Abstract
Introduction
The use of telemedicine in oncology practice is rapidly expanding and is considered safe and cost effective. However, the implications of telemedicine on patient‐physician interaction, patient satisfaction, and absence of the personal touch have not been studied to date. Following the spread of COVID‐19, telemedicine services were rapidly incorporated at the Oncology Division of Tel Aviv Medical Center. We aimed to evaluate patients' perspectives and preferences regarding telemedicine and to assess whether this virtual communication platform affects the patient‐physician relationship.
Methods
Between March 2020 and May 2020, adult cancer patients who conducted at least one successful telemedicine meeting were interviewed by trained medical personnel. The interview was based on validated patient satisfaction questionnaires and focused on patient‐physician interaction in relation to the last in‐patient visit.
Results
Of 236 patients, 172 (74%) patients agreed to participate. The study population comprised mainly patients with gastrointestinal malignancies (n = 79, 46%) with a median age of 63 years (range 21–88). The majority of patients were male (n = 93, 54%). Eighty‐nine (51.7%) patients were receiving active oncologic treatment, and 58 (33.7%) were under routine surveillance following completion of active therapy. Almost all had a sense of secured privacy (n = 171, 96%), the majority of patients affirmed that their concerns were met (n = 166, 93%) and perceived that eye contact with the treating physician was perceived (n = 156, 87%). Only a minority felt that the absence of physical clinic visits harmed their treatment (n = 36, 20%). Most patients (n = 146, 84.9%) wished to continue telemedicine services. A multivariate analysis revealed that higher satisfaction and visits for routine surveillance were both predictors of willingness to continue future telemedicine meetings over physical encounters (odds ratio [OR] = 2.41, p = .01; OR = 3.34, p = .03, respectively).
Conclusion
Telemedicine is perceived as safe and effective, and patients did not feel that it compromised medical care or the patient‐physician relationship. Integration of telemedicine is ideal for patients under surveillance after completion of active oncologic treatment. Physician communication skills workshops are warranted with implementing this platform.
Implications for Practice
During the COVID‐19 pandemic, telemedicine was rapidly implemented worldwide to facilitate continuity of quality care and treatment. Despite many potential setbacks, telemedicine has become a useful and safe tool for oncology practitioners to care for their patients. The use of telemedicine regarding patients' perspectives, emotions, and patient‐physician communication in daily oncology practice has not been studied to date. This study demonstrated telemedicine is perceived as safe and effective and does not compromise medical care or the patient‐physician relationship. Its use is ideal for surveillance after completion of active oncologic treatment. Physician communication skills workshops are warranted with implementing this platform.
Keywords: Telemedicine, COVID‐19, Cancer, Quality care
Short abstract
The use of telemedicine in oncology practice is rapidly expanding; however, the implications for patient‐physician interaction and patient satisfaction have not been well studied. This article evaluates patients' perspectives and preferences regarding telemedicine and whether a virtual communication platform affects the patient‐physician relationship.
Introduction
The telemedicine platform provides virtual communication, bridging health services and medical care disparities among select patient populations. The use of telemedicine has expanded in the practice of family medicine [1, 2] and primary care [3] and has been accredited with favorable results concerning patients' preferences [4, 5, 6] and cost‐effectiveness [7, 8]. Among health care centers worldwide, telemedicine may refer to telephone, computer‐based audio encounters, mobile phone video applications, and remote symptom and vitals reporting transmitting health care information to the treating physician. The National Institutes of Health defines telemedicine as the use of technology to provide and support health care at a distance [9]. The physical examination may be accomplished virtually, including listening to the patient and assembling a careful history to guide physical subtleties from a limited, but potentially impressionable, patient‐assisted physical examination [10].
Until recently, telemedicine service among oncology patients has been limited to serve mainly those unable to physically visit the clinic because of remote distance (e.g., those living in isolated rural areas [11, 12]) and underprivileged populations [13]. High‐quality care and better overall outcome of cancer patients require care by a multidisciplinary team. Telemedicine enables real‐time direct patient interaction and allows videoconferencing sessions with transmission of laboratory, imaging, and pathology data. Adoption of telemedicine includes remote monitoring of therapy side effects [14, 15], management of patients' symptoms [16], providing palliative care [17], enrollment and follow‐up assessment in clinical trials [18, 19], and psychological support [20].
