Abstract
Background: Plantar fasciitis is a common cause of plantar pain which is prevalent among adults. Conservative tractions, invasive injections, shock therapies and also surgical procedures are known as beneficial methods in non-responsive cases. Here we evaluated and compared the injection of platelet rich plasma (PRP) and usage of extracorporeal shockwave therapy (ESWT) in pain reduction in patients with chronic plantar fasciitis. Methods: This is a randomized clinical trial that was performed in 2017-2020 on patients with chronic plantar fasciitis who did not respond to conservative therapies. A total number of 110 patients with plantar fasciitis were entered based on inclusion and exclusion criteria. Patients were then divided into two groups. The pain of patients was measured using visual analogue scale (VAS) before interventions. The first group underwent PRP injections while the second group underwent ESWT using Shock Master 500. Patients were visited 2, 4, 8, 12, 16, and 24 weeks after interventions and the pain scores were noted using VAS. Results: Data of 104 patients were analyzed. Initial VAS scores of patients were also analyzed. These data indicated no significant differences between the pains of patients before interventions (P = 0.413). Pain evaluations in 2, 4, 8, 12, 16, and 24 weeks after interventions with controlling age and sex showed significantly reduced VAS scores in both groups after interventions (P = 0.002). We should also note that pain in the PRP group reduced more than ESWT group and this difference was also significant (P = 0.001). Conclusion: Here we showed that PRP injections and ESWT are both beneficial in pain amelioration in patients with chronic plantar fasciitis. We also indicated that PRP injections were associated with better pain reduction results compared to ESWT.
Keywords: Chronic fasciitis, platelet rich plasma, shockwave therapy, pain
Introduction
Plantar fasciitis is one of the most common causes of foot plantar pain [1]. Clinical presentations of plantar fasciitis could be a severe and sudden pain in the medial side of the heel especially early in the morning or the first gait after long term sitting [2]. Plantar fascia consists of connective tissue supporting the plantar arch and especially the longitudinal arch via attracting the stresses [3]. Although the exact histopathology and pathogenesis of plantar fasciitis remain unknown, studies revealed no significant inflation but on the other hand, myxoid degeneration, collagen necrosis, small ruptures and angiofibroblastic hyperplasia exist [4]. Different risk factors have also been reported for plantar fasciitis including higher body mass index (BMI > 25), anatomical disorders such as heel curvatures, limb discrepancy, long term standing and reduction in ankle dorsiflexion [5,6].
Different therapeutic methods have been evolved for plantar fasciitis including conservative tractions, invasive injections, shock therapies and also surgical procedures in non-responsive cases [7,8]. Extracorporeal shockwave therapy (ESWT) is a novel treatment method which might have beneficial effects on plantar fasciitis [9]. This method is associated with controlling the injuries via increasing the growth factor and is suggested for patients who do not respond to other therapies. There have been studies showing the effectiveness of ESWT in injuries to Achilles tendon, medial tibial stress syndrome and eroded tendons [10]. ESWT is performed using two methods: radial extracorporeal shockwave therapy (rESWT) and focused on extracorporeal shockwave therapy (FESWT) [11]. Studies have suggested that rESWT is more effective than FESWT due to the wider affected area especially in patients with tendinopathy [12]. Some other studies showed that both rESWT and FESWT are effective and have no preference for each other [13]. Patients with plantar fasciitis experience pain in a region and as a result, it is assumed that rESWT could have more beneficial effects.
