Abstract
Maintaining oral function in older individuals with missing teeth is important for leading a healthy and independent life. This study aimed to evaluate whether simple isometric exercises can maintain and improve the oral function [maximum occlusal force (MOF) and masticatory ability (MA)] and the masticatory muscle properties [masseter muscle thickness (MMT) and echo intensity (MMEI)] in older adults during the maintenance phase of removable prosthetic treatment. Participants were randomly categorized into the intervention and control groups. The mouthpieces were distributed, and participants were instructed to use them for exercising. The intervention group was instructed to perform maximum clenching for 10 s, whereas the control group was instructed to tap the teeth at an arbitrary speed for 10 s. Both were repeated five times at an interval of 5 s between each activity and twice daily for 4 weeks. The outcomes were measured after a month of exercise. The intervention group showed a significant improvement in the MOF, MMT during contraction, MMT at rest and MMEI during contraction. There were no significant differences in the MA and MMEI at rest. In the control group, no improvement was observed in any of the parameters. When the isometric exercises were performed using a mouthpiece, there was an improvement in the oral function and masseter muscle properties in older individuals with Eichner B status who used dentures.
Subject terms: Dentistry, Nutrition
Introduction
Background and objective
A decrease in the oral function, represented by the maximum occlusal force (MOF) and the masticatory ability (MA), is a risk factor for adverse events such as sarcopenia and death1. MOF and MA greatly influence dietary choices2; a reduced bite force quotient leads to protein, fiber, mineral, and vitamin deficiencies3–5, resulting in a risk of undernutrition6. Maintaining the oral function is important for maintaining a healthy and independent life in older individuals. Aging and tooth loss are mainly considered to be responsible for a decrease in the MA and MOF7; however, these are reportedly related to the properties of masticatory muscles, especially of the masseter (for e.g., quantity and quality). Masseter muscle thickness (MMT) is reportedly associated with MOF8, and masseter muscle echo intensity (MMEI) is negatively correlated with MOF and MMT9. Muscle echo intensity can be evaluated by an ultrasonic diagnostic device that identifies non-contractile tissues (such as fat and fibrous tissues) in the muscle, and indicates muscle quality10. Several previous studies have reported that the MA, MOF, and MMT are greatly improved with dental prosthetic treatments such as implants and dentures11–13. In addition to prosthetic treatment, isometric exercise is also used as a modality for maintaining oral function. A retrospective comparative study of 28 young people showed that a simple isometric exercise using a mouthpiece resulted in an improvement in the MOF14. However, there are no reports on an effective training for maintaining the oral function in older adults with a missing dentition. Therefore, the purpose of this study was to clarify whether simple isometric exercises can maintain and improve the oral function (MOF and MA) and masticatory muscle properties (MMT and MMEI) in older adults during the maintenance phase of removable prosthetic treatment.
Methods
Trial design
This study was a multi-center, double-blinded, randomized, controlled, parallel clinical trial. Figure 1 shows the flow diagram of this randomized, controlled trial. This study was performed with the approval of the Clinical Research Ethics Committee of the Tokyo Medical and Dental University (D2018-021), and was registered in the UMIN clinical trial registration system on August 08, 2018 (UMIN000032933). This study was also conducted in accordance with the latest revision of the Declaration of Helsinki.
Figure 1.
