Abstract
The COVID-19 pandemic has resulted in reduction of patient volumes in Ophthalmology. With only emergency surgical procedures being performed with few elective surgical procedures, surgical volumes are at an all-time low. This has resulted in decreased surgical training opportunities for trainee surgeons. We developed a simple, cost-effective, 3D printed model eye – RetiSurge – for “Dry Lab” vitreoretinal surgery training. The model incorporates a retinal film that can be changed, making it suitable for multiple uses. The RetiSurge model can be used to practice visualization, instrument manipulation and endolaser photocoagulation. RetiSurge can be sterilized by ethylene oxide and is safe for use inside the operating room. RetiSurge is a simple, cost-effective, and reusable model eye for early training in Vitreoretinal surgery.
Keywords: COVID-19, dry lab, model eye, simulator, surgical training, vitreoretinal surgery
Ophthalmic surgical training is complex and challenging.[1] Performing vitreoretinal (VR) surgeries requires focusing retina with the visualization system and manipulation of instruments in an enclosed space of the vitreous cavity. Novice surgeons often face many challenges. Use of animal eyes for VR surgery is limited by their availability, need for separate instruments and poor visibility due to corneal edema. Simulators using virtual reality platforms are excellent, but these are expensive and not widely available.[2]
In the course of the current COVID-19 pandemic, hospitals are seeing a great reduction in patient volumes.[3] The impact of this is seen in training of medical residents and fellows.[4] The new normal of teaching has the classroom moving to online platforms and surgical training to viewing videos and practice on goat‘s eye or simulators.[2]
3D printed anatomically accurate body parts are widely used for surgical training in lieu of simulators.[5,6] We describe a simple and cost-effective model eye – RetiSurge – Retinal Surgery model eye, created via 3D printing, for early “Dry Lab” training in VR surgery.
Technique
Model eye framework
For 3D printing the RetiSurge model eye, an anatomically accurate sketch of the eyeball is incorporated into Computer-Aided Design (CAD) software with appropriate dimensions. The CAD software exports this model native file format into STL (Standard triangle language) file which is used for 3D printing. Information regarding material properties, dimensions, tolerance, and manufacturing process are incorporated in this file. The STL file is then converted into machine language i.e., G-code (through a process called “slicing”) which is recognized by 3D printer to create the model eye. The RetiSurge model consists of two interlocking hemispheres, the upper half is printed using TPU (Thermoplastic polyurethane) [Fig. 1a], a flexible material with tenacity similar to human sclera. The lower half is composed of plastic filament material i.e., PLA (Polylactic acid) [Fig. 1b].
Figure 1.
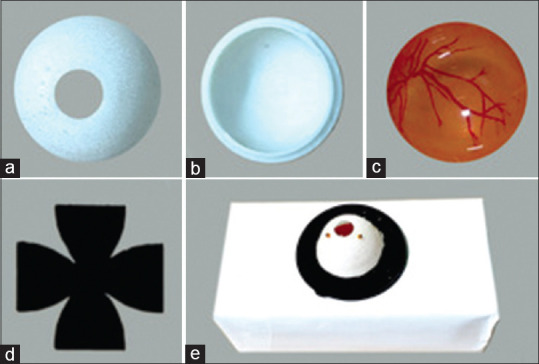
(a) Upper hemisphere of the model eye made of Thermoplastic polyurethane. (b) Lower hemisphere of the model eye made of Polylactic acid. (c) Polyethylene terephthalate glycol (PETG) sheet with printed fundus image, shaped with thermoforming technology. (d) 3D printed tracer for customization of fundus print out. (e) RetiSurge model eye assembled for use
Preparation of retinal film
A colored fundus image is printed on regular white A4 sheet and folded into a hemisphere using k comb wrapping.[7] A 3D printed tracer [Fig. 1d] is used to customize the fundus print out so that it fits perfectly into the eyeball model. For a realistic fundus image, printing on a polyethylene terephthalate glycol (PETG) sheet shaped by thermoforming technology can be an alternative [Fig. 1c]. The film is placed in the lower half of the eyeball model. Alternately, a liquid skin bandage can be placed to practice membrane peeling.
Assembly
The RetiSurge model eye needs to be fixed in place for surgical practice. We used a microscope handle cover fitted into the hole made in a cardboard box [Fig. 1e]. Using routine vitrectomy trocar canula sets, sclerotomies can be fashioned in the upper flexible half for introduction of an endoilluminator and second active instrument such as vitrectomy or endolaser probe. This assembly is used in conjunction with the operating microscope with a wide-angle visualization system to visualize the posterior segment.
The technique has been demonstrated in the supplemental surgical video.
Discussion
We describe a simple, 3D printed model eye – RetiSurge for practice of basic steps of VR surgery. Visualization is the key to successful VR surgery. RetiSurge helps develop hand-eye coordination, orientation to wide-angle viewing system, and XY movements of microscope while maintaining focus intraocularly on the retinal film. By helping the trainee surgeon in developing spatial sense as a precursor to actual vitrectomy, the risk of inadvertent retinal touch during actual surgery can be minimized. VR surgery requires bimanual manipulations for good illumination of required locus of retina while avoiding glare from instruments, as well as maintaining a stable globe while approaching various quadrants of the eye. These maneuvers require control on the non-dominant hand. This dexterity can be achieved by training with RetiSurge.
