SUMMARY:
A heretofore unreported type of facial fracture is discussed. Twenty-two cases of posterior maxillary wall fracture are reviewed, of which 59% demonstrated concomitant mandibular fracture. The proposed mechanism for this injury is an impact from the ipsilateral mandibular coronoid process striking the posterior maxillary wall, with associated mandibular dislocation or fracture. As such, further investigation of the mandible may be warranted when this type of maxillary wall fracture is encountered to exclude concomitant injury.
High-resolution CT with multiplanar reformats and 3D postprocessing has become a standard part of the assessment of facial trauma because of the exquisite sensitivity of this imaging technique for fracture. Such sensitivity for fracture is particularly relevant in the setting of facial trauma, given that soft-tissue swelling can mask underlying fractures on physical examination.1,2 Accurate fracture detection and characterization are important because facial fractures can have long-term functional and/or cosmetic sequelae.3 Extensive work, therefore, has been invested in describing patterns and underlying mechanisms of facial fracture.4–7 Data regarding specific patterns and mechanisms of fracture can be helpful to the radiologist by increasing the sensitivity for detection of distributed injuries in which 1 traumatic finding leads to a focused search for related injuries.4–7 In this retrospective case series, we describe a unique type of fracture characterized by an isolated one of the posterior maxillary wall and its association with mandibular dislocation and/or fracture. The proposed mechanism for this specific injury is also discussed.
Materials and Methods
We performed a retrospective review of the neuroradiology section case log from 2002 to 2009, searching for patients with the CT (either head or face CT) diagnosis of maxilla fracture limited to the posterior wall, including a possible associated mandibular fracture. All patients had been imaged in the setting of trauma by using single-section or multidetector CT scanners with 1, 4, 16, and 64 detectors (LightSpeed VCT; GE Healthcare, Milwaukee, Wisconsin). Axial CT images were generally obtained via the following parameters: 0.625-mm section thickness (3-mm thickness in old scanners), 1.375:1 pitch, 120 kV, 540 mA, no gantry tilt, 20 display FOVs, and a bone reconstruction algorithm. Multiplanar reconstruction was performed in most of the fractures, and 3D postprocessing was performed in recent years by using AquariusNET software (TeraRecon, San Mateo, California) to aid in the diagnosis and to exclude other fractures. All CT scans were reviewed independently by 2 neuroradiologists to determine if the patient had a fracture of the maxilla limited to the posterior wall as well as a concomitant fracture and/or dislocation of the mandible. Medical records of each patient were reviewed for clinical history and confirmation of the diagnosis.
Results
Twenty-three patients were retrospectively identified with the CT diagnosis of maxilla fracture limited to the posterior wall, with or without a concomitant mandibular fracture. One patient was excluded as an outlier because he had a complex facial crush injury (with zygoma fracture). The final cohort of 22 patients included 17 men and 5 women, with an average age of 35 years (range, 19–58 years). Sixteen patients (16/22, 73%) were involved in motor vehicle crashes; 2 patients had blunt assault injuries; 2 patients had gunshot wounds (remote from the face); the submandibular area of 1 patient was struck by compressed water via a high-pressure power washer; and 1 patient had an unknown history, being found unconscious (On-line Table). Nine patients (9/22, 41%) had right-sided and 13 patients (13/22, 59%) had left-sided maxillary fractures (Table). Thirteen patients (13/22, 59%) had concomitant mandibular fractures, and 9 patients (9/22, 41%) had no associated fractures. Twelve patients (12/22, 55%) demonstrated ipsilateral (Fig 1) and 1 patient demonstrated contralateral maxillary and mandibular fractures. One patient had an anterior ipsilateral TMJ dislocation at the time of imaging. There was 100% consensus on the final diagnosis and fracture pattern between the 2 neuroradiology reviewers.
Location and mechanism of fractures
| Right | Left | Total | |
|---|---|---|---|
| Associated mandibular fracture | 5 | 8 | 13 |
| Maxillary fracture only | 4 | 5 | 9 |
| Causes: MVC | 9 | 7 | 16 |
| Other causes | 0 | 6 | 6 |
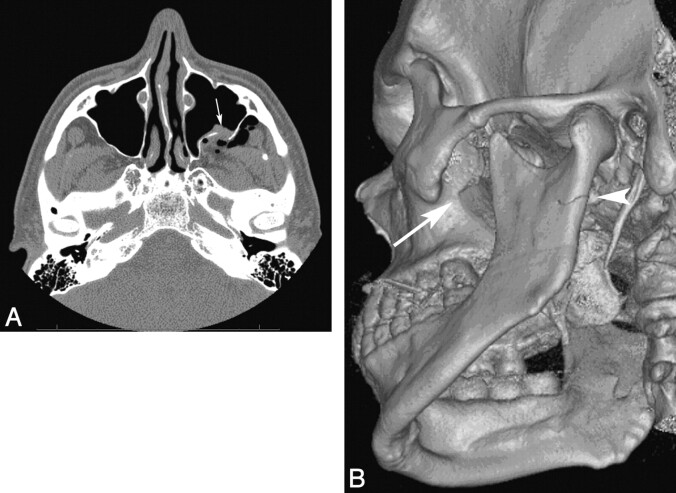
Fig 1.
