Summary
National (and global) vaccination provides an opportunity to control the COVID‐19 pandemic, which disease suppression by societal lockdown and individual behavioural changes will not. We modelled how vaccination through the UK’s vaccine priority groups impacts deaths, hospital and ICU admissions from COVID‐19. We used the UK COVID‐19 vaccines delivery plan and publicly available data to estimate UK population by age group and vaccination priority group, including frontline health and social care workers and individuals deemed ‘extreme clinical vulnerable’ or ‘high risk’. Using published data on numbers and distributions of COVID‐19‐related hospital and ICU admissions and deaths, we modelled the impact of vaccination by age group. We then modified the model to account for hospital and ICU admission, and death among health and social care workers and the population with extreme clinical vulnerability and high risk. Our model closely matches the government’s estimates for mortality after vaccination of priority groups 1–4 and groups 1–9. The model shows vaccination will have a much slower impact on hospital and ICU admissions than on deaths. The early prioritisation of healthcare staff and clinically vulnerable patients increases the impact of vaccination on admissions and also protects the healthcare service. An inflection point, when 50% of the adult population has been vaccinated – with deaths reduced by 95% and hospital admissions by 80% – may be a useful point for re‐evaluating vaccine prioritisation. Our model suggests substantial reductions in hospital and ICU admissions will not occur until late March and into April 2021.
Keywords: COVID‐19, pandemic, vaccine, modelling
Introduction
The SARS‐CoV‐2 virus that causes COVID‐19 continues to drive a pandemic with recent viral mutation increasing both spread and pressure on hospitals and intensive care units (ICU). Efforts to control spread of the virus with personal actions (reduced interpersonal contact, physical distancing, hand washing and mask wearing) or national initiatives (travel restrictions, closure of schools and lockdowns) have suppressed transmission to some extent but do not alter the fundamentals of the pandemic.
Vaccination on a national and global scale provides an opportunity to control the pandemic. Most focus has been on the impact of the vaccination program on reducing deaths, and the priority groups adopted have previously been shown to achieve this aim [1], but its impact on an overstretched healthcare system is also important. At the time of writing, the UK National Health Service (NHS) has had to reduce much elective surgical activity [2] and ICUs are in surge, meaning that they are coping only through expanding beyond their normal location, redeploying staff and decreasing staff‐to‐patient ratios [3].
In this paper, we have modelled how the vaccination program in the UK is likely to impact on COVID‐19‐related deaths, hospital admissions and ICU admissions among adults.
Methods
We modelled using data from the Department of Health and Social Care’s COVID‐19 vaccines delivery plan for the size of population in each vaccination priority group (Table 1) [4]. We based the analysis on data sources from June to July 2020 as this was complete and indicative of the overall impact of the first surge of the pandemic in the UK, enabling valid comparisons across groups. We used population distribution of UK countries from Office for National Statistics (ONS) data [5]. Deaths by age group were from ONS data for June 2020 [6]. The International Severe Acute Respiratory and Emerging Infection Consortium (ISARIC) study reporting on 20,000 COVID‐19 admissions to UK hospitals between 6 February and 19 April 2020 was used for age distribution of patients admitted to hospital [7]. Age distribution of ICU admissions was taken from the Intensive Care National Audit and Research Centre (ICNARC) report of 5 June 2020 [8]. We used publicly available national databases as sources of total numbers of COVID‐19‐related deaths in England and Wales up until 6 July [6], UK hospital admissions to 6 June UK [9] and ICU admissions in England, Northern Ireland and Wales to 5 June 2020 [8] and these were scaled up to UK populations as necessary. The number of deaths involving COVID‐19 among health and social care workers in England and Wales was taken from the ONS publication which reported those registered between 9 March and 20 July 2020 [10]. Age distribution of this group was taken from the database held by Dr Lennane and Professor Cook which underpins several publications on the topic [11, 12]. Number of healthcare workers admitted to hospital and ICU was taken from Shah et al.’s analysis of hospital and ICU admission of healthcare staff in Scotland [13]. Age distribution of NHS staff was taken from NHS Employers’ data [14]. Age distribution of people with long‐term conditions was taken from ONS data [15]. The impact of comorbidities on risk of mortality was estimated from the studies by Williamson et al. and Clift et al. that studied which patient characteristics are associated with COVID‐19‐related death, or hospital admission and death, respectively [16, 17].
Table 1.