Platelet rich plasma (PRP) is also another therapeutic method for orthopedic inflammatory diseases [14]. PRP is a part of autologous plasma with higher amounts of platelets and variable growth factors. PRP is mainly used in chronic situations that are unresponsive to other medical therapies [15]. PRP injections to affected area cause initiation of revival procedures via different growth factors. Recent studies have indicated that PRP is effective in treatments of plantar fasciitis but they have focused on signs and symptoms of the disease. Based on the results of former studies, usage of PRP was associated with improvements in clinical symptoms of plantar fasciitis that was unresponsive to usual medical treatments [16,17]. These studies have indicated that pain amelioration as the most important treatment outcome was resulted by PRP injections [18]. On the other hand, various studies declared that ESWT, that is a non-invasive therapy, is appropriate for plantar fasciitis treatments. It has been also declared that ESWT is more effective and beneficial than corticosteroid administration [19-21].
So far, no previous study has evaluated and compared the effects of ESWT usage and PRP injections in patients with plantar fasciitis. The novelty the current study is that we performed a randomized clinical trial for the first time to compare the PRP injection and ESWT administration for treatment of refractory plantar fasciitis.
Methods
Study design
This is a randomized clinical trial that was performed in 2017-2020 in Imam Khomeini hospital and Avisina clinic in Tehran. The study population consisted of patients with plantar fasciitis who did not respond to conservative therapies. The current study was approved by the Research Committee of Tehran University of Medical Sciences and the Ethical committee has confirmed it.
Inclusion and exclusion criteria
Our inclusion criteria were: 1. Patients older than 18 years. 2. Presence of pain in anterior-medial calcaneal tuberosity. 3. Normal bone anatomy. 4. Presence of pain less than 18 months. 5. Unresponsive to conservative therapies for at least 3 months (including the use of non-steroidal anti-inflammatory drugs (NSAID) and use of Ice Pack). The exclusion criteria were: surgery and interventions on the ipsilateral knee or ankle, previous history of injecting blood products such as PRP, injection of steroids or use of shock waves in the heel or Achilles tendon, inflammatory arthritis, osteoarthritis of the foot and knee, spondylitis ankylosans, psoriatic arthritis, reiter’s syndrome, rheumatoid arthritis, neurological abnormalities, infectious skin diseases or history of any infection in the foot in the past 3 months, pregnancy, malignancy, blood disorders, signs or symptoms of Radiculopathy, Tarsal tunnel syndrome and Sinus tarsi syndrome.
Study population
The study population was calculated using statistical formulas and according to sample size calculation, we considered 50 patients in each group. A total number of 110 patients with plantar fasciitis were entered based on inclusion and exclusion criteria. We should note that written informed consent was taken from all patients. All patients were examined by an expert orthopedic surgeon. Patients were randomly divided into 2 groups using SPSS software. The patients in the first group were assigned to PRP injection method and the second group of patients were assigned to ESWT technique.
Measuring tools
Foot magnetic resonance imaging (MRI) was requested for all patients to rule out the stress fractures and other bone abnormalities. We should also note that written patient’s informed consents were taken from participants. Patients were then divided into two groups. The pain of patients was measured using visual analogue scale (VAS) before interventions. This scale is a validated, subjective measure for acute and chronic pain. Scores are recorded by making a handwritten mark on a 10-cm line and also is scored from 0 (meaning “no pain”) to 10 (“worst pain”) [22]. Pain was considered as our primary research indicator while treatment time and age were secondary research indicators. Patients were divided into two groups randomly using Random Allocation Software. Each group contained 55 patients.
Study procedure
The first group underwent PRP injections. PRP preparation was performed as follows: 40 ccs of complete blood was taken from basilic or antecubital vein and was transferred to vacuum sterile test tubes containing 3.8 sodium citrate (BD Vacutainer; Becton, Diskinson and Company, NJ) as anti-coagulant. Blood samples were transferred to the laboratory and centrifuged for 10 minutes with 1800 rotations per minute (Heraeus Megafug 1.0R; Fisher Scientific, Waltham, MA). As a result, blood cells were divided. The upper plasma layer was extracted into 50 ml polypropylene cone tubes (Falcon; Fisher Scientific, Corning, NY). These samples were also centrifuged for 12 minutes with 3400 rotations per minute. PRP was then extracted from tubes. 3 ml of PRP was injected in vacuum sterile test tubes without anti-coagulants and the rest were transferred for platelet counting tests. Before PRP injections, platelet activity should be induced by adding 0.45 ml of calcium gluconate. Activated PRP was aspirated with a 5 ml syringe and injected along with 2 ml Lidocaine into the plantar fascia. All patients were instructed in exercise programs that included stretching the plantar fascia while the patient was sitting during exercise, pulling the toes with one hand and pulling the injured foot over the bone of the other foot. According to the instructions, they exercised three times a day, 10 times for 10 seconds each time.