A recent study showed that oncology patients receiving palliative care favored telemedicine visits and attributed their preference to the increased comfort and safety of their homes [21, 22]. Importantly, these visits allowed personalized care, improved quality of life [23, 24], and instilled greater confidence and support to patients' family members [25]. Telemedicine was also useful among patients with rare cancers who live far from specialized cancer centers [26].
A major concern regarding the adoption of telemedicine is possible compromise of patient‐ physician interaction [27]. Although some believe telemedicine will alter these relations [28, 29], there is virtually no evidence that patient‐physician communication using telemedicine is jeopardized. Major issues include privacy and security concerns [30] compounded by a possible breach in patients' trust, which potentially could limit patients' disclosure and cooperation with the adoption of telemedicine [31]. Although some encounters of oncology patients may be regarded as more bureaucratic, dealing mostly with procedural administrative issues such as referral to various tests or providing prescriptions, other encounters are significantly more emotive and involve subtle and sensitive discussions relaying difficult messages involving prognosis and treatment plans to patients and their families. The use of telemedicine in these complex and impressionable situations remains to be established.
During the COVID‐19 pandemic, telemedicine rapidly evolved as an unprecedented integral channel of communication and was implemented to facilitate continuity of quality care and treatment [32]. Despite many potential setbacks, including the inability to complete physical examination, restricted access to vulnerable populations with limited digital literacy, such as rural residents, ethnic minorities, elderly patients, low socioeconomic status, or lack of English proficiency [33], telemedicine has become a useful tool for oncology practitioners to care for their patients while ameliorating the risks involved with in‐patient visits [34].
Following the outbreak of the COVID‐19 pandemic in Israel and the implementation of social distancing regulations, the Oncology Division at Tel Aviv Medical Center (TLVMC) rapidly adopted the telemedicine platform as a substitute for in‐person visits to the clinic. We anticipated obstacles in the absence of face‐to‐face meetings and also in the delivery of bad news [35]. We therefore aimed to examine our patients' perspectives, sense of assurance, and satisfaction regarding the telemedicine platform.
Materials and Methods
Patient Population
A survey was conducted between March to May 2020 among adult patients with cancer treated at the Oncology Division of TLVMC after completing at least one telemedicine meeting using a mobile phone video application that enables patients to transfer medical documents. During the pandemic, all patient encounters were converted to virtual telemedicine meetings. Physical arrival to the hospital was limited to interested patients or by request of treating physician. The video telemedicine encounters were scheduled by administrative personnel and conducted by attending physicians. In an effort to avoid confounding factors affecting the experience of the telemedicine meetings, patients who encountered technical constraints in launching the program or were interrupted by technical malfunctions were excluded.
During the study period, 232 patients at TASMC were approached, and 172 respondents (74%) agreed to participate. Of these patients, 23% encountered technical difficulties, which excluded them from our study. Technical obstacles included lack of a smartphone, trouble downloading the application, and other technical obstacles such as internet failure and video and microphone malfunction.
The study was approved by the Institutional Review Board.
The Survey
The survey was based on patient satisfaction questionnaires [36, 37] and conducted via telephone by dedicated trained personnel. Each interview lasted approximately 10 minutes. The questionnaire was first validated using a pilot study among 20 patients. The survey addressed patients' telemedicine experience by assessing demographic information (three items), previous mode of arrival to the hospital (three items), user interface (seven items), the patient‐physician interaction in relation to the last in‐person visit (five items), and the physicians' humane approach and empathy (two items). Lastly, patients were asked if they were willing to continue telemedicine visits after the pandemic and the reasoning for their responses.
Data Sources
Data of patient demographics, clinical diagnosis, and visit intent were included in the questionnaire. Clinical data collection regarding the primary tumor was extracted and confirmed from the hospital medical records.
Statistical Analysis
Data were analyzed using descriptive statistics. Categorical variables were expressed as frequencies and percentages. The chi‐square test was used to evaluate the association between categorical variables. Univariate and multivariate logistic regression models were used to evaluate the effect of different parameters on patients' wishes to continue telemedicine visits.
A two‐tailed p value of <.05 was considered significant for all analyses. All analyses were performed with the IBM SPSS 25.0 software (SPSS Inc.; Chicago, IL).
