Abstract
Aims
To investigate the impact of COVID‐19 pandemic on health‐care provision to patients suffering from pelvic floor dysfunctions in Italy.
Methods
A retrospective web‐based interdisciplinary survey was mailed by the Italian Society of Urodynamics to members involved in pelvic floor dysfunctions management from June 22, 2020 to July 17, 2020. The 84‐item questionnaire investigated the period March–June 2020 (first epidemic wave) and showed high content validity. The primary outcome was the mean rate of cancellation for health‐care services. Secondary outcomes included estimation of the accumulated surgeries backload until return to baseline activity and of the recovery pattern, using linear regression and scenario‐based forecasting.
Results
A total of 85 participants provided complete responses. Respondents were mostly urologists (47%), followed by gynecologists (29.5%) and physiatrists (17.6%). On average, 78.4% of outpatient services and 82.7% of functional surgeries were canceled, without significant differences by geographical distribution. An impact on patients' quality of life was anticipated by most of the respondents (87%) and 48.2% also reported potentially serious health risks for patients. Thirty‐three percent of the respondents reported the use of telemedicine. If the nation‐wide surgical activity increases by 20% postpandemic, it would take 37 months to clear the backlog of functional surgeries. We acknowledge the inherent limitations of the survey methodology and retrospective design.
Conclusions
Access to care for patients suffering from pelvic floor dysfunctions has been dramatically affected by the COVID‐19 outbreak. The indirect effects of this unprecedented disruption on pelvic floor dysfunctions care may last for several months.
Keywords: benign prostatic hyperplasia, chronic pelvic pain, COVID‐19 pandemic, cystitis, incontinence, overactive bladder, pelvic floor dysfunction, pelvic organ prolapse, perineal fistula
1. INTRODUCTION
Italy has been early and heavily affected by the Coronavirus Disease 2019 (COVID‐19) pandemic. 1 During February 2020, a COVID‐19 outbreak occurred in Lombardy, and by the beginning of March, the virus had spread to all Italian regions, leading to the national extension of the quarantine lockdown on March 10. From March 30, 2020, Italy saw the first significant fall in the number of new cases, and starting from May 4, the government progressively reduced the restrictions. A plateau in the number of new cases fluctuating around 200/day was achieved from June 1. 2
The unprecedented measures adopted by the Italian authorities included the suspension of all time‐sensitive, elective procedures, 3 , 4 similar to what happened worldwide, 5 including treatments for pelvic floor dysfunctions (PFD). PFD are highly prevalent conditions that can severely impact patients' quality of life and may lead to severe complications; 6 , 7 , 8 however, they have been generally included altogether among nonlife‐threatening deferrable diseases. 4 , 5
Italian Society of Urodynamics (SIUD) (www.siud.it) is a multidisciplinary national Society aimed at improving the prevention and management of PFD, promoting research, and disseminating knowledge of these disabling conditions.
Scant real‐life data are available about the impact of the COVID‐19 pandemic on the health‐care services provision to patients with PFD. To fill this gap, SIUD conducted an online national interdisciplinary survey titled “Pelvic floor dysfunctions and COVID‐19” to elucidate how the medical community has been managing patients with PFD during the first wave of the pandemic, with an effort to estimate the accumulated backload of activities and the recovery times in the postcrisis period.
2. MATERIALS AND METHODS
2.1. Overview
For this national study, we used the platform www.surveymonkey.com and designed an online survey on the changes that the COVID‐19 outbreak produced on health‐care provision to PFD patients in Italy over a 4‐month period (March–June 2020). This time interval was chosen to cover both the lockdown period and the early postlockdown period. The target population was that of physicians specifically dealing with PFD patients. All physicians with SIUD memberships, including urologists, gynecologists, proctologists, and physiatrists, were invited by email to participate voluntarily in a closed survey by clicking on a link, allowing for Web‐based data entry.
2.2. Survey development and data collection
Details of the survey development process and the full questionnaire are presented in the Supporting Information File. The final questionnaire comprised 84 items divided in five pages (three domains): p. 1: “Preliminary information” covering respondents demographics (three items) and characteristics of their health‐care facility (six items); p. 2: “Professional and patients impact of COVID‐19” covering personal and professional impact (five items), use of telemedicine (one item), estimated patients impact (one item), rate of elective versus urgent health services provision (one item), estimated change in resources available for PFD patients in the coming months (one item), estimated delay of surgeries for PFD (one item); p. 3–5: “Impact of COVID‐19 on healthcare services provision,” covering baseline monthly volume of several outpatient services and functional surgery procedures (13 items) and estimated monthly rates of cancellation from March to June 2020 (52 items). Evaluated procedures covered surgery for stress urinary incontinence (SUI), pelvic organ prolapse (POP), benign prostatic hyperplasia (BPH), perineal fistulas, and anorectal dysfunctions.