The second group of patients underwent ESWT using Shock Master 500 (ApsuNInc; Gymnauniphy, NV, Belgium). As the shock wave energy passes through the tissue, ultrasound waves (Accuvin Vio, Samsung Medison, Seoul, South Korea) were used to observe the movements and depth of the therapeutic position before ESWT. This issue is due to the increase in the effectiveness of the treatment. The patients were in supine position and ESWT was administered without local anesthesia. The energy was applied vertically with a depth of 15 mm, the pressure of 1500 bar, the resistance of 4 Hz and energy of 0.089 MJ/ml until pain threshold. This procedure was performed once a week for 3 weeks. The patient was allowed to rest for 30 minutes on the bed after ESWT administration and was allowed to perform daily activities. No treatments were suggested for patients and Achilles and plantar tendon stretching movements were initiated 6 months after the last session of ESWT. The patient stretched the Achilles tendon by placing both hands against the wall, pulling the affected leg back, and then bending the knee while standing upright, stretching the affected leg. The patient had to sit on a chair, place the affected part of the foot above the knee of the opposite foot, and then do a dorsiflexion stretch for the plantar fascia.
Follow-up and statistical analysis
Patients were visited 2, 4, 8, 12, 16 and 24 weeks after interventions and the pain scores were noted using VAS. Data were analyzed in SPSS software (version 25, IBM Corporation, Armonk, NY). P < 0.05 was considered as a significance threshold. Qualitative variables were compared using X^2 and quantitative variables were compared using Paired T-test. Quantitative variables had a normal distribution and a standard deviation was presented and P-value < 0.05 was considered as the significance threshold.
Results
Study population
Here in the present study, 110 patients were included and divided into 2 groups each containing 55 patients. 6 patients were excluded due to neurologic abnormalities (1 patient), previous history of blood transfusion within the past 2 months (4 patients) and lack of proper follow-ups (1 patient). The CONSORT diagram of the present study is illustrated in Figure 1. Data of 104 patients were analyzed.
Figure 1.
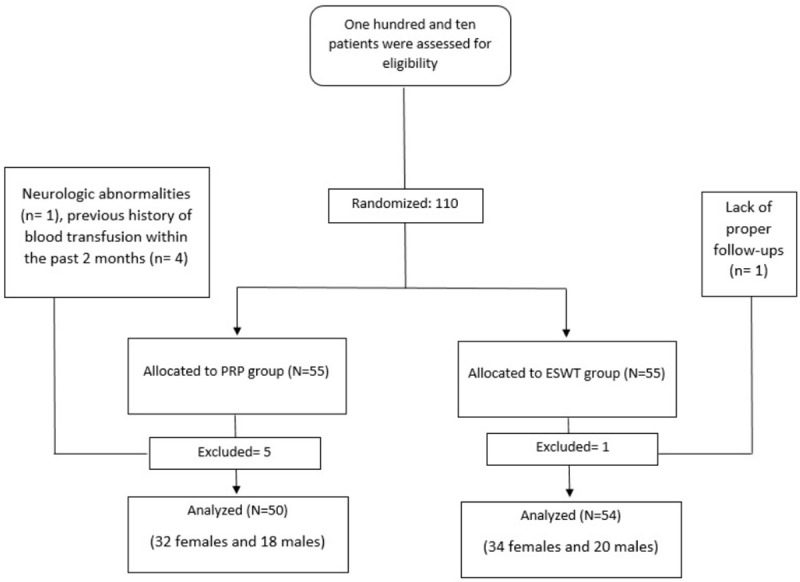
CONSORT diagram of patients.
