Abstract
Ocular manifestations of COVID-19 are still being studied. Posterior segment involvement in viral entities is either direct viral involvement or a delayed immune response to the antigen. A 22-year-old woman presented with history of perceiving absolute inferior scotoma in the right eye for 4 days and history of fever and sore throat 10 days ago. Fundus examination revealed disc edema and vessel tortuosity. Humphreys Field Analyzer confirmed inferior field defect and Optical Coherence Tomography showed superior, nasal and inferior retinal nerve fiber layer thickening in the right eye. Patient was positive for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) by reverse transcription polymerase chain reaction (RT-PCR) testing. Patient received three doses of injection methylprednisolone over 3 days. There was subjective resolution of scotoma reported 3 weeks posttreatment. We bring forward the first reported case of parainfectious optic neuritis associated with COVID-19.
Keywords: Disc edema, field defects, neuro-ophthalmology, pandemic, SARS-CoV-2
An outbreak of a novel coronavirus disease emerged in Wuhan, China in December 2019 progressively causing a pandemic, the infectious agent of it being the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). Though the pathogenesis of COVID-19 remains poorly understood and under evaluation, it has been attributed to inflammatory cytokine storm and viral evasion of cellular immune responses, causing immunothrombosis. To add to the myriad of ocular manifestations of SARS-CoV-2, which is still poorly understood and is under evaluation, we report a case of unilateral inferior altitudinal visual field defect in a COVID-19 positive patient.
Case Report
A healthy 22-year-old woman presented to our outpatient department with history of acute-onset blurring of vision and perceiving an absolute scotoma in the inferior field of vision in the right eye since the last 4 days, not accompanied by any neurological symptoms. The patient was not a known case of any systemic disease and was not on any prior medications like oral contraceptive pills. Patient gave history of fever, sore throat, and fatigue around 10 days back. She was not tested for COVID-19 at the onset of symptoms. There was history of exposure to a laboratory confirmed case of COVID-19 15 days prior. On examination, uncorrected visual acuity was 20/25 OD and 20/20 OS. Anterior segment was within normal limits in both the eyes on slit-lamp examination, including intraocular pressure (IOP). Relative afferent pupillary defect was present in the right eye. Patient could identify 24/24 plates of a standard Ishihara chart with increased latency OD. Confrontational visual fields revealed an inferior visual field defect in the right eye. Dilated fundoscopy of the right eye revealed nasal, superior and inferior blurring of disc margin with tortuosity and dilatation of vessels [Fig. 1]. Visual fields by Humphreys Field Analyzer (HFA) showed inferior altitudinal visual field defect OD [Fig. 2]. On Optic Nerve Head-Optical Coherence Tomography (ONH-OCT), retinal nerve fiber layer thickness was more than average in superior, inferior and nasal quadrants [Fig. 3]. Pupillary reactions, color vision, dilated fundoscopy, visual field analysis by HFA and ONH-OCT were normal in the left eye. Macular Optical Coherence Tomography was normal OU. Neurological examination revealed no deficit. Computed tomography of brain and orbit was within normal limits. Gadolinium contrast enhanced magnetic resonance imaging of the brain and spine was within normal limits. Chest X-ray was clear. C-reactive protein was found to be positive. Platelet count was 496,000 per cubic mL. Rest of the blood investigations were within normal limits. Patient tested positive for COVID-19 by real-time reverse transcription-polymerase chain reaction (RT-PCR) test. Patient received injection methylprednisolone 1 g three doses over 3 days, after clearance from physician. Resolution of disc edema in the inferior margin was noted and patient was discharged on oral prednisolone and was asked to follow-up. The patient could not follow up to the outpatient department and hence, posttreatment HFA could not be recorded. However, on telephonic communication 3 weeks post-discharge, the patient gave history of subjective resolution of inferior scotoma.
Figure 1.

Fundus photo of the right eye showing superior, nasal and inferior blurring of disc margins with tortuosity and dilatation of vessels
Figure 2.
