Abstract
The COVID‐19 pandemic poses novel health issues. However, the benefits and costs of the pandemic and policies to address it have a familiar economic structure. Chief among the health‐related benefits are the monetized values of the U.S. mortality costs of $3.9 trillion in 2020. The combined U.S. mortality and morbidity costs are $5.5–5.9 trillion. Global mortality costs in 2020 total $10.1 trillion. The skewed age distribution of COVID‐19 illnesses has stimulated increased advocacy of downward adjustments in the value of a statistical life (VSL) for older people. This article examines the role of age for policy analysis generally and for the rationing of scarce medical treatments, such as ventilators. Mortality risk reduction benefits should be based on the reduced probability of death multiplied by the pertinent VSL. Effective communication of risks to foster precautions hinges on the credibility of the information source, which public officials have jeopardized. Efficient control of risks imposes limits on personal freedoms to foster health improvements.
Keywords: coronavirus, COVID‐19, morbidity, mortality, value of a statistical life
1. INTRODUCTION

W. Kip Viscusi University Distinguished Professor of Law, Economics, and Management, Vanderbilt Law School, Nashville TN
COVID‐19 is a novel coronavirus. Nevertheless, the policy issues raised by this pandemic are not entirely novel but are well situated in economists' domain. The fundamental policy task is to think about this pandemic in a sensible way. How should we deal with the health risks posed by the pandemic? Is it feasible to monetize the health consequences of these risks? The economic and societal ramifications of dealing with these risks are not costless and have generated starkly divergent viewpoints. Should health concerns always be paramount and be the sole driver of policy decisions? Or should health consequences be disregarded, treating the pandemic as a hoax or, at most, as being comparable to routine flu illnesses? More rationally, how can we seek to achieve a meaningful, efficient balance between the health risks and the costs to reduce them? This article provides guidance for addressing COVID‐19 as well as lessons that are applicable to future pandemics. The advent of a major novel health crisis need not paralyze analysis or lead us to abandon the guiding principle of fostering economically efficient control of risks.
Government agencies have routinely confronted sensitive issues involving life and health for decades, particularly with respect to the design and structure of health, safety, and environmental regulations. Economic analyses in these domains are sometimes challenging and necessarily involve treading on controversial terrain. Yet, the presence of such challenges has not led policymakers to abandon the pursuit of efforts to strike a meaningful balance between risk and costs. My book, Pricing Lives: Guideposts for a Safer Society, presents economic prescriptions for analyzing these risk situations, some of which I will draw upon and extend for my analysis here.
Although the application of existing economic frameworks to COVID‐19 is instructive, this pandemic has some distinctive aspects that may require more than off‐the‐shelf analyses. Section 2 considers the mortality and morbidity consequences of the pandemic. The magnitude of the threats to health is greater than that posed in the typical regulatory context, with U.S. mortality costs in 2020 of almost $4 trillion. The impacts also are global, necessitating the valuation of health risks for countries for which quite different benefit measures are pertinent. Morbidity costs incurred by those who do not die also are substantial. Within‐country heterogeneity of the value of reducing mortality risks has emerged as a prominent concern. Treating all lives within a country as having the same value is a useful starting point, but the incidence of COVID‐19 impacts is highly skewed, with the greatest losses being experienced at the upper end of the age distribution. Section 3 explores these age‐related issues both with respect to monetization of mortality risk reductions and the rationing of scarce medical treatments, which involves ethical challenges far greater than in the usual regulatory contexts where the changes in risk probabilities are small. Because many COVID‐19 policies rely on decentralized personal decisions, it is essential to be able to effectively communicate the risks and the pertinent precautions. Section 4 outlines some key economic guidelines for effective risk communication, which is an area where U.S. policy efforts have fallen particularly short. Appropriate protective measures by the public require that they make tradeoffs involving some sacrifice of personal freedoms. Many may view personal freedoms as absolute rights that should never be compromised. An opposing point of view is that individual lives are sacred and should never be put at greater risk. Confronting the inevitable tradeoff between freedom and health in a meaningful way is the focus of Section 5. Throughout the discussion, the recurring theme is that while this pandemic poses enormous challenges, a more rational policy response requires that we apply and, in some cases, extend existing economic frameworks. Section 6 concludes, offering an estimate that the U.S. mortality cost will reach $5.5 trillion once the death toll is 500,000 by March 2021.
