Abstract
Objective
First, to investigate how psychotherapists and patients experience the change from in‐person to remote psychotherapy or vice versa during COVID‐19 regarding the therapeutic interventions used. Second, to explore the influence of therapeutic orientations on therapeutic interventions in in‐person versus remote psychotherapy.
Method
Psychotherapists (N = 217) from Austria were recruited, who in turn recruited their patients (N = 133). The therapeutic orientation of the therapists was psychodynamic (22.6%), humanistic (46.1%), systemic (20.7%) or behavioural (10.6%). All the data were collected remotely via online surveys. Therapists and patients completed two versions of the ‘Multitheoretical List of Therapeutic Interventions’ (MULTI‐30) (version 1: in‐person; version 2: remote) to investigate differences between in‐person and remote psychotherapy in the following therapeutic interventions: psychodynamic, common factors, person‐centred, process‐experiential, interpersonal, cognitive, behavioural and dialectical‐behavioural.
Results
Therapists rated all examined therapeutic interventions as more typical for in‐person than for remote psychotherapy. For patients, three therapeutic interventions (psychodynamic, process‐experiential, cognitive interventions) were more typical for in‐person than for remote psychotherapy after correcting for multiple testing. For two therapeutic interventions (behavioural, dialectical‐behavioural), differences between the four therapeutic orientations were more consistent for in‐person than for remote psychotherapy.
Conclusions
Therapeutic interventions differed between in‐person and remote psychotherapy and differences between therapeutic orientations in behavioural‐oriented interventions become indistinct in remote psychotherapy.
Keywords: COVID‐19, interventions, psychotherapy
Key Practitioner Messages.
In times of COVID‐19, psychotherapists and patients experience a change of the treatment format worldwide.
This study examined in Austria how ‘real‐world’ psychotherapists and their patients, who experienced such a change of the format, rate various therapeutic interventions (measured with the MULTI‐30) in in‐person versus remote psychotherapy.
Ratings for therapeutic interventions were higher for in‐person than for remote psychotherapy.
Differences between therapeutic orientations in behavioural and dialectical‐behavioural interventions were not as consistent in remote psychotherapy as in in‐person therapy.
1. INTRODUCTION
The COVID‐19 pandemic has been labelled as the ‘black swan’ for mental health care as well as a turning point for e‐health (Wind et al., 2020). Previous studies showed that the treatment format for the provision of therapeutic interventions changed during COVID‐19 with a reduction of in‐person sessions and an increase of remote sessions via telephone or Internet (e.g., Humer et al., 2020; Probst et al., 2020). It has already been shown before COVID‐19 that remote therapeutic interventions are effective alternatives to the traditional in‐person treatment format (e.g., Carlbring et al., 2018; Castro et al., 2020). Yet, providers of therapeutic interventions usually report that the remote treatment setting is not totally comparable to the in‐person setting (e.g., Connolly et al., 2020; Humer et al., 2020). With regard to the comparability of remote and in‐person treatment, most of the previous studies focused either on the outcome (e.g., Carlbring et al., 2018; Castro et al., 2020) or the therapeutic alliance (e.g., Irvine et al., 2020; Norwood et al., 2018). Irvine et al. (2020) recently reviewed interactional differences between telephone‐based and in‐person psychotherapy and found no substantial differences in the alliance even though telephone sessions were shorter. A randomized controlled trial allocated 80 clients to either in‐person, audio‐, or video‐based psychotherapy and investigated client participation, client hostility, and therapist exploration as alliance variables (Day & Schneider, 2002). While no differences in client hostility and therapist exploration emerged, client participation was lowest in in‐person psychotherapy (Day & Schneider, 2002). Recent studies comparing videoconference‐based and in‐person psychotherapy showed comparable outcome and alliance for both formats in individuals with panic disorder and agoraphobia (Bouchard et al., 2020) and better alliance for videoconference in individuals with generalized anxiety disorder (Watts et al., 2020).
The alliance is considered a common factor, that is, a factor relevant in all psychosocial treatments (other common factors include positive expectations, a healing setting, rationale for symptoms) (for details on common factors, see Laska et al., 2014; Mulder et al., 2017; Wampold, 2015). In contrast, specific factors are factors that are specific for specific psychosocial treatments, for example, cognitive restructuring in cognitive therapy. Although there has been a controversial debate whether common factors or specific factors are more important in psychosocial treatments, current research does not support either any common factor or any specific factor to be an empirically validated working mechanism (Cuijpers et al., 2019).
One reliable and valid instrument capturing the heterogeneity of therapeutic interventions is the ‘Multitheoretical List of Therapeutic Interventions’ (MULTI‐60; McCarthy & Barber, 2009). The MULTI‐60 assesses common factors and specific factors belonging to various specific psychosocial treatments (behavioural, cognitive, dialectical‐behavioural, interpersonal, person‐centred, psychodynamic and process‐experiential). The original MULTI is rather long with 60 items and a short version with 30 items has been developed (MULTI‐30; Solomonov et al., 2019). The MULTI has been used in various international psychotherapy studies. For example, it has been reported that MULTI ratings on therapeutic interventions are influenced by the applied therapeutic orientation (e.g., psychodynamic and behavioural) (King et al., 2020; McCarthy & Barber, 2009), that psychotherapists of a specific orientation integrate therapeutic interventions of other orientations similar to their own (Solomonov et al., 2016) and that the use of certain therapeutic interventions/their combination is associated with patient progress (Boswell et al., 2010; Fisher et al., 2020).
To expand this previous research, the following two research questions were addressed in the current study in patients and therapists, who experienced a change of the treatment format (in‐person to remote and/or remote to in‐person) during their psychotherapy in times of COVID‐19.
-
Research question 1:
Do therapists and/or patients rate the therapeutic interventions measured with the MULTI‐30 as differently typical for in‐person vs. remote psychotherapy? As we found that remote psychotherapy is not totally comparable to in‐person psychotherapy for psychotherapists in a previous study (Humer et al., 2020), we hypothesized that therapeutic interventions differ between in‐person and remote psychotherapy.
-
Research question 2:
Does the therapeutic orientation of the therapist influence how therapists rate therapeutic interventions in in‐person and/or remote psychotherapy? As previous studies showed associations between MULTI ratings and therapeutic orientations (King et al., 2020; McCarthy & Barber, 2009), we hypothesized that the therapeutic orientation influences how therapists rate therapeutic interventions. The previous studies focused on one treatment format. Therefore, we had no specific hypothesis regarding the question of whether the influence of the therapeutic orientation is the same or different in in‐person and remote psychotherapy.
2. METHODS
All participants gave electronic informed consent after reading the data protection declaration. The methods were approved by the Ethics Committee of the Danube University Krems, Austria.
