Abstract
A 42-year-old male patient presented with profound impairment of vision in both eyes, just as he was recovering from COVID-19. A known diabetic and hypertensive, he suffered from COVID-19 pneumonia further complicated by ARDS, septicaemia and acute kidney injury. His vision on presentation was finger counting close to face bilaterally with multiple, yellowish lesions at the posterior pole. Based on the clinical findings and previous blood culture report, it was diagnosed as candida retinitis and treated with oral and intravitreal anti-fungals. The lesions were regressing at follow-up. This is a post COVID-19 presumed candida retinitis case report.
Keywords: Candida retinitis, coronavirus, Covid and eye, Covid-19, intravitreal voriconazole
The coronavirus disease-2019 (COVID-19) caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has resulted in a global pandemic.[1] Recent studies reporting ocular involvement with SARS-CoV-2 infection have described conjunctivitis as the commonest ocular manifestation, with incidence ranging from 0.8%[2] to 31.6%.[3] Other manifestations like uveitis, retinitis, retinal vasculitis and optic neuritis have been described in animal models with few reports in humans. Ocular involvement in COVID-19 can also be secondary to immunosuppressive modalities used in its management.
Case Report
A 42-year-old male patient, known diabetic and hypertensive since 6 years, presented with diminution of vision in both eyes. He had contracted COVID-19 infection 2 months earlier and was hospitalised for ARDS and kept on ventilatory support for 3 weeks. He had received Tocilizumab 162 mg subcutaneous single dose and intravenous Dexamethasone 4 mg twice a day for 10 days followed by oral dexamethasone tapered over a month. After recovery from pneumonia and discharge from the hospital, he had developed acute kidney injury and urosepsis necessitating readmission. During the 2-week hospital stay, investigations revealed pancytopenia, increased serum creatinine, blood culture positive for Candida Albicans and urine culture positive for Klebsiella Pneumoniae. He was treated with IV fluids, antibiotics, antiemetics, antifungals & supportive medication. When systemically stable, he was discharged. He had noticed gradually progressive, painless diminution of vision in both eyes during these 2 weeks of hospitalization.
On visiting our eye clinic, his BCVA in both eyes was counting fingers close to face. Anterior segment evaluation was unremarkable. Fundus examination of both eyes revealed clear vitreous, with multiple, yellowish-white, fluffy lesions, 1/2 to 1-disc diameter in size scattered, predominantly across the posterior pole [Fig. 1]. The foveal centre was involved with the retinitis lesion in the left eye and just spared in the right. No retinal haemorrhages or pigmentary changes were seen. Inferotemporal periphery from 3 to 6 o clock had evidence of moderate choroidal detachment in both eyes. Retina was attached throughout in both eyes. Based on the clinical features and prior positive blood culture, a diagnosis of bilateral candida retinitis was made.
Figure 1.
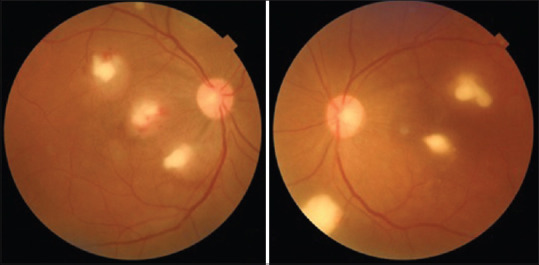
Standard 45-degree posterior pole photo of both eyes showing yellowish-white, fluffy lesions involving fovea
Standard Fundus Photography (Topcon Triton) [Fig. 1], Ultra-Wide Field retinal imaging (Optos Daytona) [Figs. 2a, b and 3a, b] & Swept Source OCT (Topcon Triton) [Figs. 2c, d and c, d] were performed. OCT revealed hyperreflective lesions mainly involving the inner layers of the retina and obscuring the deeper retinal layers & RPE in both eyes. Additionally, the right eye had a small pocket of subretinal fibrinous fluid just under the foveal centre [Fig. 3c].
Figure 2.