The first invitation to participate in the study was mailed on June 22, 2020 and three reminders were sent until the closure of the survey on July 17, 2020 (26 days). The responses were accrued through the Survey Monkey website. The final analysis included only complete cases defined as participants providing complete information about at least one health‐care service in the “Impact of COVID‐19 on healthcare services provision” domain.
2.3. Outcomes
The primary outcome was the overall mean rate of cancellation per health‐care service. The secondary outcomes were mean cancellation rates by geographical macroareas and the responses to the questions in the “Professional and patients impact of COVID‐19” domain. Furthermore, the overall accumulated procedures backload until the return to the usual activity and the subsequent projected patterns of functional surgery recovery were estimated.
2.4. Statistical analysis
Demographic data and COVID‐19 impact were presented in a descriptive manner as frequencies and proportions or mean values with standard deviation (SD). To account for the pre‐COVID number of services that each single medical center provided, cancellation mean rates were calculated using weighing by the reported baseline volumes of activity.
Heat maps were created to display the impact of COVID‐19 on outpatient services and functional surgeries for PFD patients by geographical region. The hypothesis of difference in overall cancellation rates between macroareas (North, Center, and South) was tested by χ 2 statistics. The heat map on the total number of COVID‐19 cases per region at the date of June 30, 2020 is shown in Figure S1.
A univariate analysis was performed to assess the associations between several meaningful respondents' characteristics and cancellation rates in the months of April (epidemic peak) and June (last surveyed month), based on Mann–Whitney U test, analysis of variance, and Spearman correlation, as appropriate.
All tests were two‐sided and the significance level was set to p < .05. Statistical analysis was performed using Statistical Package for the Social Sciences (SPSS®), version 25.0 (IBM Corp.).
The FORECAST function of Excel (Microsoft Excel for Office 365 MSO v.2002) projects future values along a line of best fit by using a linear regression model based on historical data; it was used to predict monthly cancellation rates (with 95% confidence intervals) from July 2020 until the return to pre‐COVID activity (zero cancellation rate) and to calculate the overall functional surgery backload. The time it would take to clear the backload was estimated assuming three possible scenarios of 10%, 20%, and 30% future increases in baseline surgical activity. 5
3. RESULTS
3.1. Respondents characteristics
Out of 91, 85 participants provided complete responses and were analyzed (completion rate of 93.4%). The mean time spent to complete the survey was 8 min and 10 s. Demographic data were summarized in Table 1. The highest proportion of respondents was based in Northern Italy (56.5%), also according to the higher offer of health‐care services in this area. 9 Most of the respondents were based in public hospitals functioning as hub centers (61.2%) and equipped with an emergency department (76.5%), and 64.9% in hospitals partly or fully involved to treat COVID‐19 patients. About half (47%) of respondents were urologists, followed by gynecologists and physiatrists.
Table 1.
Demographics of survey respondents (N = 85)
| Characteristics | N (%) |
|---|---|
| Age (years) | |
| <30 | 1 (1.2) |
| 30–39 | 17 (20.0) |
| 40–49 | 22 (25.9) |
| 50–59 | 27 (31.7) |
| >60 | 18 (21.2) |
| Gender | |
| Male | 42 (49.4) |
| Female | 43 (50.6) |
| Geographic macroarea | |
| Northern Italy | 48 (56.5) |
| Central Italy | 26 (30.6) |
| Southern Italy | 11 (12.9) |
| Hospital context | |
| Public | 58 (68.2) |
| Private | 12 (14.1) |
| Mixed | 15 (17.7) |
| Hospital function | |
| Hub | 49 (57.6) |
| Spoke | 31 (36.5) |
| Missing | 5 (5.9) |
| Hospital with emergency department | |
| Yes | 65 (76.5) |
| Hospital bed number | |
| <200 | 24 (28.2) |
| 200–500 | 21 (24.7) |
| 500–1000 | 20 (23.5) |
| >1000 | 17 (20.0) |
| Missing | 3 (3.5) |
| COVID‐19 hospital | |
| Yes | 12 (14.1) |
| No | 30 (35.3) |
| Mixed | 43 (50.6) |
| Specialty | |
| Urology | 34 (40.0) |
| Pediatric urology | 3 (3.5) |
| Neurourology | 3 (3.5) |
| Gynecology | 25 (29.5) |
| Proctology | 2 (2.4) |
| Physiatry | 15 (17.6) |
| Other | 3 (3.5) |
Note: Northern Italy: Aosta Valley, Piedmont, Liguria, Lombardy, Emilia‐Romagna, Veneto, Friuli‐Venezia Giulia, and Trentino‐Alto Adige/Südtirol; Central Italy: Abruzzo, Lazio, Marche, Tuscany, Umbria; Southern Italy: Apulia, Basilicata, Campania, Calabria, Molise, Sardinia, Sicily.
