Abstract
BACKGROUND AND PURPOSE:
Practice patterns vary widely among centers with regard to the treatment of unruptured aneurysms. The purpose of the current study was to correlate outcome data with practice patterns, specifically the proportion of unruptured aneurysms treated with neurosurgical clipping versus endovascular coiling.
MATERIALS AND METHODS:
Using the NIS, we evaluated outcomes of patients treated for unruptured aneurysms in the United States from 2001 to 2007. Hospitalizations for clipping or coiling of unruptured cerebral aneurysms were identified by cross-matching ICD codes for diagnosis of unruptured aneurysm with procedure codes for clipping or coiling of cerebral aneurysms. Mortality and morbidity, measured as “discharge to long-term facility,” were evaluated in relation to the fraction of cases treated with coils versus clipping as well as the annual number of unruptured aneurysms treated by individual hospitals and individual physicians.
RESULTS:
Markedly lower morbidity (P < .0001) and mortality (P = .0015) were noted in centers that coiled a higher percentage of aneurysms compared with the proportion of aneurysms clipped. Multivariate analysis showed that greater annual numbers of aneurysms treated by individual practitioners were significantly related to decreased morbidity (OR = 0.98, P < .0001), while the association between morbidity and the annual number of aneurysms treated by hospitals was not significant (OR = 1.00, P = .89).
CONCLUSIONS:
Centers that treated a higher percentage of unruptured aneurysms with coiling compared with clipping achieved markedly lower rates of morbidity and mortality. Our results also confirm that treatment by high-volume practitioners is associated with decreased morbidity.
S tudies of outcomes for unruptured aneurysms treated in the United States between 1996 and 2000 demonstrated that patients treated by high-volume hospitals and physicians had significantly lower morbidity and modestly lower mortality than those treated by low-volume hospitals and physicians.1,2 During the time studied by these previous publications, coiling was not as widely used as it is today. It is, therefore, important to reassess the relative risks of coiling and surgery at high- and low-volume centers with the latest data available to understand recent trends. It would also be important to know if centers that have avidly adopted endovascular coiling have different outcomes from those that have not. The purpose of the current study was to correlate outcomes data available from the NIS data base (2001–2007) with practice patterns, specifically the proportion of unruptured aneurysms treated with open clipping versus endovascular coiling.
Materials and Methods
Patients
We purchased the NIS hospital discharge data base for 2001–2007 from the HCUP of the Agency for Healthcare Research and Quality, Rockville, Maryland. The NIS is a hospital discharge data base that represents 20% of all inpatient admissions to nonfederal hospitals in the United States.
The patients included in this study were all those who had a diagnosis of unruptured aneurysm (code 437.3 in the ICD-9-CM; http://icd9cm.chrisendres.com) and a ICD-9-CM procedural code of “clipping of aneurysm” (ICD-9-CM code 39.51) or of coiling of aneurysm, which included “other repair of aneurysm” (ICD-9-CM code 39.52), “endovascular repair or occlusion of head and neck vessels” (ICD-9-CM code 39.72), and “other endovascular repair (of aneurysm) of other vessels” (ICD-9-CM code 39.79). We excluded all patients with a diagnosis of “subarachnoid hemorrhage” (ICD-9-CM code 430) and “intracerebral hemorrhage” (ICD-9-CM code 431).
Stratification of Hospital Volume
Hospital codes for each patient were available, so we were able to determine the number of unruptured aneurysms treated at each institution in a given year. We stratified hospital volume on the basis of the number of unruptured aneurysms clipped and the number of unruptured aneurysms coiled per year. For each year between 2001 and 2007, we stratified the hospitals included in the NIS data base into 4 groups based on annual volume: 1) hospitals treating ≤5 unruptured aneurysms, 2) hospitals treating 6–20 unruptured aneurysms, 3) hospitals treating 21–44 unruptured aneurysms, and 4) hospitals treating >44 unruptured aneurysms. Hospitals were assigned a separate stratification for the number of aneurysms clipped and the number of aneurysms coiled.