A, A comminuted fracture of the posterior wall of the left maxillary sinus (arrow). Note the vector of the fracture fragment displacement (anteromedially) and herniation of the retroantral fat into the maxillary sinus. B, 3D reconstructed image demonstrates a minimally displaced fracture of the left subcondylar mandibular ramus, extending into the mandibular notch (arrowhead). The comminuted left posterior maxillary wall fracture is redemonstrated (long arrow).
Discussion
There are several types of midface fracture, including LeFort, zygomatic complex or “tripod,” orbital floor, naso-orbitoethmoidal, nasal, and nasoethmoidal, as well as those that are the result of localized trauma, such as direct injury to the anterior maxillary wall,8,9 including projectile injuries. The midface fracture described in this article involves only the posterior wall of the maxillary antrum. A review of the medical literature during the last 30 years yielded no descriptions of or references to this pattern of injury.
Ellis et al10 published a review of facial fractures documented for a 10-year period. In 4711 patients who had maxillofacial fractures, 2137 (45.4%) had at least 1 mandibular fracture. Of the 2137 patients with mandibular fractures, 37 (1.7%) were associated with maxillary fracture. Unfortunately, Ellis et al did not describe the portion of the maxilla involved in these cases. Furthermore, the study began in 1973, so most patients were not imaged with CT. The major causes of mandibular fracture reported by Ellis et al included assault, fall, and automobile crash, with automobile crash being the most common cause. The findings of Ellis et al are similar to those described in this study, in which automobile crash was the most common cause of mandibular (ie, mandibular coronoid process) and associated facial bone fractures (ie, posterior maxillary wall).
A review of the relevant anatomy demonstrates that the posterior maxillary wall is very well protected by the mandible and zygomatic arch, as well as the superficial and deep facial soft tissues. We hypothesize that a blow from an anteromedially displaced mandibular coronoid process results in fracture of the posterior maxillary wall (Fig 2). Fracture of the mandible in the setting of posterior maxillary wall fracture would support this hypothesis. Indeed, the present retrospective case series demonstrates that more patients with posterior maxillary wall fractures have concomitant mandibular fractures. Furthermore, of the 13 cases of maxillary fracture associated with concomitant mandibular fracture, 12 were ipsilateral, thus supporting our proposed hypothesis. It is imperative, therefore, to recognize the possibility of an associated mandibular fracture when an isolated posterior maxillary wall fracture is detected, often on a head CT that does not image the entire mandible.
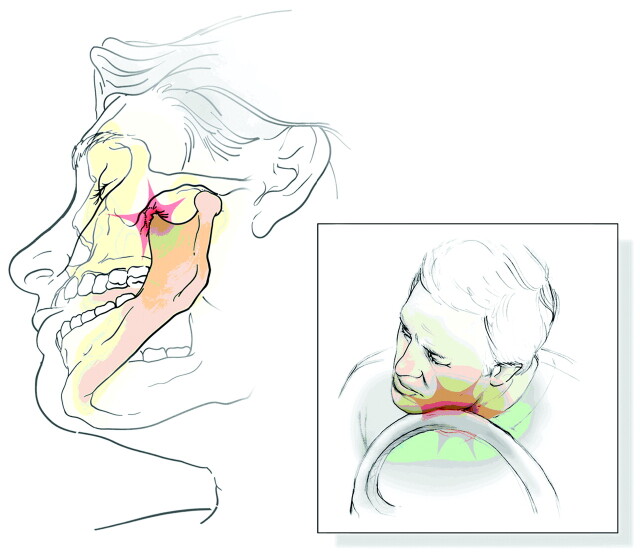
Fig 2.
Following an abrupt deceleration of a vehicle, the individual continues forward with his jaw striking the steering wheel. The momentum of the individual into the steering wheel results in rotation and medial displacement of the ipsilateral mandibular body, anteriorly dislocating the mandibular condyle and ultimately driving the coronoid process into the ipsilateral maxillary wall. Following the blow, the strong masticator musculature typically reduces the mandible into a normal anatomic position.
