Abstract
Timely diagnosis and treatment of oral and oropharyngeal cancers are central for the patient's survival. Our objective was to document the impact of the COVID‐19 pandemic on the rate of hospitalizations due to these cancers in Brazil's National Health System (SUS). The number of hospitalizations by these cancers during the first periods of the pandemic—and between the same period of 2016 to 2019—was retrieved from the SUS Hospital Information System. We compared hospitalization rates between pre‐ and pandemic periods, by State. The hospitalization rate for oral and oropharyngeal cancer during the pandemic was lower than that of the same period of previous years. The decline between 2019 and 2020 was of 49.3%, reaching 60% in the North. The reduction in hospitalization during an extended period suggests that oral and oropharyngeal cancer care will be postponed, with potentially detrimental impact on survival.
Keywords: coronavirus infections, COVID‐19, oral cancer, oropharyngeal cancer, pandemics
The diagnosis and timely treatment—in the early stages—of oral and oropharyngeal cancer are central to patients' survival. 1 , 2 Nevertheless, the profound impacts of the COVID‐19 pandemic on health systems globally are disrupting care delivery. Even in countries with structured health systems, the need to restrict contagion and ensure medical care for patients with the new coronavirus disease deranged oncology services. 3 , 4 As an additional problem, the fear of exposure to contamination may have distanced patients with symptoms from health services. 5 , 6 A few months after the pandemic reached global proportions, concerns about its consequences for the cancer management became a frequent topic in the scientific literature. 3 , 7 , 8 , 9 , 10 , 11 First, patients with cancers of almost any type have a higher risk of complicated COVID 19 infection. 12 , 13 Another critical concern is that the COVID‐19 outbreak will result in many cancer cases with delayed diagnosis and treatment and an increase in mortality. Nevertheless, there is a lack of evidence quantifying the extent to which the outbreak influenced the provision of care in oncology.
Head and neck cancers are characterized by a rapid TNM staging progression. 1 , 14 This disease may rapidly invade or metastasize, and severe tumours may then require complex surgery and/or radiotherapy (occasionally, chemotherapy) that results in long‐term orofacial deformity, oropharyngeal dryness, trismus, a risk of osteoradionecrosis and reduced quality of life. Advanced cases are also associated with a lower likelihood of survival. 2 , 15 , 16 In Brazil, oral cancer is the fifth most incident type in men, comprising 5% of all cancer cases estimated for 2020. 17 Prior research reports have shown an important reduction in the number of soft oral tissue biopsies in Brazil due to the pandemic. 18 , 19 All surgery for head and neck cancers requires hospitalization, and often radiotherapy and/or chemotherapy may require bouts of stay in hospital. 20 Measuring and comparing this metric between pre‐ and pandemic periods can inform us if the care that cannot be postponed is being neglected. In this context, we aimed to document the impact of the COVID‐19 pandemic on the number of hospitalizations due to oral and oropharyngeal cancer in Brazil's National Health System (known as ‘SUS’).
The SUS Hospital Information System (SIH‐SUS) makes available—publicly and anonymously—the information of all hospitalizations that occur in the SUS. The number of hospitalizations by oral and oropharyngeal cancer (codes C00‐C10 from ICD‐10) during the first months of the COVID‐19 outbreak in Brazil—from April to June of 2020—was gathered from SIH‐SUS. The data from June were the most up to date when this study was carried out. Data on hospitalizations that occurred between April and June of 2016, 2017, 2018 and 2019 were also gathered from SIH‐SUS for comparison, by Brazilian State of patients' residences—Brazil is divided into 26 States and one Federal District. To obtain the hospitalization rates, we divide the monthly number of hospitalizations due to oral and oropharyngeal cancer in each State by its population and multiply the result by 100 000. Unfortunately, information regarding patient distributions according to cancer stages was unavailable.