Vaccine priority groups as described by Department of Health and Social Care’s COVID‐19 vaccines delivery plan [4]. Population denominators are the adult population (≥ 18 years).
| Priority group | Characteristics of included individuals (ages in years) | Total number (millions) | Proportion of UK adult population | Cumulative proportion of UK adult population | Cumulative proportion of included groups |
|---|---|---|---|---|---|
| 1 | Care home residents | 0.3 | 0.6% | 0.6% | 15.0% |
| Care home workers | 0.5 | 0.9% | 1.5% | ||
| 2 | Age 80+ | 3.3 | 6.3% | 7.8% | |
| Healthcare workers | 2.4 | 4.5% | 12.3% | ||
| Social care workers | 1.4 | 2.7% | 15.0% | ||
| 3 | Age 75–79 | 2.3 | 4.4% | 19.3% | 27.7% |
| 4 | Age 70–74 | 3.2 | 6.1% | 25.4% | |
| Clinically extremely vulnerable age < 70 | 1.2 | 2.3% | 27.7% | ||
| 5 | Age 65–69 | 2.9 | 5.5% | 33.1% |
50.4% |
| 6 | At risk age < 65 | 7.3 | 13.8% | 47.0% | |
| 7 | Age 60–64 | 1.8 | 3.4% | 50.4% | |
| 8 | Age 55–59 | 2.4 | 4.5% | 54.9% |
60.2% |
| 9 | Age 50–54 | 2.8 | 5.3% | 60.2% | |
| 10 | Age 18–50 | 21 | 39.8% | 100.0% | 100.0% |
| Total | 52.8 | 100.0% |
We made the following assumptions in our model. The vaccination program will be on target to provide a first vaccination dose to all groups 1–4 by 15 February 2021 and will continue at the same rate. Vaccination will broadly be undertaken by group as listed in the vaccine delivery plan [4]. Vaccination will be complete in all groups with 100% take‐up. The virus affects the population baseline characteristics in the same manner as in the first wave. Vaccination is 100% effective in preventing hospitalisation, ICU admission and death (including with infection by new variants of the virus), but does not itself reduce transmission rates. Age distributions for deaths, hospital and ICU admissions are the same for each of the countries in the UK. Among health and social care workers, deaths and admission would occur disproportionately in those who were clinically extremely vulnerable or at risk (see below). Social care workers’ patterns of hospital and ICU admission match those of frontline healthcare workers. Healthcare workers in Shah et al.’s paper of undetermined status were included in the patient‐facing group as they had increased risk of admission compared with the general population and this is only consistent with staff in patient‐facing roles [11]. Although increasing age is associated with increasing numbers of long‐term conditions [18], we assumed allocation to group 4 and 6 is on the basis of any single qualifying comorbidity or condition [19], rather than multiple conditions. The age distribution of patients who are extremely clinically vulnerable and at risk is the same as that of patients with long‐term conditions. The proportion of those aged 65–70 with long‐term conditions lies at the midpoint of the proportion aged > 65 and those aged 60–65. Data were analysed using Microsoft Excel (Redmond, WA, USA).
Modelling is described in detail in online Supporting Information Appendix S1 and is described here more briefly. As much of the data available in source material were in 10‐year age bands, we combined vaccination priority groups where necessary. Denominators for UK deaths, hospital admissions and ICU admissions were taken, or extrapolated where necessary, from the above data sources.
We used the above data sources to determine deaths and hospital and ICU admissions due to COVID‐19 adjusted to UK figures [4, 5, 6, 7, 8]. The first model (Fig. 1) was based only on age bands and ignored adjustments for health and social care workers (group 2), the extremely clinically vulnerable aged < 70 years (group 4) and those at risk aged < 65 years (group 5).
Figure 1.
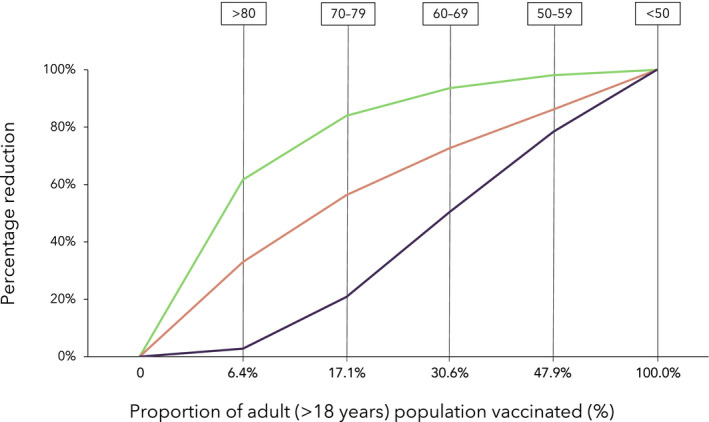
Cumulative impact of adult vaccination by age band on COVID‐19‐related hospital and ICU admissions and deaths. Green line, deaths; red line, hospital admissions; purple line, ICU admissions.