In this series, we noticed that the location of mandibular fractures was subcondylar or involved the ramus, angle, or body of the mandible. We did not specifically identify parasymphyseal/symphyseal or coronoid process fractures. The location of the associated mandibular fractures we identified could be related to the proposed mechanism of injury that causes the mandible to slide anteromedially, striking the posterior maxillary sinus wall. An alternative explanation is that our sample size may not have been large enough to detect coronoid process or symphyseal fractures. This may be examined by a larger sample study in the future.
Our data are subject to a number of limitations. One limitation is that all data were collected from a research log book. As such, we do not know the precise prevalence of posterior maxillary wall fracture in our practice. The actual prevalence of posterior maxillary fracture may be higher than reported in our case series; however, there is no specific code for posterior maxillary wall fracture in our medical records system that we can use to retrieve all patients with this specific injury. A second limitation is that though the proposed posterior maxillary wall fracture mechanism is consistent with the pattern of injury in 92% (12/13) of patients in this study, it does not explain injury distribution in all patients. For example, 1 case (1/13, 8%) of posterior maxillary wall fracture was associated with a contralateral mandibular fracture, a pattern of injury that does not fit the proposed injury mechanism. This single case of posterior maxillary wall fracture with contralateral mandibular fracture may have been spurious in nature and/or the result of an additional injury mechanism. Further investigation of the precise mechanism of injury by using human cadavers may be warranted to explore the injury biomechanics of posterior maxillary wall fractures.
A third limitation of these data is that they were collected as a retrospective case series. As such, clinical information, such as injury etiology, is dependent on the accuracy of medical records. A fourth limitation of these data is that patients with posterior maxillary wall fracture did not undergo an MR imaging examination to help with detection of soft-tissue or TMJ injuries during the study period. The current injury information, therefore, is limited to CT technology. The fifth limitation is that our sample size was small (9 versus 13); therefore, statistical analysis was not feasible in this study. Consequently, percentages are probably more appropriate to highlight our results.
Conclusions
Isolated posterior maxillary wall fractures are rare but are frequently associated with ipsilateral mandibular fractures. As a result, we believe that this fracture pattern suggests an injury mechanism consisting of a puncture to the posterior maxillary wall by the anteriorly displaced coronoid process. The presence of an isolated posterior maxillary wall fracture, therefore, should prompt further investigation of the mandible and possibly the TMJ to exclude concomitant injury.
Supplementary Material
Abbreviations
- GSW
gunshot wound
- MVC
motor vehicle crash
- TMJ
temporomandibular joint
Footnotes
indicates article with supplemental on-line table.
References
- 1. Hopper RA, Salemy S, Sze RW. Diagnosis of midface fractures with CT: what the surgeon needs to know. Radiographics 2006;26:783–93 [DOI] [PubMed] [Google Scholar]
- 2. Daffner RH. Imaging of facial trauma. Curr Probl Diagn Radiol 1997;26:153–84 [DOI] [PubMed] [Google Scholar]
- 3. Thompson JN, Gibson B, Kohut RI. Airway obstruction in LeFort fractures. Laryngoscope 1987;97:275–79 [PubMed] [Google Scholar]
- 4. LeFort R. Etude experimentale sur les fractures de la machoire superieure. Rev Chir Paris 1901;23:208–27 [Google Scholar]
- 5. Rowe NC, Killey H. Fractures of the Facial Skeleton. Baltimore: Williams & Wilkins; 1955:205–33 [Google Scholar]
- 6. Rudderman RH, Mullen RL. Biomechanics of the facial skeleton. Clin Plast Surg 1992;19:11–29 [PubMed] [Google Scholar]
- 7. Donat TL, Endress C, Mathog RH. Facial fracture classification according to skeletal support mechanisms. Arch Otolaryngol Head Neck Surg 1998;124:1306–14 [DOI] [PubMed] [Google Scholar]
- 8. Laine FJ, Conway WF, Laskin DM. Radiology of maxillofacial trauma. Curr Probl Diagn Radiol 1993;22:145–88 [DOI] [PubMed] [Google Scholar]
- 9. McRae M, Frodel J. Midface fractures. Facial Plast Surg 2000;16:107–13 [DOI] [PubMed] [Google Scholar]
- 10. Ellis E, Moos K, El-Attar A. Ten years of mandibular fractures: an analysis of 2,137 cases. Oral Surg Oral Med Oral Pathol 1985;59:120–29 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.