At the close of this analysis—the second half of August—Brazil had more than 3.5 million confirmed cases and more than 110 thousand deaths due to COVID‐19. The Brazilian Ministry of Health confirmed the first death in the middle of March, and it was also during this period that States first affected by the pandemic started to implement measures of social distancing. 21 Cancer diagnosis and treatment services were not suspended in Brazil during the pandemic. Although some services may have adapted specific protocols for postponing less severe cases, this was not a national policy. The present study results revealed that the hospitalization rate for oral and oropharyngeal cancer—average from April to June 2020—was lower than that of the same period of previous years in all regions of Brazil (Figure 1). Considering the whole country, the decline between 2019 and 2020 was 49.3%, reaching 60% in the North region—Table 1. This is the most impoverished region of the country and had been showing an increasing trend in mortality from oral and oropharyngeal cancer, even before the pandemic. 22 The States of the South and Southeast have the most structured healthcare networks and concentrate a large part of the country's wealth. During the pandemic period, they continued to have more hospitalizations than States in other regions (Figure 2). However, these States also had important reductions in hospitalizations due to oral and oropharyngeal cancers that were of 44.7% and 50.8% in the South and Southeast, respectively. The reduction found in the comparison between the 2020 rates and the average rates from 2016 to 2019 was similar to that found in the comparison between 2020 and 2019 (Table 1).
FIGURE 1.
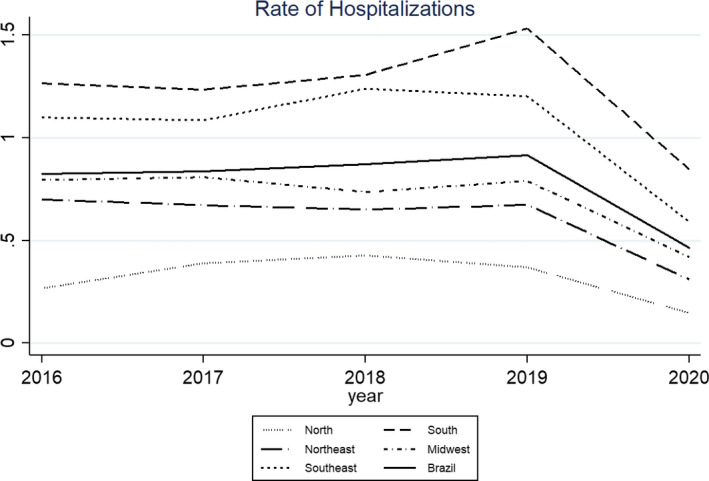
Average monthly oral and oropharyngeal cancer (C00‐C10) hospitalization rate (per 100 000 inhabitants) of April to June, by Brazilian regions. *The States Acre and Amapá were excluded due to lack of data
TABLE 1.
Number of hospitalizations for oral and oropharyngeal cancer (C00‐C10) and average monthly hospitalization rate (per 100 000 inhabitants) of April to June, by Brazilian regions
| Region (n. FU) | April–June 2016‐2019 | April–June 2019 | April–June 2020 | Change (%) d | Change (%) e | |||
|---|---|---|---|---|---|---|---|---|
| n. Hosp. b | Hosp. Rate c | n. Hosp. | Hosp. Rate | n. Hosp. | Hosp. Rate | |||
| North (n. 5 a ) | 130.5 | 0.36 | 131 | 0.37 | 47 | 0.15 | −58.3 | −60.0 |
| Northeast (n. 9) | 1194.25 | 0.67 | 1121 | 0.67 | 555 | 0.31 | −53.7 | −54.0 |
| Southeast (n. 4) | 2613.75 | 1.16 | 2600 | 1.20 | 1566 | 0.59 | −49.1 | −50.8 |
| South (n. 3) | 1164.5 | 1.33 | 1315 | 1.53 | 715 | 0.85 | −36.1 | −44.7 |
| Midwest (n. 4) | 376 | 0.78 | 383 | 0.79 | 244 | 0.42 | −46.2 | −46.7 |
| Brazil (n. 25) | 5479 | 0.86 | 5550 | 0.91 | 3127 | 0.46 | −46.5 | −49.3 |
Abbreviations: n., number of; FU, federation unity; Hosp., hospitalization.
The States Acre and Amapá were excluded due to lack of data.
Average number, considering 2016 to 2019.
Average rate, considering 2016 to 2019.
Change in hospitalization rates, comparing 2020 with the 2016 to 2019 average.
Change in hospitalization rates, comparing 2020 to 2019.
FIGURE 2.