We then adjusted for group 2 (frontline health and social care workers). The overall size of this group was taken from the UK COVID‐19 vaccines delivery plan [4]. Excess deaths, hospital and ICU admissions were calculated using the data above [9, 10, 11, 12, 13]. Calculated additional deaths in this group [10] were added to group 2. We estimated that approximately one third of deaths among health and social care workers would occur in those who were extremely clinically vulnerable and therefore removed this proportion of additional deaths from group 4. The remaining additional deaths were then removed from groups 3–10 in the same age distribution as the Lennane and Cook database. Data in Shah et al.’s publication on healthcare worker hospital and ICU admissions in Scotland were scaled up to represent UK data. These additional hospital and ICU admissions were added to group 2. We then removed these additional admissions as follows: we estimated that 20% and 40% would be clinically extremely vulnerable (group 4) or at risk (group 6), respectively, and the remainder were distributed among groups 5–10. We used group size and age distribution of NHS staff to determine distribution of these cases; 10% group 5 and 7, 24% group 8 and 9, 66% group 10. As risk of harm from COVID‐19 increases dramatically with age [20], we allocated to these groups in the adjusted distribution 20% group 5 and 7, 30% group 8 and 9, 50% group 10.
We then adjusted for group 4 extremely clinically vulnerable and group 6 at‐risk populations. The size of these groups was taken from the UK COVID‐19 vaccines delivery plan [4]. We estimated that the extremely clinically vulnerable aged < 70 years (part of group 4) had a four‐fold increased risk of hospital admission, ICU admission or death relative to others of their same age and that for those in at risk aged < 65 years population (group 6) the risk increased two‐fold. We calculated national mortality, hospital and ICU admission rates by age group and used these to calculate absolute numbers of cases in each group by age. Additional deaths, hospital and ICU admissions were then calculated using the above scalars. For the group 4 adjustment the additional numbers were then added to group 4 and the same number removed from groups 5 and 7–10 in the same proportions as the distribution of long‐term conditions in those aged < 70 years. For the group 6 adjustment, the additional numbers were then added to group 4 and the same number removed from groups and 7–10 in the same proportions as the distribution of long‐term conditions in those aged < 65 years.
Finally, we analysed the timeline of impact of vaccination on hospitalisations, ICU admissions and deaths, which will differ for several reasons. First, there is a period between vaccination and immunity becoming effective which is likely to be a minimum of 2 weeks [21, 22]. Second, a lag between infection and subsequent hospitalisation, which we estimate to be 10 days [23, 24]. Finally, there is a lag between hospitalisation and ICU admission which on average is 2–3 days [8, 25]. Time from infection to death will vary according to whether the patient is hospitalised and, if so, whether they are admitted to ICU – although far from all patients are admitted to hospital. We used the estimated time from symptoms to death in the first surge reported by Harrison et al., who estimated 13 days from symptoms to death, equivalent to 17 days from infection to death [26]. Finally, there is a time lag between events and publication of data in the public domain. The anticipated delays between vaccination and impact on reported outcomes are shown in Table 2.
Table 2.
Anticipated delays between vaccination and impact on reported outcomes.
| Time to vaccine effectiveness (days) | Period from infection to event (days) | Reporting delay (days) | Total delay (days) | |
|---|---|---|---|---|
| Hospital admission | 14 | 10 | 2 | 26 |
| ICU admission | 14 | 13 | 2 | 29 |
| Deaths | 14 | 17 | 3 | 34 |
The UK government has targeted completion of vaccination of groups 1–4 by mid‐February 2021 [4]. Our assumption is that the vaccination rate required from mid‐January to complete groups 1–4 by 15 February will continue beyond that date (approximately 2.5 million vaccinations per week). Although groups 1 and 2 have been vaccinated together, we have assumed each group is vaccinated in sequence. In practice, we will see instances where this is not the case, and so the curves should be regarded as broad representations of the timescale of expected benefits.
Results
A total of 625 additional deaths were added to group 1. The same number was removed from groups 3–10 after removing 200 health and social care workers from group 4 to account for those with extreme clinical vulnerability. We estimated an additional 5380 hospital admissions and 662 ICU admissions of health and social care workers. For hospital admissions, 5380 were added to group 2 and removed from groups 3–10. We allocated 1000 as ‘extremely clinically vulnerable’ (group 4), 2000 as ‘at risk’ (group 6) and removed the remaining 2380 in the distribution described above.