Demographic data
The first group that received PRP treatments consisted of 32 females and 18 males and the second group consisted of 34 females and 20 males. The initial analysis indicated that the mean age of the first group was 44.58 ± 4.3 and the mean age of the second group was 44.23 ± 5.8. We showed no significant differences between the two groups regarding age (P = 0.820) and sex (P = 0.751). Analysis of past medical histories of patients also showed no significant differences between the two groups (P = 0.744).
Pain assessments
Initial VAS scores of patients were also analyzed. These data indicated no significant differences between the pains of patients before interventions (P = 0.413). Pain evaluations in 2, 4, 8, 12, 16 and 24 weeks after interventions with controlling age and sex showed significantly reduced VAS scores in both groups after interventions (P = 0.002). We should also note that pain in the PRP group reduced more than the ESWT group and this difference was also significant (P = 0.001) (Table 1; Figures 2 and 3).
Table 1.
Pain scores in patients
| Evaluation time | Pain in PRP group using VAS score (mean ± SD) | Pain in ESWT group using VAS score (mean ± SD) | P-value |
|---|---|---|---|
| 0 | 6.23 ± 1.4 | 6.20 ± 1.3 | 0.512 |
| After 2 weeks | 5.40 ± 1.1 | 5.81 ± 1.3 | 0.413 |
| After 4 weeks | 4.67 ± 1.2 | 4.97 ± 1.1 | 0.072 |
| After 8 weeks | 3.20 ± 1.1 | 4.13 ± 0.9 | 0.042 |
| After 16 weeks | 2.87 ± 0.8 | 3.40 ± 0.8 | 0.001 |
| After 24 weeks | 1.40 ± 0.8 | 2.55 ± 0.6 | 0.001 |
| P-value | 0.001 | 0.001 |
Figure 2.
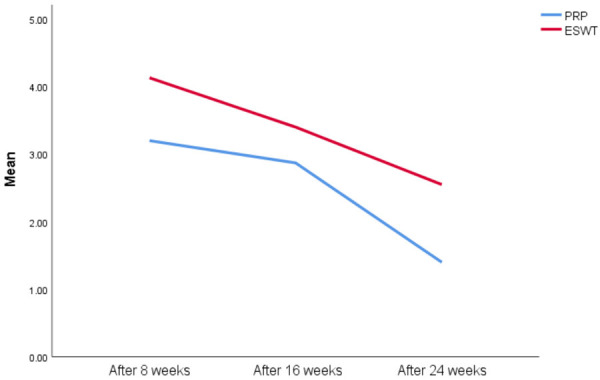
Comparison of VAS score in both groups.
Figure 3.
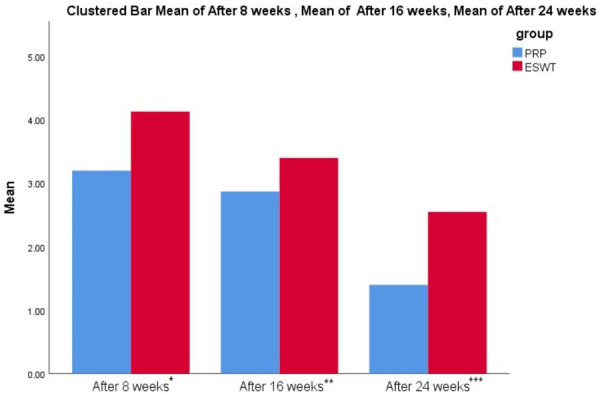
Different VAS scores within 24 weeks. *Pain in PRP group was significantly lower than ESWT group (3.20 ± 1.1 vs. 4.13 ± 0.9, P = 0.042). **Pain in PRP group was significantly lower than ESWT group (2.87 ± 0.8 vs. 3.40 ± 0.8, P = 0.001). ***Pain in PRP group was significantly lower than ESWT group (1.40 ± 0.8 vs. 2.55 ± 0.6, P = 0.001).