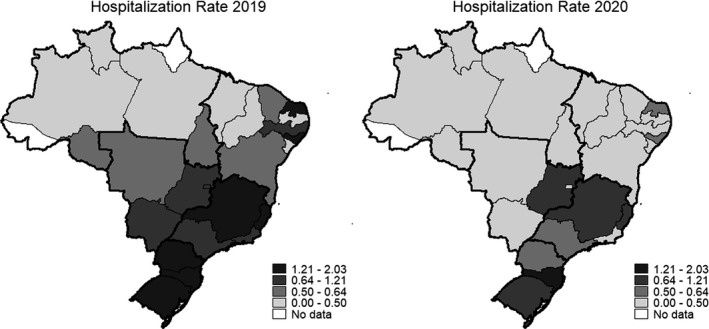
Average oral and oropharyngeal cancer (C00‐C10) hospitalization rate for April, May and June (per 100 000 inhabitants), by Brazilian states. The thin lines delimit the States of Brazil; the thick lines delimit the regions of Brazil. *The states Acre and Amapá were excluded due to lack of data
The Brazilian health authority estimated 15 000 new oral and oropharyngeal cancer cases in 2020. 17 This number will not decrease because of the pandemic. Due to the need to promptly treat malignant neoplasms, a law in Brazil stipulated that the treatment of cancer should begin in up to 60 days after the diagnosis. 23 The reduction in hospitalization during the extended period suggests that many oral and oropharyngeal cancer treatments were postponed by the hospital system for even longer than 60 days, which may lead to a poorer prognosis. It is also probable that patients who have already initiated their treatment may not have been able to attend for the management of complications given the need to shield or concerns about acquiring the infection during travel or clinical attendance. 9 All of which runs the risk of reducing the present 50% 5‐year survival rate of this group of cancers in Brazil. 24 This hypothesis is corroborated by a survey performed in the affluent city of Sao Paulo, where both inpatient and outpatient visits decreased by 47% and 61%, respectively, suggesting that even some patients under active oral cancer treatment experienced changes in visits and treatment protocols. 9 A general reduction in overall cancer care in several countries in the same period has been observed. Indeed, in the UK, urgent referrals and chemotherapy for any cancer, including oropharynx cancer, decreased by 70% and 40%, respectively, 25 while reductions by 9% in chemotherapy, 16% in radiotherapy, and 30% in surgery were observed in France. 26 Among patients with cancer under treatment in the Netherlands, treatment or follow‐up was postponed or cancelled in 11% of individuals and changed into phone/video counselling in 18%. 27 For specific head and neck cancer surgery, data from a tertiary care centre in Alabama found a 55% reduction in surgery. 28
Since cancer care services in Brazil should continue to operate during the pandemic period, a set of other reasons that fell on hospital care may explain the reduction in hospitalizations for head and neck cancer. Initially, there was a severe disruption in health systems. It was a global phenomenon that was not different in Brazil. There was a severe shortage of personal protective equipment (PPE) and ventilators because of the increase in demand and the disruption that the pandemic caused in the supply chain. Early in the pandemic, the production of PPE by Chinese factories and the exports came to a halt because of lockdowns imposed throughout this country. 29 Another crucial aspect is that hospital resources (hospital beds, ICU beds) were mobilized to fight COVID‐19. Before the pandemic, most hospitals were already operating at (or beyond) their capacity. It means that critically needed head and neck cancer care resources were allocated to treat COVID‐19 patients. 30 The more rigorous cleaning and disinfection procedures may have increased the interval between patients resulting in reduced hospital production. Finally, the worry of being exposed to infection by the new coronavirus may have led individuals to avoid health care, even with symptoms that should not be ignored. 5
The oral cancer care network will need extraordinary resilience to cope with the scenario outlined by the pandemic; its capacity to deal with this task will depend more than ever on organization and investment. Telemedicine might be useful to support diagnosis (eg determining the need for diagnostic procedures), treatment and patient well‐being, 31 but often head and neck cancer commence as a sign rather than a symptom; hence, face‐to‐face consultation with specialists is often inevitable.
Emerging literature indicates that COVID‐19 infection and mortality have been spreading unequally, with poorer, more vulnerable groups being hit the hardest. This reflects inequalities in chronic diseases and the social determinants of health that exacerbate existing NCDs. 32 The indirect effects of the pandemic on cancer care appear to be reflecting this pattern in Brazil. The task of fully recovering cancer care in the country is even more challenging because the disruptive effect of COVID‐19 on the healthcare network was more detrimental in the country's more impoverished regions. We emphasize that studies on cancer mortality in this period will be crucial to assess the pandemic's impact on the treatment and survival of patients with head and neck malignancies resident in Brazil.
