Abstract
Background
Exposure to COVID‐19 is more likely among certain occupations compared with others. This descriptive study seeks to explore occupational differences in mortality due to COVID‐19 among workers in Massachusetts.
Methods
Death certificates of those who died from COVID‐19 in Massachusetts between March 1 and July 31, 2020 were collected. Occupational information was coded and age‐adjusted mortality rates were calculated according to occupation.
Results
There were 555 deaths among MA residents of age 16–64, with usable occupation information, resulting in an age‐adjusted mortality rate of 16.4 per 100,000 workers. Workers in 11 occupational groups including healthcare support and transportation and material moving had mortality rates higher than that for workers overall. Hispanic and Black workers had age‐adjusted mortality rates more than four times higher than that for White workers overall and also had higher rates than Whites within high‐risk occupation groups.
Conclusion
Efforts should be made to protect workers in high‐risk occupations identified in this report from COVID‐19 exposure.
Keywords: Covid‐19, mortality, occupation
1. INTRODUCTION
The workplace is likely an important venue for COVID‐19 transmission. Different occupations face different risks for COVID‐19 exposure due to the nature of the work performed. 1 These occupational exposures may be contributing to geographic, racial, and ethnic disparities in COVID‐19 cases and deaths. 2 , 3 , 4 Previous research from the United Kingdom found that men in elementary occupations and women in caring and leisure occupations had significantly elevated mortality rates due to COVID‐19 compared with all other workers. 5 In Sweden it was found that taxi and bus drivers had elevated mortality rates from COVID‐19 compared with other workers 6 The objective of this study was to describe differences among occupations in mortality due to COVID‐19 in the Massachusetts workforce as well as how occupational differences varied by race and ethnicity.
2. METHODS
Death certificate data for all deaths occurring in MA between March 1 and July 31, 2020 were obtained from the MA Registry of Vital Records and Statistics. COVID‐19 deaths were identified using ICD‐10 code U07.1. Additional COVID‐19 deaths (<1%) were identified by reviewing free‐text descriptions on the death certificates. The study population was MA residents age 16–64 who were in the civilian workforce and who died of COVID‐19. Information about usual occupation on death certificates was coded into 22 US Census major occupation groups using the National Institute for Occupational Safety and Health (NIOSH) Industry and Occupation Computerized Coding System (NIOCCS). 7 American Community Survey (ACS) Public Use Micro Data Set Data for 2018 was used to generate denominator data for the civilian MA workforce according to occupation, age, sex, and, race/ethnicity. These denominator data are shown in Table S1.
Age‐adjusted mortality rates were calculated by occupation, sex, and race/ethnicity using SAS (Version 9.3; SAS Institute). Age‐standardization was performed using the COVID‐19 mortality for all workers according to five age groups (16–24, 25–34, 35–44, 45–54, 55–64).
There were 737 deaths due to COVID‐19 among Massachusetts residents 16–64 years old between March 1 and July 31, 2020. One hundred and twenty‐two deaths were excluded because the death certificate indicated that the decedent was not working/retired (n = 69), a homemaker (48), a student, 4 or in the military. 1 An additional 60 deaths were excluded because of insufficient occupation information, resulting in 555 COVID‐19 deaths.
3. RESULTS
There were a total of 555 deaths identified among MA workers aged 16–64 due to COVID‐19 between March 1 and July 31, 2020. The overall mortality rate for this population was 16.4 deaths/100,000 workers during the 5‐month study period. As shown in Figure 1, deaths increased rapidly in April and May and then declined in June and July. Workers in 11 major occupation groups had age‐adjusted mortality rates higher than the rates for all workers: healthcare support; transportation and material moving; food preparation and serving; building and grounds cleaning and maintenance; production; construction and extraction; installation, maintenance, and repair; protective service; personal care and service; arts, design, entertainment, sports, and media; and community and social service (Figure 2).
Figure 1.
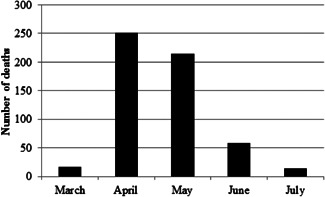
Number of COVID‐19 deaths among workers of age 18–64 by month; Massachusetts, March 1–July 31, 2020
Figure 2.
