Abstract
An 81-year-old female presented with a loss of consciousness and a history of fever, dry cough, dyspnea, and conjunctivitis during 5 days ago. On initial physical examination, the laboratory examination revealed high levels of lactate dehydrogenase and creatinine concomitant severe thrombocytopenia. Moreover, the peripheral blood smear showed schistocytes 3%, suggesting thrombotic thrombocytopenic purpura (TTP). A ground-glass pattern was reported in the high-resolution computed tomography of the lung. A positive polymerase chain reaction was reported for coronavirus disease 2019 (COVID-19). After initiating treatment for COVID-19, the patient received fresh frozen plasma and 24-h electrocardiogram monitoring in the emergency department. As the patient was being prepared for transfer to another hospital for plasmapheresis treatment, cardiac arrest occurred again, and the patient passed away. This study highlights the atypical behavior of this virus over the course of the disease including TTP with conjunctivitis, which could vary from case to case.
Keywords: Conjunctivitis, coronavirus disease 2019, thrombocytopenia
Introduction
In December 2019, in Wuhan, China, an infection occurred affecting the respiratory system that instigated a pandemic and affected health-care systems around the world. The responsible virus is a novel coronavirus and has been named the new severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2).[1,2] The disease presents more commonly with a febrile illness associated with respiratory symptoms such as cough and dyspnea, but it also has other atypical manifestations.[3] Some patients that have been diagnosed with coronavirus disease 2019 (COVID-19) have no respiratory involvement but may present with an afebrile illness, thrombocytopenia and bleeding tendency, diarrhea, confusion, renal dysfunction, and ocular manifestations.[3,4]
Although severe thrombocytopenia is rare, mild thrombocytopenia (platelet counts of 100–150 × 109/L) can be encountered in COVID-19.[5] There are different explanations for COVID-19-associated thrombocytopenia: the direct invasion of bone marrow, cytokine release persuading to hemophagocytic lymphohistiocytosis, autoimmune devastation of platelets in peripheral blood, and augmented platelet consumption as a result of thrombi in the microvasculature.[6]
A recent thrombotic thrombocytopenic purpura (TTP) case with COVID-19 has been reported based on the presence of microangiopathic hemolytic anemia and severe thrombocytopenia.[7]
TTP was first described by Moschowitz in 1925 as a disease described by the pathological findings of hyaline thrombi in many organs.[8] The classic picture of the disease includes the presence of thrombocytopenia, microangiopathic hemolytic anemia, neurologic abnormalities, fever, and renal disease. Unexplained thrombocytopenia and microangiopathic hemolytic anemia are the two essential criteria to confirm the diagnosis of thrombotic microangiopathy and initiating treatment.[9] In this article, taking into account the above definitions, we have described a case of COVID-19, presenting with TTP concomitant with conjunctivitis.
Case Report
An 81-year-old female was admitted to the Emergency Department of Khorshid Hospital in Isfahan, Iran, with a loss of consciousness and a history of fever, dry cough, and dyspnea over the past few days. The patient had attended the ophthalmology department 5 days before with a red eye and had received treatment for conjunctivitis. Over the following days, she had experienced anorexia, vomiting, and progressive loss of consciousness. She had been tested for COVID-19 before admission to the hospital, and a positive polymerase chain reaction (PCR) test was reported.
She had a history of hypertension and was using losartan/hydrochlorothiazide (50/12.5 mg daily), chlordiazepoxide tablets (2.5 mg daily), and Vitamin B6.
The initial physical examination revealed a body temperature of 37°C, oxygen saturation of 93% on air, respiratory rate of 22 breaths/min, blood pressure of 166/110 mmHg, and the pulse was 96 bpm. The laboratory results were as below: white blood cell = 145,000/mm 3, red blood cell = 2.47 × 106/μL, hemoglobin = 7.2 mg/dl, hematocrit = 23.5%, lactate dehydrogenase = 2237 unit/L, platelet = 52,000/mm 3, and creatinine (Cr) levels = 8.9–9.1 mg/dL.
After admission to Khorshid Hospital, another PCR test was performed to confirm the previous findings, and it was positive again for COVID-19. A ground-glass pattern was reported in the high-resolution computed tomography (CT) of the lung. Spiral multislices showed diffuse bilateral ground-glass opacity and crazy paving opacity with peripheral and peribronchovascular distribution, a pattern highly suggestive of COVID-19-associated pneumonia [Figure 1]. In a spiral multislice brain CT scan, irregular hypodensities in the deep white matter and centrum semiovale were detected that suggested small vessel disease. Cortical sulci and Sylvian fissures appeared prominent and indicated brain atrophy.
Figure 1.