2.1. Participants
Psychotherapists in Austria were recruited by the first author in cooperation with the Austrian Federal Association for Psychotherapy. Therapists received the link to the online psychotherapist survey (see below). In Austria, there are 23 accredited psychotherapy methods (Heidegger, 2017), which can be classified into four orientations: Psychodynamic (25.9% of the therapists in Austria), humanistic (37.8% of the therapists in Austria), systemic (24.3% of the therapists in Austria) and behavioural (12.0% of the therapists in Austria). The behavioural orientation focus on behavioural and cognitive techniques to change maladaptive behaviours or thoughts. Humanistic psychotherapies focus on human development, individual needs, and emphasize positive growth as well as subjective meaning. Psychodynamic approaches focus on revealing or interpreting unconscious conflicts, which are thought to cause mental disorders. The systemic orientation focuses rather on the interactions of groups such as families, their dynamics and patterns. Only these four orientations and not the 23 methods were examined for research question 2. To motivate the therapists to participate, continuing education credit points were offered to them for their participation. In total, N = 222 psychotherapists gave electronic informed consent and completed the survey.
Patients were recruited by the participating psychotherapists. The psychotherapists provided the link to the online patient survey to their patients. In total, N = 139 patients gave electronic informed consent and completed the survey.
To be able to compare in‐person and remote therapeutic interventions, only those psychotherapists and patients were analysed who experienced a change of the treatment format in times of COVID‐19. The change could be from in‐person to remote psychotherapy (in times of COVID‐19 restrictions) and/or from remote psychotherapy to in‐person psychotherapy (when COVID‐19 restrictions were lifted). Five therapists and six patients did not experience a change of treatment format and were excluded from further analyses so that the final sample for the present study comprised N = 217 therapists and N = 133 patients.
2.2. Study design
Two cross‐sectional online surveys were set up with REDCap (Harris et al., 2009, 2019), one for psychotherapists and one for patients. The therapists' and patients' surveys were open from 26 June 2020 until 3 September 2020. This time interval was after the first Austrian COVID‐19 lockdown, which went into force on the 16 March 2020 during which homes were only allowed to be left for five specific reasons and during which in‐person psychotherapy decreased and remote psychotherapy increased in Austria (Probst et al., 2020). This first curfew ended on 30th of April 2020.
The survey for psychotherapists comprised 128 items in total (including the MULTI‐30 as well as other questions, such as free text questions about content, intensity, alliance, and structure of remote vs. in‐person sessions). The psychotherapists received the link to the online psychotherapist survey from the first author or the Austrian Federal Association for Psychotherapy. The items described in the measures below were analysed in the present study.
The survey for the patients consisted of 159 items (including the MULTI‐30 as well as other questions, such as free text questions about content, intensity, alliance, and structure of remote vs. in‐person sessions). The patients received the link to the online patient survey from their psychotherapists, who in turn received this link from the first author or the Austrian Federal Association for Psychotherapy. The items described in the measures below were analysed in the present study. To ensure anonymous data collection, the patients were not matched to the therapists in the online survey.
2.3. Measures
2.3.1. Multitheoretical List of Therapeutic Interventions—30 items
The Multitheoretical List of Therapeutic Interventions (MULTI‐30; Solomonov et al., 2019) is a reliable and valid instrument to assess various therapeutic interventions (common factors and specific factors). It consists of 30 items measuring interventions on the following eight scales (some items belong to more than more scale): Psychodynamic (five items, example item: ‘The therapist made connections between the client's current situation and his/her past’.), common factors (4 items, example item: ‘The therapist worked to give the client hope or encouragement’.), person‐centred (three items, example item: ‘The therapist repeated back to the client (paraphrased) the meaning of what the client was saying’.), process‐experiential (four items, example item: ‘The therapist encouraged the client to identify or label feelings that he/she had in or outside of the session’.), interpersonal (four items, example item: ‘The therapist tried to help the client better understand how the client's problems were due to difficulties in his/her social relationships’.), cognitive (five items, example item: ‘The therapist encouraged the client to explore explanations for events or behaviors other than those that first came to the client's mind’.), behavioural (five items, example item: ‘The therapist encouraged the client to think about, view, or touch things that the client is afraid of’.), dialectical‐behavioural (seven items, example item: ‘The therapist both accepted the client for who he/she is and encouraged him/her to change’.). Each item is rated on a five‐point Likert‐scale (1–5) and the scales are built by averaging the answers given to the related items. There exist versions for patients, therapists and observers. In the current study only the patient and therapist versions were applied. Cronbach's Alpha of the scales have been reported to range between 0.76 and 0.91 for the patient version and between 0.76 and 0.93 for the therapist version (Solomonov et al., 2019). In the original instruction of the MULTI‐30, patients and therapists are asked to rate how typical each item was for the last session. We changed this introduction and asked how typical each item is for in‐person / remote psychotherapy sessions. Thus, therapists and patients had to complete the MULTI‐30 twice. First for remote therapy, then for in‐person psychotherapy.
2.3.2. ICD‐10‐Symptom‐Rating
The ICD‐10‐Symptom‐Rating (ISR; Tritt et al., 2015) is a reliable and valid instrument to assess distress due to mental health problems. It consists of 29 items (rated on five‐point Likert scale), which are used to calculate one global score and five syndrome scores—depression (four items), anxiety (four items), obsessive–compulsive (three items), somatoform (three items) and eating (three items). The ISR was administered to the patients only in order to examine their mental health distress.
2.3.3. Change of treatment format
The change of treatment format was asked as follows. Psychotherapists had to state with how many of their patients there was a change of the treatment format either from in‐person to remote psychotherapy or from remote psychotherapy to in‐person psychotherapy. Patients had to click yes or no to the question of whether they experienced a change of the treatment format either from in‐person to remote psychotherapy or from remote psychotherapy to in‐person psychotherapy.
All digital treatment formats were considered as remote psychotherapy (telephone, internet, chats, E‐mail, …). Both change options (in‐person to remote and remote to in‐person) were considered, since changes from in‐person to remote psychotherapy occurred when COVID‐19 restrictions were applied and changes from remote to in‐person psychotherapy occurred when COVID‐19 restrictions were lifted.
2.4. Statistics
All statistical analyses were performed with SPSS26. Frequencies, percentages, means (M) and standard deviations (SD) were calculated to describe the sample. Differences between therapists of the four therapeutic orientations in gender, age, and professional experience were examined with chi‐squared tests and analyses of variances (ANOVAs). These tests were performed two‐tailed and the significance value was set to p < 0.05.
To investigate research question 1 on differences between the MULTI‐30 scales between in‐person and remote psychotherapy, t tests for dependent samples were calculated, that is, eight t tests to compare the eight MULTI‐30 scales between in‐person and remote psychotherapy in patients and eight further t tests to compare the eight MULTI‐30 scales between in‐person and remote psychotherapy in therapists. The t tests were performed two‐tailed. The significance value was p < 0.05, and we report Bonferroni‐corrected results with p < 0.003125 (p < 0.05/16 t tests). Cohen's d was calculated as effect size, which can be interpreted as follows: small effect 0.2–0.5, medium effect 0.5–0.8 and large effect >0.8.
