Abstract
Aim
This cross‐sectional study sought to investigate the factors possibly related to the impact caused by the coronavirus disease 2019 pandemic in the practice of periodontists, in two countries.
Materials and methods
A total of 254 periodontists with active periodontics licensing in Brazil and the United States participated in the survey. Data were collected through an online questionnaire and the dependent variable was the perceived impact of the pandemic on periodontists' practice routines. Odds ratios were assessed by logistic regression analysis.
Results
Periodontists in private practice were 83% less likely to report a significant impact of the pandemic on their clinical routine as compared with professionals who work in the public sector or in academic institutions (CI 95%: 0.05–0.47). The financial impact of the pandemic was significantly associated with a perceived severe impact of the pandemic on their routines (OR: 1.36; CI 95%: 1.16–1.61). Professionals who have enhanced their hand‐washing routine were more likely to report a significant impact of the pandemic by 3.41 times (CI 95%: 1.28–9.04) relative to those who have not altered their hand‐washing protocols.
Conclusion
The pandemic is associated with a negative impact on the practice of periodontists, especially those working in public sectors and academic institutions.
Keywords: coronavirus infection, COVID‐19 pandemic, epidemiology, periodontal medicine, periodontics
Clinical Relevance.
Scientific rationale for the study: Despite the rapid expansion of the coronavirus disease 2019 pandemic and the large number of publications covering this event, data on the impact of the pandemic on the clinical practice of periodontists remain scarce.
Principal findings: The impact of the pandemic on the clinical practice of periodontists was deemed to be larger in association with greater financial costs and more time spent adhering to hygiene procedures.
Practical implications: As the coronavirus disease 2019 pandemic has disturbed the clinical practice of periodontists, support strategies should be suggested and implemented to help periodontists move forward.
1. INTRODUCTION
The coronavirus disease 2019 (COVID‐19) pandemic, caused by the spread of infections by a novel coronavirus, severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2), has generated a series of challenges for dental professionals to overcome and uncertainties regarding the future of the field in both public and private spheres (Ahmed et al., 2020; Goswami et al., 2020; Sharma et al., 2020).
The high rate of dissemination of the SARS‐CoV‐2 virus due to the inhalation of small airborne particles from aerosols and droplets is well‐recognized (Chen, 2020). Therefore, among health professionals, dentists are at high risk of infection (Meng et al., 2020), including particularly periodontists, because of their frequent use of ultrasound and polishing devices and other surgical instruments that generate aerosols (Holloman et al., 2015).
In response to the rapid spread of COVID‐19, dentists around the world were initially instructed to stop their activities in mid‐March 2020 and to treat patients only in cases of urgency or emergency and to focus on increasing cross‐contamination control measures (Ather et al., 2020). The return to elective activities has been carried out gradually since May 2020 and has been varied in its degree in the United States and Brazil, depending on the number of COVID‐19 cases, hospital bed capacity levels, and COVID‐19‐related deaths in each country.
In this challenging scenario, health professionals have faced drastic changes in their clinical routines, including enacting strict practices against cross‐infection, enhancing the management of minimally invasive procedures that generate less aerosols, reducing the number of patient visits (Jamal et al., 2020), and developing protocols for teleodontology services (Maret et al., 2020). Recent studies have indicated that the COVID‐19 pandemic has had not only negative economic consequences (Ali et al., 2020; Nibali et al., 2020; Schwendicke et al., 2020) but also increased the levels of fear and anxiety among the dental workforce (Ahmed et al., 2020; Chaudhary et al., 2020; Sharma et al., 2020). In this context, periodontists have been forced to adapt their clinical practice in various ways to reduce the transmission of SARS‐CoV‐2 while, at the same time, figuring out how to manage the emotional and financial impacts related to their new professional routine.
Despite the rapid growth of the COVID‐19 pandemic and the large number of publications covering this event, data on the impact of the pandemic on the clinical practice of periodontists remain scarce. Thus, the objective of this study was to investigate the possible factors associated with the perception of the impact of the COVID‐19 pandemic on the clinical practice of periodontists in Brazil and the United States.
2. MATERIALS AND METHODS
This was a cross‐sectional study whose data were collected through a self‐administered online questionnaire sent to periodontists living in Brazil and the United States. The survey was approved by the research ethics committees of the Federal University of Jequitinhonha and Mucuri Valleys (no. 4,079,814) in Brazil and the University of Florida (no. IRB202001643) in the United States.