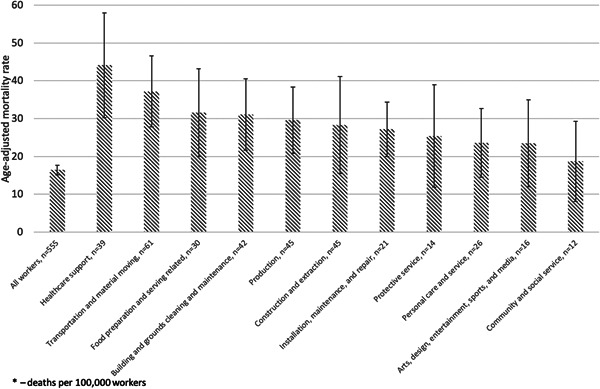
Age‐adjusted COVID‐19 mortality rates among workers of age 18–64 by occupation groups with elevated rates; Massachusetts, March 1–July 31, 2020
Hispanic and Black workers had mortality rates more than four times higher than that for White workers (53.4 and 50.4, respectively vs. 10.7/100,000). In almost all instances when sufficient data by race/ethnicity were available, Hispanic and Black workers had higher mortality rates than White workers in the same occupation group. Within the occupation groups with the five highest rates, Hispanic and Black workers had substantially higher rates than White workers in the same occupation group. For example, Hispanic food preparation and serving workers had a rate eight times that of White food preparation and serving workers. Black healthcare support workers had a rate nearly three times higher than that of White healthcare support workers. White workers in high‐risk occupation groups still had elevated rates compared with White workers overall. For example, the rate of White healthcare support workers was more than double that of all White workers (Table 1).
Table 1.
COVID‐19 deaths and age‐adjusted mortality ratesa among workers according to occupation group, age, and sex by race/ethnicity, Massachusetts, March 1–July 31, 2020
| All workersb | White, non‐Hispanic workers | Hispanic workers | Black, non‐Hispanic workers | Asian, non‐Hispanic | Other | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n (%) | Age‐adjusted mortality rate (95% CI)c | n (%) | Age‐adjusted mortality rate (95% CI)c | n (%) | Age‐adjusted mortality rate (95% CI)c | n (%) | Age‐adjusted mortality rate (95% CI)c | n (%) | Age‐adjusted mortality rate (95% CI)c | n (%) | Age‐adjusted mortality rate (95% CI)c | |
| Occupation group | ||||||||||||
| Healthcare support | 39 (7.0) | 44.1 (30.3, 58.0) | 13 (4.4) | 27.1 (12.4, 41.8) | 5 (4.1) | 51.3 (5.6, 97.0) | 18 (17.8) | 75.0 (40.3, 109.7) | d | d | d | d |
| Transportation and material moving | 61 (11.0) | 37.2 (27.8, 46.5) | 26 (8.8) | 22.7 (13.9, 31.4) | 17 (14.0) | 57.4 (29.9, 84.9) | 10 (9.9) | 62.6 (23.6, 101.6) | d | d | d | d |
| Food preparation and serving related | 30 (5.4) | 31.6 (20.0, 43.3) | 9 (3.1) | 15.1 (5.2, 25.0) | 13 (10.7) | 125.5 (40.9, 210.1) | d | d | d | d | d | d |
| Building and grounds cleaning and maintenance | 42 (7.6) | 31.1 (21.7, 40.6) | 16 (5.4) | 19.4 (9.8, 29.0) | 22 (18.2) | 65.6 (38.1, 93.1) | d | d | 0 (0.0) | 0.0 | d | d |
| Production | 45 (8.1) | 29.6 (20.8, 38.3) | 22 (7.5) | 19.7 (11.5, 28.0) | 14 (11.6) | 76.4 (33.4, 119.5) | 8 (7.9) | 99.4 (29.5, 169.3) | d | d | d | d |
| Installation, maintenance, and repair | 21 (3.8) | 27.2 (15.5, 38.9) | 13 (4.4) | 18.7 (8.5, 28.9) | d | d | d | d | d | d | 0 (0.0) | 0.0 |
| Construction and extraction | 45 (8.1) | 28.3 (20.0, 36.5) | 25 (8.5) | 17.2 (10.4, 23.9) | 15 (12.4) | 362.1 (152.3, 571.9) | d | d | 0 (0.0) | 0.0 | d | d |
| Protective service | 14 (2.5) | 25.4 (11.9, 38.9) | 6 (2.0) | 15. 9 (3.0, 28.7) | d | d | d | d | 0 (0.0) | 0.0 | d | d |
| Personal care and service | 26 (4.7) | 23.6 (14.5, 32.7) | 13 (4.4) | 18.1 (8.3, 28.0) | 5 (4.1) | 32.6 (3.8, 61.4) | 6 (5.9) | 69.0 (9.7, 128.3) | d | d | d | d |