2. MORTALITY AND MORBIDITY EFFECTS
2.1. The mortality costs in the United States
The mortality costs of COVID‐19 have increased since the onset of the pandemic, have not begun to stabilize, and remain a moving target. For purposes of my presentation at the Southern Economic Association conference, I used the mortality totals as of September 26, 2020, for my analysis. At that time, there had been 209,177 U.S. deaths. By January 1, 2021, this total had risen by 70% to 355,631 deaths. Here I will use the mortality figures on January 1, 2021, for my analysis, thus focusing on the health loss in 2020.1
To calculate the value of the mortality costs, I apply my labor market estimates of the value of a statistical life (VSL). The VSL is the local rate of the tradeoff between money and small risks of death. Empirical estimates of the VSL using labor market data correspond to the estimated wage‐risk tradeoff rate. After appropriate updates for inflation, the focal VSL estimate that I report in Viscusi (2018) is $11 million. This value is the estimate based on labor market studies in which workers are matched to measures of job risks using the most reliable and refined fatality rate data, the U.S. Bureau of Labor Statistics Census of Fatal Occupational Injuries. The $11 million figure also incorporates adjustments for potential publication selection effects that may influence which estimates are submitted for publication and are published in the literature. If there is no adjustment for publication selection effects, the VSL would be about $2 million higher. Although government agencies have long had a history of undervaluing risks to life, policy analysis practices are now better aligned with estimates in the economics literature. In recent years, U.S. government agencies have used VSL estimates in the $9 million to $11 million range. Multiplying the number of deaths by a VSL figure of $11 million yields a mortality cost estimate through September 26, 2020, of $2.3 trillion. By the end of the year, the mortality cost had risen to $3.9 trillion.2
While the application of a uniform VSL to all mortality risks is consistent with prevailing government practices, it is also feasible to incorporate potential sources of heterogeneity. The VSL is not a natural constant but reflects individual preferences with respect to bearing risk. The possible refinements in the applicable VSL include adjustments for age, income, the size of the risk change, and the direction of the risk change. The subsequent discussion focuses on the principal modifications for age and income.
This article sets aside adjustments based on the magnitude of the risk changes involved. Policies that involve large risk changes have a lower associated willingness‐to‐pay value for risk reductions, such as those associated with the advent of a vaccine. Similarly, there is a higher willingness‐to‐accept value for increases in risk, as would occur if all protective restrictions are lifted. For small changes in risk, the direction of the risk change does not alter the VSL. While COVID‐19 mortality risks are substantial, the magnitude of the risk is similar to that of many high‐risk occupations that are used to generate the VSL estimates. Most important is to consider the size of the risk change for any particular policy intervention. Except for interventions such as the COVID‐19 vaccines, which was not first approved until December 2020, all policy actions have been fairly limited in scope. Restricting restaurant dining, urging use of face masks, and promoting social distancing do not lead to risk changes that are so great that the usual VSL figure is inappropriate. If larger risk changes are contemplated, modest adjustments to the VSL level based on the structure of utility functions are feasible (Hammitt, 2020; Viscusi, 2010, 2020).
Although my focus is on the monetization of the health risks generated by COVID‐19, the downturn in the economy and the accompanying reduction in income have health ramifications as well. Comprehensive assessments of the mortality cost also should include the mortality costs that are associated with a loss in income. Based on the conceptual approach in Viscusi (1994) coupled with recent empirical estimates in Broughel and Viscusi (2021), a loss in income of just over $100 million will lead to one expected death based on a VSL of $10 million. This relationship highlights the important link between the performance of the economy and individual health. Shutting down economic activity to limit the pandemic has adverse health consequences in addition to the favorable reduction in risk due to decreased social contacts. Income transfers such as unemployment compensation consequently serve a health‐related function in dampening these losses.
2.2. Global mortality costs
The COVID‐19 pandemic has caused over one million deaths worldwide. As of September 26, 2020, there had been 996,879 deaths based on reports for 163 countries. By the end of the year, the number of global deaths had reached 1,829,126 based on Worldometer (2021) data.
It is feasible to monetize these risks using the VSL, but the VSL that should be used for these calculations should reflect the risk preferences of the residents in the particular country. To generate estimates consistent with those for the United States, I use the U.S. VSL as the baseline and make appropriate adjustments given the differences in income as compared with the United States. While there may be other international differences in risk preferences, income adjustments are the most feasible. The international income elasticity of the VSL is 1.0 based on evidence in meta‐analyses of revealed preference studies (Viscusi and Masterman 2017) and stated preference studies (Masterman and Viscusi, 2018). Coupling this elasticity estimate with the GNI per capita yields the VSL estimates by the country that appear in Column (2) of Appendix Table A1. For example, the pertinent VSL is $7.8 million in the U.K., $2.9 million in Brazil, $7.1 million in Italy, and $8.0 million in France. Multiplying the number of deaths in each country by the country‐specific VSL yields the mortality cost figures in column 3 of that table. Countries appear in Table A1 in order of their total mortality cost. Through September 26, the global mortality cost was $5.4 trillion, but by the end of the year it had climbed to $10.1 trillion.