The questionnaire was developed for this study by the authors involved and was divided into four domains as follows: the first included personal data (e.g. age, sex, dental degree, areas of living and working, working status); the second covered health conditions (comorbidities, COVID‐19 status); the third included working conditions and personal protective equipment adopted following the start of the pandemic; and the fourth encompassed the knowledge about COVID‐19 and the self‐perceived risk of infection. Brazilian Portuguese and English language versions of the questionnaire were created. The topics included in the questionnaire to assess the impact of the COVID‐19 pandemic on periodontal practice were established based on a literature review, recommendations released by the American Association of Periodontology (AAP) and Brazilian Society of Periodontology (BSP) for dental practices to consider in light of the COVID‐19 pandemic, and the authors' experiences. The questionnaire was tested for face validity by two dentists not otherwise involved in the study. The questionnaire resulting from this expert analysis was tested by five participants not involved in dentistry to assess the organization of the tool and the layout in HTML style. The Google Forms platform was used to develop the layout of the tool, which was shared with the target audience via email with members of the BSP and AAP and with different institutional stakeholders from June to July 2020. In addition, the link to access the research was shared on social media (i.e. WhatsApp, Instagram, and Facebook).
Survey respondents were required to be dentist surgeons with postgraduation periodontics experience and active registration with either the Regional Councils of Dentistry (in Brazil) or the American Board of Periodontology (in the United States); all participants were also required to agree to participate in the survey by checking the box seen during the survey related to consent. Periodontists who had ceased their professional activities more than 1 year ago, who did not complete the survey, or did not sign the consent form and dentists who responded but who did not have a certificate in periodontics were excluded. A convenience sample was used, considering all the questionnaires answered within 1 month by clinicians who met the eligibility criteria of the study.
The interest‐dependent variable was the perceived impact of the COVID‐19 pandemic on periodontal clinical practice. Periodontists were instructed to use a numerical rating scale ranging from zero to 10 points to indicate their responses, where zero points represented “no impact” and 10 points represented the “maximum impact possible.” During data analyses, the following ranges were arbitrarily determined by the research team, who made the decision based on a desired level of detail: 0 points, no impact; one to two points, very low impact; three to four points, low impact; five to six points, moderate impact; seven to eight points, significant impact; and nine to 10 points, very significant impact. Therefore, the analyses were conducted using the value of “seven points” as the cut‐off point for a “significant impact” and the survey respondents were dichotomized into “low/moderate impact” and “high (significant) impact” groups. Thus, periodontists who scored seven points or more were categorized as perceiving a significant impact of the pandemic on their clinical practice, while those who scored lower than seven points were classified as perceiving a low/moderate impact concerning the same.
In addition to information about professional performance, biosafety measures, and adjustments in professional practice routines during the pandemic, sociodemographic variables were collected from the survey respondents to verify their influence on the dental clinical routines of periodontists.
2.1. Statistical analysis
Descriptive analyses were used to describe the sociodemographic and pandemic features. Absolute and relative frequencies and mean and standard deviation values were used for the categorical independent variables. The Wilcoxon test was used to compare financial impacts between Brazil and the United States. The dependent variable was the impact value of the COVID‐19 pandemic on periodontal clinical practice. Independent variables were initially screened by univariate analysis and those with a p‐value of less than .20 were then included in the multivariate regression analysis concerning the perceived impact of COVID‐19 on periodontists' professional routines. The stepwise method assisted in selecting the variables to be included in the final impact model using the Akaike information criterion. The fit of the model was assessed using the Hosmer–Lemeshow test. Thus, the odds ratios (ORs) and 95% confidence intervals (CIs) for the impact of the pandemic as perceived by periodontists were calculated. Collinearity statistics were used to assess the possible collinearity between covariates. The R software (R Foundation for Statistical Computing, Vienna, Austria) was used in the data analysis (readxl and car packages), and p < .05 was regarded as statistically significant.
3. RESULTS
Data from 254 periodontists, including 138 from Brasil and 116 from the United States, were collected and analysed for this study. Table 1 summarizes the personal and professional profiles of periodontists included in this study. In all, 56.3% of respondents participated in training on measures aimed towards preventing the spread of SARS‐CoV‐2 and the frequency of this training was significantly higher among periodontists residing in the United States (p = .039).
TABLE 1.