Stratification of Physician Volume
Physician identifiers for each patient were available, thus allowing us to determine the number of unruptured aneurysms treated by each interventionalist or neurosurgeon at each institution in a given year. For each year between 2001 and 2007, we stratified the physicians included in the NIS data base into 4 groups based on annual volume: 1) physicians treating ≤5 unruptured aneurysms, 2) physicians treating 6–10 unruptured aneurysms, 3) physicians treating 11–20 unruptured aneurysms, and 4) physicians treating >20 unruptured aneurysms. Physicians were assigned a separate stratification for the number of aneurysms clipped and the number of aneurysms coiled.
Data Collection
The major demographic factors we collected were age, race, and sex. The 2 major end points examined in this study were 1) discharge to long-term facility, which we use to define “morbidity” in the context of the current study; and 2) in-hospital mortality. Discharge to long-term facility was studied by using the HCUP variable name “DISPUNIFORM.” In-hospital mortality was studied by using the binary HCUP variable name “DIED” and calculating the number of patients who had died during their hospital stay.
Statistical Analysis
For the purposes of statistical analysis, we summed the data from 2001 to 2007 according to stratification. χ2 tests were used to compare categoric variables, and 1-way analysis of variance was used to compare continuous variables. For determining predictors of death and discharge to other than home, we performed a multivariate logistic regression analysis by using the variables of age, sex, race, treatment technique, hospital volume, and physician volume. ORs are presented as unit ORs for continuous variables such as age, hospital volume, and physician volume (ie, the OR is presented as per change in regressor during each year in the case of age and each patient treated in the case of physician/hospital volume). The weights provided in the NIS data base were not applied to statistical analysis, thus our study represents data only from hospitals that participated in the NIS data base during this time period. All statistical analysis was performed by using the SAS-based statistical package JMP (www.jmp.com).
Results
Patients
Between 2001 and 2007, a total of 10,644 patients in the NIS data base underwent treatment for unruptured aneurysms. Of these patients, hospital volume data was available for 10,624 with 5219 (49%) patients undergoing surgical clipping and 5405 patients undergoing endovascular coiling. The average age of the patients was 54.7 ± 12.6 years; 7942/10,580 (75%) of the patients were women. Race information was available for 7168 patients: 5535 were white. Patients undergoing coiling were significantly older than those undergoing clipping (56.1 ± 13.2 and 53.5 ± 11.6 years, respectively, P < .0001). There was no significant difference in the race and sex distributions between the 2 groups. Data on demographics and the number of patients treated for given hospital and physician volumes are provided in Table 1.
Table 1:
Baseline patient data for 2001–2007
| Clipping | Coiling | P | |
|---|---|---|---|
| No. | 5219 | 5405 | |
| Mean age (SD) | 53.3 (11.6) | 56.1 (13.2) | <.0001 |
| Race (No.) (%) | |||
| White | 2695 (76.2) | 2840 (78.3) | .06 |
| Black | 361 (10.2) | 359 (9.9) | |
| Hispanic | 335 (9.5) | 283 (7.8) | |
| Asian | 55 (1.6) | 70 (1.9) | |
| Native American | 18 (0.5) | 16 (0.4) | |
| Other | 75 (0.2) | 61 (1.7) | |
| Female (No.) (%) | 3878 (74.6) | 4064 (75.5) | .27 |
| Hospital volume stratification (No.) (%) | |||
| ≤5 Cases per year | 1237 (23.7) | 499 (9.2) | <.00001 |
| 6–20 Cases per year | 1996 (38.2) | 1632 (30.2) | |
| 21–44 Cases per year | 944 (18.1) | 1453 (26.9) | |
| ≥45 Cases per year | 1042 (20.0) | 1821 (33.7) | |
| Physician volume stratification (No.) (%) | |||
| ≤5 Cases per year | 1494 (49.2) | 1241 (35.8) | <.0001 |
| 6–10 Cases per year | 432 (14.2) | 488 (14.1) | |
| 11–20 Cases per year | 439 (14.5) | 611 (17.6) | |
| ≥21 Cases per year | 670 (22.1) | 1124 (32.5) |
Relative Coiling Volume and Outcomes
A strong relationship existed between the proportion of aneurysms coiled at an institution and both morbidity and mortality. As the proportion of aneurysms coiled increased, the rate of discharge to long-term facilities decreased significantly (r = 0.14, P < .0001). At centers that coiled >75%-99% of unruptured aneurysms, the rate of discharge to long-term facility was 5.9% (128/2158), compared with 16.8% (303/1195) at centers that coiled 0% of aneurysms. Patient mortality also decreased as the proportion of aneurysms coiled at an institution increased (r = 0.11, P = <.0001). Centers that coiled 0% of aneurysms had a mortality rate of 2.0% (21/1195), while centers that coiled 75%–99% of aneurysms had a mortality rate of only 0.5% (11/2158) (P = .0015). Centers that coiled 100% of unruptured aneurysms had the best outcomes with only 4.3% (27/627) of patients discharged to long-term facilities, and a mortality rate of 0.5% (2/627). These trends are demonstrated in Fig 1.