This article is being made freely available through PubMed Central as part of the COVID-19 public health emergency response. It can be used for unrestricted research re-use and analysis in any form or by any means with acknowledgement of the original source, for the duration of the public health emergency.
3.2. Professional and patients impact of COVID‐19
The results of this domain are summarized in Table 2. During the emergency, most of the respondents (70.6%) had their workload decreased or much decreased, while 25.9% were deployed to activities not related to their specialty. Interestingly, 25 (29.4%) respondents reported unchanged or increased/much‐increased workload; they have been more frequently deployed to assist COVID‐19 patients (48% vs. 16.7%; p = .002), were more frequently working in a public context (88% vs. 60%; p = .008) and COVID/mixed (84% vs. 56.7%; p = .02) facilities, and in hospitals with an emergency department (92% vs. 70%; p = .03), compared with those reporting decreased workload.
Table 2.
Answers to the "Professional and patients impact of COVID‐19" domain (N = 85)
| Questions | N (%) |
|---|---|
| Have you undergone a COVID‐19 examination (swab, serology)? | |
| Yes | 73 (85.9) |
| Have you been infected by SARS‐Cov‐2? | |
| Yes | 3 (3.5) |
| Have you had close contact with COVID‐19 patients in your clinical practice? | |
| Yes | 44 (51.8) |
| Your workload during the emergency was: | |
| Much decreased | 27 (31.8) |
| Decreased | 33 (38.8) |
| Unchanged | 10 (11.8) |
| Increased | 13 (15.3) |
| Much increased | 2 (2.3) |
| Have tele‐medicine been used in your department for patients with pelvic floor dysfunctions? | |
| Yes | 28 (32.9) |
| Did you carry out clinical or supporting activities, not related to your specialty during the emergency? | |
| Yes, in a COVID ward | 15 (17.7) |
| Yes, in the Emergency Department | 7 (8.2) |
| No | 63 (74.1) |
| In your opinion, postponing nonurgent services for pelvic floor dysfunctions, what kind of impact did it have, or will it have on patients? | |
| Impact on quality of life | 33 (38.8) |
| Impact on quality of life but also potentially serious health risks in some cases | 36 (42.4) |
| Impact on quality of life but also potentially serious health risks in many cases | 5 (5.9) |
| Negligible impact | 11 (12.9) |
| No impact | 0 |
| In the coming months, the resources for pelvic floor dysfunctions care in your healthcare facility will be | |
| Much decreased | 12 (14.1) |
| Decreased | 32 (37.7) |
| Unchanged | 33 (38.8) |
| Increased | 8 (9.4) |
| The average waiting time in your department for surgical procedures in patients with pelvic floor dysfunctions is | |
| Increased by up to 3 months | 27 (31.7) |
| Increased by 4–5 months | 28 (32.9) |
| Increased by more than 5 months | 15 (17.7) |
| Unchanged | 15 (17.7) |
Abbreviations: COVID‐19, Coronavirus Disease 2019; SARS‐Cov‐2, severe acute respiratory syndrome coronavirus 2.
This article is being made freely available through PubMed Central as part of the COVID-19 public health emergency response. It can be used for unrestricted research re-use and analysis in any form or by any means with acknowledgement of the original source, for the duration of the public health emergency.
Most of the clinical activity (75.4%; SD: 27.1) during the emergency was performed for urgent conditions. About one‐third (32.9%) of the respondents reported some use of telemedicine for PFD patients. Most of the respondents (87%) reported that the health‐care services postponement affected or will affect PFD patients' quality of life, and 48.2% also reported potentially serious health risks for patients.