Among the extremely clinically vulnerable aged < 70 years in group 4 we estimated 1515 deaths, 7422 hospital admissions and 1509 ICU admissions. These were added to group 4 and the excess numbers removed from groups 5 and 7–10 as described above.
Among the population at risk aged < 65 years (group 6) we estimated 2535 deaths, 14,760 hospital admissions and 2864 ICU admissions. These were added to group 6 and the same number removed from groups 7–10 as described above.
Adding these adjustments to those for health and social care workers provides a fully adjusted estimate of the impact of effective vaccination of all those in each priority group on deaths, hospital and ICU admissions (Fig. 2; Table 3).
Figure 2.
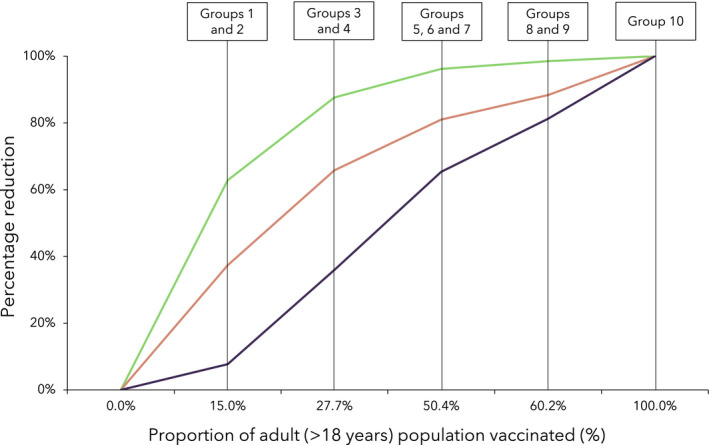
Cumulative impact of adult vaccination by vaccination priority group on COVID‐19‐related hospital and ICU admissions and deaths. Green line, deaths; red line, hospital admissions; purple line, ICU admissions.
Table 3.
Cumulative impact of vaccination on COVID‐19‐related hospital and ICU admissions and deaths modelled by age and adjusted by clinical priority groups.
| Groups vaccinated by age only | ||||
|
Group vaccinated (years) |
Proportion of adult population vaccinated | Reduction in deaths | Reduction in hospital admissions | Reduction in ICU admissions |
| None | 0% | 0% | 0% | 0% |
| >80 | 6% | 62% | 33% | 3% |
| 70–79 | 17% | 84% | 56% | 21% |
| 60–69 | 31% | 94% | 73% | 51% |
| 50–59 | 48% | 98% | 86% | 78% |
| 18–50 | 100% | 100% | 100% | 100% |
| Groups vaccinated adjusted for health and social care workers | ||||
| Group vaccinated | Proportion of adult population vaccinated | Reduction in deaths | Reduction in hospital admissions | Reduction in ICU admissions |
| None | 0% | 0% | 0% | 0% |
| 1 and 2 | 15% | 63% | 37% | 8% |
| 3 and 4 | 28% | 85% | 60% | 25% |
| 5 and 7 | 50% | 94% | 74% | 52% |
| 8 and 9 | 60% | 98% | 87% | 79% |
| 10 | 100% | 100% | 100% | 100% |
| Groups vaccinated adjusted for health and social care workers, extremely clinically vulnerable and at risk | ||||
| Group vaccinated | Proportion of adult population vaccinated | Reduction in deaths | Reduction in hospital admissions | Reduction in ICU admissions |
| None | 0% | 0% | 0% | 0% |
| 1 and 2 | 15% | 63% | 37% | 8% |
| 3 and 4 | 28% | 88% | 66% | 36% |
| 5–7 | 50% | 96% | 81% | 65% |
| 8 and 9 | 60% | 98% | 88% | 81% |
| 10 | 100% | 100% | 100% | 100% |
Figure 3 shows the estimated timeline for impact of vaccinations on the three metrics described. That target appears to be achievable given reported progress over recent weeks [27]. If the current rate of vaccination is maintained, vaccination of the first nine groups may be achieved before material numbers of second doses will become due (in early April, based on the current 12‐week dosing interval) which would begin to impact on the rate of further progress. Any increase or decrease in availability of vaccines will of course accelerate or decrease the timescales shown.
Figure 3.