| Arts, design, entertainment, sports, and media | 16 (2.9) | 23.5 (12.0, 35.1) | 12 (4.1) | 18.7 (8.1, 29.3) | d | d | d | d | 0 (0.0) | 0.0 | d | d |
| Community and social service | 12 (2.2) | 18.7 (8.1, 29.3) | d | d | d | d | 6 (5.9) | 75.6 (15.0, 136.2) | 0 (0.0) | 0.0 | 0 (0.0) | 0.0 |
| Life, physical, and social science | 7 (1.3) | 14.3 (3.6, 25.0) | d | d | 0 (0.0) | 0.0 | d | d | d | d | 0 (0.0) | 0.0 |
| Sales and related | 40 (7.2) | 13.9 (9.6, 18.2) | 30 (10.2) | 11.5 (7.4, 15.7) | 6 (5.0) | 48.8 (6.4, 91.2) | d | d | d | d | 0 (0.0) | 0.0 |
| Healthcare practitioners and technical | 30 (5.4) | 11.2 (7.2, 15.2) | 17 (5.8) | 7.5 (3.9, 11.1) | 0 (0.0) | 0.0 | 18 (17.8) | 57.5 (23.5, 91.5) | d | d | d | d |
| Architecture and engineering | 12 (2.2) | 13.7 (5.9, 21.4) | 9 (3.1) | 11.7 (4.0, 19.5) | d | d | d | d | 0 (0.0) | 0.0 | d | d |
| Office and administrative support | 47 (8.5) | 11.8 (8.5, 15.2) | 31 (10.5) | 8.9 (5.8, 12.0) | 7 (5.8) | 22.8 (5.1, 94.3) | 7 (6.9) | 34.0 (8.8, 59.2) | d | d | d | d |
| Business and financial operations | 17 (3.1) | 8.7 (4.6, 12.8) | 9 (3.1) | 5.4 (1.9, 8.9) | d | d | d | d | 0 (0.0) | 0.0 | d | d |
| Legal | 4 (0.7) | 8.2 (0.2, 16.3) | d | d | 0 (0.0) | 0.0 | 0 (0.0) | 0.0 | 0 (0.0) | 0.0 | 0 (0.0) | 0.0 |
| Computer and mathematical | 7 (1.3) | 5.7 (1.5, 10.0) | 6 (2.0) | 5.8 (1.2, 10.5) | 0 (0.0) | 0.0 | 0 (0.0) | 0.0 | d | d | 0 (0.0) | d |
| Management | 28 (5.0) | 5.4 (3.4, 7.4) | 17 (5.8) | 3.8 (2.0, 5.6) | d | d | 6 (5.9) | 26.3 (5.0, 47.6) | d | d | d | d |
| Education, training, and library | 10 (1.8) | 4.3 (1.6, 6.9) | 9 (3.1) | 4.6 (1.6, 7.6) | d | d | d | d | d | d | d | d |
| Age groupsb | ||||||||||||
| 16–34e | 13 (2.3) | 1.0 (0.7, 1.3) | d | d | 8 (6.6) | 4.4 (2.8, 6.0) | d | d | d | d | d | d |
| 35–44 | 27 (4.9) | 3.8 (3.1, 4.6) | d | d | 9 (7.4) | 9.9 (6.6, 13.1) | d | d | d | d | d | d |
| 45–54 | 113 (20.4) | 15.1 (13.7, 16.6) | 41 (13.9) | 7.3 (6.2, 8.4) | 37 (30.6) | 52.6 (44.0, 61.3) | 24 (23.8) | 51.3 (40.9, 61.8) | 6 (31.6) | 12.0 (7.1, 16.9) | 5 (26.3) | 28.6 (15.8, 41.4) |
| 55–64 | 402 (72.4) | 61.6 (58.5, 64.7) | 243 (82.4) | 44.7 (41.9, 47.6) | 67 (55.4) | 197.4 (173.3, 221.6) | 70 (69.3) | 188.7 (166.2, 211.3) | 10 (52.6) | 34.1 (23.3, 44.8) | 12 (63.2) | 134.7 (95.8, 173.6) |
| Sex | ||||||||||||
| Male | 366 (65.9) | 21.4 (19.2, 23.6) | 186 (63.1) | 13.3 (15.1, 17.8) | 91 (75.2) | 79.1 (62.0, 96.3) | 62 (61.4) | 67.7 (50.7, 84.7) | 13 (68.4) | 13.4 (6.0, 20.9) | 14 (73.7) | 57.8 (26.6, 89.9) |
| Female | 189 (34.1) | 11.3 (9.7, 12.9) | 109 (36.9) | 8.1 (6.5, 9.6) | 30 (24.8) | 28.0 (17.6, 38.4) | 39 (38.6) | 36.0 (24.7, 47.3) | 6 (31.6) | 6.2 (1.0, 11.4) | 5 (26.3) | 7.3 (1.9, 30.5) |
| All workersb | 555 (100.0) | 16.4 (15.1, 17.8) | 295 | 10.7 (9.5, 12.0) | 121 (21.8) | 53.4 (43.4, 63.4) | 101 (18.2) | 50.4 (40.5, 60.2) | 19 (3.4) | 10.2 (5.5, 14.9) | 19 (3.4) | 34.1 (18.2, 50.0) |
Deaths per 100,000 workers.
Total for categories do not sum to total for all workers due to some categories not being shown because of cell size suppression rules.