According to 81.3% of the respondents, the average waiting time for surgeries will increase (by at least 5 months for 50.6% of respondents). Future shortage of resources for PFD care was anticipated by 51.8% of respondents.
3.3. Impact of COVID‐19 on health‐care services
3.3.1. Outpatient activity
Figure 1 shows the cancellation rates for consultations, outpatient investigations, and procedures during March–June 2020. The overall mean cancellation rate was 78.4% (SD: 21.6), with a cancellation peak in April (91.1%; SD: 17.5). Among outpatient investigations, uroflowmetry and urodynamics have suffered the greatest cutdown. Overall cancellation rates of outpatient procedures were quite overlapping around 81%.
Figure 1.
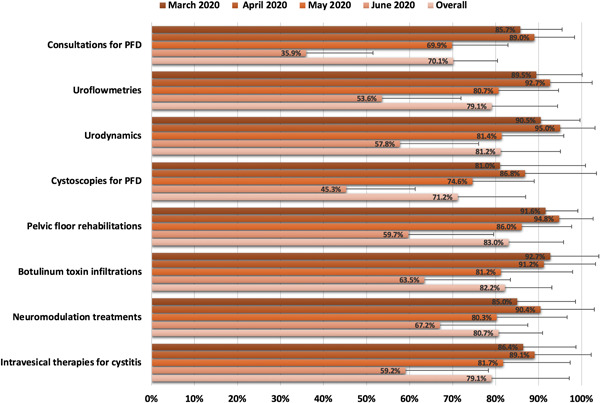
Mean cancellation rates (with standard deviations) for outpatient consultations, investigations, and procedures
3.3.2. Functional surgery
Figure 2 shows the cancellation rates for different functional surgeries during March–June 2020. The overall mean cancellation rate was 82.7% (SD: 14.2), with a cancellation peak again in April 2020 (90.4%; SD: 12.7). All evaluated surgeries were affected by a substantial cutdown, with numerically higher overall cancellation rates for SUI and POP procedures.
Figure 2.
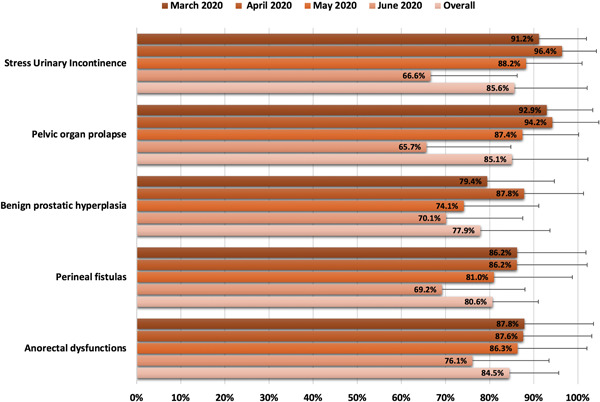
Mean cancellation rates (with standard deviations) for functional surgeries
3.3.3. Impact by geographical distribution
The heat map in Figure 3A shows the degree of cancellation of outpatient activities by geographical distribution. No statistically significant differences were found between high COVID‐19 incidence—Northern macroarea (72.7%; SD: 17.8) and intermediate incidence—Central macroarea (83.7%; SD: 9.7; p = .4) or low incidence—Southern macroarea (85.8%; SD: 8.7; p = .3).
Figure 3.

Heat maps showing mean cancellation rates by region over the period covered by the survey (March–April 2020) for outpatient health‐care services (A) and functional surgery procedures (B)
The geographical distribution of the degree of functional surgery cancellation is shown in Figure 3B. Again, no statistically significant differences were found between high COVID‐19 incidence—Northern macroarea (79.5%; SD: 17.5) and intermediate incidence—Central macroarea (93.9%; SD: 5.6; p = .3) or low incidence—Southern macroarea (86.8%; SD: 7.65; p = .7).