Fig 1.
Proportion of cases coiled and morbidity and mortality.
Hospital Volume and Distribution of Procedures
A majority of patients (3233/5219, 62%) who underwent clipping of their unruptured aneurysms did so at centers treating ≤20 cases/year, whereas only 39% (2131/5405) of patients who underwent coiling did so at centers treating ≤20 cases/year. Overall, patients who were coiled tended to be treated at higher volume coiling centers, whereas patients who were clipped tended to be treated at lower volume clipping centers (P < .0001). These data are summarized in Table 1.
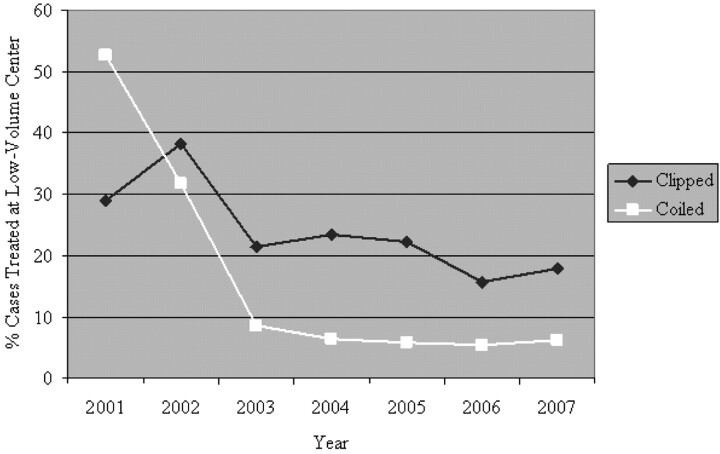
Between 2001 and 2007, there was a large decline in the proportion of patients being coiled at low-volume centers (cases per year, ≤20) compared with the proportion treated at high-volume centers (Fig 2). In 2001, 53% of coiled patients were treated at low-volume centers (cases per year, ≤20), whereas in 2007, 6.0% were coiled at low-volume centers. In 2001, 29% of clipped patients were being clipped at low-volume centers, whereas in 2007, only 18% were being clipped at low-volume centers.
Fig 2.
Percentage of cases treated at low-volume (≤20 cases/year) centers.
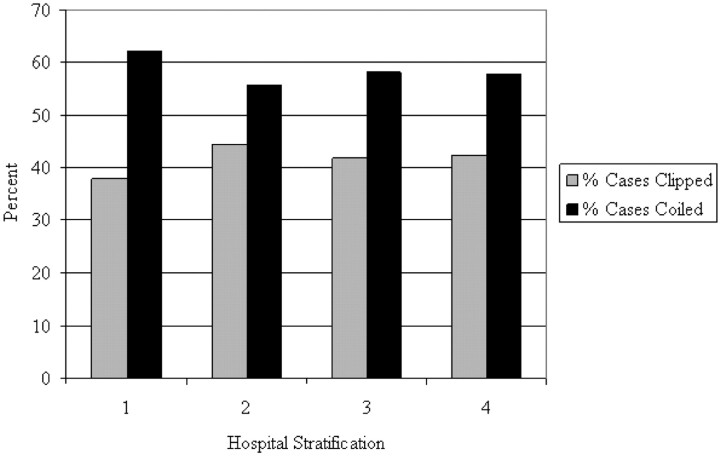
When assessing the distribution of clipping and coiling in relation to center volume, we found that for centers that practice both clipping and coiling, there was no significant difference in the distribution of clipping and coiling volumes (P = .08). These data are summarized in Fig 3.