Analysis using repeated measures ANCOVA indicated that there was a significant difference between the results of repeated measurements in the PRP group. These results are indicated in Table 2.
Table 2.
Repeated measures ANCOVA test results
| Source of changes | Sum of squares | Degree of freedom | F distribution | P-value |
|---|---|---|---|---|
| Time | 27.111 | 2.638 | 4.608 | 0.006 |
| Gender interaction and repetition time | 1.352 | 2.638 | 0.230 | 0.824 |
| Age interaction and repetition time | 4.144 | 2.638 | 0.704 | 0.442 |
| Interaction of repetition time and group | 26.504 | 2.638 | 4.505 | 0.004 |
| Error | 258.849 | 116.072 |
Side effects
Evaluation of complications in two groups showed that 14 patients in ESWT had irritations and 6 patients in PRP group had mild localized reactions. But no significant differences were observed among the two groups (P = 0.108).
Discussion
In the current study, we indicated that the pain of the patients reduced significantly following both PRP and ESWT treatments. We also showed that the pain reduction was more among patients treated with PRP compared to ESWT method. The results of the present study, by comparing the mean pain score of plantar fasciitis between PRP and ESWT treatments with control of age and sex variables showed that the difference between the two treatments was significant. Regarding the mean values of both methods during the treatment period, the PRP method caused more pain reduction than ESWT. So far, very few studies have evaluated and compared the effectiveness of PRP injection and ESWT in patients with chronic plantar fasciitis.
The efficacy of ESWT has been indicated in previous studies [23]. In a study by Dastgir in Ireland in 2004, 70 feet with chronic plantar fasciitis were examined using ESWT. Significant pain improvement was reported in patients [24]. In a meta-analysis by Zhiyun and colleagues in 2013, they showed that usage of ESWT is associated with beneficial results and pain improvements in patients with chronic plantar fasciitis who are also unresponsive to routine conservative treatments [25]. These studies showed significant efficacy of ESWT in patients which is in line with our findings. The usage of various techniques has been discussed in previous studies. In the present study, we compared the two effective methods in reducing pain in plantar fasciitis. The use of PRP in orthopedic interventions has recently become an interesting technique which is indicated to be associated with beneficial results. Based on the present study, we showed that pain reduction following PRP injections as significant. There were also mild localized reactions in some patients but no serious discontinuing complications were observed. As a result, we assume that this method is safe and could be used in patients with plantar fasciitis.
In another meta-analysis by Hsiao and colleagues in 2015, data of 10 clinical trials and 604 patients with chronic plantar fasciitis were analyzed. They showed that injection of autologous blood-derived products (ABPs) following corticosteroid injections was the most effective therapeutic method. They also declared that ESWT was as useful and efficient as ABPs and caused pain improvements within 6 months but PRP as a subgroup of ABPs was considered more efficient than ESWT [26]. These results were in line with our findings emphasizing the effectiveness of PRP in patients with chronic plantar fasciitis. In the current study, we measured the pain of patients using VAS score and showed a significant improvement in the pain of patients who were treated with PRP method. We believe that pain is the most important symptom of plantar fasciitis. Based on recent guidelines, most of the physicians should concentrate on pain reduction in patients with plantar fasciitis by the means of analgesics that in turn could lead to various complications. Using the PRP technique was associated with significantly reduced pain that could also influence every aspect of a patient’s life. The Usage of PRP has been shown to be more efficient than corticosteroid injections in a study by Tiwari and Bhargava in 2013. They evaluated 60 patients within 6 months after corticosteroid and PRP injections and reported that the PRP method had better pain amelioration results [27].