3.4. Univariate analysis
Higher urodynamics cancellation rates were observed in April in public (98%) versus private (94%) and mixed (90%) hospitals (p = .029), and in COVID (100%) versus mixed (98%) and no‐COVID (90%) hospitals (p = .018) (Table S1). The public context was also associated with a higher cutdown on BPH surgery in April (p = .015). Hospitals with an emergency department suffered the highest cancellation rates in June compared with those without; the differences were statistically significant for uroflowmetry (51.2% vs. 81.4%; p = .047), urodynamics (51.4% vs. 89.3%; p = .019), and pelvic floor rehabilitation (51.8% vs. 69%; p = .001). Redeployment to assist COVID‐19 patients was associated with higher consultation cancellation rates in April (95.3% vs. 85.1%; p = .037).
3.5. Surgical backloads and recovery times
Estimated backload of functional surgeries and projected recovery patterns are displayed in Figure 4. Based on a 20% increase in baseline surgical volume, it was estimated that it would take 37 months to clear the accumulated backload of surgeries resulting from previous cancellations. If baseline surgical volume was increased by 10%, it would take 64 months to recover the backload, whereas with a 30% increase in baseline activity, it would take 28 months.
Figure 4.
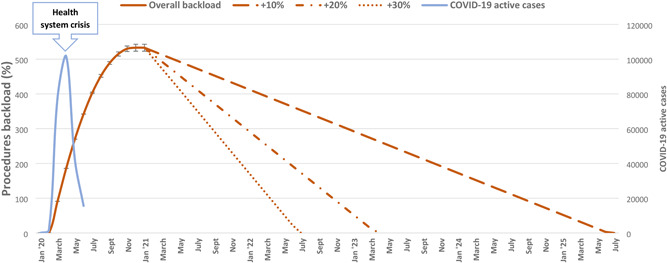
Estimated functional surgery backload (with 95% confidence intervals) and projected recovery patterns based on three hypothetical scenarios (10%, 20%, and 30% increases in baseline surgical volume). The incidence of COVID‐19 in Italy during the period covered by the survey is also shown. COVID‐19, Coronavirus Disease 2019
4. DISCUSSION
To our knowledge, this is the first survey to examine the impact of the COVID‐19 pandemic on health‐care provision to patients with PFD, elucidating how the medical specialists changed the management of these patients in a severely affected country. Sudden, drastic, and widespread cancellation/postponement of all elective health‐care services, prioritization according to an emergency/urgency principle, and an initial effort in the use of telemedicine emerged to be the main features of the early reaction. Both outpatient and inpatient clinical activities were heavily affected. More than 75% of the activity was performed only for urgent conditions. Cancellation rates reached a peak in the month of April 2020 and started to decrease later. These results are in line with the dynamics of the pandemic in Italy and the corresponding trend in restrictive measures. 2 , 3 , 4
The very high cancellation rates are not surprising because in agreement with Italian health‐care authorities' directives and with guidelines on patients prioritization issued by various expert groups and scientific societies during the COVID‐19 crisis.
Cancellations/postponements of all in‐office consultations, investigations, and treatments labeled as “elective” were recommended. 4 , 10 , 11 Functional urogynecological procedures were mostly considered elective and in the low/intermediate group of priority. 4 , 10 , 11 , 12 , 13 , 14 Although the term “elective” is open to various interpretations and deferment is rational when therapeutic alternatives with satisfactory outcomes are available, the extensive and often indiscriminate deprioritization of health‐care services for PFD patients likely turned on largely unknown implications for patients' physical and psychological health. 12 , 14 , 15 , 16 A substantial agreement emerged among respondents about the impact of the health‐care suspension on the quality of life of PFD patients. In this regard, further patient‐directed studies using validated patient‐reported tools are needed to assess the impact of this major disruption on patients' quality of life outcomes and clinical course of the different categories of PFD.
Although reporting high cancellation rates, 29.4% of respondents still reported unchanged or increased/much‐increased workload during the period covered by the survey. More frequent deployment to assist COVID‐19 patients, working in public/COVID facilities and hospitals with an emergency department may partly justify this apparent discrepancy.
Trends toward a progressive return to pre‐COVID activity have been noticed from May onwards. Based on these trends, we estimated a return to baseline activity for overall functional surgery in January 2021. The persistent cancellation/postponement of health‐care services for PFD in the postcrisis period can be explained by shortage of resources, persistent prioritization of urgent and oncological diseases, need for a reduced number of hospital visitors, and last but not least, patients' fear of visiting hospitals. 17 Of note, PFD patients are mostly over 60 years old (a vulnerable population for contracting COVID‐19) and often suffer from obesity, a risk factor for both PFD and worse outcomes with COVID‐19. 18 Neurologic patients are an even more challenging population due to their frailty and comorbidities. 19
No significant differences were observed in the degree of cutdown between macroareas across the various health‐care services. The early nation‐wide extension of strict governmental protective measures may have flattened possible regional differences.