For age groups, rates are age‐stratum‐specific rates.
Excluded due to cell size suppression rules.
The 16–24 and 25–34 age groups are combined due to cell size suppression rules. For age‐standardization, these two age groups were separated.
This article is being made freely available through PubMed Central as part of the COVID-19 public health emergency response. It can be used for unrestricted research re-use and analysis in any form or by any means with acknowledgement of the original source, for the duration of the public health emergency.
4. DISCUSSION
Among a working‐age population, there were wide disparities in mortality due to COVID‐19 according to occupation. Occupation groups that would be expected to have frequent contact with ill people or close contact with the public, and jobs where working from home is impractical had particularly elevated mortality rates. Additionally, we identified Hispanic and Black workers as having mortality rates four times higher than that of White workers. Even within many high‐risk occupation groups these elevated mortality rates persisted.
Exposure to COVID‐19 varies by occupation and this is likely to be an important contributor to the differences observed in this study. 1 Many of the occupations with elevated mortality rates are essential services or jobs which cannot be performed from home. 8 , 9 Workers in some of these occupations may also be at increased risk of death if infected because they have less access to healthcare. A previous study examined the percentage of workers that did not have insurance according to occupation. Of the 11 occupation groups with elevated mortality rates in this study, 7 had higher a higher percentage of workers without insurance compared with the average for all workers. 10 Workers in high‐risk occupations may also be more likely to have underlying comorbidities that increase the risk of dying of COVID‐19. 11
Healthcare support workers were identified as having the highest age‐adjusted mortality rates in this study. This finding likely reflects the nature of the work being performed by healthcare support workers where exposure to infected patients would be common. However, among healthcare practitioners, mortality rates were not elevated. This finding may be due to the fact that healthcare practitioners likely have more of an ability to work from home compared with healthcare support workers. 12
These findings also suggest that occupational exposures may be an important contributing factor to well‐documented racial and ethnic disparities in COVID‐19 deaths. Some of these disparities may be due to Black and Hispanic workers being more likely to work in occupations with higher exposure to the coronavirus and in essential industries. 2 This may be true even within the same broad occupational groups. For example, while both Black and White workers in transportation and material moving occupations had high age‐adjusted mortality rates; the rate for Black workers was nearly three times that for Whites. At the same time, occupational exposures may also exacerbate other structural inequalities faced by workers of color in terms of poverty and access to health care.