Results
Between March and May 2020, 232 patients used the telemedicine platform; of those, 172 (74%) agreed to participate in the survey. The median age was 63, 99 (54%) participants were men, and the most common cancer diagnoses included gastrointestinal (n = 79, 46%), genitourinary (n = 30, 17.4%), breast (n = 25, 14.5%), and lung cancer (n = 15, 8.4%; Table 1). The purpose of visit was follow‐up during active oncologic treatment in 89 participants (51.7%) and routine surveillance after recovery in 58 (33.7%) patients. In accordance with institutional policy, the first meetings with an oncologist were predominantly conducted in person and not utilizing the telemedicine platform. This is reflected in the small number of newly diagnosed patients in the study cohort (n = 25, 14.5%).
Table 1.
Patient characteristics and demographics
| Characteristics and demographics | n (%) |
|---|---|
| Median age (range) | 63 (21–88) |
| Male sex | 93 (54) |
| Primary malignancy | |
| Gastrointestinal | 79 (46) |
| Genitourinary | 30 (17.4) |
| Breast | 25 (14.5) |
| Lung | 15 (8.7) |
| Gynecological | 3 (1.7) |
| Others | 20 (11.7) |
| Visit purpose | |
| New diagnosis/second opinion consultation | 25 (14.5) |
| Follow‐up during active disease | 89 (51.7) |
| Surveillance | 58 (33.7) |
| Time from diagnosis (months) | |
| <3 | 34 (19.8) |
| 3–6 | 12 (7) |
| 7–12 | 21 (12.2) |
| >12 | 105 (61) |
| Years of education | |
| Nonacademic | 76 (44.1) |
| Academic | 96 (55.8) |
Most patients (n = 105, 61%) were diagnosed over 12 months prior to the telemedicine meeting. The majority (n = 144, 83.2%) had only one telemedicine visit preceding the survey (Table 2). Conversation time lasted less than 10 minutes in 66 of the encounters (37.7%), 10–20 minutes in 89 of encounters (52.5%), and more than 20 minutes in a minority of cases (n = 17, 9.7%). The established follow‐up in‐person visits at our center are scheduled for 20 minutes, while newly diagnosed patient visits are scheduled for one hour.
Table 2.
Application user interface
| Application user interface | n (%) |
|---|---|
| No. of telemedicine visits | |
| 1 | 144 (83.2) |
| 2–3 | 24 (13.8) |
| >4 | 4 (2.3) |
| Conversation time (minutes) | |
| <10 | 66 (37.7) |
| 10–20 | 89 (52.5) |
| >20 | 17 (9.7) |
| People present during the conversation | |
| Spouse | 57 (33.1) |
| Children | 24 (14) |
| Friend | 1 (0.6) |
| Alone | 90 (52.3) |
| Telemedicine encounter location at patient's home | 162 (94.1) |
| Telemedicine encounter atscheduled time (yes) | 116 (67.4) |
| Telemedicine with treating oncologist and not another physician (yes) | 165 (95.9) |
Family members and friends were commonly present during the telemedicine meetings (n = 82, 47%), and approximately half of the patients met the oncologist unaccompanied (n = 90, 52.3%). Patients preferred to participate in the telemedicine encounter from their home in 91% of the cases (n = 162, 94%). The conversations were conducted at a predetermined time for 65% of the participants (n = 116), and 35% of the participants (n = 56) recounted that their encounter did not take place at the scheduled time. In almost all cases, the telemedicine meeting was conducted by the treating oncologist and not another physician (n = 165, 92%).
Patients' perceptions regarding sense of assurance and satisfaction following telemedicine encounters are described in Figure 1. Most patients felt that all relevant medical records were accessible to the physician (n = 168, 97%). The majority of patients were able to describe and appropriately reflect their physical and mental condition (n = 168, 97%) and felt that the physicians' explanations and treatment plans were clearly elucidated (n = 162, 91%). Patients affirmed a strong sense of secured privacy (n = 171, 99%). Moreover, the majority of patients perceived direct eye contact with the treating physician (n = 156, 90%) and affirmed that the physician was patiently attentive throughout the meeting (n = 166, 96%). A majority of the patients felt all their needs were provided for (n = 146, 82%) and their concerns were acknowledged (n = 166, 93%). A minority of the patients (n = 36, 20%) asserted that the absence of an in‐person visit harmed their treatment.