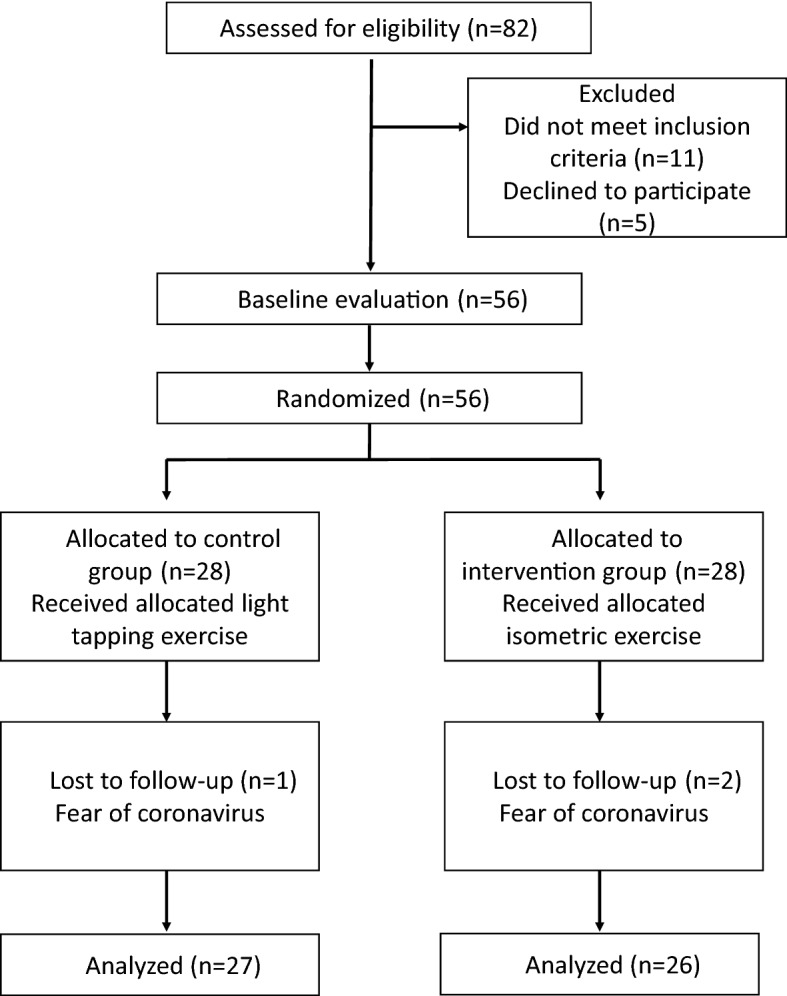
Flow diagram of this randomized-controlled trial.
Participants
Participants were adults who were aged 65 years and above and had removable dentures as prostheses for partial edentulism. They were recruited at an outpatient clinic (Tokyo, Japan) and at the dental hospital of the Tokyo Medical and Dental University.
The state of tooth-loss was categorized using the Eichner classification15. The inclusion criteria were as follows: (1) Eichner B-1 to B-3 groups that have occlusal support areas, which are the upper, lower, left, and right premolars and molars, and one to three of these are lost and (2) patients in the maintenance phase who had already completed denture adjustment. Patients excluded from the study were those who: (1) had difficulty in following instructions, (2) had progressive neuromuscular disease, (3) had severe temporomandibular joint symptoms (for e.g., trismus and pain during jaw movement), (4) required denture adjustment (for e.g., pain due to the denture), (5) had mobile teeth due to severe periodontal disease, and (6) had parafunctional findings. All participants had used the current dentures for at least 4 weeks. Written informed consent was obtained from all participants after a detailed explanation of the procedure.
Intervention
At the beginning of the study, the baseline outcomes were measured, and the impression of the upper jaw was obtained for the mouthpiece. The mouthpiece was fabricated by softening a 1.0-mm-thick thermoplastic sheet (for soft splint), which was then adapted on a plaster model with the help of a vacuum adapter (Yamahachi Dental Industry, Aichi, Japan), as described in a previous study14. On the next visit, the participants received the mouthpieces after proper adjustment and were randomly divided into two groups (Fig. 2). Thereafter, one of the dentists (who is not the doctor who measured the baseline outcomes) explained the intervention method to the participants.
Figure 2.
Mouthpiece and its placement in the oral cavity.
Intervention group
In the intervention group, a denture was provided to replace missing teeth in either the upper or lower jaw, and then a mouthpiece was fabricated for the upper jaw. If there was a denture in the upper jaw, the mouthpiece was worn over the denture. Subsequently, the participant was instructed to perform maximum clenching for 10 s. The training was repeated five times at an interval of 5 s between each clenching activity.
Control group
In the control group, a denture was provided to replace missing teeth in either the upper or lower jaw, and a mouthpiece was then fabricated for the upper jaw. If there was a denture in the upper jaw, the mouthpiece was worn over the denture. However, unlike in the intervention group, participants in the control group were instructed to tap their teeth at an arbitrary speed for 10 s, and this was repeated five times at an interval of 5 s.
Both groups performed their respective exercises twice a day, in the morning and evening, for a period of 4 weeks.
Measurement of the MOF, MA, MMT, and MMEI
The MOF, MA, MMT, and MMEI were measured using appropriate diagnostic devices. Participants were instructed to be seated on chairs in a relaxed position with their backs stretched, feet firmly touching the floor, and the Frankfurt horizontal plane parallel to the floor.