Male workers had nearly twice the mortality rate for COVID‐19 as female workers. This difference was particularly stark for Hispanic, Black, and workers of other races and ethnicities. Although this finding of a higher risk of mortality among males compared with females is broadly consistent with previous research about differences in the risk of mortality due to COVID‐19 by age and sex, 13 , 14 reasons for these differences deserve particular attention. Additionally, the scale of the differences seems to be greater than in other studies that did not deal solely with working populations. Some of the differences identified here may be due to employment in higher‐risk occupations. Due to the relatively small sample size analyzed here, the relationship between sex and occupation could not be further explored.
Deaths were highest in April and May, the peak of the first pandemic surge in MA. Some of the deaths that occurred in April and May could be attributable to occupational exposures that occurred before the mid‐March lockdown in MA and implementation of exposure controls because of the delay between initial exposure and death. The decline in later months likely reflects a combination of multiple factors including fewer workers—even those in essential jobs—actually going to the workplace in Phase 2 of the pandemic, 15 improved treatment for severe COVID cases, 16 and the effectiveness of both community‐wide and workplace‐specific interventions, in decreasing the risk of exposure to COVID‐19 in MA workplaces. The latter includes increased access to personal protective equipment (PPE) and new requirements for employers to implement infection prevention and control measures in the workplace. 17
Assessing the work‐relatedness of COVID‐19 cases and deaths for surveillance purposes is a challenge. The Council of State and Territorial Epidemiologists (CSTE) has proposed a surveillance case definition for work‐related COVID, to promote a standard approach to classifying cases for purposes of population‐based surveillance. The definition considers work‐related transmission to be likely when (a) the worker was present in the workplace during the 14 days before disease onset and (b) the case was identified as part of a workplace cluster or as having had close contact with a co‐worker, patient, or resident classified as confirmed or probable case. For healthcare workers and those in public‐facing jobs, as defined by O*NET, work‐related transmission is also considered likely when the case has had no known contact with a confirmed or probable case of COVID‐19 outside of the workplace. 18
This study has some limitations. Conclusions about the causal role of occupational factors in explaining differences in mortality rates cannot be firmly established from the findings of this study alone. For example, different comorbidities among workers in different occupations could explain some of the differences in mortality. 11 Unfortunately, because we lacked data about comorbidities among the decedents or other potential confounders; we could not perform the multivariate analysis necessary to explore other potential explanations for the differences observed here.
Although we sought to include only decedents who were presumed to be working at or close to the time of death, we cannot be certain that this is the case because death certificates only provide information about usual, and not current, occupation. For the same reason, we cannot be certain that if the decedent was working at the time of death that they were working in the occupation listed on their death certificate.
Additionally, the denominator used to calculate rates was employment in 2018. It is likely that employment patterns in 2020 were different than in 2018, especially given the large changes in employment due to the pandemic. Differential access to testing may result in some misclassification, for example, workers in some occupations may have been less likely to be tested, which could have resulted in underestimates of mortality identified as due to COVID‐19. However, this may not have much of an impact on the findings because COVID‐19 can be coded as a cause of death without a positive test. 19 However, it has been suggested that lower availability of testing among people of color may lead to underestimates of disparities in the burden of COVID‐19. 20
Interpretations of differences, especially those between racial and ethnic groups should be made with caution because of small sample sizes. This caution is especially true when findings are stratified by both race/ethnicity and occupation.