Our results agree with those of other surveys investigating the impact of COVID‐19 on nonurgent health conditions. A global impact on the cutdown of urological services has been reported in a web‐based survey conducted by Teoh et al. 20 from March 30, 2020 to April 7, 2020. They observed that 83%, 87%, and 77% of uroflowmetries, urodynamics, and cystoscopies have been cancelled together with 93% and 85% of surgeries for BPH and female UI. In another online global survey among urologists, Dotzauer et al. 21 reported that surgeries with the highest cancellation rates were reconstruction surgery (87%) and surgery for BPH (84%). Another global expert‐response study by the COVIDSurg Collaborative has recently estimated global cancellations for benign surgery in urology and gynecology over a 12‐week period of the epidemic peak to be as high as 2,492,604 and 2,175,774, respectively (roughly 82% cancellation rate). 5
A rump‐up period due to the huge accumulated workload can be anticipated. For instance, based on the reported Italian volumes of activity, 22 we can estimate that 1637 procedures for female SUI will need to be recovered as a consequence of the first epidemic wave. The resumption time will depend on baseline volumes and resource availability. Furthermore, the protracted and changing pandemic situation and the likely scenario of COVID‐19 becoming endemic 23 may make it very challenging to resume deferred health‐care services. Based on our scenario‐based forecasting, it will take from 28 months to more than 5 years to completely recover the backload, without even considering other epidemic peaks. Published recommendations can assist in these difficult tasks for all health‐care providers dealing with PFD. 11 , 13 , 14 , 19 , 24 However, common sense, careful assessment, and case‐by‐case discussions should be used in patients' prioritization, decision‐making, and risk/benefit balance evaluation. 15 , 16 , 19 Transitioning to telemedicine will also be critical in the field of pelvic floor medicine. 24 Several conservative treatment modalities that showed the efficacy for PFD (e.g., behavioral therapy and pelvic floor muscle training) can be prescribed with a virtual consultation together with online instructions, home devices, telemonitoring systems, and digital technologies, such as electronic questionnaires and smartphone applications. 24 , 25
We acknowledge some limitations to this study. The survey methodology and the retrospective design have some inherent shortcomings due to self‐reported answers, recall bias, and nonresponse bias. Recall bias may involve both underestimation and overestimation of the cancellation rates, but its magnitude can reasonably be assumed to be small in consideration of the drastic and widespread cancellation of health‐care services for all deferrable conditions in the first 2 months (likely most affected by a recall bias) covered by our survey, according to the restrictions issued by the national government, leading to a quite homogeneous cutdown. Accordingly, standard deviations indicate a lower dispersion of reported cancellation rates in March–April compared with May–June. Furthermore, the survey lasted for 26 days, providing the respondents with the possibility to retrospectively assess the rates of cutdown in their institutions. We recognize a strong representation from Northern Italy (more heavily hit by the pandemic) and an underrepresentation of southern regions, involving nonresponse bias, potentially leading to an overestimation of cancellation rates. However, about two‐thirds of functional surgery for PFD is performed in the Northern Italian regions (e.g., 67% of SUI procedures 9 ); furthermore, weighing mean values by the reported baseline surgical volumes should have limited this bias. Facilities dealing with COVID‐19 patients and public‐hub hospitals were overrepresented; as a result, the responses may have reflected mostly these settings. Projected rates of cancellation were calculated under the assumptions of the linear model, without considering all the possible factors that may influence them, including future organizational changes in health‐care provision and unpredictable further pandemic waves (a second wave already started in September in Italy). The scenario‐based forecasting of backload recovery suffers from the same limitations. Furthermore, we assumed an early transition from the end of the down escalation phase to the recovery phase that will probably not be possible in many hospitals. As a result, an underestimation of projected recovery times must be considered.
Despite these shortcomings, our survey presents a perspective from an interdisciplinary group of experts specifically involved in the management of PFD that provided longitudinal real‐life, first‐hand data on the dramatic change in health‐care provision to PFD patients. Even though our projections involve various assumptions, our data provide a revealing forecast on the upcoming burden and recovery times in the surgical treatment of PFD that can inform both patients and physicians on the treatment delay they are going to face. Furthermore, our insight into the severe consequences of the indiscriminate cancellation policy adopted during the first COVID‐19 wave may help to guide the health‐care stakeholders' choices during subsequent waves.