To examine research question 2, that is, whether the therapeutic orientation of the therapist influences how therapists rate therapeutic interventions in in‐person and remote psychotherapy, eight mixed ANOVAs (one for each MULTI‐30 scale) were performed. These ANOVAs included one within‐subject factor (‘format’: in‐person vs. remote) and one between‐subject factor (‘orientation’: psychodynamic, humanistic, systemic and behavioural). Significant main effects for ‘orientation’ were followed‐up by Bonferroni‐corrected post‐hoc tests. To explain significant interaction effects for ‘format x orientation’, Bonferroni‐corrected simple effects tests compared each pair of therapeutic orientation for each treatment format. The ANOVAs were performed two‐tailed. The significance value was p < 0.05, and we report Bonferroni‐corrected results for main effects of ‘orientation’ and interaction effects for ‘format x orientation’ with p < 0.00625 (p < 0.05/8 ANOVAs).
3. RESULTS
3.1. Sample description
3.1.1. Psychotherapists
Of the N = 217 analysed therapists, 77.0% were female. The therapists were M = 50.66 (SD = 9.65) years old. Most of the therapists were certified psychotherapists in Austria (91.2%) and the rest (8.8%) were trainees conducting psychotherapy under supervision. The professional experience was M = 10.61 (SD = 9.50) years (value was set to 0 for the trainees). Their therapeutic orientations were psychodynamic (22.6%), humanistic (46.1%), systemic (20.7%) or behavioural (10.6%). Table 1 shows comparisons between the four therapeutic orientations in gender, age, and professional experience. Bonferroni‐corrected post‐hoc tests showed that behavioural therapists were significantly younger than psychodynamic (p = 0.017) and systemic (p = 0.004) therapists.
TABLE 1.
Comparisons between therapists of the four therapeutic orientations with regard to gender, age and professional experience
| Variable | Psychodynamic N = 49 | Humanistic N = 100 | Systemic N = 45 | Behavioural N = 23 | Statistics |
|---|---|---|---|---|---|
| Female n (%) | 40 (81.6) | 74 (74.0) | 33 (73.3) | 20 (87.0) | χ 2(3) = 2.73; p = 0.436 |
| Age in years M (SD) | 52.02 (10.69) | 50.24 (9.28) | 53.11 (7.96) | 44.83 (9.87) | F(3;213) = 4.35; p = 0.005 |
| Professional experience in years M (SD) | 12.22 (10.70) | 10.16 (9.84) | 11.71 (8.56) | 6.93 (5.65) | F(3;213) = 1.92; p = 0.128 |
Note: M = Mean; SD = standard deviation.
Most of the therapists worked in their own independent practice (96.8%). The majority had no experience with remote psychotherapy before COVID‐19 (60.4%). Telephone was the preferred treatment format for remote psychotherapy, which was used by 88.5% of the therapists, followed by videoconferencing (76.5%), E‐mail (22.6%), chats (9.2%) and other digital media (2.8%). The therapists changed from in‐person to remote psychotherapy with M = 11.21 (SD = 10.12) patients and from remote psychotherapy to in‐person psychotherapy with M = 9.62 (SD = 10.34) patients.
3.1.2. Patients
Of the N = 133 patients who participated, 70.7% were female. The patients were M = 38.92 (SD = 11.98) years old. Their treatment duration of the current psychotherapy, during which they experienced a change of the treatment format, was M = 21.20 (SD = 18.21) months. Change from in‐person to remote psychotherapy occurred in 96.2% of the patients and change from remote to in‐person psychotherapy occurred in 66.2% of the patients. Most of the patients (84.2%) had no previous experiences with remote psychotherapy before COVID‐19. The patients received remote psychotherapy mostly via telephone (58.6%) or via videoconference (55.6%), whereas E‐mail (12.0%), chats (7.5%) and other digital media (0.8%) were less common. The general symptom distress was moderate with an ISR global score reaching M = 1.16 (SD = 0.69). The ISR syndrome scores were as follows: depression: M = 1.78 (SD = 0.98); anxiety: M = 1.60 (SD = 1.13); obsessive–compulsive: M = 1.29 (SD = 1.16); somatoform: M = 0.62 (SD = 0.90); eating: M = 0.87 (SD = 1.06). These values for the ISR syndrome scales indicate low syndrome distress (Tritt et al., 2015).
3.2. Results for research question 1
Table 2 shows the results of the 16 t tests. To summarize, therapists consistently gave higher ratings for all MULTI‐30 scales for in‐person than for remote psychotherapy and this was statistically significant even after correcting for multiple testing (p < 0.003125). Patients' ratings for therapeutic interventions did not differ that consistently between in‐person and remote psychotherapy. Although, without Bonferroni‐correction, all MULTI‐30 scales (except interpersonal therapy) were higher for in‐person than for remote psychotherapy in the patients' perspective (p < 0.05), differences remained statistically significant only for psychodynamic interventions, process‐experiential interventions, and cognitive interventions after correcting for multiple testing (p < 0.003125). Effect sizes were small for patients and mostly moderate for therapists.
TABLE 2.
Comparisons between in‐person and remote psychotherapy with regard to the MULTI‐30 scales for patients and therapists (across all therapeutic orientations).
| In‐person psychotherapy | Remote psychotherapy | ||||
|---|---|---|---|---|---|
| Perspective | MULTI‐30 scale | M (SD) | M (SD) | Statistics | d |
|
Therapists N = 217 |
PD | 4.04 (0.62) | 3.52 (0.76) | T(216) = 11.68; p < 0.001 | 0.79 |
| CF | 4.37 (0.55) | 4.26 (0.55) | T(216) = 4.93; p < 0.001 | 0.33 | |
| PC | 4.31 (0.61) | 4.11 (0.62) | T(216) = 6.03; p < 0.001 | 0.41 | |
| PE | 4.20 (0.59) | 3.79 (0.70) | T(216) = 10.03; p < 0.001 | 0.68 | |
| IPT | 4.00 (0.73) | 3.64 (0.75) | T(216) = 8.97; p < 0.001 | 0.61 | |
| CT | 3.32 (0.91) | 3.05 (0.83) | T(216) = 7.80; p < 0.001 | 0.53 | |
| BT | 3.18 (1.03) | 2.83 (0.85) | T(216) = 8.65; p < 0.001 | 0.59 | |
| DBT | 3.52 (0.82) | 3.21 (0.69) | T(216) = 9.46; p < 0.001 | 0.64 | |
|
Patients N = 133 |
PD | 3.79 (0.78) | 3.60 (0.73) | T(132) = 4.11; p < 0.001 | 0.36 |
| CF | 4.54 (0.53) | 4.46 (0.55) | T(132) = 2.80; p = 0.006 | 0.24 | |
| PC | 4.28 (0.61) | 4.18 (0.56) | T(132) = 2.04; p = 0.044 | 0.18 | |
| PE | 3.89 (0.77) | 3.72 (0.73) | T(132) = 4.00; p < 0.001 | 0.35 | |
| IPT | 3.92 (0.85) | 3.81 (0.80) | T(132) = 1.91; p = 0.059 | 0.17 | |
| CT | 3.33 (0.79) | 3.15 (0.77) | T(132) = 4.50; p < 0.001 | 0.39 | |
| BT | 3.32 (0.87) | 3.17 (0.83) | T(132) = 2.92; p = 0.004 | 0.25 | |
| DBT | 3.57 (0.72) | 3.46 (0.68) | T(132) = 2.78; p = 0.006 | 0.24 |
Note: MULTI‐30 = Multitheoretical List of Therapeutic Interventions—30 items; PD = psychodynamic scale; CF = common factors scale; PC = Person‐centred scale; PE = process‐experiential scale; IPT = interpersonal scale; CT = cognitive scale; BT = behavioural scale; DBT = dialectical‐behavioural scale; M = mean; SD = standard deviation; d = effect size Cohen's d.