To measure the MOF, a pressure-sensitive film (Dental Prescale II, GC, Tokyo, Japan) was aligned with the dentition, and the participant was instructed to bite with maximum force. The scanner was calibrated16, the pressure-sensitive film was fitted to the template, and analysis was performed using an analysis software (Bite Force Analyzer GC, Tokyo, Japan).
For the measurement of MA, participants were instructed to freely chew a cylindrical-shaped gummy jelly (GC, Tokyo, Japan) composed of 40% maltose, 10% sorbitol, and 5% glucose, for 20 s. After chewing, the participants were asked to hold 10 mL of distilled water in their mouth and to spit the gummy jelly, distilled water, and saliva into a cup with a filter. The glucose concentration in the filtrate was measured using a glucose measuring device (Glucosensor GS-II, GC, Tokyo, Japan)17.
An ultrasonic diagnostic device (fST9600 Lequio Power Technology, Naha, Japan) was used to measure the MMT and MMEI. A linear probe was used with a broadband frequency ranging from 6.7 to 8.0 MHz. Scanning was performed in the B mode. The scanning depth was 38 mm and the gain was 80 dB, and these values were constant during the measurement. The measurements were performed by a dentist with 12 years of clinical experience.
As described in a previous study18, the probe was placed parallel to the mandibular margin, approximately midway between the zygomatic arch and the mandibular angle, and perpendicular to the skin surface. In accordance with existing literature, the probe was applied lightly19.
While measuring the thickness of the masseter muscle and its echo intensity, the patients were instructed to maintain the mandibular rest position for at least 20 min before ultrasonography in order to reduce the effects of muscle contraction on the blood flow and interstitial fluid20.
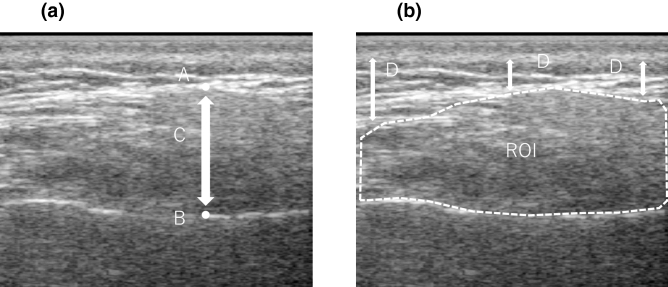
Ultrasound images were analyzed using the Image-J software version 1.49 (National Institutes of Health, Bethesda, MD), and the maximum distance from the exterior portion of the ramus to the masseteric fascia was measured as MMT (Fig. 3). When measuring the MMEI, the region of interest was set to include the entire masseter muscle (Fig. 3). Echo intensity is attenuated due to the influence of subcutaneous fat; therefore, the following correction calculation was performed:
Figure 3.
Masseter muscle evaluation by ultrasound diagnostic apparatus. (a) Masseter muscle thickness (MMT). (b) Masseter muscle echo intensity (MMEI) measurement. (A) Masseter muscle surface (B) Mandibular ramus (C) Masseter muscle thickness (D) subcutaneous fat thickness. ROI : region of interest.
The corrected masseter muscle echo intensity was used as the measured value10,21. Subcutaneous fat thickness was measured at three locations and the average of the three measurements was used for calculations.
Sample size
G * Power software version 3.1 (Kiel University) was used to calculate the sample size. The effect size was set to 0.8 in accordance with previous studies11,14 (d = 0.65, 0.88)22. When the α value was set to 0.05, the detection power was set to 0.8 and the effect size d to 0.8, and the required number of samples was 52. The number of dropouts was expected to be 8% for a total of 56 subjects.
Randomization
The sampling followed a randomized stratified block method that combined a stratified method (gender) and a block method (intervention, control). One dentist was in charge of the outcome measurement, while the participants who received the dentures and mouthpieces were trained by another dentist. In other words, the dentist who measured the outcome and the dentists who explained the allocation and intervention methods were different. Therefore, both the research participants and the dentists who measured the outcomes were blinded.
Statistical method
The Shapiro–Wilk test was performed for each measured value to confirm its normality.
Parametric (MA, rMMT, cMMT, rMMEI, cMMEI) and nonparametric (MOF) items were compared between the two groups using the two-sampled t test and the Mann–Whitney U test, respectively, before and after the intervention.
For each group comparison before and after the intervention, a paired t-test was used for parametric items and the Wilcoxon signed-rank test was used for nonparametric items.