The RetiSurge with PETG film is excellent for endolaser practice. The laser spots resemble those on the human retina with power settings comparable with real-life scenario [Fig. 2]. The retinal film inside can be changed easily and multiple pre-cut or pre-printed images can be at hand for ease of use. The same model eye can be used numerous times by various trainee surgeons. The materials used in manufacturing this model eye are safe for sterilization by ethylene oxide. As there is no biological tissue used, a sterilized model Retisurge can be used inside the regular operating room for training. This enables use of microscope, wide-angle viewing system as well as vitrectomy machine and laser. The limitations of RetiSurge model eye include inability of practice all surgical maneuvers and it simulates the fundus view of an aphakic eye.
Figure 2.
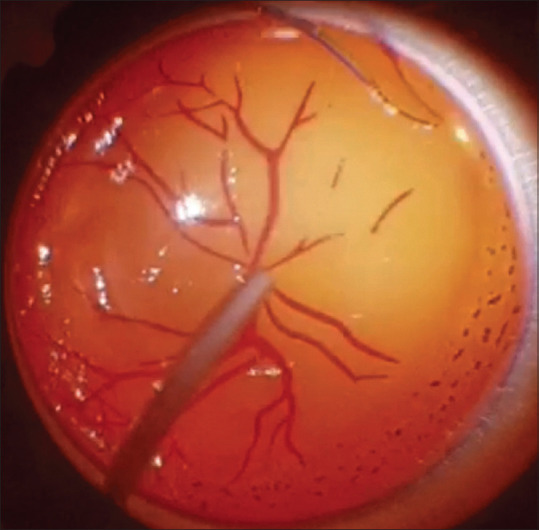
Image demonstrating laser photocoagulation practice on PETG film
Eyeball models for training have been previously described. An eyeball model created using a ping-pong ball for practice for Slit-lamp laser photocoagulation described by Ganne et al. is an excellent low-cost model that utilizes pre-printed fundus images on paper.[8] The use of liquid skin bandage inside commercially available model eye for membrane peeling is also described.[9]
Ophthalmology is a medical speciality that largely deals with elective care. In the ongoing COVID -19 pandemic, there have been large reductions in ophthalmic practices as well as a cessation of elective surgeries.[3] An online survey amongst trainee ophthalmologists revealed that 80.7% felt an impact on surgical training, with a perceived 50% reduction in surgical volume.[10] In addition, 54.8% reported higher stress and 46.5% of respondents stated to be “feeling unhappy”.
Conclusion
Challenging times call for innovations. In the new normal of a society that has to continue to function amidst a global pandemic, “Dry Lab” training is a way forward. With reduction in patient volumes and need for lesser surgical times, training can continue by an initial phase of simulation on the model eyes like RetiSurge. To conclude, RetiSurge is simple, cost-effective and reusable model for early VR Surgical training.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Video Available on: www.ijo.in
References
- 1.Sindal MD, Chhabra K. Commentary: Optimizing surgical training. Indian J Ophthalmol. 2020;68:82–3. doi: 10.4103/ijo.IJO_1791_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kumar A, Agarwal D. Commentary: Restructuring residency training in ophthalmology during COVID-19 era: Challenges and opportunities. Indian J Ophthalmol. 2020;68:1005–6. doi: 10.4103/ijo.IJO_1462_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Babu N, Kohli P, Mishra C, Sen S, Arthur D, Chhablani D, et al. To evaluate the effect of COVID-19 pandemic and national lockdown on patient care at a tertiary-care ophthalmology institute. Indian J Ophthalmol. 2020;68:1540–44. doi: 10.4103/ijo.IJO_1673_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wong TY, Bandello F. Academic ophthalmology during and after the COVID-19 pandemic. Ophthalmology. 2020;127:e51–2. doi: 10.1016/j.ophtha.2020.04.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Prsic A, Boyajian MK, Snapp WK, Crozier J, Woo AS. A 3-dimensional-printed hand model for home-based acquisition of fracture fixation skills without fluoroscopy. J Surg Educ. 2020;77:1341–4. doi: 10.1016/j.jsurg.2020.05.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Shahrubudin N, Lee TC, Ramlan R. An overview on 3D printing technology: Technological, materials, and applications. Procedia Manuf. 2019;35:1286–96. [Google Scholar]
- 7.Demaine ED, Demaine ML, Iacono J, Langerman S. Wrapping spheres with flat paper. Comput Geom. 2009;42:748–57. [Google Scholar]
- 8.Ganne P, Krishnappa NC, Baskaran P, Sulaiman SM, Venkatesh R. Retinal laser and photography practice eye model: A cost-effective innovation to improve training through simulation. Retina. 2018;38:207–10. doi: 10.1097/IAE.0000000000001885. [DOI] [PubMed] [Google Scholar]
- 9.Iyer MN. An eye model for practicing vitreoretinal membrane peeling. Arch Ophthalmol. 2006;124:108–10. doi: 10.1001/archopht.124.1.108. [DOI] [PubMed] [Google Scholar]
- 10.Mishra D, Nair A, Gandhi R, Gogate P, Mathur S, Bhushan P, et al. The impact of COVID-19 related lockdown on ophthalmology training programs in India – Outcomes of a survey. Indian J Ophthalmol. 2020;68:999–1004. doi: 10.4103/ijo.IJO_1067_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