3.3. Results for research question 2
Figures 1, 2, 3, 4, 5, 6, 7, 8 illustrate the therapists' scores on the MULTI‐30 scales for in‐person and remote psychotherapy for the four therapeutic orientations (please note: therapists could only select 1 therapeutic school in the online survey, each therapist was categorized into only one orientation).
FIGURE 1.
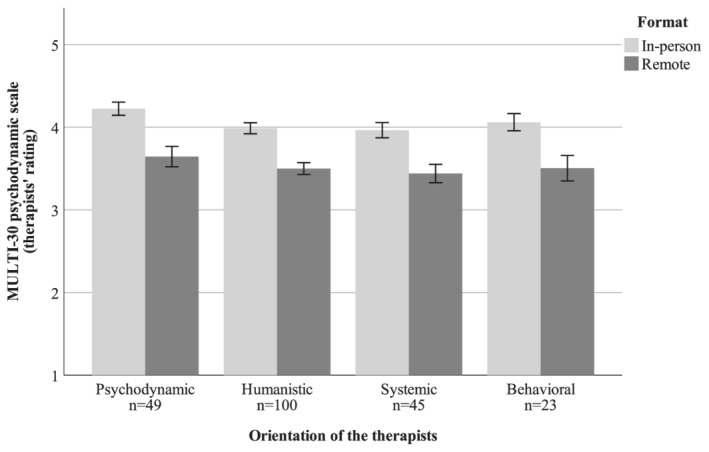
Means ± 1 standard error of the therapists' scores for psychodynamic interventions for in‐person and remote psychotherapy. Note: MULTI‐30 = multitheoretical list of therapeutic interventions—30 items
FIGURE 2.
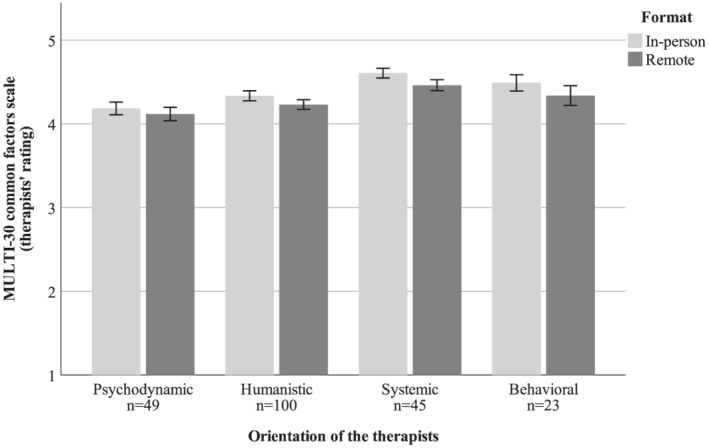
Means ± 1 standard error of the therapists' scores for common factors interventions for in‐person and remote psychotherapy. Note: MULTI‐30 = multitheoretical list of therapeutic interventions—30 items
FIGURE 3.
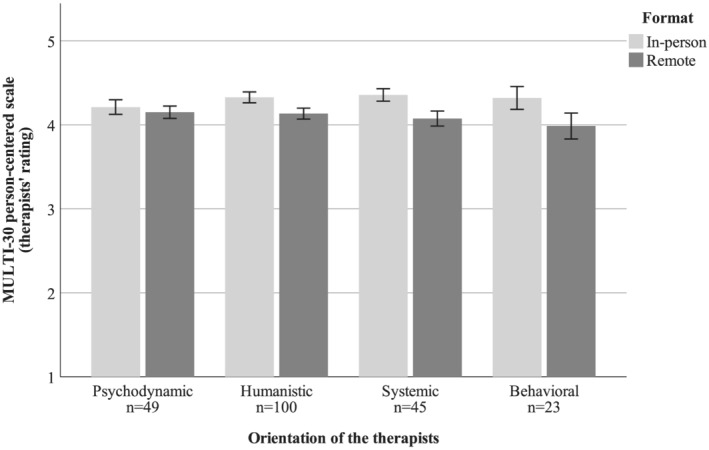
Means ± 1 standard error of the therapists' scores for person‐centred interventions for in‐person and remote psychotherapy. Note: MULTI‐30 = multitheoretical list of therapeutic interventions—30 items
FIGURE 4.
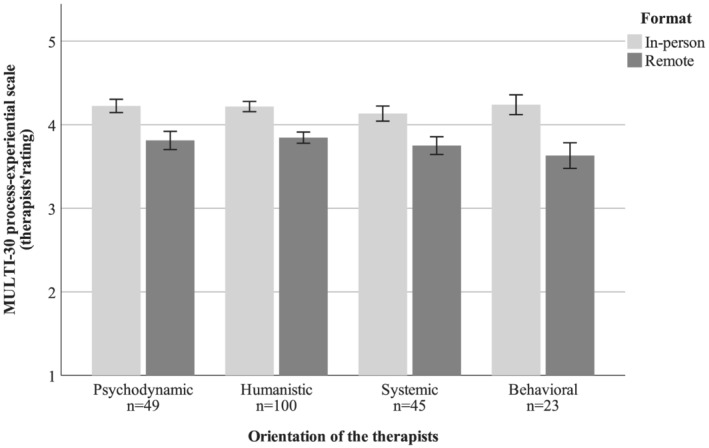
Means ± 1 standard error of the therapists' scores for process‐experiential interventions for in‐person and remote psychotherapy. Note: MULTI‐30 = multitheoretical list of therapeutic interventions—30 items
FIGURE 5.