Figure 1.

Patients’ perspectives regarding telemedicine and patient‐physician relationship.
Most patients (n = 151, 84.8%) reported interest in continuing telemedicine meetings in the future. Of those, 15 participants (8.7%) employed telemedicine upon a first meeting with an oncologist with a new diagnosis, 64 patients (37.2%) used the telemedicine platform for a follow‐up visit during active treatment, and 47 patients (27.3%) used it during routine follow‐up after completion of oncology treatment. There was no correlation between visit purpose and willingness to continue telemedicine in the future, as demonstrated with a chi test (p = .12). Moreover, among the patient population interested in continuing telemedicine meetings, 36% (n = 36) conducted the video encounter with the presence of a family member or friend, whereas 41% (n = 41) conducted the visit without company. We did not note an effect of family and friend participation in telemedicine visit upon satisfaction and likelihood to continue telemedicine visits (p = .51). Reasons included shorter absolute travel time to the hospital (n = 73, 42%), sense of a safer home environment (n = 64, 37%), reduced risk of infection from COVID‐19 (n = 64, 37%), other infections (n = 46, 26%), affirming that their medical treatment was not compromised (n = 46, 26%), and reduced expenses (n = 29, 16.8%; Fig. 2A).
Figure 2.
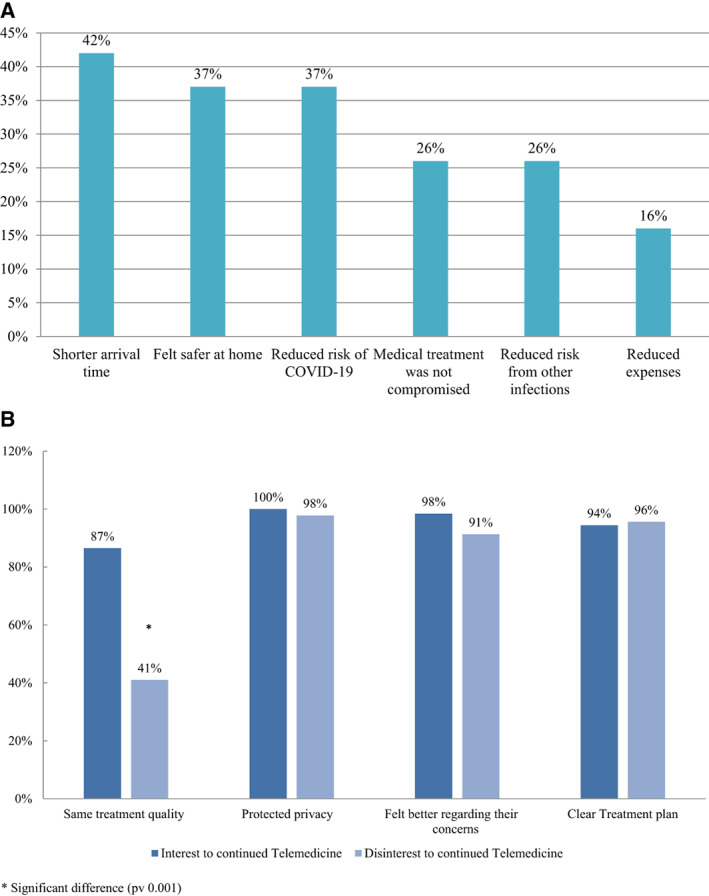
Reasons to continue telemedicine visits in the future (A) and comparison between patients willing or not to continue telemedicine meetings (B).
We evaluated patients' perceptions regarding telemedicine and compared the patients willing to continue telemedicine (n = 126) with those who were not inclined to continue using this format (n = 46). Patients' perspectives differed among their satisfaction of treatment quality. Among the patients not interested to continue telemedicine, 19 (41%) felt that the medical services were significantly harmed during the telemedicine meetings, whereas 109 (86%) patients who were interested in continuing telemedicine felt their meetings addressed all their needs (p = .001; Fig. 2B).
