. Cancer Cell. 2016;29:783–803. doi: 10.1016/j.ccell.2016.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Overholtzer M, Zhang J, Smolen GA, Muir B, Li W, Sgroi DC, et al. Transforming properties of YAP, a candidate oncogene on the chromosome 11q22 amplicon. Proc Natl Acad Sci U S A. 2006;103:12405–12410. doi: 10.1073/pnas.0605579103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Zender L, Spector MS, Xue W, Flemming P, Cordon-Cardo C, Silke J, et al. Identification and validation of oncogenes in liver cancer using an integrative oncogenomic approach. Cell. 2006;125:1253–1267. doi: 10.1016/j.cell.2006.05.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Camargo FD, Gokhale S, Johnnidis JB, Fu D, Bell GW, Jaenisch R, et al. YAP1 increases organ size and expands undifferentiated progenitor cells. Curr Biol. 2007;17:2054–2060. doi: 10.1016/j.cub.2007.10.039. [DOI] [PubMed] [Google Scholar]
- 150.Debaugnies M, Sánchez-Danés A, Rorive S, Raphaël M, Liagre M, Parent MA, et al. YAP and TAZ are essential for basal and squamous cell carcinoma initiation. EMBO Rep. 2018;19:e45809. [DOI] [PMC free article] [PubMed]
- 151.Dupont S, Morsut L, Aragona M, Enzo E, Giulitti S, Cordenonsi M, et al. Role of YAP/TAZ in mechanotransduction. Nature. 2011;474:179–183. doi: 10.1038/nature10137. [DOI] [PubMed] [Google Scholar]
- 152.Piccolo S, Dupont S, Cordenonsi M. The biology of YAP/TAZ: hippo signalling and beyond. Physiol Rev. 2014;94:1287–1312. doi: 10.1152/physrev.00005.2014. [DOI] [PubMed] [Google Scholar]
- 153.Elosegui-Artola A, Oria R, Chen Y, Kosmalska A, Pérez-González C, Castro N, et al. Mechanical regulation of a molecular clutch defines force transmission and transduction in response to matrix rigidity. Nat Cell Biol. 2016;18:540–548. doi: 10.1038/ncb3336. [DOI] [PubMed] [Google Scholar]
- 154.Aragona M, Panciera T, Manfrin A, Giulitti S, Michielin F, Elvassore N, et al. A mechanical checkpoint controls multicellular growth through YAP/TAZ regulation by actin-processing factors. Cell. 2013;154:1047–1059. doi: 10.1016/j.cell.2013.07.042. [DOI] [PubMed] [Google Scholar]
- 155.Smith Q, Chan XY, Carmo AM, Trempel M, Saunders M, Gerecht S. Compliant substratum guides endothelial commitment from human pluripotent stem cells. Sci Adv. 2017;3:e1602883. doi: 10.1126/sciadv.1602883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Price AJ, Huang EY, Sebastiano V, Dunn AR. A semi-interpenetrating network of polyacrylamide and recombinant basement membrane allows pluripotent cell culture in a soft, ligand-rich microenvironment. Biomaterials. 2017;121:179–192. doi: 10.1016/j.biomaterials.2016.12.005. [DOI] [PubMed] [Google Scholar]
- 157.Wang HB, Dembo M, Hanks SK, Wang YL. Focal adhesion kinase is involved in mechanosensing during fibroblast migration. Proc Natl Acad Sci U S A. 2001;98:11295–11300. doi: 10.1073/pnas.201201198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Hadden WJ, Young JL, Holle AW, McFetridge ML, Kim DY, Wijesinghe P, et al. Stem cell migration and mechanotransduction on linear stiffness gradient hydrogels. Proc Natl Acad Sci U S A. 2017;114:5647–5652. doi: 10.1073/pnas.1618239114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Lachowski D, Cortes E, Robinson B, Rice A, Rombouts K, Del Río Hernández AE. FAK controls the mechanical activation of YAP, a transcriptional regulator required for durotaxis. The FASEB J. 2017;32:1099–1107. doi: 10.1096/fj.201700721R. [DOI] [PubMed] [Google Scholar]
- 160.Ong CS, Yesantharao P, Huang CY, Mattson G, Boktor J, Fukunishi T, et al. 3D bioprinting using stem cells. Pediatr Res. 2018;83:223. doi: 10.1038/pr.2017.252. [DOI] [PubMed] [Google Scholar]
- 161.Jeon O, Lee YB, Jeong H, Lee SJ, Wells D, Alsberg E. Individual cell-only bioink and photocurable supporting medium for 3D printing and generation of engineered tissues with complex geometries. Mater Horiz. 2019;6:1625–1631. doi: 10.1039/c9mh00375d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Gershovich JG, Buravkova LB. Morphofunctional status and osteogenic differentiation potential of human mesenchymal stromal precursor cells during in vitro modeling of microgravity effects. Bull Exp Biol Med. 2007;144:608–613. doi: 10.1007/s10517-007-0387-1. [DOI] [PubMed] [Google Scholar]
- 163.Baio J, Martinez AF, Silva I, Hoehn CV, Countryman S, Bailey L, et al. Cardiovascular progenitor cells cultured aboard the International Space Station exhibit altered developmental and functional properties. NPJ Microgravity. 2018;4:13. doi: 10.1038/s41526-018-0048-x. [DOI] [PMC free article] [PubMed] [Google Scholar]