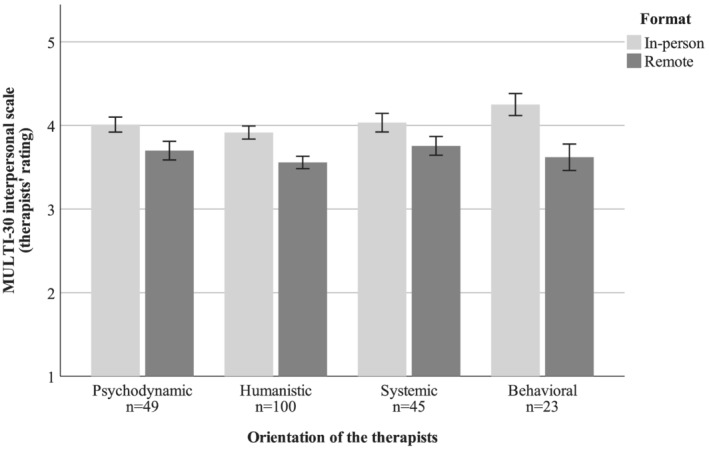
Means ± 1 standard error of the therapists' scores for interpersonal interventions for in‐person and remote psychotherapy. Note: MULTI‐30 = multitheoretical list of therapeutic interventions—30 items
FIGURE 6.
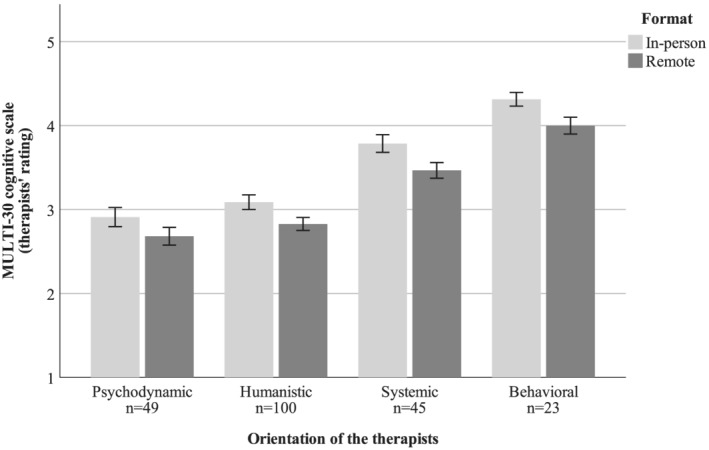
Means ± 1 standard error of the therapists' scores for cognitive interventions for in‐person and remote psychotherapy. Note: MULTI‐30 = multitheoretical list of therapeutic interventions—30 items
FIGURE 7.
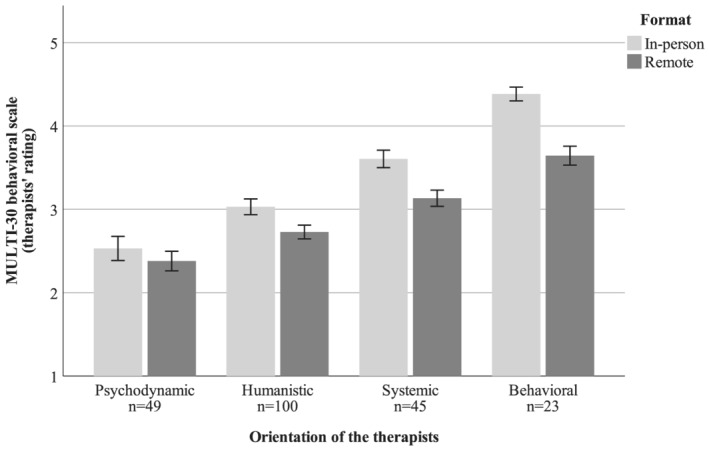
Means ± 1 standard error of the therapists' scores for behavioural interventions for in‐person and remote psychotherapy. Note: MULTI‐30 = multitheoretical list of therapeutic interventions—30 items
FIGURE 8.
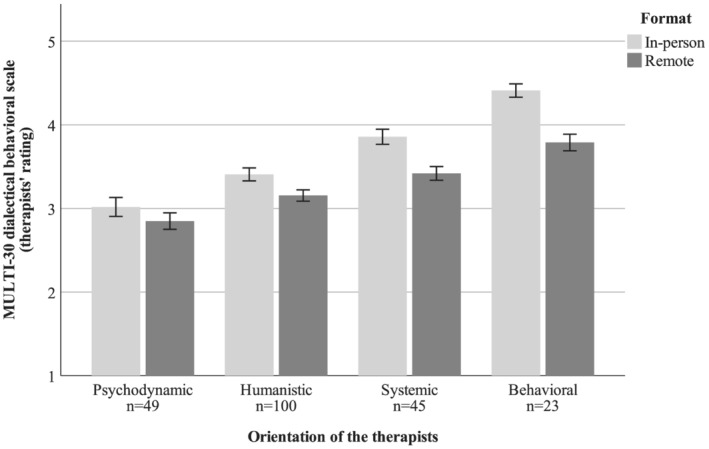
Means ± 1 standard error of the therapists' scores for dialectical behavioural interventions for in‐person and remote psychotherapy. Note: MULTI‐30 = multitheoretical list of therapeutic interventions—30 items
The results of the ANOVAs to address RQ 2 are summarized in Table 3.
TABLE 3.
Results of ANOVAs for main effect ‘orientation’ and interaction effect ‘format x orientation’ for MULTI‐30 therapists' scores.
| MULTI‐30 scale | Main effect ‘orientation’ | Interaction effect ‘format x orientation’ |
|---|---|---|
| PD | F(3;213) = 1.42; p = 0.239 | F(3;213) = 0.231; p = 0.875 |
| CF | F(3;213) = 4.82; p = 0.003 | F(3;213) = 0.59; p = 0.622 |
| PC | F(3;213) = 0.16; p = 0.921 | F(3;213) = 2.44; p = 0.066 |
| PE | F(3;213) = 0.36; p = 0.781 | F(3;213) = 1.00; p = 0.395 |
| IPT | F(3;213) = 0.94; p = 0.421 | F(3;213) = 2.04; p = 0.109 |
| CT | F(3;213) = 29.00; p < 0.001 | F(3;213) = 0.31; p = 0.815 |
| BT | F(3;213) = 25.72; p < 0.001 | F(3;213) = 6.38; p < 0.001 |
| DBT | F(3;213) = 21.19; p < 0.001 | F(3;213) = 6.50; p < 0.001 |
Note: MULTI‐30 = Multitheoretical List of Therapeutic Interventions—30 items; PD = psychodynamic scale; CF = common factors scale; PC = Person‐centred scale; PE = process‐experiential scale; IPT = interpersonal scale; CT = cognitive scale; BT = behavioural scale; DBT = dialectical‐behavioural scale.
For four MULTI‐30 scales (psychodynamic, person‐centred, process‐experiential, interpersonal), the therapeutic orientation of the therapist did not significantly (regardless of correcting for multiple testing, all p > .05) influence how therapists rate therapeutic interventions for in‐person and remote psychotherapy (no significant main effect ‘orientation’ and no significant interaction effect ‘format x orientation’).
Across in‐person and remote psychotherapy, the therapeutic orientation influenced the therapists' ratings on two MULTI‐30 scales (common factors, cognitive) even after correcting for multiple testing with p < 0.00625 (significant main effect ‘orientation’ but no significant interaction effect ‘format x orientation’).