Fig 3.
Distribution of clipping and coiling in relation to hospital volume at centers that practice both clipping and coiling: 1) hospitals treating ≤5 unruptured aneurysms, 2) hospitals treating 6–20 unruptured aneurysms, 3) hospitals treating 21–44 unruptured aneurysms, and 4) hospitals treating >44 unruptured aneurysms.
Annual Number of Unruptured Aneurysms Treated versus Death Rate and Discharge Status of Hospitals
For patients being clipped, a total of 63/5202 (1.2%) patients died during their hospitalization. There was no significant association between the number of patients who died and the hospital clipping volume (P = .14). For patients being coiled, a total of 43/5417 (0.8%) patients died during their hospitalization. No significant association was found between the number of patients who died and hospital coiling volume. Patients who were clipped were significantly more likely to die during their hospitalization than patients who were coiled (P = .03).
For patients being clipped, a total of 14.1% (735/5202) of patients were discharged to long-term facilities. There was a significant association between hospital clipping volume and discharge to long-term facilities (P < .0001) because larger volume centers had a lower proportion of patients discharged to long-term facilities than low-volume centers. Hospitals clipping ≤5 unruptured aneurysms discharged 19.2% (237/879) of patients to long-term facilities, while centers clipping ≥45 unruptured aneurysms per year discharged 11.1% (116/1042) of patients to these facilities. For patients being coiled at all centers, 5.0% (270/5417) were discharged to long-term facilities. Again, a significant association was noted between hospital volume and the proportion of patients not being discharged to home. Centers that coiled ≤5 unruptured aneurysms per year discharged 7.4% (37/499) of patients to long-term facilities, and centers coiling ≥45 unruptured aneurysms per year discharged 4.3% (78/1826) of patients to these facilities (P < .0001). Patients who were coiled were significantly less likely to be discharged to long-term facilities than those who were clipped (P < .0001). These data are summarized in Table 2.
Table 2:
Outcomes based on hospital volume
| Hospital Volume (Cases/Year) | Clipping |
Coiling |
||
|---|---|---|---|---|
| Death (No.) (%)a | Discharge to Long-Term Facility (No.) (%)b | Death (No.) (%)c | Discharge to Long-Term Facility (No.) (%)d | |
| ≤5 | 22 (1.8) | 237 (19.2) | 5 (1.0) | 37 (7.4) |
| 6–20 | 21 (1.1) | 274 (13.8) | 15 (0.9) | 86 (5.3) |
| 21–44 | 7 (0.7) | 108 (11.4) | 13 (0.9) | 69 (4.7) |
| ≥45 | 13 (1.2) | 116 (11.1) | 10 (0.5) | 78 (4.3) |
P = .14.
P < .0001.
P = .54.
P = .03.
Physician's Annual Number of Unruptured Aneurysms Treated versus Death Rate and Discharge Status
For patients being clipped, no significant association existed between the physician's volume of clipped unruptured aneurysms per year and the death rate (P = .27). There was a significant association between the physician's volume of clipped unruptured aneurysms per year and patient discharge status because physicians with the lowest volumes (≤5 cases/year) had 16.8% (248/1074) of patients discharged to long-term facilities, whereas physicians with the highest volumes (>20 cases per year) had only 11.1% (74/669) of patients discharged to long-term facilities (P = .001).
For patients being coiled, there was a significant association between the death rate and the physician's annual volume of coiled unruptured aneurysms. Practitioners who coiled ≤5 unruptured aneurysms per year had a death rate of 1.5% (19/1239), compared with physicians who coiled >20 unruptured aneurysms per year who had a death rate of 0.3% (3/1121) (P = .0005). There was also a significant association between the physician's volume and the proportion of patients being discharged home because patients treated by physicians coiling ≤5 unruptured aneurysms per year had a discharge to long-term facility rate of 6.6% (82/1239),while those who were treated by the highest volume physicians had a discharge to long-term facility rate of 3.3% (37/1124) (P < .0001). These data are summarized in Table 3.