Personal and professional profiles of the periodontists included in the study (n = 254)
| Characteristic | N (%) |
|---|---|
| Age, years, mean (±SD) | 47.4 (±12.8) |
| Sex | |
| Female | 119 (46.9%) |
| Male | 132 (52.2%) |
| Not reported | 3 (1.2%) |
| Country | |
| Brazil | 138 (54.3%) |
| USA | 116 (45.7%) |
| Belonging to the COVID‐19 risk group | |
| Yes | 96 (37.8%) |
| No | 157 (61.8%) |
| Current professional status | |
| Active periodontist only | 204 (80.3%) |
| Periodontist plus general dentist | 18 (7.1%) |
| Periodontist teaching in academic institution | 60 (23.6%) |
| Unemployed | 2 (0.8%) |
| Type of specialty training | |
| Specialization/residency | 90 (35.4%) |
| Master's degree | 45 (17.7%) |
| Doctorate degree | 47 (18.5%) |
| Length of experience as a periodontist | |
| <1 year | 5 (2.0%) |
| 1–5 years | 13 (5.1%) |
| >5 years | 78 (30.7%) |
| Not reported | 158 (62.2%) |
| Other specialty training than periodontics | |
| Yes | 127 (50.0%) |
| No | 112 (44.1%) |
| Not reported | 15 (5.9%) |
| COVID‐19 disease status | |
| Reported positive test for COVID‐19 | 9 (3.5%) |
| Confirmed cases in the region where they reside | 237 (93.3%) |
| Social isolation measures in their municipality of residence | |
| No social isolation measures enacted | 13 (5.1%) |
| Vertical or horizontal isolation | 191 (75.2%) |
| Lockdown | 45 (17.7%) |
Abbreviations: COVID‐19 risk group include at least one following factor: elderly (≥60 years old), diabetic, hypertensive, pregnant women, patients with heart disease, patients with pulmonary/respiratory diseases, chronic kidney disease, immunosuppression, obese, smokers; COVID‐19: coronavirus disease 2019.
The most commonly used personal protective equipment in periodontal care after the start of the pandemic were disposable procedure gloves (82.7%) and face shields (81.2%), while the least commonly used equipment were overalls (12.2%) and waterproof jackets (26.3%). A greater degree of difficulty than usual in purchasing this equipment due to the pandemic was reported by a majority of dentists (66.1%), with no significant difference in the level of difficulty found between Brazil and the United States (p = .332). The adjustments (and respective frequencies) made by periodontists in their work routine after the beginning of the pandemic are described in Table 2.
TABLE 2.
Frequency of adjustments made by periodontists in their clinical practice following the beginning of the pandemic (n = 254)
| Characteristic | N (%) |
|---|---|
| Change in clinical routine | |
| Adjustments of the working environment | 188 (74.0) |
| Disinfection of the working environment | 188 (74.0) |
| Increased use of PPE | 203 (79.9) |
| Incorporation of preliminary remote patient screening | 182 (71.7) |
| Enhanced personal hygiene | 185 (72.8) |
| Adjustments of clinical procedures | 171 (67.3) |
| Reduction of working hours | 2 (0.8) |
| Incorporation of teledentistry | 31 (12.2) |
| Precautionary measures in sorting | |
| Use of a specific questionnaire for COVID‐19 to screen patients in person | 124 (48.8) |
| Use of a specific questionnaire for COVID‐19 for remote patient screening | 108 (42.5) |
| Temperature measurement at the dental clinic | 148 (58.3) |
| Request for patients to check their temperature before going to the dental clinic | 41 (16.1) |
| Mouthwash with antimicrobial use in the dental clinic | 179 (70.5) |
| Mouthwash with antimicrobial use before arriving at the dental clinic | 16 (6.3) |
| Change in periodontal procedures | |
| Pre‐ and postoperative mouthwash | 175 (68.9) |
| Use of high‐volume suction | 168 (66.1) |
| Performance of minimally invasive and conservative procedures | 121 (47.6) |
| Use of handpieces or other devices connected to the air/water lines only when indispensable | 147 (57.9) |
| Use of reinforced disinfection, sterilization, and protection of all potentially contaminated surfaces and equipment | 189 (74.4) |
| Replacement of intra‐oral radiographic techniques by extraoral techniques | 19 (7.5) |
| Implementation of sutures with resorbable threads | 36 (14.2) |
| Remote assistance used during the pandemic | |
| 90 (35.4) | |
| 27 (10.6) | |
| Telephone call | 94 (37.0) |
| Video conference | 18 (7.1) |
Abbreviations: COVID‐19, coronavirus disease 2019; PPE, personal protective equipment.
Regarding the impact of COVID‐19 on periodontists' professional routine, 50% of periodontists reported seeing a mean of 10 patients per day before the pandemic and a mean of five patients after the start of the pandemic, for a difference that was statistically significant (p < .001). The financial impact assessed by professionals on a scale ranging from zero (no impact) to 10 (maximum impact) points averaged 7.97 (± 2.26) points, with 50% of participants rating the financial impact as greater than eight points. The level of financial impact (p < .001), the perceived impact on the current clinical routine (p = .002), and the perspective on the future of clinical practice (p = .008) were statistically higher among dentists residing in Brazil than those residing in the United States (Figure 1).