5. CONCLUSIONS
PFD patients are among those who suffered most from the health‐care fallout of the COVID‐19 pandemic, with all respondent Italian experts reporting a drastic cutdown of both outpatient and inpatient clinical activities. A huge dip in health‐care services inevitably led to a wide disruption of regular access to care for PFD patients. We anticipate that the indirect effects of the pandemic on PFD management may last for several months. Clinical and epidemiological studies are needed to investigate the impact of this unprecedented health system disruption on patients' quality of life and the clinical course of PFD.
CONFLICT OF INTERESTS
Emilio Sacco: Pierrefabre (financial support for attending symposia and financial support for educational academic courses), Tegea (financial support for educational academic courses). Carlo Gandi: Pierrefabre (financial support for attending symposia), Lolipharma (financial support for attending symposia), Boston Scientific (financial support for attending symposia). Vincenzo Li Marzi: Ferring (speaker honorarium), IBSA (speaker honorarium). Enrico Finazzi Agro': Pierrefabre (speaker honorarium), Laborie (speaker and consultant honorarium), Recordati (speaker honorarium). Gianfranco Lamberti, Maurizio Serati, Marco Soligo: the remaining authors declare that there are no conflict of interests.
AUTHOR CONTRIBUTIONS
Conception and design, acquisition of data, data analysis and interpretation, statistical analysis, drafting of the manuscript: Emilio Sacco. Data analysis and interpretation, drafting of the manuscript, statistical analysis, drafting of the manuscript: Carlo Gandi. Conception, critical revision, and final approval of the manuscript: Vincenzo Li Marzi. Conception, critical revision, and final approval of the manuscript: Gianfranco Lamberti. Conception, critical revision, and final approval of the manuscript: Maurizio Serati. Conception, critical revision, and final approval of the manuscript: Enrico Finazzi Agrò. Conception and design, acquisition of data, drafting, critical revision, and final approval of the manuscript: Marco Soligo.
Supporting information
Supporting information.
Sacco E, Gandi C, Li Marzi V, et al. Extensive impact of COVID‐19 pandemic on pelvic floor dysfunctions care: A nationwide interdisciplinary survey. Neurourology and Urodynamics. 2021;40:695–704. 10.1002/nau.24610
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from SIUD (Società Italiana di Urodinamica). Restrictions apply to the availability of these data, which were used under license for this study. Data are available from the authors with the permission of SIUD.
REFERENCES
- 1. Boccia S, Cascini F, McKee M, Ricciardi W. How the Italian NHS is fighting against the COVID‐19 emergency. Front Public Health. 2020;8:167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Italian Ministry of Health. Nuovo coronavirus. 2020. http://www.salute.gov.it/nuovocoronavirus. Accessed August 19, 2020.
- 3. Naspro R, Da Pozzo LF. Urology in the time of corona. Nat Rev Urol. 2020;17(5):251‐253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Ficarra V, Novara G, Abrate A, et al. Urology practice during COVID‐19 pandemic. Minerva Urol Nefrol. 2020;72(3):369‐375. [DOI] [PubMed] [Google Scholar]
- 5. COVIDSurg Collaborative . Elective surgery cancellations due to the COVID‐19 pandemic: global predictive modelling to inform surgical recovery plans [published online ahead of print, May 12, 2020]. Br J Surg. 2020. 10.1002/bjs.11746 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Sacco E, Tienforti D, D'Addessi A, et al. Social, economic, and health utility considerations in the treatment of overactive bladder. Open Access J Urol. 2010;2:11‐24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Ugurlucan FG, Evruke I, Yasa C, Dural O, Yalcin O. Sexual functions and quality of life of women over 50 years with urinary incontinence, lower urinary tract symptoms and/or pelvic organ prolapse. Int J Impot Res. 2020;32(5):535‐543. [DOI] [PubMed] [Google Scholar]
- 8. Sacco E, D'Addessi A, Racioppi M, Pinto F, Totaro A, Bassi P. Bladder pain syndrome associated with highest impact on sexual function among women with lower urinary tract symptoms. Int J Gynaecol Obstet. 2012;117(2):168‐172. [DOI] [PubMed] [Google Scholar]
- 9. Italian Ministry of Health . 2020. http://www.salute.gov.it/portale/documentazione/p6_2_8_3_1.jsp?lingua=italiano%26id=33. Accessed August 19, 2020.