According to MA official death data, there were 1341 deaths among those of ages 0–69 through July 31, 2020. 21 Assuming about half of the deaths in the 60–69 group were those 60–64, this works out to be 898 deaths for those 16–64 which is higher than our total of 737 deaths among those 16–64. This difference may be due to a lower risk of deaths in the 60–64 group (meaning less than half of the deaths among those 60–69 occurred among those 60–64). Additionally, there may have been incomplete reporting of COVID‐19 deaths in the death certificates analyzed here.
Even with these limitations, the role that work plays in the transmission of COVID‐19 deserves further attention. This study addressed only mortality risk, but many more workers are contracting COVID‐19 at work, becoming sick, and dealing with the long‐term impacts of the disease. Employers have a responsibility to protect workers from known occupational hazards. Workplace initiatives should both seek to prevent the transmission of the virus in the workplace and support workers who become sick. Prevention should involve implementation and enforcement of comprehensive workplace COVID control programs including the use of masks and PPE, social distancing, adequate ventilation, cleaning and disinfection, worker training, and policies assuring that sick workers get adequate care, time off, and sick pay. Previous research has suggested that workers with decreased access to adequate PPE may be at a higher risk for contracting COVID‐19. Some of this decreased access may contribute to racial and ethnic differences in the risk for COVID‐19 infection. 22 The findings from this study identify occupations where these efforts are particularly urgent. Efforts to control the spread of COVID‐19 in the workplace can both help to protect all workers and reduce health disparities.
CONFLICTS OF INTEREST
The authors declare that there are no conflicts of interest.
DISCLOSURE BY AJIM EDITOR OF RECORD
John D. Meyer declares that he has no conflict of interest in the review and publication decision regarding this article.
AUTHOR CONTRIBUTIONS
Devan Hawkins conceived the study, acquired data, performed initial analysis, and drafted the paper. Letitia Davis and David Kriebel suggested further analyses, produced tables and figures, and revised the manuscript. All authors approve this version of the manuscript and agree to be accountable for all aspects of the work.
PEER REVIEW
The peer review history for this article is available at https://publons.com/publon/10.1002/ajim.23227.
ETHICS APPROVAL AND INFORMED CONSENT
This project was considered exempt from review by the MCPHS University Institutional Review Board, because it was conducted with previously collected, deidentified data.
Supporting information
Supporting information.
Hawkins D, Davis L, Kriebel D. COVID‐19 deaths by occupation, Massachusetts, March 1–July 31, 2020. Am J Ind Med. 2021;64:238–244. 10.1002/ajim.23227
[Correction added after first publication on 25 January 2021: The co‐author Letitia Davis's affiliation was revised.]
DATA AVAILABILITY STATEMENT
The data in this report are publicly available data. It can be obtained by making a public data request to the Massachusetts Registry of Vital Records and Statistics.
REFERENCES
- 1. Baker MG, Peckham TK, Seixas NS. Estimating the burden of United States workers exposed to infection or disease: a key factor in containing risk of COVID‐19 infection. PLOS One. 2020;15(4):e0232452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Hawkins D. Differential occupational risk for COVID‐19 and other infection exposure according to race and ethnicity. Am J Ind Med. 2020;63(9):817‐820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. McLaren J. Racial Disparity in COVID‐19 Deaths: Seeking Economic Roots with Census data. National Bureau of Economic Research; 2020. [Google Scholar]
- 4. Hawkins D. Social determinants of COVID‐19 in Massachusetts, United States: an ecological study. J Prev Med Public Health. 2020;53(4):220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Office for National Statistics . Coronavirus (COVID‐19) Related Deaths by Occupation, England and Wales: Deaths Registered up to and Including 20 April 2020. UK: ONS; 2020. [Google Scholar]
- 6. Billingsley S, Brandén M, Aradhya S, Drefahl S, Andersson G, Mussino E. Deaths in the frontline: Occupation‐specific COVID‐19 mortality risks in Sweden; 2020. https://su.figshare.com/articles/preprint/Deaths_in_the_frontline_Occupation-specific_COVID19_mortality_risks_in_Sweden/12816065/2
- 7. NIOSH . NIOSH Industry and Occupation Computerized Coding System (NIOCCS). U.S. Department of Health and Human Services, Public Health Service, Centers for Disease Control and Prevention, National Institute for Occupational Safety and Health, Division of Surveillance, Hazard Evaluation and Field Studies, Surveillance Branch; 2018. https://www.cdc.gov/niosh/topics/coding/overview.html. Accessed September 8, 2020.