In 2017, a clinical trial was conducted by Acosta-Olivo and colleagues on 32 patients with chronic plantar fasciitis that did not respond to conservative treatments. They compared the results of PRP and corticosteroid injections in patients and reported that both methods led to significant pain reduction but no significant differences could be observed between two methods [28]. On the other hand, Martinelli and others reported that PRP injections in 14 patients were associated with significant pain improvements and no complications [29]. The same results were reported by O’Malley and colleagues that investigated 23 patients with chronic plantar fasciitis [30]. We believe that such differences between studies could be due to variations in study populations and follow-up durations. A key point of our study was that we evaluated and compared the results of two therapeutic methods on 104 patients. The present study supports the usage of PRP in patients with chronic fasciitis but furthermore, we assume that more studies might be required.
Based on orthopedic guidelines, refractory plantar fasciitis should be treated with interventional therapies or advanced medical treatments to reduce the patient’s pain. These therapies include surgical treatments, advanced medical treatments (such as PRP) and physiotherapy (such as ESWT). Each of these methods is associated with advantages and disadvantages. Patients with refractory plantar fasciitis that have been involved with long-term medical treatments may have higher compliance with physiotherapy and physicians also suggest these therapies. Based on the results of our study, the usage of PRP had better therapeutic results compared to ESWT with no significant differences regarding complications of both therapies. These results could change the insight of physicians and also could bring appropriate treatment results for patients. The combination of two methods could also have better therapeutic results but evaluation of these results and also complications require further studies. The limitations of the present study was that we could not evaluate the effects of previous and also the effects of analgesics used by patients. We had also limitation in long term follow up of patients.
Conclusion
Here in the present study, we showed that PRP injection is a beneficial and efficient method for reducing the pain in plantar fasciitis and is associated with significantly reduced pain compared to ESWT. The use of ESWT in patients was also associated with significant pain amelioration but we indicated that pain reduction following PRP injection is significantly more than ESWT method. These findings were in line with previous studies but we also believe that further evaluations especially about the quality of life in patients and other related symptoms might be required.
Disclosure of conflict of interest
None.
References
- 1.Wearing SC, Smeathers JE, Urry SR, Hennig EM, Hills AP. The pathomechanics of plantar fasciitis. Sports Med. 2006;36:585–611. doi: 10.2165/00007256-200636070-00004. [DOI] [PubMed] [Google Scholar]
- 2.Tahririan MA, Motififard M, Tahmasebi MN, Siavashi B. Plantar fasciitis. J Res Med Sci. 2012;17:799. [PMC free article] [PubMed] [Google Scholar]
- 3.McPoil TG, Martin RL, Cornwall MW, Wukich DK, Irrgang JJ, Godges JJ. Heel pain-plantar fasciitis. J Orthop Sports Phys Ther. 2008;38:A1–A18. doi: 10.2519/jospt.2008.0302. [DOI] [PubMed] [Google Scholar]