Multivariate logistic regression for factors associated with willingness to continue telemedicine visits (Table 3) found no significant association between age (p = .31), gender (p = .67), profession (p = .71), education level (p = .69), and the presence of direct eye contact during telemedicine encounters (p = .98). However, patients who felt satisfied regarding their concerns following their telemedicine visits expressed interest in continuing telemedicine (odds ratio [OR] = 2.41; p = .01). Additionally, patients who adopted telemedicine during routine surveillance, after completing their oncology treatment plan, were more likely to continue telemedicine versus patients who encountered an oncologist upon their first meeting in the telemedicine platform (OR = 3.34; p = .03). As presented in Fig. 3, telemedicine was integrated at our institution and within one month over 600 patients utilized this virtual platform.
Table 3.
Multivariant logistic regression for factors associated with willingness to continue telemedicine visits (n = 172)
| Variable | Adjusted OR (95% CI) | p value |
|---|---|---|
| Age | 2.56 (0.40–16.29) | .31 |
| Gender | 1.22 (0.47–3.16) | .67 |
| Profession | 0.71 (0.28–1.75) | .45 |
| Education level | 0.69 (0.30–1.54) | .36 |
| Purpose of visit | ||
| Follow‐up during active disease | 1.60 (0.52–4.89) | .40 |
| Surveillance | 3.34 (0.93–11.89) | .03 a |
| Doctor clarified disease status | 12.76 (0.62–262.34) | .09 |
| Doctor made eye contact | 0.98 (0.22–4.24) | .97 |
| Doctor listened to patient | 0.68 (0.05–8.05) | .76 |
| Patient felt better after conversation with doctor | 2.41 (1.64–76.55) | .01 a |
| Tumor primary | 0.16 (0.20–3.58) | .82 |
| Arrival time to hospital | 0.18 (0.16–4.31) | .82 |
P value less than 0.05 was considered significant.
Abbreviations: CI, confidence interval; OR, odds ratio.
Figure 3.
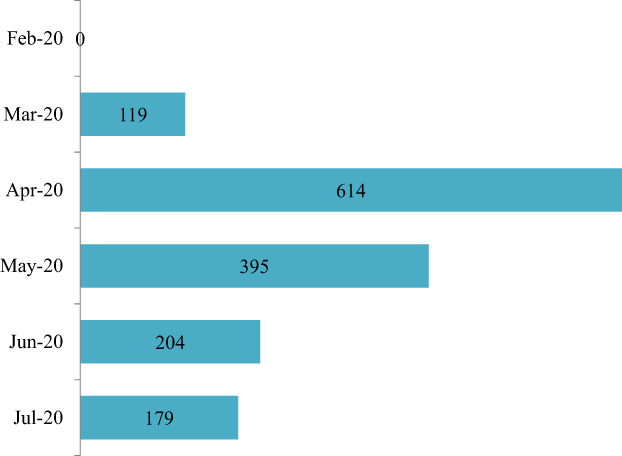
Number of telemedicine visits at Tel Aviv Medical Center during COVID‐19 pandemic.
Discussion
Our study demonstrates that telemedicine is perceived as safe and effective, and often does not compromise medical care or the patient‐physician relationship. Telemedicine platforms have been a mode of virtual communication, especially among patients isolated in rural areas, with satisfying results [38]. Nevertheless, it was not established as a common practice at centers worldwide until the COVID‐19 pandemic, which expedited its widespread adoption. The European Society of Medical Oncology issued guidelines [39] concerning patient care during the pandemic, suggests reduced clinic visitations by bolstering telemedicine services. In line with other oncology centers, we adopted telemedicine in our daily practice almost overnight (Fig. 3). When the national quarantine was lifted, the number of telemedicine visits decreased in the following months.
Major concerns involving the integration of telemedicine include potentially compromising patient–health care professional relationships [40, 41] and exclusion of populations without access or with technology limitations, as was addressed in our work. Telemedicine was perceived as safe and effective with a minor compromise of medical care and patient‐physician relationship.
Our study results indicate high satisfaction, as was expressed by the overwhelming number of patients enthusiastic to continue with telemedicine meetings in the future (84.6%). We did not find that family and friend participation during the telemedicine visit influenced satisfaction or likelihood to continue telemedicine (p = .51). However, Israel is a small country with short commutes, we believe the cut travel time with telemedicine will be a greater advantage in larger countries. It is notable that most patients (83.2%) had only one telemedicine visit prior to the survey. Of the patients willing to continue telemedicine, a fifth felt that their medical treatment was slightly compromised by this remote communication platform, consistent with the previous literature [27, 42].