For common factors, post‐hoc tests revealed that common factors were significantly more typical for systemic therapists than for psychodynamic and humanistic therapists.
For cognitive interventions: Post hoc tests revealed that cognitive interventions were significantly more typical for behavioural therapists than for psychodynamic, humanistic and systemic therapists. Moreover, cognitive interventions were significantly more typical for systemic therapists than for psychodynamic and humanistic therapists.
The therapeutic orientation influenced how therapists rated therapeutic interventions and this was different for in‐person vs. remote treatment format for two MULTI‐30 scales (behavioural, dialectical behavioural) even after correcting for multiple testing with p < 0.00625 (significant main effect ‘orientation’ and significant interaction effect ‘format x orientation’).
For behavioural interventions, simple effects tests to explain the interaction showed the following effects.
For in‐person format, behavioural interventions were significantly more typical for behavioural therapists than for psychodynamic, humanistic and systemic therapists. Moreover, behavioural interventions were significantly more typical for systemic than for humanistic and psychodynamic therapists. In addition, behavioural interventions were more typical for humanistic than for psychodynamic therapists.
For remote format, behavioural interventions were significantly more typical for behavioural therapists than for psychodynamic and humanistic therapists. Moreover, behavioural interventions were significantly more typical for systemic than for humanistic and psychodynamic therapists. Systemic and behavioural as well as humanistic and psychodynamic were not significantly different concerning behavioural interventions in remote format anymore, although they were in in‐person format.
For dialectical‐behavioural intervention, simple effects tests to explain the interaction showed the following effects.
For in‐person format, dialectical‐behavioural interventions were significantly more typical for behavioural therapists than for psychodynamic, humanistic, and systemic therapists. Moreover, dialectical behavioural interventions were significantly more typical for systemic than for humanistic and psychodynamic therapists. In addition, dialectical behavioural interventions were more typical for humanistic than for psychodynamic therapists.
For remote format, dialectical‐behavioural interventions were significantly more typical for behavioural therapists than for psychodynamic and humanistic therapists. Moreover, dialectical behavioural interventions were significantly more typical for systemic than for psychodynamic therapists. In addition, dialectical behavioural interventions were more typical for humanistic than for psychodynamic therapists. Systemic and behavioural as well as systemic and humanistic were not significantly different concerning dialectical behavioural interventions in remote format anymore, although they were in the in‐person format.
4. DISCUSSION
The current cross‐sectional study evaluated whether therapeutic interventions, that is, common and specific factors measured with the MULTI‐30, differ between in‐person and remote psychotherapy. This was examined in Austrian therapists and their patients, who experienced a change of the treatment format during COVID‐19. For therapists, also the influence of the therapeutic orientation was analysed. This was not possible for patients in the current study, since the patients were not matched to the therapists in the online survey (to collect data anonymously) and asking the patients to provide the therapeutic orientation of their therapist might produce invalid data as not all mental health care patients are that well informed (e.g., Blease et al., 2020; Paccaloni et al., 2004; Trachsel et al., 2015).
Results showed that therapists rated all examined therapeutic interventions as more typical for the in‐person treatment format than for remote treatment format. Patients rated most MULTI‐30 scales (except interpersonal therapy) higher for in‐person than for remote psychotherapy, but only the differences for psychodynamic, process‐experiential, and cognitive interventions remained significant after correcting for multiple testing. These results expand previous research on the therapeutic alliance showing more differences between in‐person and remote treatment in therapists than in patients (Ertelt et al., 2011). In general, the first hypothesis can be confirmed for therapists and partly for patients, the examined therapeutic interventions differ between face‐to‐face and remote psychotherapy and are more typical for in‐person psychotherapy. This could be explained as follows. First, the remote setting might indeed not be as suited to deliver these therapeutic interventions as the in‐person setting (possibly ‘more activity’, intensity in in‐person therapy). Second, Austrian psychotherapists learned in their psychotherapy training to deliver therapeutic interventions exclusively in‐person and remote psychotherapy was almost non‐existent in Austria before COVID‐19 (patients treated on average per week via telephone M = 0.42, Internet M = 0.18; see Probst et al., 2020). Third, other therapeutic interventions might have been necessary in the time intervals when remote sessions were applied in contrast to the time intervals when in‐person sessions took place. Changes from in‐person to remote sessions occurred in times of COVID‐19 restrictions and changes from remote to in‐person sessions in times when COVID‐19 restrictions were lifted. Hence, other therapeutic interventions, for example, crisis interventions might have been more typical during COVID‐19 restrictions in the remote sessions than in times when in‐person sessions were more common and the MULTI‐30 does not cover crisis interventions. Therapist dyads may also focus more on actual external events and life changes than outside of pandemic times. Fourth, the stressfulness of the pandemic situation for both the therapist and patient might prevent from working in the ‘business as usual’ manner.
The second hypothesis taking the therapists' therapeutic orientation into account can be confirmed to some extent. For behavioural and dialectical‐behavioural interventions, there was an interaction between therapeutic orientation and treatment format meaning that the differences between the orientations on these scales were different in in‐person and remote psychotherapy. Differences between the therapeutic orientations in these two behavioural‐oriented interventions became more indistinct in remote psychotherapy. It should be kept in mind here that the dialectical behavioural scale of the MULTI‐30 includes all five items of the behavioural scale with only two additional unique items added. The results for the dialectical behavioural scale might therefore be a by‐product of the results for the behavioural scale. Regardless of the treatment format, cognitive interventions were more typical in behavioural therapists followed by systemic therapists and common factors were more typical in systemic therapists than in psychodynamic and humanistic ones. Although common factors are thought to be equally relevant in all therapeutic approaches (Laska et al., 2014; Mulder et al., 2017; Wampold, 2015), our result for differences between therapeutic approaches in common factors corresponds to another study, which found higher common factor use in cognitive‐behavioural therapy than in supportive listening (King et al., 2020). Again, regardless of the treatment format, there was no influence of the therapeutic orientation of the therapist on how therapists rated psychodynamic, person‐centred, process‐experiential and interpersonal interventions. This is surprising, since, in relation to other therapeutic orientations, higher psychodynamic intervention scores would be expected for psychodynamic therapists and higher person‐centred as well as process‐experiential intervention scores could be expected for humanistic therapists. This might be explained by the previous finding that therapists of a specific orientation also integrate therapeutic interventions of other orientations (Solomonov et al., 2016).