FIGURE 1.
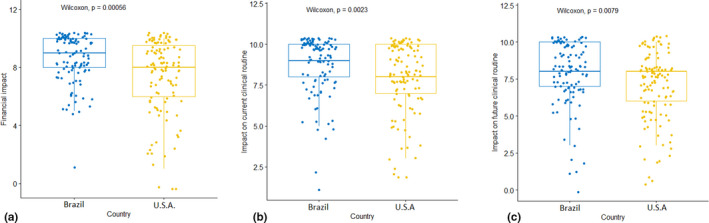
Comparison of periodontists' perceptions of the impact of the COVID‐19 pandemic between Brazil and the United States. (a) Perceived impact of the pandemic on the routine financial costs of periodontists in Brazil and the United States. (b) Perceived impact of the pandemic on the current routine of periodontists in Brazil and the United States. (c) Perceived impact of the pandemic on the daily future practice of periodontists in Brazil and the United States. Analysis was performed by Wilcoxon's non‐parametric test and p‐values of less than .05 indicated statistical differences in the impacts observed by periodontists between countries
In the univariate analyses, the financial impact due to the pandemic and changes in the clinical routine, such as the need to alter the work environment, the intensification of hand‐washing, and the need to modify clinical procedures, were significantly associated with periodontists perceiving the COVID‐19 pandemic to have had a significant impact on their clinical practice (Table 3).
TABLE 3.
Univariate analysis of factors related to periodontists' perceptions of the impact of the COVID‐19 pandemic on professional practice (n = 254)
| Variable | Low/moderate impact (n = 64) | High impact (n = 191) | p‐value | OR (CI 95%) |
|---|---|---|---|---|
| Sex | ||||
| Female | 33 (27.7%) | 86 (72.3%) | .327 | 1 |
| Male | 31 (23.5%) | 99 (76.5%) | 1.31 (0.76–2.28) | |
| Age group | ||||
| 22–59 years | 51 (25.5%) | 149 (74.5%) | .943 | 1 |
| 60–78 years | 12 (24.0%) | 38 (76.0%) | 1.02 (0.50–2.19) | |
| Country | ||||
| Brazil | 40 (29.0%) | 98 (71.0%) | .151* | 1 |
| USA | 24 (20.7%) | 92 (79.3%) | 0.65 (0.36–1.16) | |
| Confirmed cases of COVID‐19 in the municipality of residence | ||||
| No | 1 (10.0%) | 9 (90.0%) | .271 | 1 |
| Yes | 62 (26.2%) | 173 (73.8%) | 0.31 (0.01–1.69) | |
| Social isolation measures in the municipality of residence | ||||
| None | 5 (38.5%) | 8 (61.5%) | .124* | 1 |
| Isolation | 48 (25.1%) | 143 (74.9%) | 1.83 (0.53–5.77) | |
| Lockdown | 8 (17.8%) | 37 (82.2%) | 2.89 (0.71–11.28) | |
| Acting as a periodontist in | ||||
| Academic institution or public service | 22 (47.8%) | 24 (52.2%) | <.001 a , * | 1 |
| Private clinic | 31 (23.0%) | 104 (77.0%) | 3.01 (1.49–6.13) | |
| Two or more services | 9 (13.0%) | 60 (87.0%) | 6.11 (2.53–15.82) | |
| Difficulty in purchasing PPE | ||||
| No | 7 (13.5%) | 45 (86.5%) | .627 | 1 |
| Yes | 27 (16.1%) | 141 (83.9%) | 0.80 (0.30–1.87) | |
| Remote prescription | ||||
| No | 13 (13.5%) | 83 (86.5%) | .506 | 1 |
| Yes | 21 (16.5%) | 106 (83.5%) | 0.77 (0.35–1.62) | |
| Changes in clinical routine | ||||
| No alterations to the work environment | 10 (29.4%) | 24 (70.6%) | .017 a , * | 1 |
| Alterations in the work environment | 24 (12.8%) | 162 (87.2%) | 2.81 (1.16–6.50) | |
| No change in the disinfection routine of the work environment | 7 (20.6%) | 27 (79.4%) | .370 | 1 |
| Intensification of the disinfection of the work environment | 27 (14.4%) | 161 (85.6%) | 1.52 (0.56–3.70) | |
| No change in/routine use of PPE | 4 (21.1%) | 15 (78.9%) | .482 | 1 |
| Increased use of PPE | 30 (14.8%) | 173 (85.2%) | 1.52 (0.41–4.53) | |
| No change in patient screening | 7 (17.5%) | 33 (82.5%) | .692 | 1 |
| Remote patient screening | 27 (14.8%) | 152 (85.2%) | 1.20 (0.45–2.86) | |
| Service hours unchanged | 33 (15.0%) | 187 (85.0%) | .227 | 1 |
| Alteration of the service hours | 1 (50.0%) | 1 (50.0%) | 0.17 (0.00–4.58) | |
| Maintenance of the same hand‐washing routine | 13 (35.1%) | 24 (64.9%) | <.001 a , * | 1 |
| Intensified hand‐washing routine | 21 (11.4%) | 164 (88.6%) | 4.17 (1.82–9.40) | |
| Maintenance of the same clinical procedures | 13 (25.5%) | 38 (74.5%) | .026 a , * | 1 |
| Alteration of the clinical procedures | 21 (12.3%) | 150 (87.7%) | 2.41 (1.08–5.21) | |
| Financial impact (±SD) | 6.38 (± 2.45) | 8.25 (± 2.12) | <.001 a , * | 1.34 (1.16–1.56) |
Abbreviations: CI, confidence interval; COVID‐19, coronavirus disease 2019; OR, odds ratio; PPE, personal protective equipment.