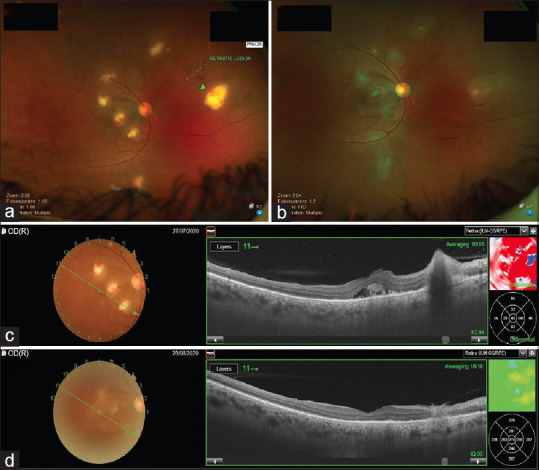
(a) Ultra-wide field retinal imaging showing right eye candida retinitis lesions (b) Regressed lesions one month post intravitreal Voriconazole. (c) OCT of right eye shows sub foveal fibrinous fluid and parafoveal lesion (d) One month post Intravitreal Voriconazole there is resolution of fluid and lesion
Figure 3.
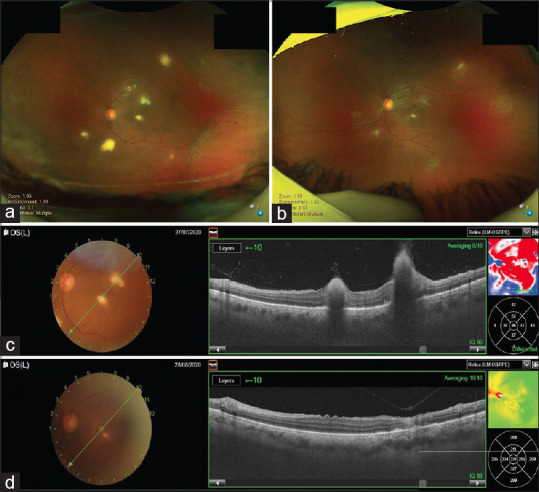
(a) Left eye retinitis lesions and inferotemporal choroidal detachment (b) One month post intravitreal Voriconazole, both appear to have regressed. (c) Left eye OCT image of foveal and parafoveal retinitis (d) One month post Intravitreal Voriconazole resolution of lesions
With bilateral macular involvement and profound impairment of vision, intravitreal Voriconazole injection (100 micrograms in 0.1 ml) was planned in both eyes sequentially. Simultaneously, systemic Fluconazole therapy was restarted in co-ordination with his physician. A month later, vision had improved to 3/60 in both eyes; retinitis lesions and choroidals had regressed significantly [Figs. 2b and 3b]. OCT showed regression of lesions in both eyes [Figs. 2d and 3d] with clearance of right eye subfoveal fluid [Fig. 2d]. This was his last follow-up visit and though his eye condition was improving, the patient died 6 weeks later of other systemic complications.
Discussion
The grave morbidity and mortality associated with the COVID-19 pandemic is due to the collateral damage caused by an exaggerated host immune response.[4] Corticosteroids and monoclonal antibody against IL6 receptor (tocilizumab) are used in the mainstream treatment protocols of COVID-19 for their effectiveness in controlling the cytokine storm.[5] This particular diabetic patient received both, corticosteroids and tocilizumab, making him susceptible for opportunistic infections.
Differential diagnoses for retinal infiltrates without significant vitritis or anterior segment inflammation are cytomegalovirus (CMV) retinitis and progressive outer retinal necrosis (PORN). Causes for retinal infiltrates with vitritis and anterior segment inflammation include acute retinal necrosis (ARN), bacterial or fungal endophthalmitis, toxoplasmosis and Behcet‘s disease. In this case, blood culture was positive for fungal (Candida) infection and corelating it with the clinical picture, it was presumed that the retinal infiltrates were also likely to be due to Candida. OCT image clearly showed retinal infiltrates sparing the choroid, hence conditions causing predominant choroidal infiltrates like tuberculosis, toxoplasmosis, sarcoidosis, VKH, sympathetic ophthalmia, white dot syndromes were excluded.