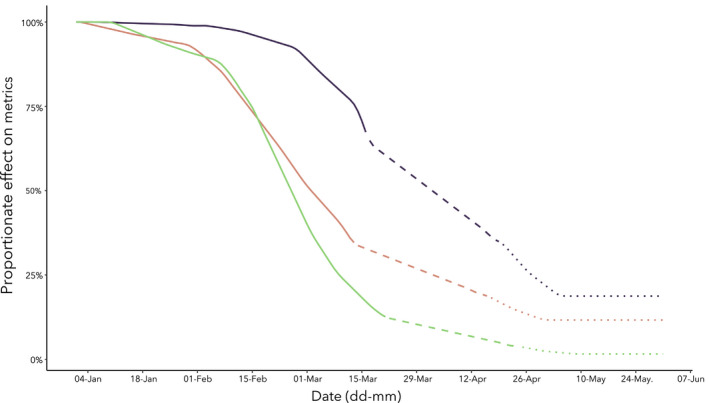
Estimated timescale for impact of adult vaccination by vaccination priority group on COVID‐19‐related hospital and ICU admissions and deaths. Green line, deaths; red line, hospital admissions; purple line, ICU admissions; solid line, priority groups 1–4; dashed line, priority groups 5–7; dotted line priority groups 8–9.
The two key assumptions that impact the model are the vaccination take‐up rate and vaccine effectiveness. We assume 100% for both, from which any adjustments can then be derived: our estimates can therefore be considered to model a ‘best‐case scenario’. We have undertaken sensitivity modelling to demonstrate how the model varies if take‐up rates are 90% (95% for those over 80), and also if vaccine effectiveness is 90% (Table 4).
Table 4.
Sensitivity analysis of the impact of different rates of vaccine take‐up and vaccine effectiveness. Base scenarios assume 100% take‐up and 100% effectiveness.
| Proportionate reduction after priority groups 1–4 | |||
| Scenario | Hospital admissions | ICU admissions | Deaths |
| Base | 66% | 36% | 88% |
|
Take‐up: 95% (> 80 years), 90% (Other) Effectiveness: 100% |
60% | 32% | 82% |
|
Take‐up: 100% Effectiveness: 90% |
59% | 32% | 79% |
| Proportionate reduction after priority groups 5–7 | |||
| Scenario | Hospital admissions | ICU admissions | Deaths |
| Base | 81% | 65% | 96% |
| Take‐up: 95% (> 80 years), 90% (Other)Effectiveness: 100% | 75% | 59% | 90% |
|
Take‐up: 100% Effectiveness: 90% |
73% | 59% | 86% |
| Proportionate reduction after priority groups 8 and 9 | |||
| Scenario | Hospital admissions | ICU admissions | Deaths |
| Base | 88% | 81% | 98% |
|
Take‐up: 95% (> 80 years), 90% (Other) Effectiveness: 100% |
81% | 73% | 92% |
|
Take‐up: 100% Effectiveness: 90% |
79% | 73% | 89% |
Discussion
Our modelling illustrates how vaccination will impact on deaths, predominantly in the elderly population, more rapidly than on hospital and ICU admissions. This has important implications for healthcare policy and in particular for decisions regarding management of national initiatives that seek to maintain control of community viral transmission, most particularly lockdown. The marked variation in impact is highlighted by the notably different median ages of patients: age 83 years for those who die [28], 73 years for hospital admissions [7] and 61 years for ICU admissions [25].
The findings have several clear implications. First, that the impact of COVID‐19 on hospitals and in particular on ICU admissions will last considerably longer than the time taken to dramatically reduce deaths. Second, there is a large benefit from maintaining high vaccination rates beyond groups 1–4: vaccinating through groups 5–7 has a substantial impact on all three metrics including reducing hospital admissions by > 80% and ICU admissions by almost 70%. Third, it provides some support for the strategy of delaying the second dose of vaccine, as within approximately 3 months around half of the adult population can be vaccinated, and as all three slopes are relatively steep up to this point, this will optimise the impact on deaths and healthcare service pressures. Fourth, the data generally support the government priority groups [1, 2]. This is shown by comparing Figs. 1 and 2 as the adjusted model, which includes early prioritisation of health and social care workers, the extremely clinically vulnerable and those at high risk, is somewhat more favourable than the unadjusted in reducing impact on healthcare pressures while maintaining early impact on deaths. Importantly, early vaccination of health and social care workers (in the front line) will support the very systems that we need to keep hospitals and care services running for the prolonged period that this will be needed [29].