- 4.Neufeld SK, Cerrato R. Plantar fasciitis: evaluation and treatment. J Am Acad Orthop Surg. 2008;16:338–346. doi: 10.5435/00124635-200806000-00006. [DOI] [PubMed] [Google Scholar]
- 5.Werner RA, Gell N, Hartigan A, Wiggerman N, Keyserling WM. Risk factors for plantar fasciitis among assembly plant workers. PM R. 2010;2:110–116. doi: 10.1016/j.pmrj.2009.11.012. [DOI] [PubMed] [Google Scholar]
- 6.Lee HS, Choi YR, Kim SW, Lee JY, Seo JH, Jeong JJ. Risk factors affecting chronic rupture of the plantar fascia. Foot Ankle Int. 2014;35:258–263. doi: 10.1177/1071100713514564. [DOI] [PubMed] [Google Scholar]
- 7.Cardenuto RF. Talalgia: plantar fasciitis. Rev Bras Ortop. 2014;49:213–217. doi: 10.1016/j.rboe.2014.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kudo P, Dainty K, Clarfield M, Coughlin L, Lavoie P, Lebrun C. Randomized, placebo-controlled, double-blind clinical trial evaluating the treatment of plantar fasciitis with an extracoporeal shockwave therapy (ESWT) device: a North American confirmatory study. J Orthop Res. 2006;24:115–123. doi: 10.1002/jor.20008. [DOI] [PubMed] [Google Scholar]
- 9.Gerdesmeyer L, Frey C, Vester J, Maier M, Lowell W Jr, Weil L Sr, Russlies M, Stienstra J, Scurran B, Fedder K. Radial extracorporeal shock wave therapy is safe and effective in the treatment of chronic recalcitrant plantar fasciitis: results of a confirmatory randomized placebo-controlled multicenter study. Am J Sports Med. 2008;36:2100–2109. doi: 10.1177/0363546508324176. [DOI] [PubMed] [Google Scholar]
- 10.d’Agostino M, Craig K, Tibalt E, Respizzi S. Shock wave as biological therapeutic tool: from mechanical stimulation to recovery and healing, through mechanotransduction. Int J Surg. 2015;24:147–153. doi: 10.1016/j.ijsu.2015.11.030. [DOI] [PubMed] [Google Scholar]
- 11.Speed C. A systematic review of shockwave therapies in soft tissue conditions: focusing on the evidence. Br J Sports Med. 2014;48:1538–1542. doi: 10.1136/bjsports-2012-091961. [DOI] [PubMed] [Google Scholar]
- 12.Wang CJ. Extracorporeal shockwave therapy in musculoskeletal disorders. J Orthop Surg Res. 2012;7:11. doi: 10.1186/1749-799X-7-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.van der Worp H, Zwerver J, Hamstra M, van den Akker-Scheek I, Diercks RL. No difference in effectiveness between focused and radial shockwave therapy for treating patellar tendinopathy: a randomized controlled trial. Knee Surg Sports Traumatol. 2014;22:2026–2032. doi: 10.1007/s00167-013-2522-z. [DOI] [PubMed] [Google Scholar]
- 14.Foster TE, Puskas BL, Mandelbaum BR, Gerhardt MB, Rodeo SA. Platelet-rich plasma: from basic science to clinical applications. Am J Sports Med. 2009;37:2259–2272. doi: 10.1177/0363546509349921. [DOI] [PubMed] [Google Scholar]
- 15.De Vos RJ, Weir A, van Schie HT, Bierma-Zeinstra SM, Verhaar JA, Weinans H, Tol JL. Platelet-rich plasma injection for chronic Achilles tendinopathy: a randomized controlled trial. JAMA. 2010;303:144–149. doi: 10.1001/jama.2009.1986. [DOI] [PubMed] [Google Scholar]
- 16.Mahindra P, Yamin M, Selhi HS, Singla S, Soni A. Chronic plantar fasciitis: effect of platelet-rich plasma, corticosteroid, and placebo. Orthopedics. 2016;39:e285–e289. doi: 10.3928/01477447-20160222-01. [DOI] [PubMed] [Google Scholar]
- 17.Jain K, Murphy PN, Clough TM. Platelet rich plasma versus corticosteroid injection for plantar fasciitis: a comparative study. Foot. 2015;25:235–237. doi: 10.1016/j.foot.2015.08.006. [DOI] [PubMed] [Google Scholar]