Our study included all oncology patients at our tertiary cancer center who adopted telemedicine and agreed to participate; the age of the patients ranged from 21 to 88. We observed high satisfaction across all age groups. We anticipated that the absence of in‐person visits would potentially compromise treatment because of limited patient‐physician personal touch and possibly hinder patients' ability to express feelings and concerns. However, patients asserted that this platform was safe and effective.
Tele‐oncology refers to telemedicine among oncology patients and is a novel method of remote communication that is especially relevant in times of COVID‐19, but we foresee it will be a common, integral channel of communication in our daily practice long after COVID‐19. We expect tele‐oncology to be more appropriate for patients under surveillance after completion of active oncology treatment and can be considered for follow‐up visits alternately with in‐person meetings.
Our study strengths include an assessment of a heterogenic patient population: a wide range of age groups and primary tumors and the entire team of oncologists from a tertiary oncology center. Additionally, the survey was conducted by telephone a few days following the telemedicine encounter by an independent surveyor and not by the patient's physician. These factors contribute to the accuracy and authenticity of the patients' responses.
Study limitations involve recall bias and a single institution experience. Moreover, the exclusion of patients who encountered technological obstacles, as noted in other studies, is a major concern highlighting the inequality and curbed access to health care among a subset of the population and is another study constraint. Patients who had technological limitations, which included lack of access and competency employing the technology, most likely would not be satisfied with the telemedicine platform. Additionally, we report limited telemedicine experience per patient, as telemedicine was applied when in‐person visits were largely curtailed. Satisfaction may change over time with broader experience. Our study results from a tertiary care oncology center may not be generalizable to local oncology practices. The results of one country with distinct technological and cultural environments may not be translatable to or pertain to cancer care centers elsewhere. The first peak COVID‐19 effects on acceptability of telemedicine may not apply later in the pandemic or to post‐pandemic care.
Conclusion
Telemedicine is likely to be an integral means of communication among oncologists' daily practice. It is perceived as safe, effective, and without major compromise of patient‐physician relationship. Future communication skills workshops adopting this platform are warranted.
Author Contributions
Conception/design: Shira Peleg Hasson, Barliz Waissengrin, Ravit Geva, Ido Wolf
Provision of study material or patients: Shira Peleg Hasson, Barliz Waissengrin, Sharon Pelles, Ido Wolf
Collection and/or assembly of data: Shira Peleg Hasson, Barliz Waissengrin, Eliya Shachar, Marah Hodruj,
Mirika Brezis, Sharon Pelles, Ido Wolf
Data analysis and interpretation: Shira Peleg Hasson, Barliz Waissengrin, Alla Nikolaevski‐Berlin, Tamar Safra, Ido Wolf
Manuscript writing: Shira Peleg Hasson, Barliz Waissengrin, Eliya Shachar, Rochelle Fayngor, Ido Wolf
Final approval of manuscript: Shira Peleg Hasson, Barliz Waissengrin, Eliya Shachar, Marah Hodruj, Rochelle Fayngor, Mirika Brezis, Alla Nikolaevski‐Berlin, Sharon Pelles, Tamar Safra, Ravit Geva, Ido Wolf
Disclosures
The authors indicated no financial relationships.
Disclosures of potential conflicts of interest may be found at the end of this article.
No part of this article may be reproduced, stored, or transmitted in any form or for any means without the prior permission in writing from the copyright holder. For information on purchasing reprints contact commercialreprints@wiley.com. For permission information contact permissions@wiley.com.