The curves all begin to flatten after priority group 7 has been vaccinated and this raises questions. It may be that vaccination priorities may reasonably be reconsidered, for instance to target high‐risk key workers, such as those involved in transport and education [30] to enable community control of transmission and accelerate return to normality in some areas of public life. The major gains of rapidly vaccinating groups 1–7 will likely reduce viral circulation in the community and this may reduce spread among the unvaccinated (even if vaccination does not itself reduce infection and transmission). This in turn would reduce the evolutionary pressure on the virus, thereby reducing the risks of emergence of higher risk viral strains including those that may escape vaccine sensitivity. Vaccination is a global imperative [31] and on reaching the flatter part of the curves it may also be rational and moral to consider whether UK stocks of vaccine might also be redistributed to support the global attempts at vaccination in countries with lower access to vaccines [31].
The main limitations to our study are the assumptions we have made in order to create our model. Our assumptions about similarity of mortality rates between UK countries are supported, as calculating total UK deaths by combining numbers from individual countries [32, 33] rather than scaling up figures from England and Wales leads to a variation of less than 2%. Our assumptions on vaccination uptake rates are supported by the fact that vaccination acceptance is highest in older patients, high in all groups aged over 50 years and increasing. In a December 2020 report, 78% of respondents were ‘very’ or ‘fairly’ likely to accept vaccination, but among those aged > 70 years the rate was 95% and among those aged 50–69 years it was 84% [34]. In January 2021, the acceptance rate had increased to 89% of the whole population, to 98% in those aged > 70 years and to 94% among those aged 50–69 years [35]. Vaccine effectiveness for the purpose of this paper is its ability to prevent serious illness, rather than symptomatic or asymptomatic infection, which is how the results of the trials of the two vaccines in use to date have been presented. Vaccine efficacy in preventing serious illness is currently expected to be greater than its efficacy in preventing infection or any symptomatic illness [22, 23, 36]. For current vaccines, the ability to prevent serious illness seems to be high even 2 weeks after a single dose [22, 23], and this is likely to exceed 90%. Regarding comorbidity, the average number of comorbidities reported among patients dying from COVID‐19 in England and Wales is 2.2, varying little across ages, which supports the contention that priority risk groups are selected on severity of comorbidity rather than number [37]. Our estimates for a four‐ and two‐fold increase in risk of harm among the extremely clinically vulnerable and at‐risk patients, respectively, are based on the studies by Williamson et al. and Clift et al. in which comorbidities were associated with hazard ratios for hospitalisation or death broadly in this range [16, 17]. Using these scalars, the reduction in deaths we estimate after vaccination of groups 1–4 and 1–9 (87.7% and 98.5%) almost exactly matches those reported in the Department of Health and Social Care’s COVID‐19 vaccines delivery plan (88% and 99%). It is uncertain whether vaccination will be as effective with the new variants of the virus as those prevalent during vaccine studies, but most predictions and emerging evidence is currently reassuring.
In conclusion, we have modelled the impact of the UK’s vaccine strategy and use of priority groups on COVID‐19 deaths, hospital and ICU admissions. Our model matches the government’s estimates for mortality reductions very well. The model shows that the impact of vaccination on deaths due to COVID‐19 will be much more rapid than the impact on hospital and ICU admissions. The early prioritisation of healthcare staff and clinically vulnerable patients is likely to increase the impact of vaccination on hospital and ICU admissions and to also protect the healthcare service. An inflection point, when 50% of the adult population has been vaccinated – and when deaths have been reduced by 95% and hospital admissions by 80% – may be a useful point for re‐evaluating vaccine prioritisation. Our model suggests substantial reductions in hospital and ICU admissions will not occur until late March and into April 2021.
Supporting information
Appendix S1. Modelling used. [Correction added on 18 February 2021, after first online publication: The supplementary Appendix S1 has been replaced in this version]
Acknowledgements
No external funding or competing interests declared.
Contributor Information
T. M. Cook, Email: timcook007@gmail.com, @, doctimcook.
J. V. Roberts, @john_actuary.
References
- 1. Gong Y, McDonald S. How logical is the UK’s vaccine priority ordering? COVID‐19 Actuaries Response Group. 7 December 2020. https://www.covid‐arg.com/post/vaccine‐priorities (accessed 30/01/2021).
- 2. Kursumovic E, Kane A, Armstrong R, Soar J, Cook TM. Anaesthesia and critical care COVID Activity survey (ACCC‐track survey) round 1. Executive Summary. https://www.nationalauditprojects.org.uk/ACCC‐track‐Anaesthesia‐and‐Critical‐Care‐COVID‐Activity#pt (accessed 30/01/2021).