A p value of <0.05 was considered statistically significant.
Results
Participants
Research participants were recruited from January 2019 to September 2020. Fifty-six participants were randomly assigned to two groups. Three dropped out of the study due to anxiety regarding hospital visits during the ongoing COVID-19 pandemic, and the final number of participants was 53 (Fig. 1). Table 1 shows the participants’ background characteristics in both groups.
Table 1.
Baseline characteristics of the participants (n = 53).
| Group | P value | ||
|---|---|---|---|
| Control (n = 27) | Intervention (n = 26) | ||
| Age, years, median(IQR) | 76.00 (10) | 73.27 (8) | |
| Gender | 0.908b | ||
| Male | 16 | 15 | |
| Female | 11 | 11 | |
| Body height, cm, mean(SD) | 156.52 (± 6.45) | 159.15 (± 7.51) | 0.176c |
| Body weight, kg, mean(SD) | 53.98 (± 9.85) | 59.10 (± 8.87) | 0.048*,c |
| BMI, kg/m2, mean(SD) | 21.93 (± 3.23) | 23.33 (± 2.82) | 0.099c |
| Eichner | 0.280b | ||
| B1 | 6 | 6 | |
| B2 | 6 | 10 | |
| B3 | 15 | 10 | |
| MA, mg/dL, mean (SD) | 181.19 (± 54.87) | 178.54 (± 62.81) | 0.871c |
| MOF, N, median (IQR) | 539.00 (553.1) | 608.45 (434.5) | 0.176a |
| rMMT, mm, mean (SD) | 7.87 (± 1.73) | 8.89 (± 2.16) | 0.064c |
| cMMT, mm (SD) | 10.33 (± 2.46) | 11.53 (± 2.61) | 0.088c |
| rMMEI, mean (SD) | 158.25 (± 17.89) | 149.09 (± 17.20) | 0.063c |
| cMMEI, mean (SD) | 135.39 (± 20.93) | 131.49 (± 16.16) | 0.452c |
IQR interquartile range, SD standard deviation, BMI body mass index, MA masticatory ability, MOF maximum occlusal force, rMMT masseter muscle thickness at rest, cMMT masseter muscle thickness during contraction, rMMEI masseter muscle echo intensity at rest, cMMEI masseter muscle echo intensity during contraction.
*p-value < 0.05.
aMann–whitney U test.
bPearson’s χ2 test.
cTwo sample t test.
Outcomes
At the baseline measurement stage, no significant differences were observed in any items, except for the body weight (Table 1). After the intervention, the intervention group showed a significantly greater improvement in the MOF (P = 0.001), MMT during contraction (cMMT) (P = 0.017), MMT at rest (rMMT) (P = 0.017), and MMEI during contraction (cMMEI) (P = 0.042) as compared to the control group. There was no significant difference in the MA and MMEI at rest (rMMEI) between the two groups (Table 2).
Table 2.
Comparison between the control (n = 27) and intervention (n = 26) groups before and after intervention.
| Baseline | p value | At 4 weeks post intervention | p value | |||
|---|---|---|---|---|---|---|
| Control (n = 27) | Intervention (n = 26) | Control (n = 27) | Intervention (n = 26) | |||
| MA, mg/dL, mean (SD) | 181.19 (± 54.87) | 178.54 (± 62.81) | 0.871a | 185.19 (± 60.92) | 197.92(± 52.89) | 0.421a |
| MOF, N, median (IQR) | 539.00 (553.1) | 608.45 (434.5) | 0.176b | 564.80(511.6) | 905.15(525.4) | 0.001*,b |
| rMMT, mm, mean (SD) | 7.87 (± 1.73) | 8.89 (± 2.16) | 0.064a | 7.69 (± 1.92) | 9.07 (± 2.16) | 0.017*,a |
| cMMT, mm, mean (SD) | 10.33 (± 2.46) | 11.53 (± 2.61) | 0.088a | 10.42 (± 2.68) | 12.65 (± 2.76) | 0.017*,a |
| rMMEI, mean (SD) | 158.25(± 17.89) | 149.09(± 17.20) | 0.063a | 156.30(± 17.62) | 149.28(± 18.02) | 0.158a |
| cMMEI, mean (SD) | 135.39(± 20.93) | 131.49(± 16.16) | 0.452a | 134.59(± 18.23) | 124.72(± 16.04) | 0.042*,a |
SD standard deviation, IQR interquartile range, MA masticatory ability, MOF maximum occlusal force, rMMT masseter muscle thickness at rest, cMMT masseter muscle thickness during contraction, rMMEI masseter muscle echo intensity at rest, cMMEI masseter muscle echo intensity during contraction.