- 10. Stensland KD, Morgan TM, Moinzadeh A, et al. Considerations in the triage of urologic surgeries during the COVID‐19 pandemic. Eur Urol. 2020;77(6):663‐666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Ribal MJ, Cornford P, Briganti A, et al. European Association of Urology Guidelines Office Rapid Reaction Group: an organisation‐wide collaborative effort to adapt the European association of urology guidelines recommendations to the coronavirus disease 2019 era. Eur Urol. 2020;78(1):21‐28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. American College of Surgeons . COVID‐19: guidance for triage of non‐emergent surgical procedures. 2020. https://www.facs.org/covid-19/clinical-guidance/electivesurgery. Accessed September 5, 2020.
- 13. López‐Fando L, Bueno P, Carracedo D, et al. Management of female and functional urology patients during the COVID pandemic. Eur Urol Focus. 2020;6(5):1049‐1057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Thakar R, Robinson D, Rantell A, Ness W, Seleme M, Berghmans B. Guidance for the management of urogynecological conditions during the Coronavirus (COVID‐19) pandemic. IUGA; 2020. https://www.iuga.org/publications/covid-19-guidance-for-urogynecological-conditions. Accessed October 14, 2020.
- 15. Finazzi Agrò E, Farullo G, Balzarro M, et al. Triage of functional, female and neuro‐urology patients during and immediately after the Covid‐19 outbreak. Minerva Urol Nefrol. 2020;72(4):513‐515. [DOI] [PubMed] [Google Scholar]
- 16. Phé V, Karsenty G, Robert G, Gamé X, Cornu JN. Widespread postponement of functional urology cases during the COVID‐19 pandemic: rationale, potential pitfalls, and future consequences. Eur Urol. 2020;78(1):4‐5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Ficarra V, Mucciardi G, Giannarini G. Re: Riccardo Campi, Daniele Amparore, Umberto Capitanio, et al. Assessing the burden of nondeferrable major uro‐oncologic surgery to guide prioritisation strategies during the COVID‐19 pandemic: insights from three Italian high‐volume referral centres. Eur Urol. 2020;78:11‐15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Banerjee M, Gupta S, Sharma P, Shekhawat J, Gauba K. Obesity and COVID‐19: a fatal alliance. Indian J Clin Biochem. 2020;35(4):1‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Musco S, Del Popolo G, Lamartina M, et al. Neuro‐Urology during the COVID‐19 pandemic: triage and priority of treatments. Neurourol Urodyn. 2020;39(7):2011‐2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Teoh JYC, Ong WLK, Gonzalez‐Padilla D, et al. A global survey on the impact of COVID‐19 on urological services. Eur Urol. 2020;78(2):265‐275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Dotzauer R, Böhm K, Brandt MP, et al. Global change of surgical and oncological clinical practice in urology during early COVID‐19 pandemic [published online ahead of print July 4, 2020]. World J Urol. 10.1007/s00345-020-03333-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Italian Ministry of Health. 2017. http://www.salute.gov.it/imgs/C_17_ReportDispositivi_5_documentoInglese_inglese_itemName_0_documentoENG.pdf. Accessed October 14, 2020.
- 23. Ghai S. Will the guidelines and recommendations for surgery during COVID‐19 pandemic still be valid if it becomes endemic? Int J Surg. 2020;79:250‐251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Grimes CL, Balk EM, Crisp CC, et al. A guide for urogynecologic patient care utilizing telemedicine during the COVID‐19 pandemic: review of existing evidence. Int Urogynecol J. 2020;31(6):1063‐1089.32342112 [Google Scholar]
- 25. Soligo M, Nelva Stellio L, De Ponti E, et al. Italian electronic personal assessment questionnaire‐pelvic floor (I.ePAQ‐PF): psychometric validation of the urinary section [online ahead of print, August 4, 2020]. Neurourol Urodyn. 2020;39:2192‐2197. 10.1002/nau.24472 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supporting information.
Data Availability Statement
The data that support the findings of this study are available from SIUD (Società Italiana di Urodinamica). Restrictions apply to the availability of these data, which were used under license for this study. Data are available from the authors with the permission of SIUD.