CONFLICT OF INTEREST
None to declare.
AUTHOR CONTRIBUTION
Cunha, AR provided substantial contributions to conception and design, acquisition of data, analysis, and interpretation of data; drafting the article; and final approval of the version to be published. Antunes, JLF provided substantial contributions to conception and design, analysis and interpretation of data; revising the article critically for important intellectual content; and final approval of the version to be published. Martin, MD provided substantial contributions to conception and design and interpretation of data; revising the article critically for important intellectual content; and final approval of the version to be published. Petti, S provided substantial contributions to conception and design and interpretation of data; revising the article critically for important intellectual content; and final approval of the version to be published. Hugo, FN provided substantial contributions to conception and design, analysis and interpretation of data; revising the article critically for important intellectual content; and final approval of the version to be published.
da Cunha AR, Antunes LF, Martins MD, Petti S, Hugo FN. The impact of the COVID‐19 pandemic on hospitalizations for oral and oropharyngeal cancer in Brazil. Community Dent Oral Epidemiol. 2021;49:211–215. 10.1111/cdoe.12632
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are openly available in DATASUS at https://datasus.saude.gov.br/
REFERENCES
- 1. Schutte HW, Heutink F, Wellenstein DJ, et al. Impact of time to diagnosis and treatment in head and neck cancer: a systematic review. Otolaryngol Head Neck Surg. 2020;162:446‐457. [DOI] [PubMed] [Google Scholar]
- 2. Graboyes EM, Kompelli AR, Neskey DM, et al. Association of treatment delays with survival for patients with head and neck cancer: a systematic review. JAMA Otoryngol Head Neck Surg. 2019;145:166‐177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Maringe C, Spicer J, Morris M, et al. The impact of the COVID‐19 pandemic on cancer deaths due to delay in diagnosis in England, UK: a national, population‐based, modelling study. Lancet Oncol. 2020;21:1023‐1034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Sud A, Torr B, Jones ME, et al. Effect of delays in the 2‐week‐wait cancer referral pathway during the COVID‐19 pandemic on cancer survival in the UK: a modelling study. Lancet Oncol. 2020;21:1035‐1044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Olmo MJG, Martínez ARO, Ramos BD, Maroto MR, Diaz MC. Perceived vulnerability to coronavirus infection: impact on dental practice. Braz Oral Res. 2020;34:e044. [DOI] [PubMed] [Google Scholar]
- 6. Sardella A, Varoni E, Carrassi A, Pispero A, Lombardi N, Lodi G. Who's afraid of the big bad wolf? The experience of an Oral Medicine Unit in the time of Corona‐Virus. Oral Dis. 2020;1–2. 10.1111/odi.13461. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Ueda M, Martins R, Hendrie PC, et al. Managing cancer care during the COVID‐19 pandemic: agility and collaboration toward a common goal. J Natl Compr Canc Netw. 2020;18:366‐369. [DOI] [PubMed] [Google Scholar]
- 8. Hamilton W. Cancer diagnostic delay in the COVID‐19 era: what happens next? Lancet Oncol. 2020;21:1000‐1002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Alves FA, Saunders D, Sandhu S, Xu Y, Mendonça NF, Treister NS. Implication of COVID‐19 in oral oncology practices in Brazil, Canada, and the United States. Oral Dis. 2020;1–3. 10.1111/odi.13493. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. The Lancet Oncology . Building a more resilient cancer healthcare system. Lancet Oncol. 2020;21:999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. The Lancet Oncology . Safeguarding cancer care in a post‐COVID‐19 world. Lancet Oncol. 2020;21:603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Liang W, Guan W, Chen R, et al. Cancer patients in SARS‐CoV‐2 infection: a nationwide analysis in China. Lancet Oncol. 2020;21:335‐337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Zhang L, Zhu F, Xie L, et al. Clinical characteristics of COVID‐19‐infected cancer patients: a retrospective case study in three hospitals within Wuhan, China. Ann Oncol. 2020;31:894‐901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Jensen AR, Nellemann HM, Overgaard J. Tumor progression in waiting time for radiotherapy in head and neck cancer. Radiother Oncol. 2007;84:5‐10. [DOI] [PubMed] [Google Scholar]