Table 3:
Outcomes based on physician volume
| Physician Volume Stratification (Cases/Year) | Clipping |
Coiling |
||
|---|---|---|---|---|
| Death (No.) (%)a | Discharge to Long-Term Facility (No.) (%)b | Death (No.) (%)c | Discharge to Long-Term Facility (No.) (%)d | |
| ≤5 | 27 (1.8) | 248 (16.8) | 19 (1.5) | 82 (6.6) |
| 6–10 | 4 (0.9) | 58 (13.6) | 2 (0.4) | 25 (5.1) |
| 11–20 | 4 (0.9) | 53 (12.1) | 1 (0.2) | 14 (2.3) |
| ≥21 | 7 (1.0) | 74 (11.1) | 3 (0.3) | 37 (3.3) |
P = .27.
P = .001.
P = .0005.
P < .0001.
Predictors of Discharge to Other than Home and Predictors of Death
Our multivariate logistic regression analysis demonstrated that independent factors associated with discharge to long-term facilities were increased age (P < .0001), sex (male > female, P = .04), being clipped rather than coiled (P < .0001), and the number of cases per year for the practitioner (P < .0001). Total hospital volume (clipping + coiling) was not associated with discharge status based on this model.
We found the independent factors associated with in-hospital death were increased age (P = .0002), sex (male > female, P = .03), and being clipped rather than coiled (P = .01). In this model, physician volume and hospital volume were not associated with in-hospital death. These data are summarized in Table 4.
Table 4:
Results from multivariate logistic regression analysis: predictors of discharge to other than home and predictors of death
| Discharge to Long-Term Facility |
Death |
|||
|---|---|---|---|---|
| P Multivariate | OR | P Multivariate | OR | |
| Age (yr) | <.0001 | 1.1 | .0002 | 1.04 |
| Female | .04 | 0.81 | .03 | 0.56 |
| Treatment modality (coiling vs clipping) | <.0001 | 0.24 | .01 | 0.51 |
| Practitioner cases/year | <.0001 | 0.98 | .09 | 0.98 |
| Total hospital cases/year (clipping + coiling) | .89 | 1.00 | .36 | 1.00 |
Discussion
This study shows significantly lower morbidity and mortality rates among patients treated for unruptured aneurysms at centers that treated a higher percentage of patients with coiling than with clipping. Some have recommended guidelines for the treatment of unruptured intracranial aneurysms to include “microsurgical clipping rather than endovascular coiling as the first treatment choice in low-risk cases.”3 In keeping with these guidelines, it would be reasonable to expect that all patients treated with clipping in the NIS were offered clipping because the surgeon thought that it was a reasonably low-risk procedure relative to coiling. The outcomes for the NIS data base, however, suggest that outcomes of surgical clipping were less favorable than those for endovascular coiling, even when we compared hospitals and physicians with high-volume clipping with those with low-volume coiling. This finding would indicate that the guidelines recommending microsurgical clipping as the first treatment choice should be reconsidered.