*p-value < 0.05.
aTwo-sampled t test.
bMann–Whitney U test.
Significant improvements in the MOF (P < 0.001), cMMT (P = 0.003), cMMEI (P = 0.007), and MA (P = 0.007) were observed in the intervention group following intervention. In the control group, no improvement was observed in any of the measured values (Table 3).
Table 3.
Intra-group comparison in the control (n = 27) intervention (n = 26) groups before and after intervention.
| Control | p value | Intervention | p value | |||
|---|---|---|---|---|---|---|
| Baseline | Post intervention | Baseline | Post intervention | |||
| MA, mg/dL, mean(SD) | 181.19 (± 54.87) | 185.19 (± 60.92) | 0.549a | 178.54 (± 62.81) | 197.92 (± 52.89) | 0.007*,a |
| MOF, N, median(IQR) | 539.00 (553.1) | 564.80 (511.6) | 0.683b | 608.45 (434.5) | 905.15 (525.4) | 0.000*,b |
| rMMT, mm, mean(SD) | 7.87 (± 1.73) | 7.69 (± 1.92) | 0.280a | 8.89 (± 2.16) | 9.07 (± 2.16) | 0.220a |
| cMMT, mm, mean(SD) | 10.33 (± 2.46) | 10.42 (± 2.68) | 0.673a | 11.53 (± 2.61) | 12.65 (± 2.76) | 0.003*,a |
| rMMEI, mean(SD) | 158.25 (± 17.89) | 156.30 (± 17.62) | 0.373a | 149.09(± 17.20) | 149.28(± 18.02) | 0.940a |
| cMMEI, mean(SD) | 135.39 (± 20.93) | 134.59 (± 18.23) | 0.789a | 131.49(± 16.16) | 124.72(± 16.04) | 0.007*,a |
SD standard deviation, IQR interquartile range, MA masticatory ability, MOF maximum occlusal force, rMMT masseter muscle thickness at rest, cMMT masseter muscle thickness during contraction, rMMEI masseter muscle echo intensity at rest, cMMEI masseter muscle echo intensity during contraction.
*p-value < 0.05.
aPaired t test.
bWilcoxon signed-rank test.
Discussion
In this intervention study, the following observations were made: On performing isometric exercises using a mouthpiece, there was (1) an improvement in the oral function and (2) an improvement in the masseter muscle properties in older individuals with an Eichner B status who used dentures.
First, as a result of training, the oral function, especially MOF, improved. There are many reports on resistance training for limb muscles, which increases the muscle mass and strength23,24. It has been reported that a significant improvement in the MOF was achieved by resistance training in adults without missing teeth14. The masseter tissue is dominated by Type 1 muscle fibers and has a composition different from that of the quadriceps femoris, which has a large number of Type 2 muscle fibers25. Type 1 muscle fibers are more susceptible to disuse than to aging26. Tooth loss is also an independent factor associated with the MMT27. Furthermore, it has been reported that chewing exercises for older people with 24 or more remaining teeth improved the MOF28. In this study, we targeted older adults with missing teeth and found an improvement in the MOF, which was consistent with the findings of previous studies14,28.
The pre- and post-intervention MA differed significantly in the intervention group, but not in the control group. Since the masticatory ability and occlusal force are related29, improvement of occlusal force by isometric exercise may contribute to the improvement of the masticatory ability. However, the masticatory ability is also an important factor associated with the tongue function30, therefore the lack of significant difference in MA could be probably due to the target muscle of the training being the masseter, and not the tongue.
Second, an improvement in the masseter muscle properties was also observed. Significant improvements were observed in both the rMMT and the cMMT. It has been found that age-related changes strongly affect the muscle strength and muscle mass31. Muscle weakness is a risk factor for subsequent hospitalization and death32. Muscle strengthening is known to occur before muscle mass gain33. While muscle hypertrophy was said to occur after 6 weeks34, it has recently been reported to occur in the skeletal muscle (for e.g., the thigh muscle) from about 4 weeks35. In this study as well, a significant improvement in masseter muscle hypertrophy was observed at 4 weeks. One of the factors that causes muscle hypertrophy at a relatively early stage is the high sensitivity of the masseter muscle to testosterone. Testosterone promotes protein synthesis in the muscle36. In a study of rats, injection of testosterone increased the masseter muscle mass by 38%, which was reportedly more sensitive than other muscles37. Isometric exercise has been shown to significantly increase the testosterone levels38,39. The masseter may be a muscle that is more affected by isometric exercise as compared to the other muscles.