- 15. Abrahão R, Perdomo S, Pinto L, et al. Predictors of survival after head and neck squamous cell carcinoma in South America: the InterCHANGE study. JCO Glob Oncol. 2020;6:486‐499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Seoane J, Alvarez‐Novoa P, Gomez I, et al. Early oral cancer diagnosis: the Aarhus statement perspective. A systematic review and meta‐analysis. Head Neck. 2016;38:E2182‐E2189. [DOI] [PubMed] [Google Scholar]
- 17. Ministry of Health of Brazil . Estimativa 2020 da Incidência de Câncer no Brasil do Instituto Nacional do Câncer José Alencar Gomes da Silva. Rio de Janeiro: INCA; 2019. [Google Scholar]
- 18. Gomes A, Schuch LF, Tarquinio S, Etges A, Vasconcelos A. Reduced demand for oral diagnosis during COVID‐19: a Brazilian center experience. Oral Dis. 2020;1–2. 10.1111/odi.13547. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Cunha AR, Antunes JLF, Martins MD, Petti S, Hugo FN. The impact of the COVID‐19 pandemic on oral biopsies in the Brazilian National Health System. Oral Dis. 2020;1–4. 10.1111/odi.13620. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. National Comprehensive Cancer Network . NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines) – Head and Neck Cancers. Version 2.2020.
- 21. Ministry of Health of Brazil . Painel Coronavírus. https://covid.saude.gov.br/
- 22. Perea LME, Peres MA, Boing AF, Antunes JLF. Trend of oral and pharyngeal cancer mortality in Brazil in the period of 2002 to 2013. Rev Saúde Públ. 2018;52:10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Ministry of Health of Brazil . Lei nº 12.732. de 22 de novembro de 2012. Brasília: Ministry of Health of Brazil; 2012. [Google Scholar]
- 24. Dantas TS, Silva PGB, Sousa EF, et al. Influence of educational level, stage, and histological type on survival of oral cancer in a Brazilian population: a retrospective study of 10 years observation. Medicine. 2016;95:e2314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Lai AG, Pasea L, Banerjee A, et al. Estimated impact of the COVID‐19 pandemic on cancer services and excess 1‐year mortality in people with cancer and multimorbidity: near real‐time data on cancer care, cancer deaths and a population‐based cohort study. BMJ Open. 2020;10:e043828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Brugel M, Carlier C, Essner C, et al. Dramatic changes in oncology care pathways during the COVID‐19 pandemic: the French ONCOCARE‐COV Study. Oncologist. 2020;26:e338–e341. 10.1002/onco.13578 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Poll‐Franse LV, Rooij BH, Horevoorts NJE, et al. Perceived care and well‐being of patients with cancer and matched norm participants in the COVID‐19 crisis – results of a survey of participants in the Dutch PROFILES Registry. JAMA Oncol. 2020;7:279–284. 10.1001/jamaoncol.2020.6093 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Morrison DR, Gentile C, McCammon S, Buczek E. Head and neck oncologic surgery in the COVID‐19 pandemic: our experience in a deep south tertiary care center. Head Neck. 2020;42:1471‐1476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Ranney ML, Griffeth V, Jha AK. Critical supply shortages – the need for ventilators and personal protective equipment during the Covid‐19 pandemic. N Engl J Med. 2020;382:e41. [DOI] [PubMed] [Google Scholar]
- 30. Noronha KVMS, Guedes GR, Turra CM, et al. The COVID‐19 pandemic in Brazil: analysis of supply and demand of hospital and ICU beds and mechanical ventilators under different scenarios. Cad Saúde Pública. 2020;36:e00115320. [DOI] [PubMed] [Google Scholar]
- 31. Martins MD, Carrard VC, Santos CM, Hugo FN. COVID‐19 – are telehealth and tele‐education the answers to keep the ball rolling in dentistry? Oral Dis. 2020;1–2. 10.1111/odi.13527. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Bambra C, Riordan R, Ford J, Matthews F. The COVID‐19 pandemic and health inequalities. J Epidemiol Community Health. 2020;74:964‐968. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are openly available in DATASUS at https://datasus.saude.gov.br/