We also found that outcomes of surgical clipping and endovascular coiling of unruptured intracranial aneurysms were significantly better when treatment was performed by higher volume physicians. Multivariate analysis showed that hospital volume was not an independent predictor of outcome; thus, hospital volume appears to be associated with good outcome largely because high-volume physicians work at high-volume hospitals. We have also found that treatment of unruptured aneurysms with endovascular coiling is associated with improved discharge status. This was true across all volumes. Thus, these data suggest that the best outcomes for the treatment of unruptured intracranial aneurysms are seen in those patients who are treated by high-volume physicians with endovascular coiling. With regard to surgical clipping, lower rates of adverse outcomes have been reported by high-volume surgeons4 and high-volume hospitals.5–7
Prior studies used the NIS to assess the effect of hospital volume on morbidity and mortality for unruptured aneurysm treatment from 1996–2000 for surgical clipping2 and coiling.1 For that time period, it was found that patients with unruptured aneurysms treated with both surgical clipping2 and coiling1 at high-volume centers had lower rates of discharge to sites other than home. A study of the NIS data base from 1995 to 1999 recommended that patients with cerebral aneurysms be referred to high-volume centers to improve outcomes.8 A later study by using state hospital data bases from 1998 to 2000 found that outcomes of patients admitted for subarachnoid hemorrhage were significantly better at high-volume centers compared with lower volume centers.9
Centers that are highly experienced in both clipping and coiling might offer improved outcomes because they are best suited to select the optimal treatment technique for each patient. Barker et al2 noted that the availability or frequent use of endovascular therapy at the same hospital had no effect on surgical outcome after adjustment for volume of surgical care. However, Berman et al10 and Johnston6 showed a relationship of improved outcome to endovascular availability. Johnston also showed that the availability of endovascular procedures was associated with a reduction of in-hospital death. Our study has taken a different approach, by showing that centers that preferentially offer endovascular therapy tend to have less morbidity and mortality than centers that preferentially offer surgical clipping.
The use of coiling was less widespread from 1996 to 2000 than between 2001 and 2007. Indeed, there were only 421 cases treated with coiling in the NIS during 1996–20001 compared with 5420 cases during 2001–2007. An interesting trend observed in our study is the proportion of aneurysms treated with clipping and coiling at high- and low-volume centers. From 2001 to 2007, 58% of cases clipped and 75% of cases coiled were treated in high-volume centers (>20 cases per year) versus 27% of cases clipped2 and 23% of cases coiled1 from 1996 to 2000. In our study period, 18% of clipped aneurysms were treated at low-volume hospitals (≤5 cases per year), whereas only 4% of coiled unruptured aneurysms were treated at low-volume hospitals. There is no formal process of regionalization in the United States leading to referral to higher volume centers, but it appears to be occurring without an organized effort. It is difficult to understand why it is occurring, but factors might include malpractice concerns and an overall shortage of neurosurgeons. The reason that surgical clipping appears to be the treatment mode of choice at these very low-volume centers may be that surgical clipping expertise is available but endovascular expertise is not.
Limitations
Many of the limitations of this study are intrinsic to the use of administrative data bases.11 We acknowledge that coding inaccuracies undoubtedly occur, which affect the retrospective evaluation of an administrative data base. Because our center is not included in the NIS data base, we were unable to perform an audit of our own cases to determine the degree of error in coding. Reasons that patients were discharged to long-term facilities are not collected as part of the NIS. Due to the lack of a specific code for iatrogenic subarachnoid hemorrhage, we were unable to report on unruptured aneurysms that ruptured during treatment. In addition, we are unable to determine whether discharge to a long-term facility was related to important factors such as anesthesia and pre- and postoperative care.
Another limitation associated with using an administrative data base is the retrospective nature of the data. Patients in this study were not treated in a randomized manner. Therefore, there is significant potential for selection bias that might affect outcomes of clipping or coiling. For example, the NIS does not provide data on aneurysm size and location, which can affect outcomes of treatment. In addition, there is no means of determining treatment efficacy (eg, degree of angiographic occlusion). It is possible that data on treatment efficacy may favor surgical clipping because this is considered definitive in the treatment of intracranial aneurysms. This study does not intend to provide a threshold for the number or proportion of aneurysms that should be treated with clipping or coiling to optimize outcomes, but rather it provide readers with an understanding of a general trend in outcomes during the study period.
In our study, ruptured aneurysms were not included as part of physician and hospital volume. Thus, the volume of unruptured aneurysms may not accurately represent the total volume of aneurysms that a center may treat because some physicians and medical centers may treat significantly more ruptured aneurysms than unruptured ones.