5. LIMITATIONS AND STRENGTHS
As our study is no randomized controlled trial, there are numerous confounders that could have influenced the results (e.g., remote sessions mostly during COVID‐19 restrictions, younger age of behavioural therapists, …). The nonrandomized design is a limitation of the study. Another shortcoming is the cross‐sectional design, which did not allow to obtain session‐by‐session MULTI‐30 ratings, but MULTI‐30 ratings across sessions for the respective treatment format (in‐person; remote). A longitudinal study investigating session‐by‐session MULTI‐30 ratings and, in parallel, session‐by‐session outcomes (e.g., ISR) would be interesting in the future to compare the impact of therapeutic intervention on the outcome in in‐person versus remote therapy (see, e.g., Boswell et al., 2010 or Fisher et al., 2020). A further limitation is the lack of observer‐based MULTI‐30 ratings. In addition, MULTI‐30 ratings were obtained for the broad category ‘remote psychotherapy’ and MULTI‐30 ratings for specific remote treatment formats (e.g., telephone‐based, videoconferencing) would allow more detailed analyses regarding differences to in‐person psychotherapy. As our participants had to fill out the MULTI‐30 already twice (for in‐person and remote), MULTI‐30 ratings for more specific remote treatment formats were not implemented in the survey. A further shortcoming refers to the recruitment of patients by their therapists. Therapists could have invited preferably their compliant and not too severely distressed patients to partake in the study. This could explain the rather low syndrome scores on the ISR and limit the generalizability of the results. Another explanation for the rather low ISR syndrome scores is that the patients were already in treatment, on average almost 2 years, and the symptoms which were the cause for the psychotherapy had likely improved at the time of this study. Representativeness is further limited due to the overrepresentation of humanistic psychotherapists in our sample compared to the distribution of the therapeutic orientations in the official list of Austrian psychotherapists (46% vs. 38%). It should also be kept in mind that therapists could select exactly one therapeutic school in the online survey. Some therapists could have more than one therapeutic orientation (e.g., psychodynamic and humanistic) and results might differ when these therapists are grouped not only in one but multiple orientations. Future research should consider this and also engagement measures or even synchronicity to evaluate the differences in the dyadic dimension.
Despite these limitations, the study also has several strengths. The MULTI‐30 was used to broaden the focus on therapeutic interventions including specific and common factors and not only the therapeutic alliance was examined as in most previous studies. In addition, we could present the therapists' and patients' perspectives on in‐person and remote therapeutic interventions. The results have high clinical relevance and representativeness, since therapists and patients were examined during the clinical routine in the real‐world setting. Moreover, we could recruit a rather large sample size of therapists and patients who experienced changes in the treatment format, which is a relevant topic during COVID‐19. Thereby, therapists of all four orientations eligible in Austria were represented and research integrating various therapeutic orientations is scarce.
Practical implications of the results are as follows: Incorporating training modules to provide remote therapeutic interventions both in psychotherapy basic training as well as in training programmes aimed at graduated psychotherapists might help therapists to become better acquainted with remote therapeutic interventions, which might increase these therapists' MULTI‐30 ratings for remote sessions. Moreover, practitioners should be aware that different therapeutic interventions can be tailored differently well to the requirements of remote psychotherapy (e.g., the largest differences between remote and in‐session for therapists emerged for psychodynamic interventions).
To conclude, the results of the current study show that the examined therapeutic interventions are more typical for in‐person than for remote psychotherapy, especially for therapists and less pronounced for patients. In addition, remote psychotherapy is associated with fewer differences between therapeutic orientations in behavioural‐oriented interventions. Further qualitative research of the free text questions of the survey is ongoing and will reveal further insights.
6.
CONFLICT OF INTEREST
All authors have no conflict of interest related to this paper. Some co‐authors work for the ‘Austrian Federal Association for Psychotherapy’ (partner of the Danube University Krems for this research project) and are therefore interested in representing the Austrian psychotherapists well, but this did not influence the study or the results.
ACKNOWLEDGEMENTS
The authors would like to thank the participating therapists and patients.
Probst T, Haid B, Schimböck W, et al. Therapeutic interventions in in‐person and remote psychotherapy: Survey with psychotherapists and patients experiencing in‐person and remote psychotherapy during COVID‐19. Clin Psychol Psychother. 2021;28:988–1000. 10.1002/cpp.2553
DATA AVAILABILITY STATEMENT
Data regarding this study will not be shared, because clinical data were investigated and the data protection the participants signed included a statement that the data will not be shared.
REFERENCES
- Blease, C. R. , Arnott, T. , Kelley, J. M. , Proctor, G. , Kube, T. , Gaab, J. , & Locher, C. (2020). Attitudes about informed consent: An exploratory qualitative analysis of UK psychotherapy trainees. Frontiers in Psychiatry, 11, 183. 10.3389/fpsyt.2020.00183 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boswell, J. F. , Castonguay, L. G. , & Wasserman, R. H. (2010). Effects of psychotherapy training and intervention use on session outcome. Journal of Consulting and Clinical Psychology, 78, 717–723. 10.1037/a0020088 [DOI] [PubMed] [Google Scholar]
- Bouchard, S. , Allard, M. , Robillard, G. , Dumoulin, S. , Guitard, T. , Loranger, C. , … Corno, G. (2020). Videoconferencing psychotherapy for panic disorder and agoraphobia: Outcome and treatment processes from a non‐randomized non‐inferiority trial. Frontiers in Psychology, 11, 2164. 10.3389/fpsyg.2020.02164 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carlbring, P. , Andersson, G. , Cuijpers, P. , Riper, H. , & Hedman‐Lagerlöf, E. (2018). Internet‐based vs. face‐to‐face cognitive behavior therapy for psychiatric and somatic disorders: An updated systematic review and meta‐analysis. Cognitive Behaviour Therapy, 47, 1–18. 10.1080/16506073.2017.1401115 [DOI] [PubMed] [Google Scholar]
- Castro, A. , Gili, M. , Ricci‐Cabello, I. , Roca, M. , Gilbody, S. , Perez‐Ara, M. Á. , … McMillan, D. (2020). Effectiveness and adherence of telephone‐administered psychotherapy for depression: A systematic review and meta‐analysis. Journal of Affective Disorders, 260, 514–526. 10.1016/j.jad.2019.09.023 [DOI] [PubMed] [Google Scholar]