- 18.Jain SK, Suprashant K, Kumar S, Yadav A, Kearns SR. Comparison of plantar fasciitis injected with platelet-rich plasma vs corticosteroids. Foot Ankle Int. 2018;39:780–786. doi: 10.1177/1071100718762406. [DOI] [PubMed] [Google Scholar]
- 19.Metzner G, Dohnalek C, Aigner E. High-energy Extracorporeal Shock-Wave Therapy (ESWT) for the treatment of chronic plantar fasciitis. Foot Ankle Int. 2010;31:790–796. doi: 10.3113/FAI.2010.0790. [DOI] [PubMed] [Google Scholar]
- 20.Böddeker I, Schäfer H, Haake M. Extracorporeal shockwave therapy (ESWT) in the treatment of plantar fasciitis-a biometrical review. Clin Rheumatol. 2001;20:324–330. doi: 10.1007/pl00011207. [DOI] [PubMed] [Google Scholar]
- 21.Giordani F, Bernini A, Müller-Ehrenberg H, Stecco C, Masiero S. A global approach for plantar fasciitis with extracorporeal shockwaves treatment. Eur J Transl Myol. 2019;29:8372. doi: 10.4081/ejtm.2019.8372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hawker GA, Mian S, Kendzerska T, French M. Measures of adult pain: Visual analog scale for pain (vas pain), numeric rating scale for pain (nrs pain), mcgill pain questionnaire (mpq), short-form mcgill pain questionnaire (sf-mpq), chronic pain grade scale (cpgs), short form-36 bodily pain scale (sf-36 bps), and measure of intermittent and constant osteoarthritis pain (icoap) Arthritis Care Res. 2011;63:S240–S252. doi: 10.1002/acr.20543. [DOI] [PubMed] [Google Scholar]
- 23.Leigheb M, Janicka P, Andorno S, Marcuzzi A, Magnani C, Grassi F. Italian translation, cultural adaptation and validation of the “American Orthopaedic Foot and Ankle Society’s (AOFAS) ankle-hindfoot scale”. Acta Biomed. 2016;87:38–45. [PubMed] [Google Scholar]
- 24.Dastgir N. Extracorporeal shock wave therapy for treatment of plantar fasciitis. J Pak Med Assoc. 2014;64:675–678. [PubMed] [Google Scholar]
- 25.Zhiyun L, Tao J, Zengwu S. Meta-analysis of high-energy extracorporeal shock wave therapy in recalcitrant plantar fasciitis. Swiss Med Wkly. 2013;143:w13825. doi: 10.4414/smw.2013.13825. [DOI] [PubMed] [Google Scholar]
- 26.Hsiao MY, Hung CY, Chang KV, Chien KL, Tu YK, Wang TG. Comparative effectiveness of autologous blood-derived products, shock-wave therapy and corticosteroids for treatment of plantar fasciitis: a network meta-analysis. Rheumatology. 2015;54:1735–1743. doi: 10.1093/rheumatology/kev010. [DOI] [PubMed] [Google Scholar]
- 27.Tiwari M, Bhargava R. Platelet rich plasma therapy: a comparative effective therapy with promising results in plantar fasciitis. J Clin Orthop Trauma. 2013;4:31–35. doi: 10.1016/j.jcot.2013.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Acosta-Olivo C, Elizondo-Rodriguez J, Lopez-Cavazos R, Vilchez-Cavazos F, Simental-Mendia M, Mendoza-Lemus O. Plantar fasciitis-a comparison of treatment with intralesional steroids versus platelet-rich plasma: a randomized, blinded study. J Am Podiatr Med Assoc. 2017;107:490–496. doi: 10.7547/15-125. [DOI] [PubMed] [Google Scholar]
- 29.Martinelli N, Marinozzi A, Carnì S, Trovato U, Bianchi A, Denaro V. Platelet-rich plasma injections for chronic plantar fasciitis. Int Orthop. 2013;37:839–842. doi: 10.1007/s00264-012-1741-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.O’Malley MJ, Vosseller JT, Gu Y. Successful use of platelet-rich plasma for chronic plantar fasciitis. HSS J. 2013;9:129–133. doi: 10.1007/s11420-012-9321-9. [DOI] [PMC free article] [PubMed] [Google Scholar]