Conclusions
Centers that treated a higher percentage of unruptured aneurysms with coiling versus clipping have less morbidity and mortality. Our results also confirm that outcomes for treatment of cerebral aneurysms by higher volume practitioners is associated with decreased morbidity. Aneurysms treated with endovascular coils have significantly better outcomes than those treated with clipping regardless of hospital or physician volume. Finally, there does appear to be an element of regionalization in the treatment of unruptured intracranial aneurysms because the proportion of aneurysms coiled at higher volume centers is significantly greater than those at very-low volume centers.
Abbreviations
- HCUP
Healthcare Cost and Utilization Project
- ICD-9-CM
International Classification of Diseases, 9th Revision, Clinical Modification
- NIS
National Inpatient Sample
- OR
odds ratio
Footnotes
The authors disclose relationships to the following companies: Cardio Net, research grant for an investigator-initiated project regarding the value of ambulatory heart rhythm monitoring in patients with cryptogenic stroke (A.A.R.); eV3, Synthes, unrestricted educational grants (G.L.); Edge Therapeutics (G.L., consultant); NFocus, Sequent, Micrus, eV3, MicroVention (D.F.K.); and Mindframe, Cordis Endovascular (H.J.C.).
References
- 1. Hoh BL, Rabinov JD, Pryor JC, et al. In-hospital morbidity and mortality after endovascular treatment of unruptured intracranial aneurysms in the United States, 1996–2000: effect of hospital and physician volume. AJNR Am J Neuroradiol 2003; 24: 1409– 20 [PMC free article] [PubMed] [Google Scholar]
- 2. Barker FG, 2nd, Amin-Hanjani S, Butler WE, et al. In-hospital mortality and morbidity after surgical treatment of unruptured intracranial aneurysms in the United States, 1996–2000: the effect of hospital and surgeon volume. Neurosurgery 2003; 52: 995– 1007, discussion 1007–09 [PubMed] [Google Scholar]
- 3. Komotar RJ, Mocco J, Solomon RA. Guidelines for the surgical treatment of unruptured intracranial aneurysms: the first annual J Lawrence Pool Memorial Research Symposium—controversies in the management of cerebral aneurysms. Neurosurgery 2008; 62: 183– 93, discussion 193–184 [DOI] [PubMed] [Google Scholar]
- 4. Chyatte D, Porterfield R. Functional outcome after repair of unruptured intracranial aneurysms. J Neurosurg 2001; 94: 417– 21 [DOI] [PubMed] [Google Scholar]
- 5. Bardach NS, Zhao S, Gress DR, et al. Association between subarachnoid hemorrhage outcomes and number of cases treated at California hospitals. Stroke 2002; 33: 1851– 56 [DOI] [PubMed] [Google Scholar]
- 6. Johnston SC. Effect of endovascular services and hospital volume on cerebral aneurysm treatment outcomes. Stroke 2000; 31: 111– 17 [DOI] [PubMed] [Google Scholar]
- 7. Solomon RA, Mayer SA, Tarmey JJ. Relationship between the volume of craniotomies for cerebral aneurysm performed at New York state hospitals and in-hospital mortality. Stroke 1996; 27: 13– 17 [DOI] [PubMed] [Google Scholar]
- 8. Cowan JA, Jr, Ziewacz J, Dimick JB, et al. Use of endovascular coil embolization and surgical clip occlusion for cerebral artery aneurysms. J Neurosurg 2007; 107: 530– 35 [DOI] [PubMed] [Google Scholar]
- 9. Cross DT, 3rd, Tirschwell DL, Clark MA, et al. Mortality rates after subarachnoid hemorrhage: variations according to hospital case volume in 18 states. J Neurosurg 2003; 99: 810– 17 [DOI] [PubMed] [Google Scholar]
- 10. Berman MF, Solomon RA, Mayer SA, et al. Impact of hospital-related factors on outcome after treatment of cerebral aneurysms. Stroke 2003; 34: 2200– 07 [DOI] [PubMed] [Google Scholar]
- 11. Woodworth GF, Baird CJ, Garces-Ambrossi G, et al. Inaccuracy of the administrative database: comparative analysis of two databases for the diagnosis and treatment of intracranial aneurysms. Neurosurgery 2009; 65: 251– 56, discussion 256–57 [DOI] [PubMed] [Google Scholar]