- Connolly, S. L. , Miller, C. J. , Lindsay, J. A. , & Bauer, M. S. (2020). A systematic review of providers' attitudes toward telemental health via videoconferencing. Clinical Psychology: Science and Practice, 27, e12311. 10.1111/cpsp.12311 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cuijpers, P. , Reijnders, M. , & Huibers, M. J. H. (2019). The role of common factors in psychotherapy outcomes. Annual Review of Clinical Psychology, 15, 207–231. 10.1146/annurev-clinpsy-050718-095424 [DOI] [PubMed] [Google Scholar]
- Day, S. X. , & Schneider, P. L. (2002). Psychotherapy using distance technology: A comparison of face‐to‐face, video, and audio treatment. Journal of Counseling Psychology, 49, 499–503. 10.1037/0022-0167.49.4.499 [DOI] [Google Scholar]
- Ertelt, T. W. , Crosby, R. D. , Marino, J. M. , Mitchell, J. E. , Lancaster, K. , & Crow, S. J. (2011). Therapeutic factors affecting the cognitive behavioral treatment of bulimia nervosa via telemedicine versus face‐to‐face delivery. The International Journal of Eating Disorders, 44, 687–691. 10.1002/eat.20874 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fisher, H. , Rafaeli, E. , Bar‐Kalifa, E. , Barber, J. P. , Solomonov, N. , Peri, T. , & Atzil‐Slonim, D. (2020). Therapists' interventions as a predictor of clients' emotional experience, self‐understanding, and treatment outcomes. Journal of Counseling Psychology, 67, 66–78. 10.1037/cou0000377 [DOI] [PubMed] [Google Scholar]
- Harris, P. A. , Taylor, R. , Minor, B. L. , Elliott, V. , Fernandez, M. , O'Neal, L. , … Duda, S. N. (2019). The REDCap consortium: Building an international community of software platform partners. Journal of Biomedical Informatics, 95, 103208. 10.1016/j.jbi.2019.103208 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris, P. A. , Taylor, R. , Thielke, R. , Payne, J. , Gonzalez, N. , & Conde, J. G. (2009). Research electronic data capture (REDCap)—A metadata‐driven methodology and workflow process for providing translational research informatics support. Journal of Biomedical Informatics, 42, 377–381. 10.1016/j.jbi.2008.08.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heidegger, K.‐E. (2017). Psychotherapy in Austria. European Association for Psychotherapy. https://www.europsyche.org/app/uploads/2019/05/Situation-Psychotherapy-in-Austria-2017-10-20.pdf
- Humer, E. , Pieh, C. , Kuska, M. , Barke, A. , Doering, B. K. , Gossmann, K. , … Probst, T. (2020). Provision of psychotherapy during the COVID‐19 pandemic among Czech, German and Slovak psychotherapists. International Journal of Environmental Research and Public Health, 17, 4811. 10.3390/ijerph17134811 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Humer, E. , Stippl, P. , Pieh, C. , Pryss, R. , & Probst, T. (2020). Psychodynamic, humanistic, systemic, and behavioral psychotherapists' experiences with remote psychotherapy during COVID‐19 in Austria: A cross‐sectional online survey. Journal of Medical Internet Research, 22, e20246. 10.2196/20246 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Irvine, A. , Drew, P. , Bower, P. , Brooks, H. , Gellatly, J. , Armitage, C. J. , … Bee, P. (2020). Are there interactional differences between telephone and face‐to‐face psychological therapy? A systematic review of comparative studies. Journal of Affective Disorders, 265, 120–131. 10.1016/j.jad.2020.01.057 [DOI] [PMC free article] [PubMed] [Google Scholar]
- King, B. R. , Boswell, J. F. , Schwartzman, C. M. , Lehrbach, K. , Castonguay, L. G. , & Newman, M. G. (2020). Use of common and unique techniques in the early treatment phase for cognitive‐behavioral, interpersonal/emotional, and supportive listening interventions for generalized anxiety disorder. Psychotherapy, 57, 457–463. 10.1037/pst0000277 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laska, K. M. , Gurman, A. S. , & Wampold, B. E. (2014). Expanding the lens of evidence‐based practice in psychotherapy: A common factors perspective. Psychotherapy, 51, 467–481. 10.1037/a0034332 [DOI] [PubMed] [Google Scholar]
- McCarthy, K. S. , & Barber, J. P. (2009). The Multitheoretical List of Therapeutic Interventions (MULTI): Initial report. Psychotherapy Research, 19, 96–113. 10.1080/10503300802524343 [DOI] [PubMed] [Google Scholar]
- Mulder, R. , Murray, G. , & Rucklidge, J. (2017). Common versus specific factors in psychotherapy: Opening the black box. The Lancet Psychiatry, 4, 953–962. 10.1016/S2215-0366(17)30100-1 [DOI] [PubMed] [Google Scholar]
- Norwood, C. , Moghaddam, N. G. , Malins, S. , & Sabin‐Farrell, R. (2018). Working alliance and outcome effectiveness in videoconferencing psychotherapy: A systematic review and noninferiority meta‐analysis. Clinical Psychology & Psychotherapy, 25, 797–808. 10.1002/cpp.2315 [DOI] [PubMed] [Google Scholar]
- Paccaloni, M. , Pozzan, T. , & Zimmermann, C. (2004). Being informed and involved in treatment: What do psychiatric patients think? A review. Epidemiology and Psychiatric Sciences, 13, 270–283. 10.1017/s1121189x00001792 [DOI] [PubMed] [Google Scholar]
- Probst, T. , Stippl, P. , & Pieh, C. (2020). Changes in provision of psychotherapy in the early weeks of the COVID‐19 lockdown in Austria. International Journal of Environmental Research and Public Health, 17, 3815. 10.3390/ijerph17113815 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Solomonov, N. , Kuprian, N. , Zilcha‐Mano, S. , Gorman, B. S. , & Barber, J. P. (2016). What do psychotherapy experts actually do in their sessions? An analysis of psychotherapy integration in prototypical demonstrations. Journal of Psychotherapy Integration, 26, 202–216. 10.1037/int0000021 [DOI] [Google Scholar]
- Solomonov, N. , McCarthy, K. S. , Gorman, B. S. , & Barber, J. P. (2019). The Multitheoretical List of Therapeutic Interventions—30 items (MULTI‐30). Psychotherapy Research, 29, 565–580. 10.1080/10503307.2017.1422216 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trachsel, M. , Holtforth, M. G. , Biller‐Andorno, N. , & Appelbaum, P. S. (2015). Informed consent for psychotherapy: Still not routine. The Lancet Psychiatry, 2, 775–777. 10.1016/S2215-0366(15)00318-1 [DOI] [PubMed] [Google Scholar]
- Tritt, K. , Heymann, F. , Zaudig, M. , Probst, T. , Loew, T. , Klapp, B. , … Buehner, M. (2015). ICD‐10‐Symptom‐Rating (ISR)—Das Handbuch zum Fragebogen. Graz: Neobooks. [Google Scholar]
- Wampold, B. E. (2015). How important are the common factors in psychotherapy? An update. World Psychiatry, 14, 270–277. 10.1002/wps.20238 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watts, S. , Marchand, A. , Bouchard, S. , Gosselin, P. , Langlois, F. , Belleville, G. , & Dugas, M. J. (2020). Telepsychotherapy for generalized anxiety disorder: Impact on the working alliance. Journal of Psychotherapy Integration, 30, 208–225. 10.1037/int0000223 [DOI] [Google Scholar]
- Wind, T. R. , Rijkeboer, M. , Andersson, G. , & Riper, H. (2020). The COVID‐19 pandemic: The “black swan” for mental health care and a turning point for e‐health. Internet Interventions, 20, 100317. 10.1016/j.invent.2020.100317 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data regarding this study will not be shared, because clinical data were investigated and the data protection the participants signed included a statement that the data will not be shared.