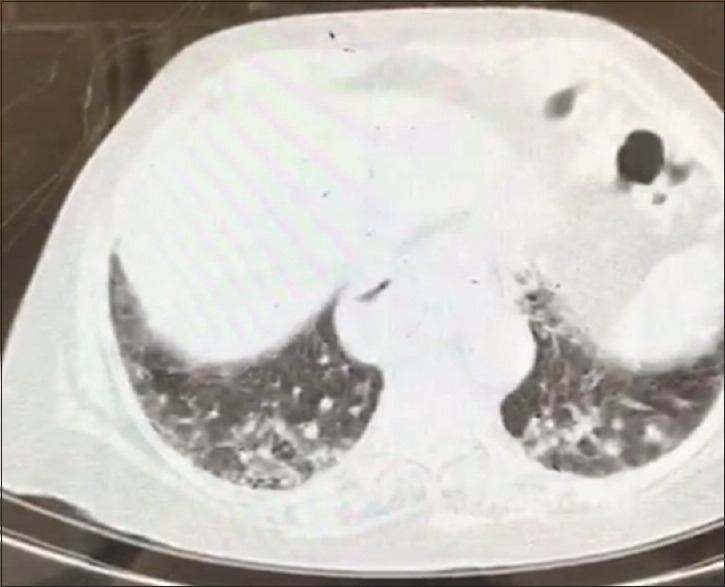
Ground-glass view in lung computed tomography showing positive for COVID-19
Upon admission, the patient was immediately treated with nasal oxygen (3–5 L/min) and amlodipine 5 mg oral. Based on the hospital protocol, treatment for COVID-19 infection was initiated: hydroxychloroquine 200 mg tablet twice a day, azithromycin 500 mg daily, and ceftriaxone 1 g intravenous daily. The peripheral blood smear showed schistocytes 3% [Figure 2] without platelet aggregation, suggesting TTP. An infusion of 500 mg methylprednisolone and ISO group fresh frozen plasma was commenced and electrocardiogram monitoring in the emergency department. Unfortunately, 45 min later, the patient developed ventricular tachycardia and subsequently suffered a cardiac arrest. Cardiopulmonary resuscitation was performed immediately, and cardiac shock was given. The cardiac rhythm returned to normal after approximately 30 min of effort. As the patient was being prepared for transfer to another hospital for plasmapheresis treatment, cardiac arrest occurred again, and the patient passed away.
Figure 2.
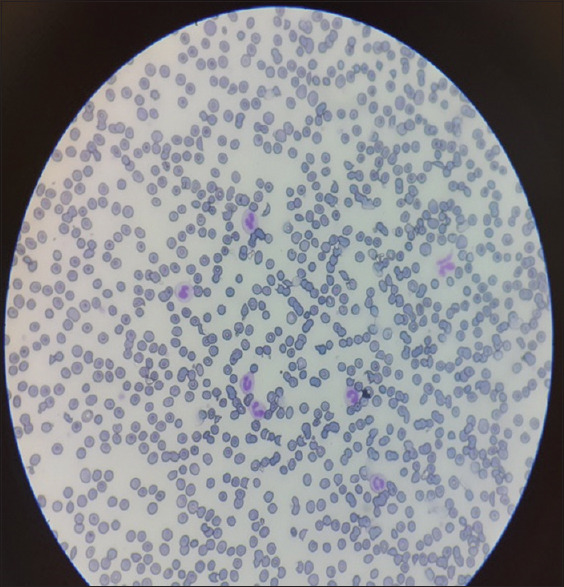
Peripheral blood showing schistocytes, characteristic of microangiopathic hemolytic anemia
Discussion
In this study, we have reported a case of COVID-19 disease presented with TTP and conjunctivitis. Thrombocytopenia in COVID-19 patients may be caused by disseminated intravascular coagulation (DIC), may be sepsis, or may be drug induced.[10] A recent case series suggested that immune thrombocytopenia may also be associated with COVID-19 infection.[10,11]
Thrombocytopenia is a risk factor for increased morbidity and mortality in patients infected with the new SARS-CoV-2 (COVID-19 infection).[12] Other studies have indicated that COVID-19 can affect the hematopoietic system, the most common representation of which could be significant lymphopenia.[9,13]
In this case, we observed decreasing levels of platelets, which we assume may be a result of an immunologic reaction seen in many viral infections [14] and has been previously suggested to occur as an autoimmune response in COVID-19. Abnormal hematopoiesis and platelet aggregation in the lungs and increased platelet consumption can also be a direct effect of the virus on the bone marrow.[6,15] TTP was confirmed in this case by the presence of microangiopathic hemolytic anemia and severe thrombocytopenia. Assuming a direct causal association between COVID-19 and TTP is difficult because of several other potential causes, for example, the coagulation activation by COVID-19 infection, leading to DIC and subsequent thrombocytopenia. Furthermore, drug reactions to treatments for COVID-19, including heparin, azithromycin, and hydroxychloroquine, can cause thrombocytopenia.[12]
To the best of our knowledge, there has been only one case reported with TTP,[7] and this is the first report of a COVID-19 infection with TTP and concomitant conjunctivitis. The concomitance of thrombocytopenia and conjunctivitis has been observed in many viruses.[16]
Conclusion
It is important to be aware of this severe complication of the COVID-19 viral infection to prompt immediate diagnosis and treatment. TTP is a medical emergency that is usually fatal if exchange plasmapheresis is not initiated early. Failure of timely diagnosis may have fatal consequences.