References
- 1. Powell RE, Henstenburg JM, Cooper G et al. Patient perceptions of telehealth primary care video visits. Ann Fam Med 2017;15:225–229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Olayiwola JN, Magaña C, Harmon A et al. Telehealth as a bright spot of the COVID‐19 pandemic: Recommendations from the virtual frontlines (“Frontweb”). JMIR Public Health Surveill 2020;6:e19045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Bashshur RL, Howell JD, Krupinski EA et al. The empirical foundations of telemedicine interventions in primary care. Telemed J E Health 2016;22:342–375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Raffenaud A, Gurupur V, Fernandes SL et al. Utilizing telemedicine in oncology settings: Patient favourability rates and perceptions of use analysis using chi‐square and neural networks. Technol Health Care 2019;27:115–127. [DOI] [PubMed] [Google Scholar]
- 5. Humer MF, Campling BG. The role of telemedicine in providing thoracic oncology care to remote areas of British Columbia. Curr Oncol Rep 2017;19:52. [DOI] [PubMed] [Google Scholar]
- 6. Gurupur V, Shettian K, Xu P et al. Identifying the readiness of patients in implementing telemedicine in northern Louisiana for an oncology practice. Health Informatics J 2017;23:181–196. [DOI] [PubMed] [Google Scholar]
- 7. Lewis GD, Hatch SS, Wiederhold LR et al. Long‐term institutional experience with telemedicine services for radiation oncology: A potential model for long‐term utilization. Adv Radiat Oncol 2020;5:780–782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Aponte‐Tinao LA, Farfalli GL, Albergo JI et al. Face to face appointment vs. telemedicine in first time appointment orthopedic oncology patients: A cost analysis. Stud Health Technol Inform 2019;264:512–515. [DOI] [PubMed] [Google Scholar]
- 9. Telehealth . Available at https://www.nibib.nih.gov/science‐education/science‐topics/telehealth. Accessed December 6, 2020.
- 10. Benziger CP, Huffman MD, Sweis RN et al. The telehealth ten: A guide for a patient‐assisted virtual physical examination. Am J Med 2021;134:48–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Doolittle GC, Spaulding AO. Providing access to oncology care for rural patients via telemedicine. J Oncol Pract 2006;2:228–230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Mooi JK, Whop LJ, Valery PC et al. Teleoncology for Indigenous patients: The responses of patients and health workers. Aust J Rural Health 2012;20:265–269. [DOI] [PubMed] [Google Scholar]
- 13. Doolittle GC, Spaulding AO, Williams AR. The decreasing cost of telemedicine and telehealth. Telemed J E Health 2011;17:671–675. [DOI] [PubMed] [Google Scholar]
- 14. Kofoed S, Breen S, Gough K et al. Benefits of remote real‐time side‐effect monitoring systems for patients receiving cancer treatment. Oncol Rev 2012;6:e7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Jhaveri D, Larkins S, Kelly J et al. Remote chemotherapy supervision model for rural cancer care: Perspectives of health professionals. Eur J Cancer Care (Engl) 2016;25:93–98. [DOI] [PubMed] [Google Scholar]
- 16. Breen S, Ritchie D, Schofield P et al. The Patient Remote Intervention and Symptom Management System (PRISMS) – a telehealth‐mediated intervention enabling real‐time monitoring of chemotherapy side‐effects in patients with haematological malignancies: Study protocol for a randomised controlled trial. Trials 2015;16:472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Worster B, Swartz K. Telemedicine and palliative care: An increasing role in supportive oncology. Curr Oncol Rep 2017;19:37. [DOI] [PubMed] [Google Scholar]
- 18. Clark JM, Heifetz LJ, Palmer D et al. Telehealth allows for clinical trial participation and multimodality therapy in a rural patient with stage 4 non‐small cell lung cancer. Cancer Treat Res Commun 2016;9:139–142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Galsky MD, Shahin M, Jia R et al. Telemedicine‐enabled clinical trial of metformin in patients with prostate cancer. JCO Clin Cancer Inform 2017;1:1–10. [DOI] [PubMed] [Google Scholar]
- 20. Harky A, Chiu CM, Yau THL et al. Cancer patient care during COVID‐19. Cancer Cell 2020;37:749–750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Tasneem S, Kim A, Bagheri A et al. Telemedicine video visits for patients receiving palliative care: A qualitative study. Am J Hosp Palliat Care 2019;36:789–794. [DOI] [PubMed] [Google Scholar]