- 3. O'Connor M, Hand J. Covid: number of patients on ventilators passes 4,000 for first time. BBC News. 24 Jan 2021. https://www.bbc.co.uk/news/uk‐55782716 (accessed 30/01/2021).
- 4. Department of Health and Social Care . UK COVID‐19 vaccines delivery plan. 11 Jan 2021. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/951284/UK_COVID‐19_vaccines_delivery_plan.pdf (accessed 30/01/2021).
- 5. Park N. Population estimates for 2019. ONS. Released 24 June 2020. https://www.ons.gov.uk/peoplepopulationandcommunity/populationandmigration/populationestimates/datasets/populationestimatesforukenglandandwalesscotlandandnorthernireland (accessed 30/01/2021).
- 6. Campbell A, Caul S. Deaths involving COVID‐19, England and Wales. Office for National Statistics. 17 July 2020. https://www.ons.gov.uk/peoplepopulationandcommunity/birthsdeathsandmarriages/deaths/datasets/deathsinvolvingcovid19englandandwales (accessed 30/01/2021).
- 7. Docherty AB, Harrison EM, Green CA, et al. Features of 20 133 UK patients in hospital with covid‐19 using the ISARIC WHO clinical characterisation protocol: prospective observational cohort study. British Medical Journal 2020; 369: m1985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Intensive Care National audit and Research Centre . Report on COVID‐19 in critical care. 5 June 2020. https://www.icnarc.org/Our‐Audit/Audits/Cmp/Reports (accessed 30/01/2021).
- 9. Covid‐19 data dashboard. UK Government. https://coronavirus.data.gov.uk/details/healthcare (accessed 31/01/2021).
- 10. Office for National Statistics . Deaths involving the coronavirus (COVID‐19) among health and social care workers in England and Wales, deaths registered between 9 March and 20 July 2020. ONS. 7 August 2020. https://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/causesofdeath/adhocs/12112deathsinvolvingthecoronaviruscovid19amonghealthandsocialcareworkersinenglandandwalesdeathsregisteredbetween9marchand20july2020 (Accessed 30/01/2021).
- 11. Cook TM, Kursumovic E, Lennane S. Deaths of NHS staff from covid‐19 analysed. Health Service Journal 2020. https://www.hsj.co.uk/exclusive‐deaths‐of‐nhs‐staff‐from‐covid‐19‐analysed/7027471.article (accessed 30/01/2021). [Google Scholar]
- 12. Cook TM, Lennane S. Occupational COVID‐19 risk for anaesthesia and intensive care staff – low‐risk specialties in a high‐risk setting. Anaesthesia 2020. Epub 11 December. 10.1111/anae.15358. [DOI] [PubMed] [Google Scholar]
- 13. Shah ASV, Wood R, Gribben C, et al. Risk of hospital admission with coronavirus disease 2019 in healthcare workers and their households: nationwide linkage cohort study. British Medical Journal 2020; 371: m3582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. NHS Employers . Age in the NHS. https://www.nhsemployers.org/‐/media/Employers/Documents/Plan/DIVERSITY‐AND‐INCLUSION/EQW19/Age‐in‐the‐NHS‐infographic.pdf (accessed 30/01/2021).
- 15. Office for National Statistics . People with long‐term health conditions. UK: January to December 2019. 26 March 2020. https://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/conditionsanddiseases/adhocs/11478peoplewithlongtermhealthconditionsukjanuarytodecember2019 (accessed 30/01/2021).
- 16. Williamson EJ, Walker AJ, Bhaskaran K, et al. Factors associated with COVID‐19‐related death using OpenSAFELY. Nature 2020; 584: 430–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Clift AK, Coupland CAC, Keogh RH, et al. Living risk prediction algorithm (QCOVID) for risk of hospital admission and mortality from coronavirus 19 in adults: national derivation and validation cohort study. British Medical Journal 2020; 371: m3731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Southampton City Council . Southampton City Health and Care Strategy 2020‐2025. 2020. https://www.southampton.gov.uk/images/southampton‐city‐5‐year‐health‐care%20strategy_final_post‐covid_tcm63‐435823.pdf (accessed 30/01/2021).
- 19. National Health Service . Who's at higher risk from coronavirus. 2020. https://www.nhs.uk/conditions/coronavirus‐covid‐19/people‐at‐higher‐risk/whos‐at‐higher‐risk‐from‐coronavirus/ (accessed 30/01/2021).