Candida albicans is a common culprit causing opportunistic infections in the immunocompromised. Candida retinitis has been reported after influenza virus type A infection.[6] Its diagnoses can be challenging in the initial stage with only chorioretinal involvement.[7] Candida endophthalmitis has been reported in the immunocompromised, however, its treatment options have not been evaluated through well-designed trials. Traditional systemic therapy for chorioretinitis has been amphotericin B with or without flucytosine or fluconazole.[8] More aggressive treatment involving vitrectomy with or without intravitreal antifungal agents like amphotericin B, caspofungin[9] or voriconazole would be necessary for endophthalmitis.[8] Though the clinical picture in this case was not in favour of endophthalmitis, we decided to treat with additional intravitreal antifungal Voriconazole as the patient had bilateral foveal involvement and was not on any systemic anti-fungal medication for more than one week.
Conclusion
Even though the recommendation of routine ophthalmic evaluation of patients with systemic infections and immunosuppressive therapies is not very strong, those with candidemia should have a dilated retinal examination.[10]
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Cascella M, Rajnik M, Cuomo A, Dulebohn SC, Di Napoli R. StatPearls [Internet] Treasure Island (FL): StatPearls Publishing; 2020. May 18, Features, Evaluation and Treatment Coronavirus (COVID-19) [Google Scholar]
- 2.Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382:1708–20. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wu P, Duan F, Luo C, Liu Q, Qu X, Liang L, et al. Characteristics of ocular findings of patients with coronavirus disease 2019 (COVID-19) in Hubei Province, China. JAMA Ophthalmol. 2020;138:575–8. doi: 10.1001/jamaophthalmol.2020.1291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mehta P, McAuley DF, Brown M, Sanchez E, Tattersall RS, Manson JJ on behalf of the HLH Across Speciality Collaboration, UK. COVID-19: Consider cytokine storm syndromes and immunosuppression. Lancet. 2020;395:P1033–4. doi: 10.1016/S0140-6736(20)30628-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Riegler LL, Jones GP, Lee DW. Current approaches in the grading and management of cytokine release syndrome after chimeric antigen receptor T-cell therapy. Ther Clin Risk Manag. 2019;15:323–35. doi: 10.2147/TCRM.S150524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Menia NK, Sharma SP, Bansal R. Fungal retinitis following influenza virus type A (H1N1) infection. Indian J Ophthalmol. 2019;67:1483–4. doi: 10.4103/ijo.IJO_1691_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Invernizzi A, Symes R, Miserocchi E, Cozzi M, Cereda M, Fogliato G, et al. Spectral domain optical coherence tomography findings in endogenous Candida endophthalmitis and their clinical relevance. Retina. 2018;38:1011–8. doi: 10.1097/IAE.0000000000001630. [DOI] [PubMed] [Google Scholar]
- 8.Khan FA, Slain D, Khakoo RA. Candida endophthalmitis: Focus on current and future antifungal treatment options. Pharmacotherapy. 2007;27:1711–21. doi: 10.1592/phco.27.12.1711. [DOI] [PubMed] [Google Scholar]
- 9.Yadav HM, Thomas B, Thampy C, Panaknti TK. Management of a case of Candida albicans endogenous endophthalmitis with intravitreal caspofungin. Indian J Ophthalmol. 2017;65:529–31. doi: 10.4103/ijo.IJO_781_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pappas PG, Kauffman CA, Andes D, Benjamin DK, Jr, Calandra TF, Edwards JE, Jr, et al. Clinical practice guidelines for the management of candidiasis: 2009 update by the Infectious Diseases Society of America. Clin Infect Dis. 2009;48:503–35. doi: 10.1086/596757. [DOI] [PMC free article] [PubMed] [Google Scholar]