In this study, the cMMEI was also significantly improved. The higher the number, the more non-contractile tissues in the muscle, indicating a decrease in muscle quality. Previous studies in healthy older adults have shown a strong negative correlation between the cMMT and cMMEI9. It is considered that an improvement in the cMMT by isometric exercise also led to an improvement in the cMMEI.
This study has several limitations. First, it targeted older people in the Eichner B group with a limited number of missing teeth. In order to clarify the usefulness of isometric exercises for the masseter muscle, it will be necessary to conduct studies on patients with multiple missing teeth, including the Eichner C group. Second, the training period for this study was 1 month, and long-term effects were not considered. Tracking the long-term effects of isometric exercises is warranted in future research. Third, echo is used for muscle mass evaluation. It has been reported that there is a strong correlation between the muscle cross section in magnetic resonance imaging and the muscle thickness estimated in the B mode of echo at the same location; however, the gold standard for muscle mass evaluation is magnetic resonance imaging and computed tomography.
Significance and future implications
In this study, isometric exercise using a mouthpiece was shown to significantly improve occlusal force and masseter muscle properties (quantity and quality) in older people using Eichner B dentures. Masseter muscle hypertrophy was confirmed in a short span of 1 month. Therefore, it is possible to sufficiently improve and maintain oral function even in older individuals who are in the maintenance phase after the completion of prosthetic treatment. The possibility of self-management of oral function and masticatory muscle properties has been demonstrated in this study. This time, we have achieved good results in the research targeting the Eichner B group, and we would like to perform further studies targeting the C group in the future.
Acknowledgements
The authors are grateful to the staff of Avenue Dental Clinic for coordinating the interaction between the participants and researchers and their assistance in collecting participant data. We would like to thank Editage (https://www.editage.com) for English language editing.
Author contributions
S.T., K.Y. and H.T. designed the study. S.T. collected and analyzed the data. S.T., K.Ya., K. Yo., A. N., K.N., T.O., and H.T. interpreted the data. S.T. drafted the manuscript, and K.Y. and H.T. finalized the manuscript after revision. All authors have read and approved the final manuscript for submission.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Change history
4/21/2021
A Correction to this paper has been published: 10.1038/s41598-021-88765-9
References
- 1.Cruz-Jentoft AJ, Sayer AA. Sarcopenia. Lancet. 2019;393:2636–2646. doi: 10.1016/S0140-6736(19)31138-9. [DOI] [PubMed] [Google Scholar]
- 2.Nowjack-Raymer RE, Sheiham A. Association of edentulism and diet and nutrition in US adults. J. Dent. Res. 2003;82:123–126. doi: 10.1177/154405910308200209. [DOI] [PubMed] [Google Scholar]
- 3.Borie E, et al. Maximum bite force in elderly indigenous and non-indigenous denture wearers. Acta Odontol. Latinoam. 2014;27:115–119. doi: 10.1590/S1852-48342014000300003. [DOI] [PubMed] [Google Scholar]
- 4.Moynihan P, et al. Researching the impact of oral health on diet and nutritional status: methodological issues. J. Dent. 2009;37:237–249. doi: 10.1016/j.jdent.2008.12.003. [DOI] [PubMed] [Google Scholar]
- 5.Nowjack-Raymer RE, Sheiham A. Numbers of natural teeth, diet, and nutritional status in US adults. J. Dent. Res. 2007;86:1171–1175. doi: 10.1177/154405910708601206. [DOI] [PubMed] [Google Scholar]
- 6.Houston, D. K. et al. Dietary protein intake is associated with lean mass change in older, community-dwelling adults: the health, aging, and body composition (Health ABC) study. Am. J. Clin. Nutr.871, 50e5 (2008). [DOI] [PubMed]