Lower case numbers drove statistical differences in the perception of a significant impact between the variables reported by periodontists (p < .05).
p < .20 included in the multivariate regression analysis.
Table 4 shows the results of the multivariate logistic regression analysis performed after including the variables that were added to the final model. Dental professionals who work in the private sector showed an 83% lower chance of reporting a significant impact of the COVID‐19 pandemic on their clinical routine as compared with those working in the public service sector or academic institutions. The impact of the pandemic on the finances of dental practices was significantly associated with a perceived significant impact of the pandemic (OR: 1.36; 95% CI: 1.16–1.61). Finally, professionals who enhanced their hand‐washing routine were more likely to report a significant impact of the pandemic by 3.41 times (95% CI: 1.28–9.04) relative to those who have not changed their hygiene routine in this manner. The ORs for social isolation and clinical procedure adaptation were not statistically associated with the perception of a significant impact of the pandemic. The p‐value for the Hosmer and Lemeshow test was .22.
TABLE 4.
Multiple logistic analysis of factors related to periodontists' perceptions of the impact of the COVID‐19 pandemic on professional practice (n = 254)
| Variable | b | SE(b) | p‐value | OR | 95% CI |
|---|---|---|---|---|---|
| Social isolation | 0.36 | 0.46 | .428 | 1.44 | 0.56–3.52 |
| Professional practice in sector private | −1.75 | 0.55 | .001* | 0.17 | 0.05–0.47 |
| Financial impact of the pandemic | 0.31 | 0.08 | <.001* | 1.36 | 1.16–1.61 |
| Intensification of hand‐washing habits | 1.22 | 0.49 | .012* | 3.41 | 1.28–9.04 |
| Alteration of clinical procedures | 0.46 | 0.47 | .319 | 1.59 | 0.61–3.98 |
Abbreviations: CI, confidence interval; COVID‐19, coronavirus disease 2019; OR, odds ratio; SE, standard error.
Variables statistically associated with periodontists' perceptions of the COVID‐19 having a significant impact on clinical practice (p < .05).
4. DISCUSSION
In light of the COVID‐19 pandemic, health professionals, especially dentists, have adopted new approaches to patient care. Adjustments made by dental practices worldwide were necessary to contain the spread of the virus and protect both clinicians and patients alike from possible contamination in the workplace (Ather et al., 2020), leading to a significant impact on the routine of dentists. The present study clearly demonstrated that the perception of a significant impact reported by periodontists was associated with the number of changes that occurred in their clinical practice in response to the pandemic. The intensification of hand‐washing and the financial effect suffered by periodontists as well as the type of sector to which the periodontist belongs were significantly associated with the perception of a significant impact of the COVID‐19 pandemic.
It is important to mention that there has been no effective level of control of the spread of SARS‐CoV‐2 attained in either country examined here to date and that a long interruption of services could generate an imminent economic crisis for dental professionals (Farooq & Ali, 2020; Nicola et al., 2020) and inappropriate or inadequate patient care. However, during the time of our survey, some states had resumed routine dental activities due to lessened case counts with special provisions in place. Thus, despite the worrying health crisis being experienced worldwide and the strict guidelines provided by the BSP and AAP, periodontists polled here did report a continuation of patient care, albeit to a reduced degree, with their service hours remaining unchanged during the pandemic. The high rate of confirmed cases of COVID‐19 in the region of residence (93.3%), the inclusion of measures of social distancing, and the fear of contamination could lead to a reduced demand for dental care by the population and reduced working hours by professionals, negatively impacting both the short‐ and long‐term financial stability of the dental practice and the quality of life of the health care workers.