- 22. Raskin J, Lebeer M, De Bondt C et al. Cancer in the time of COVID‐19: Expert opinion on how to adapt current practice. Eur Respir J 2020;55:2000959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Cox A, Lucas G, Marcu A et al. Cancer survivors' experience with telehealth: A systematic review and thematic synthesis. J Med Internet Res 2017;19:e11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Larson JL, Rosen AB, Wilson FA. The effect of telehealth interventions on quality of life of cancer patients: A systematic review and meta‐analysis. Telemed J E Health 2018;24:397–405. [DOI] [PubMed] [Google Scholar]
- 25. Hennemann‐Krause L, Lopes AJ, Araújo JA et al. The assessment of telemedicine to support outpatient palliative care in advanced cancer. Palliat Support Care 2015;13:1025–1030. [DOI] [PubMed] [Google Scholar]
- 26. Smrke A, Younger E, Wilson R et al. Telemedicine during the COVID‐19 pandemic: Impact on care for rare cancers. JCO Global Oncology 2020;6:1046–1051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Miller EA. Telemedicine and doctor‐patient communication: An analytical survey of the literature. J Telemed Telecare 2001;7:1–17. [DOI] [PubMed] [Google Scholar]
- 28. Institute of Medicine (US) Committee on Evaluating Clinical Applications of Telemedicine , Field MJ, ed. Telemedicine: A Guide to Assessing Telecommunications in Health Care. Washington, DC: National Academies Press (US), 1996. [PubMed] [Google Scholar]
- 29. Wootton R, Darkins A. Telemedicine and the doctor‐patient relationship. J R Coll Physicians Lond 1997;31:598–599. [PMC free article] [PubMed] [Google Scholar]
- 30. Parrott R, Burgoon JK, Burgoon M et al. Privacy between physicians and patients: More than a matter of confidentiality. Soc Sci Med 1989;29:1381–1385. [DOI] [PubMed] [Google Scholar]
- 31. Mechanic D. Public trust and initiatives for new health care partnerships. Milbank Q 1998;76:281–302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Shirke MM, Shaikh SA, Harky A. Tele‐oncology in the COVID‐19 era: The way forward? Trends Cancer 2020;6:547–549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Nouri S, Khoong E, Lyles CR et al. Addressing equity in telemedicine for chronic disease management during the Covid‐19 pandemic. NEJM Catalyst Available at https://catalyst.nejm.org/doi/full/10.1056/CAT.20.0123. Accessed November 20, 2020.
- 34. Elkaddoum R, Haddad FG, Eid R et al. Telemedicine for cancer patients during COVID‐19 pandemic: Between threats and opportunities. Future Oncol 2020;16:1225–1227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Wolf I, Waissengrin B, Pelles S. Breaking bad news via telemedicine: A new challenge at times of an epidemic. The Oncologist 2020;25:e879–e880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Loblaw DA, Bezjak A, Bunston T. Development and testing of a visit‐specific patient satisfaction questionnaire: The Princess Margaret Hospital Satisfaction with Doctor Questionnaire. J Clin Oncol 1999;17:1931–1938. [DOI] [PubMed] [Google Scholar]
- 37. Davidson R, Mills ME. Cancer patients' satisfaction with communication, information and quality of care in a UK region. Eur J Cancer Care (Engl) 2005;14:83–90. [DOI] [PubMed] [Google Scholar]
- 38. Sabesan S, Simcox K, Marr I. Medical oncology clinics through videoconferencing: An acceptable telehealth model for rural patients and health workers. Intern Med J 2012;42:780–785. [DOI] [PubMed] [Google Scholar]
- 39. European Society for Medical Oncology . Cancer patient management during the COVID‐19 pandemic. Available at https://www.esmo.org/guidelines/cancer‐patient‐management‐during‐the‐covid‐19‐pandemic. Accessed August 6, 2020.
- 40. Sarhan F. Telemedicine in healthcare. 1: Exploring its uses, benefits and disadvantages. Nurs Times 2009;105:10–13. [PubMed] [Google Scholar]
- 41. Olsen DR, Bruland S, Davis BJ. Telemedicine in radiotherapy treatment planning: Requirements and applications. Radiother Oncol 2000;54:255–259. [DOI] [PubMed] [Google Scholar]
- 42. Agha Z, Schapira RM, Laud PW et al. Patient satisfaction with physician‐patient communication during telemedicine. Telemed J E Health 2009;15:830–839. [DOI] [PubMed] [Google Scholar]