- 7.Okamoto, N., Amano, N., Nakamura, T. & Yanagi, M. Relationship between tooth loss, low masticatory ability, and nutritional indices in the elderly: a cross-sectional study. B.M.C. Oral Health. 19, 110 (2019). [DOI] [PMC free article] [PubMed]
- 8.Raadsheer MC, van Eijden TM, van Ginkel FC, Prahl-Andersen B. Contribution of jaw muscle size and craniofacial morphology to human bite force magnitude. J. Dent. Res. 1999;78:31–42. doi: 10.1177/00220345990780010301. [DOI] [PubMed] [Google Scholar]
- 9.Yamaguchi K, et al. Factors associated with masseter muscle quality assessed from ultrasonography in community-dwelling elderly individuals: A cross-sectional study. Arch. Gerontol. Geriatr. 2019;82:128–132. doi: 10.1016/j.archger.2019.02.003. [DOI] [PubMed] [Google Scholar]
- 10.Young HJ, Jenkins NT, Zhao Q, Mccully KK. Measurement of intramuscular fat by muscle echo intensity. Muscle Nerve. 2015;52:963–971. doi: 10.1002/mus.24656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Melo ACM, Ledra IM, Vieira RA, Coró ER, Sartori IAM. Maximum bite force of edentulous patients before and after dental implant rehabilitation: Long-term follow-up and facial type Influence. J. Prosthodont. 2018;27:523–527. doi: 10.1111/jopr.12544. [DOI] [PubMed] [Google Scholar]
- 12.Müller F, et al. Implant-supported mandibular overdentures in very old adults: A randomized controlled trial. J. Dent. Res. 2013;92:154S–160S. doi: 10.1177/0022034513509630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.von der Gracht I, Derks A, Haselhuhn K, Wolfart S. EMG correlations of edentulous patients with implant overdentures and fixed dental prostheses compared to conventional complete dentures and dentates: A systematic review and meta-analysis. Clin. Oral Implants Res. 2017;28:765–773. doi: 10.1111/clr.12874. [DOI] [PubMed] [Google Scholar]
- 14.Thompson DJ, Throckmorton GS, Buschang PH. The effects of isometric exercise on maximum voluntary bite forces and jaw muscle strength and endurance. J. Oral Rehab. 2001;28:909–917. doi: 10.1046/j.1365-2842.2001.00772.x. [DOI] [PubMed] [Google Scholar]
- 15.Eichner K. Über eine Gruppeneintelung des lückengebisses für die prothetik. Deutsche Zahnarztliche Z. 1955;10:1831–1834. [Google Scholar]
- 16.Shiga H, et al. Comparison of two dental pre scale systems used for the measurement of occlusal force. Odontology. 2020;108:676–680. doi: 10.1007/s10266-020-00509-9. [DOI] [PubMed] [Google Scholar]
- 17.Takeshima T, Fujita Y, Maki K. Factors associated with masticatory performance and swallowing threshold according to dental formula development. Arch. Oral Biol. 2019;99:51–57. doi: 10.1016/j.archoralbio.2018.12.012. [DOI] [PubMed] [Google Scholar]
- 18.Serra, M. D., Duarte Gavião, M. B. & dos Santos Uchôa, M. N. The use of ultrasound in the investigation of the muscles of mastication. Ultrasound Med. Biol. 34, 1875–1884 (2008). [DOI] [PubMed]
- 19.Thoirs K, English C. Ultrasound measures of muscle thickness: Intra-examiner reliability and influence of body position. Clin. Physiol. Funct. Imaging. 2009;29:440–446. doi: 10.1111/j.1475-097X.2009.00897.x. [DOI] [PubMed] [Google Scholar]
- 20.Yoshiko A, et al. Effect of 12-month resistance and endurance training on quality, quantity, and function of skeletal muscle in older adults requiring long-term care. Exp. Gerontol. 2017;98:230–237. doi: 10.1016/j.exger.2017.08.036. [DOI] [PubMed] [Google Scholar]
- 21.Stock MS, et al. Echo intensity versus muscle function correlations in older adults are influenced by subcutaneous fat thickness. Ultrasound Med. Biol. 2018;44:1597–1605. doi: 10.1016/j.ultrasmedbio.2018.04.009. [DOI] [PubMed] [Google Scholar]
- 22.Cohen J. A power primer. Psycohol. Bull. 1992;112:155–159. doi: 10.1037/0033-2909.112.1.155. [DOI] [PubMed] [Google Scholar]