To provide dental care safely until a vaccine is readily available and administered to an adequate degree, health professionals must be diligent about following new protocols, including the use of personal protective equipment, establishing changes in work routine, and intensifying biosecurity measures. The introduction of these practices was reported by most of the periodontists who responded to the survey in both countries (Tables 2 and 3). It is supposed that such measures may have financial implications, as was previously reported by a recent Brazilian study (Cavalcanti et al., 2020). Furthermore, the difficulty in acquiring common personal protective equipment due to its scarcity and exorbitant cost on the market, as demonstrated recently (Chamorro‐Petronacci et al., 2020; Consolo et al., 2020) and reported by 66.1% of the periodontists in this study, is another negative factor to take into consideration in securing clinical practice after the pandemic.
In this context, the results of this study demonstrate that a financial impact was felt by periodontists in both countries, with a statistically significantly higher negative impact on the current routine and with consideration of the future of the clinical practice reported by those in Brazil. It was also concluded that the perception of a significant impact of the COVID‐19 pandemic in clinical practice was related to the financial impact suffered. The difference observed between Brazil and the United States may be linked to variations in economic stability and the cost of living between the two countries as well as to the average monthly salary of the survey respondents.
Another factor associated with the perception of a significant impact of the pandemic in clinical practice was related to changes in the clinical routine adopted by periodontists after the spread of SARS‐CoV‐2 began. According to our results, adjustments made by periodontists to their routine after the start of the pandemic were consistent with those reported by other studies (Ather et al., 2020; Farooq & Ali, 2020) and followed the guidelines proposed by health organizations (Barabari & Moharamzadeh, 2020) to avoid the spread of the disease and minimize the risk of contamination of health professionals and patients. It is noteworthy that the majority of periodontists from both countries reported following most of the COVID‐19–related recommendations for dental practices released by the AAP and BSP, which took into consideration the guidance from the Centers for Disease Control and Prevention, the World Health Organization, and the American Dental Association (Tables 2 and 3). Such recommendations include conducting screenings of patients and visitors, focusing on a history of international travel and symptoms of acute respiratory illness (e.g. fever, cough, having difficulty with breathing), performing temperature readings, adopting proper use of PPE, inventorying available PPE, use of high‐speed evacuation equipment by all dental procedures producing aerosols, having patients rinse with 1% hydrogen peroxide before each appointment, encouraging sick employees to stay home, implementing strategies to prevent patients who can be cared for at home from coming to the dental facility (e.g. use of telephone systems, telemedicine technologies, self‐assessment tools, or the dental practice's website or social media pages (Jamal et al., 2020; Maret et al., 2020).
The univariate analyses in the present study demonstrated that there were differences in the perception of impact by the periodontists who adapted their work environment in an attempt to make it safer and those who adapted clinical procedures to reduce aerosol generation when compared with those who did not (p = .017 and p = .026, respectively). However, in the multivariate analysis, the perception of a significant impact of the COVID‐19 pandemic on clinical practice was not related to the adjustment of periodontal clinical procedures. Therefore, it seems that most periodontists did not consider altering procedures to minimize the dispersion of aerosols as a priority in the pandemic period.
On the other hand, those periodontists who intensified their hand‐washing habits demonstrated a greater chance of reporting a significant impact of COVID‐19 on their clinical practice. In fact, more frequent and thorough hand‐washing and disinfection have become imperative practices during the COVID‐10 pandemic for inactivation of the SARS‐CoV‐2 virus and the reduction of contamination. Therefore, the enhancement of hand‐washing protocols during the work routine was the most immediate and noticeable change in clinical practice noted by the periodontists of both countries after the start of the COVID‐19 pandemic.
Moreover, this study identified that periodontists who work only in the private sector are more likely to report a smaller impact of the pandemic on the clinical practice as compared with those who work in the public sector, an academic institution, or in two or more service sectors. As many academic institutions have adopted remote education measures (Elangovan et al., 2020) and public sectors have developed teleconsultation guidelines (Maret et al., 2020), the greater impact reported among those in the public and academic sectors here may be due to the smaller number of patients and non‐urgent procedures seen in these locations as a result of restrictions imposed by governments and organizations like the BSP and AAP. Contrary to the findings of this study, recent studies (Barabari & Moharamzadeh, 2020; Consolo et al., 2020) have reported a greater impact of the COVID‐19 pandemic on the private sector and showed that about 100% of the periodontists interviewed closed their practices at the time of the initial outbreak, experiencing a negative impact on their work routine. Therefore, the actual short‐ and long‐term effects of the COVID‐19 pandemic on periodontists working in the public and private sectors need to be better elucidated by future studies focusing on this topic.