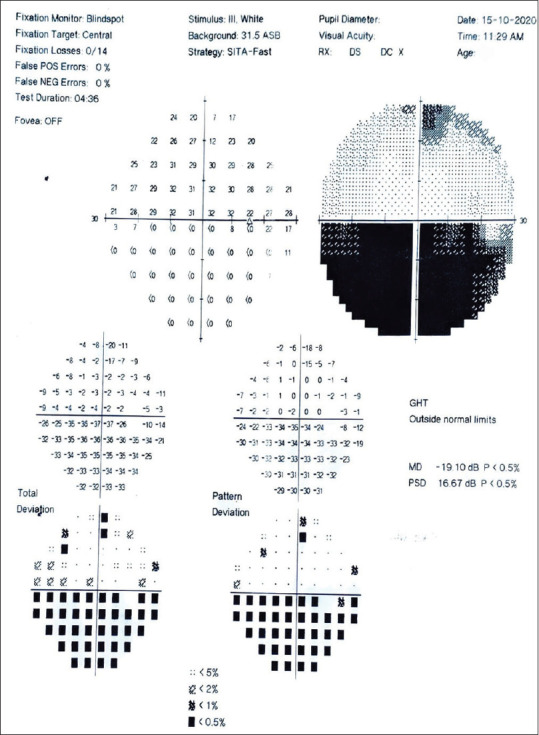
Visual fields by Humphreys Field Analyzer (HFA) showing inferior altitudinal visual field defect in the right eye
Figure 3.
Optical Coherence Tomography showing more than average thickness of retinal nerve fiber layer in the nasal, superior and inferior quadrants
Discussion
Not much has been published regarding SARS-CoV-2 with respect to ocular manifestations and their pathogenesis. The most common ocular manifestation is conjunctivitis (0.8%)[1] due to direct infection of ocular surface. Systemic vasculitis has been extensively described in relation to COVID-19.[2] It occurs secondary to type-3 hypersensitivity (immune complex disease). Few cases of retinal vascular occlusion have been documented and are presumed to be due to vasculitis. Hypercoagulable state induced by COVID-19 can result in venous thromboembolism, leading to central retinal vein occlusion.[3] In our case, a young woman presented with disc edema and altitudinal visual field defect without any comorbidities with spontaneous resolution of symptoms following treatment. Viral infections can lead to posterior segment involvements such as retinitis, neuroretinitis, optic neuritis, and panuveitis. The proposed mechanisms for such ocular manifestations in viral entities include direct viral involvement or a delayed immune response to the viral antigen.[4,5] Posterior segmental involvement is usually seen in 1–4 weeks following the onset of fever in viral infections.[5,6] Like in our case the time lag of 10 days between acute infection and retinal manifestation suggests immune-mediated pathogenesis, post-viral infection.[7] COVID-19 is also a prothrombotic situation and may lead to Non-arteritic Anterior Ischemic Optic Neuropathy (NA-AION) and a fundus fluorescein angiography should be done to rule out the same. However, the patient in this case was unwilling to follow up for any more additional tests, thus limiting the diagnosis. To the best of our knowledge, this is the first reported case of parainfectious type of optic neuritis following COVID-19 infection.
Conclusion
Knowledge of this new entity will make clinicians aware that patients with COVID19 infection are at a risk for atypical type of optic neuritis and the visual symptoms may occur with milder forms of systemic viral infection.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382:1708–20. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.RECOVERY Collaborative Group. Horby P, Lim WS, Emberson J, Mafham M, Bell J, et al. Dexamethasone in hospitalized patients with Covid-19 - preliminary report. N Engl J Med. 2020 doi: 10.1056/NEJMoa2021436. doi: 101056/NEJMoa2021436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Panigada M, Bottino N, Tagliabue P, Grasselli G, Novembrino C, Chantarangkul V, et al. Hypercoagulability of COVID-19 patients in intensive care unit: A report of thromboelastography findings and other parameters of hemostasis. J Thromb Haemost. 2020;18:1738–42. doi: 10.1111/jth.14850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Velaitham P, Vijayasingham N. Central retinal vein occlusion concomitant with dengue fever. Int J Retina Vitreous. 2016;2:1. doi: 10.1186/s40942-016-0027-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lalitha P, Rathinam S, Banushree K, Maheshkumar S, Vijayakumar R, Sathe P. Ocular involvement associated with an epidemic outbreak of chikungunya virus infection. Am J Ophthalmol. 2007;144:552–6. doi: 10.1016/j.ajo.2007.06.002. [DOI] [PubMed] [Google Scholar]
- 6.Chan DP, Teoh SC, Tan CS, Nah GK, Rajagopalan R, Prabhakaragupta MK, et al. Ophthalmic complications of dengue. Emerg Infect Dis. 2006;12:285–9. doi: 10.3201/eid1202.050274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sheth JU, Narayanan R, Goyal J, Goyal V. Retinal vein occlusion in COVID-19: A novel entity. Indian J Ophthalmol. 2020;68:2291–3. doi: 10.4103/ijo.IJO_2380_20. [DOI] [PMC free article] [PubMed] [Google Scholar]