The chronological sequence in this case suggests, but does not prove, that COVID-19 was a causal factor in this patient's thrombocytopenia. This study highlights the atypical behavior of this virus over the course of the disease, which could vary from case to case. During the current epidemic of COVID-19, it appears to be important to exclude a diagnosis of COVID-19 infection in a patient with thrombocytopenia.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given her consent for her images and other clinical information to be reported in the journal. The patient understands that her name and initials will not be published, and due efforts will be made to conceal identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
We are particularly grateful for the assistance given by the clinical informationist research group. This group is a part of the Health Information Technology Research Center at Isfahan University of Medical Sciences (Isfahan, Iran).
References
- 1.Wang C, Horby PW, Hayden FG, Gao GF. A novel coronavirus outbreak of global health concern. Lancet. 2020;395:470–3. doi: 10.1016/S0140-6736(20)30185-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization. Coronavirus Disease 2019 (COVID-19): Situation Report, 72 World Health Organization. 2020 [Google Scholar]
- 3.Zhang JJ, Dong X, Cao YY, Yuan YD, Yang YB, Yan YQ, et al. Clinical characteristics of 140 patients infected with SARS-CoV-2 in Wuhan, China. Allergy. 2020;75:1730–41. doi: 10.1111/all.14238. [DOI] [PubMed] [Google Scholar]
- 4.Tin SS, Wiwanitkit V. Uncommon atypical presentations of COVID-19: Important and should not be under recognized! J Health Sci Med Res. 2020;38:153–8. [Google Scholar]
- 5.Fan BE, Chong VC, Chan SS, Lim GH, Lim KG, Tan GB, et al. Hematologic parameters in patients with COVID-19 infection. Am J Hematol. 2020;95:E131–4. doi: 10.1002/ajh.25774. [DOI] [PubMed] [Google Scholar]
- 6.Xu P, Zhou Q, Xu J. Mechanism of thrombocytopenia in COVID-19 patients. Ann Hematol. 2020;99:1205–8. doi: 10.1007/s00277-020-04019-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Albiol N, Awol R, Martino R. Autoimmune thrombotic thrombocytopenic purpura (TTP) associated with COVID-19. Ann Hematol. 2020;99:1673–4. doi: 10.1007/s00277-020-04097-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Moschcowitz E. An acute febrile pleiochromic anemia with hyaline thrombosis of the terminal arterioles and capillaries; an undescribed disease. Am J Med. 1952;13:567–9. doi: 10.1016/0002-9343(52)90022-3. [DOI] [PubMed] [Google Scholar]
- 9.George JN. How I treat patients with thrombotic thrombocytopenic purpura: 2010. Blood. 2010;116:4060–9. doi: 10.1182/blood-2010-07-271445. [DOI] [PubMed] [Google Scholar]
- 10.Bomhof G, Mutsaers PG, Leebeek FW, Te Boekhorst PA, Hofland J, Croles FN, et al. COVID-19-associated immune thrombocytopenia. Br J Haematol. 2020;190:e61–4. doi: 10.1111/bjh.16850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zulfiqar AA, Lorenzo-Villalba N, Hassler P, Andrès E. Immune thrombocytopenic purpura in a patient with COVID-19. N Engl J Med. 2020;382:e43. doi: 10.1056/NEJMc2010472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Liu Y, Sun W, Guo Y, Chen L, Zhang L, Zhao S, et al. Association between platelet parameters and mortality in coronavirus disease 2019: Retrospective cohort study. Platelets. 2020;31:490–6. doi: 10.1080/09537104.2020.1754383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Terpos E, Ntanasis-Stathopoulos I, Elalamy I, Kastritis E, Sergentanis TN, Politou M, et al. Hematological findings and complications of COVID-19. Am J Hematol. 2020;95:834–47. doi: 10.1002/ajh.25829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hottz ED, Bozza FA, Bozza PT. Platelets in immune response to virus and immunopathology of viral infections. Front Med (Lausanne) 2018;5:121. doi: 10.3389/fmed.2018.00121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lippi G, Plebani M, Henry BM. Thrombocytopenia is associated with severe coronavirus disease 2019 (COVID-19) infections: A meta-analysis. Clin Chim Acta. 2020;506:145–8. doi: 10.1016/j.cca.2020.03.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chraïbi S, Najioullah F, Bourdin C, Pegliasco J, Deligny C, Résière D, et al. Two cases of thrombocytopenic purpura at onset of Zika virus infection. J Clin Virol. 2016;83:61–2. doi: 10.1016/j.jcv.2016.08.299. [DOI] [PubMed] [Google Scholar]