- 23.Wang E, et al. Impact of maximal strength training on work efficiency and muscle fiber type in the elderly: Implications for physical function and fall prevention. Exp. Gerontol. 2017;91:64–71. doi: 10.1016/j.exger.2017.02.071. [DOI] [PubMed] [Google Scholar]
- 24.Abe T, DeHoyos DV, Pollock ML, Garzarella L. Time course for strength and muscle thickness changes following upper and lower body resistance training in men and women. Eur. J. Appl. Physiol. 2000;81:174–180. doi: 10.1007/s004210050027. [DOI] [PubMed] [Google Scholar]
- 25.Monemi M, Eriksson PO, Eriksson A, Thornell LE. Adverse changes in fibre type composition of the human masseter versus biceps brachii muscle during aging. J. Neurol. Sci. 1998;154:35–48. doi: 10.1016/S0022-510X(97)00208-6. [DOI] [PubMed] [Google Scholar]
- 26.Cullins MJ, Connor NP. Alterations of intrinsic tongue muscle properties with aging. Muscle Nerve. 2017;56:E119–E125. doi: 10.1002/mus.25605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Yamaguchi, K. et al. Relationship of aging, skeletal muscle mass, and tooth loss with masseter muscle thickness. B.M.C. Geriatr.18, 67 (2018). [DOI] [PMC free article] [PubMed]
- 28.Kim MJ, et al. Effects of chewing exercises on the occlusal force and masseter muscle thickness in community-dwelling Koreans aged 65 years and older: A randomized assessor-blind trial. J. Oral Rehabil. 2020;47:1103–1109. doi: 10.1111/joor.13036. [DOI] [PubMed] [Google Scholar]
- 29.Kosaka T, et al. Factors influencing the changes in masticatory performance: The Suita study. JDR Clin. Trans. Res. 2018;3:405–412. doi: 10.1177/2380084418785863. [DOI] [PubMed] [Google Scholar]
- 30.Sagawa K, et al. Tongue function is important for masticatory performance in the healthy elderly: A cross-sectional survey of community-dwelling elderly. J. Prosthodont. Res. 2019;63:31–34. doi: 10.1016/j.jpor.2018.03.006. [DOI] [PubMed] [Google Scholar]
- 31.Goodpaster BH, et al. The loss of skeletal muscle strength, mass, and quality in older adults: The health, aging and body composition study. J. Gerontol. A. Biol. Sci. Med. Sci. 2006;61:1059–1064. doi: 10.1093/gerona/61.10.1059. [DOI] [PubMed] [Google Scholar]
- 32.Fried, L. P. et al. Cardiovascular Health Study Collaborative Research Group. Frailty in older adults: evidence for a phenotype. J. Gerontol. A. Biol. Sci. Med. Sci.56, M146–M156 (2001). [DOI] [PubMed]
- 33.Moritani T, DeVries HA. Neural factors versus hypertrophy in the time course of muscle strength gain. Am. J. Phys. Med. 1979;58:115–130. [PubMed] [Google Scholar]
- 34.Staron RS, et al. Skeletal muscle adaptations during early phase of heavy-resistance training in men and women. J. Appl. Physiol. 1994;76:1247–1255. doi: 10.1152/jappl.1994.76.3.1247. [DOI] [PubMed] [Google Scholar]
- 35.DeFreitas, J. M., Beck, T. W., Stock, M.S., Dillon, M.A. & Kasishke, P. R. 2nd. An examination of the time course of training-induced skeletal muscle hypertrophy. Eur. J. Appl. Physiol. 111, 2785–2790 (2011). [DOI] [PubMed]
- 36.Griggs RC, et al. Effect of testosterone on muscle mass and muscle protein synthesis. J. Appl. Physiol. 1989;66:498–503. doi: 10.1152/jappl.1989.66.1.498. [DOI] [PubMed] [Google Scholar]
- 37.Widmer CG, Morris-Wiman J. Limb, respiratory, and masticatory muscle compartmentalization: Developmental and hormonal considerations. Prog. Brain Res. 2010;187:63–80. doi: 10.1016/B978-0-444-53613-6.00005-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kraemer WJ, Ratamess NA. Hormonal responses and adaptations to resistance exercise and training. Sports Med. 2005;35:339–361. doi: 10.2165/00007256-200535040-00004. [DOI] [PubMed] [Google Scholar]
- 39.Vingren JL, et al. Testosterone physiology in resistance exercise and training: the up-stream regulatory elements. Sports Med. 2010;40:1037–1053. doi: 10.2165/11536910-000000000-00000. [DOI] [PubMed] [Google Scholar]