Despite the relevance of the findings in this study, some limitations should be highlighted. Since this was a cross‐sectional study, no causal relationship can be evaluated here; instead, only associations between individual factors and the perception of the impact of the pandemic on clinical practice may be assessed. Another limitation is the use of a self‐applied online questionnaire and a possible degree of bias in the recruitment of participants. Despite the ease of dissemination of the questionnaire due to the current benefits of virtual technology, the response rate was incredibly low and our convenience sample was smaller than expected. However, important factors related to the COVID‐19 impact on the clinical practice of periodontists in the United States and Brazil were identified, despite our small study sample size. Moreover, high and low perceptions of the impact of the pandemic were grouped according to an arbitrary cut‐off point established by the study team. Finally, considering the broad way in which the questionnaire was distributed, unfortunately, there was no control over how many periodontists were approached. Likewise, it is not known whether the demographic data of the population that responded to the survey is representative of the general population of periodontists from both countries.
5. CONCLUSIONS
The COVID‐19 pandemic has driven significant changes to occur in the routine of periodontists in both Brazil and the United States. The main factors associated to the perception of periodontists of the impact of the COVID‐19 pandemic on clinical practice were the financial effect of the pandemic and the intensification of hand‐washing habits. Such consequences were more impactful among periodontists working in the public sector and academic institutions.
CONFLICT OF INTEREST
The authors state that there are no conflicts of interest to report in connection with this article.
AUTHOR CONTRIBUTIONS
Gabriela Rocha‐Gomes: conceived and designed the study, acquired the data, drafted the article, and provided final approval of the manuscript.Olga D Flecha: conceived and designed the study, revised the article critically for important intellectual content, and provided final approval of the manuscript. Tamires S Miranda, Poliana M Duarte, and Luciana M Shaddox: acquired the data, revised the article critically for important intellectual content, and provided final approval of the manuscript. Endi L Galvão: conceived and designed the study, analysis and interpretation of data, drafted the article and revised it critically for important intellectual content, and provided final approval of the manuscript. Patricia F Gonçalves: conceived and designed the study, analysed and interpreted the data, revised the article critically for important intellectual content, and provided final approval of the manuscript.
ACKNOWLEDGMENTS
The authors thank CAPES for supporting academic and professional development. We also offer our deepest thanks to the Programa de Pós‐graduação em Odontologia (PPGOdonto), Universidade Federal dos Vales do Jequitinhonha e Mucuri, which provided technical support for the development and implementation of this study.
Funding information
This study was financed in part by Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES) (finance code 001). The funder had no role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript.
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.
REFERENCES
- Ahmed, M. A. , Jouhar, R. , Ahmed, N. , Adnan, S. , Aftab, M. , Zafar, M. S. , & Khurshid, Z. (2020). Fear and practice modifications among dentists to combat novel coronavirus disease (COVID‐19) outbreak. International Journal of Environmental Research and Public Health, 17(8), 2821. 10.3390/ijerph17082821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ali, S. , Farooq, I. , Abdelsalam, M. , & AlHumaid, J. (2020). Current clinical dental practice guidelines and the financial impact of COVID‐19 on dental care providers. European Journal of Dentistry, 14(S 01), S140–S145. 10.1055/s-0040-1716307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ather, A. , Patel, B. , Ruparel, N. B. , Diogenes, A. , & Hargreaves, K. M. (2020). Coronavirus disease 19 (COVID‐19): Implications for clinical dental care. Journal of Endodontics, 46(5), 584–595. 10.1016/j.joen.2020.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barabari, P. , & Moharamzadeh, K. (2020). Novel Coronavirus (COVID‐19) and Dentistry‐A Comprehensive Review of Literature. Dent J (Basel), 8. 10.3390/dj8020053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cavalcanti, Y. W. , Silva, R. O. D. , Ferreira, L. D. F. , Lucena, E. H. G. D. , Souza, A. M. L. B. D. , Cavalcante, D. D. F. B. , Meneghim, M. D. C. , & Pereira, A. C. (2020). Economic impact of new biosafety recommendations for dental clinical practice during COVID‐19 pandemic. Pesquisa Brasileira em Odontopediatria e Clínica Integrada, 20(supp1), 1–9. 10.1590/pboci.2020.143. [DOI] [Google Scholar]