- 20. Spiegelhalter D. Use of “normal” risk to improve understanding of dangers of covid‐19. British Medical Journal 2020; 370: m3259. [DOI] [PubMed] [Google Scholar]
- 21. Polack FP, Thomas SJ, Kitchin N, et al. Safety and efficacy of the BNT162b2 mRNA Covid‐19 vaccine. New England Journal of Medicine 2020; 383: 2603–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Voysey M, Clemens SAC, Madhi SA, et al. Safety and efficacy of the ChAdOx1 nCoV‐19 vaccine (AZD1222) against SARS‐CoV‐2: an interim analysis of four randomised controlled trials in Brazil, South Africa, and the UK. Lancet 2021; 397: 99–111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020; 395: 497–506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Hall M, Pritchard M, Dankwa EA, et al. ISARIC Clinical Data Report 20 November 2020. International Severe Acute Respiratory and emerging Infections Consortium. https://www.medrxiv.org/content/10.1101/2020.07.17.20155218v5.full.pdf (accessed 30/01/2021).
- 25. Intensive Care National audit and Research Centre . Report on COVID‐19 in critical care. 22 January 2021. https://www.icnarc.org/Our‐Audit/Audits/Cmp/Reports (accessed 30/01/2021).
- 26. Harrison EM, Docherty A, Semple C. COVID‐19: time from symptom onset until death in UK hospitalised patients. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/928729/S0803_CO‐CIN_‐_Time_from_symptom_onset_until_death.pdf (accessed 30/01/2021).
- 27. UK Government . Vaccinations in the UK. 2020. https://coronavirus.data.gov.uk/details/vaccinations (accessed 30/01/2021).
- 28. Office for National Statistics . Average age of death (median and mean) of persons whose death was due to COVID‐19 or involved COVID‐19, by sex, deaths registered up to week ending. 2 October 2020, England and Wales. https://www.ons.gov.uk/peoplepopulationandcommunity/birthsdeathsandmarriages/deaths/adhocs/12376averageageofdeathmedianandmeanofpersonswhosedeathwasduetocovid19orinvolvedcovid19bysexdeathsregistereduptoweekending2october2020englandandwales (accessed 30/01/2021).
- 29. Cook TM, Lennane S. Nurses, ambulance crews and support workers should get the COVID vaccine first. Health Service Journal 2020; 30. https://www.hsj.co.uk/coronavirus/nurses‐ambulance‐crews‐and‐support‐workers‐should‐get‐the‐covid‐vaccine‐first/7029239.article (accessed 30/01/2021). [Google Scholar]
- 30. Office for National Statistics . Coronavirus (COVID‐19) Infection Survey, UK. 6 November 2020. https://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/conditionsanddiseases/bulletins/coronaviruscovid19infectionsurveypilot/6november2020#analysis-of-the-number-of-school-workers-key-workers-and-other-professions-in-england-who-had-covid-19 (accessed 30/01/2021).
- 31. Cook TM, Farrar J. COVID‐19 vaccines: one step towards the beginning of the end of the global impact of the pandemic. Anaesthesia 2020. Epub 14 December. 10.1111/anae.15365. [DOI] [PubMed] [Google Scholar]
- 32. Scottish Government . Coronavirus (COVID‐19): daily data for Scotland. 2020. https://www.gov.scot/publications/coronavirus‐covid‐19‐daily‐data‐for‐scotland/ (accessed 30/01/2021).
- 33. Northern Ireland Statistics and Research Agency . Deaths registered dashboard. 2020. https://datavis.nisra.gov.uk/vitalstatistics/weekly‐deaths‐dashboard.html (accessed 30/01/2021).
- 34. Office for National Statistics . Coronavirus and the social impacts on Great Britain. 22 January 2021. https://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/healthandwellbeing/bulletins/coronavirusandthesocialimpactsongreatbritain/18december2020#attitudes‐to‐covid‐19‐vaccination (accessed 30/01/2021).
- 35. Office for National Statistics . Coronavirus and the social impacts on Great Britain: 22 January 2021. https://www.ons.gov.uk/releases/coronavirusandthesocialimpactsongreatbritain22january2021 (accessed 30/01/2021).
- 36. Knoll MD, Wonodi C. Oxford–AstraZeneca COVID‐19 vaccine efficacy. Lancet 2020; 397: 72–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Office for National Statistics . Deaths involving COVID‐19, England and Wales. 17 July 2020. https://www.ons.gov.uk/peoplepopulationandcommunity/birthsdeathsandmarriages/deaths/datasets/deathsinvolvingcovid19englandandwales (accessed 30/01/2021).
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix S1. Modelling used. [Correction added on 18 February 2021, after first online publication: The supplementary Appendix S1 has been replaced in this version]