- 8. Van Drie H, Reeves RV. Many essential workers are in “low‐prestige” jobs. Time to change our attitudes—and policies? [Internet]; 2020. Brookings. https://www.brookings.edu/blog/up-front/2020/05/28/many-essential-workers-are-in-low-prestige-jobs-time-to-change-our-attitudes-and-policies/. Accessed January 10, 2021.
- 9. Baker MG. Nonrelocatable occupations at increased risk during pandemics: United States, 2018. Am J Public Health. 2020;1108:1126‐1132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Boal WL, Li J, Sussell A. Health insurance coverage by occupation among adults aged 18–64 years—17 States, 2013–2014. MMWR Morb Mortal Wkly Rep. 2018;67(21):593‐598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Silver SR, Li J, Boal WL, Shockey TL, Groenewold MR. Prevalence of underlying medical conditions among selected essential critical infrastructure workers—behavioral risk factor surveillance system, 31 states, 2017–2018. MMWR Morb Mortal Wkly Rep. 2020;69(36):1244‐1249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Allard MD, Lacey J. Work‐at‐Home Patterns by Occupation. US Department of Labor, US Bureau of Labor Statistics; 2009. [Google Scholar]
- 13. Bhopal SS, Bhopal R. Sex differential in COVID‐19 mortality varies markedly by age. Lancet (London, England). 2020;396:532‐533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Pradhan A, Olsson PE. Sex differences in severity and mortality from COVID‐19: are males more vulnerable? Biol Sex Differ. 2020;11(1):1‐11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Brynjolfsson E, Horton JJ, Ozimek A, Rock D, Sharma G, TuYe HY. COVID‐19 and Remote Work: An Early Look at US Data. National Bureau of Economic Research; 2020. No. w27344. [Google Scholar]
- 16. Horwitz L, Jones SA, Cerfolio RJ, et al. Trends in Covid‐19 risk‐adjusted mortality rates in a single health system. medRxiv. 2020. https://www.medrxiv.org/content/medrxiv/early/2020/08/14/2020.08.11.20172775.full.pdf [DOI] [PubMed] [Google Scholar]
- 17. Office of the Attorney General . Workplace Health and Safety During COVID‐19: A Resource Guide for Employees; 2020. https://www.mass.gov/info-details/workplace-health-and-safety-during-covid-19-a-resource-guide-for-employees. Accessed November 18, 2020.
- 18. Council of State and Territorial Epidemiologists . Interim 20‐ID‐02: update to the standardized surveillance case definition and national notification for 2019 novel coronavirus disease (COVID‐19) [position statement]. Atlanta, GA: Council of State and Territorial Epidemiologists; 2020.
- 19. Centers for Disease Control and Prevention, & National Center for Health Statistics . Guidance for Certifying Deaths due to Coronavirus Disease 2019 (COVID19). 2020; No. 3: 2020‐1126.
- 20. Lieberman‐Cribbin W, Tuminello S, Flores RM, Taioli E. Disparities in COVID‐19 testing and positivity in New York City. Am J Prev Med. 2020;59(3):326‐332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Massachusetts Department of Public Health . Massachusetts Department of Public Health COVID‐19 Dashboard—Dashboard of Public Health Indicators; 2020. https://www.mass.gov/doc/covid-19-dashboard-july-31-2020/download. Accessed December 15, 2020.
- 22. Nguyen LH, Drew DA, Graham MS, et al. Risk of COVID‐19 among front‐line health‐care workers and the general community: a prospective cohort study. Lancet Public Health. 2020;5(9):e475‐e483. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supporting information.
Data Availability Statement
The data in this report are publicly available data. It can be obtained by making a public data request to the Massachusetts Registry of Vital Records and Statistics.