- Chamorro‐Petronacci, C. , Martin Carreras‐Presas, C. , Sanz‐Marchena, A. , A Rodríguez‐Fernández, M. , María Suárez‐Quintanilla, J. , Rivas‐Mundiña, B. , Suárez‐Quintanilla, J. , & Pérez‐Sayáns, M. (2020). Assessment of the economic and health‐care impact of COVID‐19 (SARS‐CoV‐2) on public and private dental surgeries in Spain: A pilot study. International Journal of Environmental Research and Public Health, 17(14), 5139. 10.3390/ijerph17145139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chaudhary, F. A. , Ahmad, B. , Ahmad, P. , Khalid, M. D. , Butt, D. Q. , & Khan, S. Q. (2020). Concerns, perceived impact, and preparedness of oral healthcare workers in their working environment during COVID‐19 pandemic. Journal of Occupational Health, 62(1), e12168. 10.1002/1348-9585.12168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen, J. (2020). Pathogenicity and transmissibility of 2019‐nCoV‐A quick overview and comparison with other emerging viruses. Microbes and Infection, 22(2), 69–71. 10.1016/j.micinf.2020.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Consolo, U. , Bellini, P. , Bencivenni, D. , Iani, C. , & Checchi, V. (2020). Epidemiological aspects and psychological reactions to COVID‐19 of dental practitioners in the Northern Italy districts of Modena and Reggio Emilia. International Journal of Environmental Research and Public Health, 17(10), 3459. 10.3390/ijerph17103459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elangovan, S. , Mahrous, A. , & Marchini, L. (2020). Disruptions during a pandemic: Gaps identified and lessons learned. Journal of Dental Education, 84(11), 1270–1274. 10.1002/jdd.12236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farooq, I. , & Ali, S. (2020). COVID‐19 outbreak and its monetary implications for dental practices, hospitals and healthcare workers. Postgraduate Medical Journal, 96(1142), 791–792. 10.1136/postgradmedj-2020-137781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goswami, M. , Sharma, S. , Kumar, G. , Gogia, M. , Grewal, M. , Garg, A. , Bhardwaj, S. , Vignesh, R. P. , Narula, V. , & Bidhan, R. (2020). Dealing with “coronavirus pandemic”: A dental outlook. International Journal of Clinical Pediatric Dentistry, 13(3), 269–278. 10.5005/jp-journals-10005-1757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holloman, J. L. , Mauriello, S. M. , Pimenta, L. , & Arnold, R. R. (2015). Comparison of suction device with saliva ejector for aerosol and spatter reduction during ultrasonic scaling. The Journal of the American Dental Association (1939), 146(1), 27–33. 10.1016/j.adaj.2014.10.001. [DOI] [PubMed] [Google Scholar]
- Jamal, M. , Shah, M. , Almarzooqi, S. H. , Aber, H. , Khawaja, S. , El Abed, R. , Alkhatib, Z. , & Samaranayake, L. P. (2020). Overview of transnational recommendations for COVID‐19 transmission control in dental care settings. Oral Diseases, 00, 1–10. 10.1111/odi.13431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maret, D. , Peters, O. A. , Vaysse, F. , & Vigarios, E. (2020). Integration of telemedicine into the public health response to COVID‐19 must include dentists. International Endodontic Journal, 53(6), 880–881. 10.1111/iej.13312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meng, L. , Hua, F. , & Bian, Z. (2020). Coronavirus disease 2019 (COVID‐19): Emerging and future challenges for dental and oral medicine. Journal of Dental Research, 99(5), 481–487. 10.1177/0022034520914246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nibali, L. , Ide, M. , Ng, D. , Buontempo, Z. , Clayton, Y. , & Asimakopoulou, K. (2020). The perceived impact of Covid‐19 on periodontal practice in the United Kingdom: A questionnaire study. Journal of Dentistry, 102, 103481. 10.1016/j.jdent.2020.103481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nicola, M. , Alsafi, Z. , Sohrabi, C. , Kerwan, A. , Al‐Jabir, A. , Iosifidis, C. , Agha, M. , & Agha, R. (2020). The socio‐economic implications of the coronavirus pandemic (COVID‐19): A review. International Journal of Surgery (London, England), 78, 185–193. 10.1016/j.ijsu.2020.04.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwendicke, F. , Krois, J. , & Gomez, J. (2020). Impact of SARS‐CoV2 (Covid‐19) on dental practices: Economic analysis. Journal of Dentistry, 99, 103387. 10.1016/j.jdent.2020.103387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharma, S. , Parolia, A. , & Kanagasingam, S. (2020). A review on COVID‐19 mediated impacts and risk mitigation strategies for dental health professionals. European Journal of Dentistry, 14(S 01), S159–S164. 10.1055/s-0040-1718240. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.