These health costs represent the monetized value of the adverse health impacts that have been incurred despite efforts to reduce the risk. From the standpoint of policy decisions, what is pertinent are the marginal risk reduction benefits and marginal costs of individual policy actions. The overall health cost figure for the mortality losses incurred to date is, however, demonstrative of the enormous scale of the damage that results in the absence of vigorous precautionary actions.
Although some countries such as the United States have been particularly hard hit, there have been some outstanding performers as well. Because of its highly responsible policies to control the virus, New Zealand has had an especially laudatory record in that it had only 25 deaths based on the data that I used at the time of my conference presentation, which covered the period through September 26, 2020. Remarkably, New Zealand still only had 25 deaths by the end of the year. Total COVID‐19 mortality has completely abated in New Zealand, while the United States experienced an additional 146,454 deaths during this three‐month period. Based on New Zealand's VSL of $6.9 million, that country's mortality cost is $173 million through 2020. Although some observers may attribute New Zealand's excellent performance not to its vigorous precautionary efforts but to its advantage of being relatively isolated and comprised of islands, other islands have not fared as well. Hawaii has a population of 1.4 million, or less than one‐third of the New Zealand population of 4.7 million. Yet Hawaii has had over 10 times as many COVID‐19 deaths—289 deaths by the start of 2021.
2.3. Assessing the U.S. mortality rate performance
The United States share of the global mortality costs is out of line with its population share. As shown in Figure 1, by the end of 2020 the United States had 19% of the global deaths. Given the high VSL figure in the United States, the U.S. share of the global mortality costs is 39%. The international spread of COVID‐19 by the end of 2020 has made the U.S. performance a bit less appalling than it was based on data at the end of September when the United States had 21% of the deaths and 42% of the mortality costs. Figure 2 lists the top five countries in terms of global mortality costs. The United States is followed by the United Kingdom, Brazil, Italy, and France.
FIGURE 1.
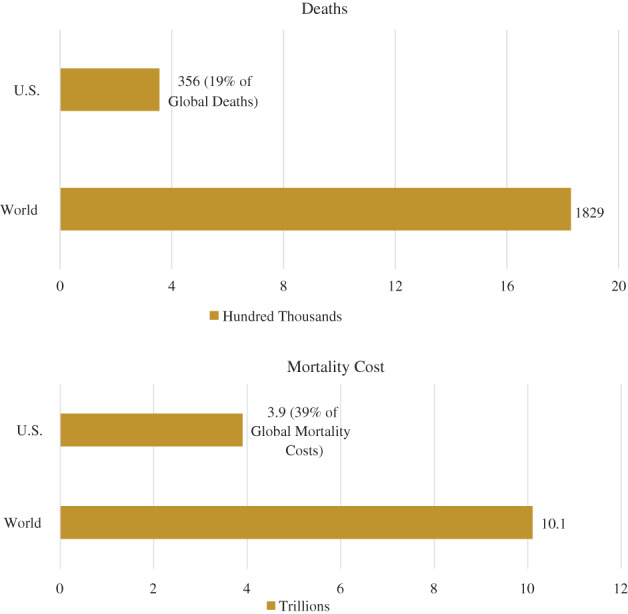
The U.S. share of COVID‐19 deaths and mortality costs [Color figure can be viewed at wileyonlinelibrary.com]
FIGURE 2.
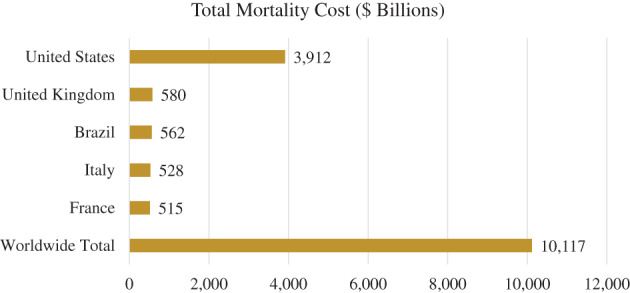
The top five countries by total COVID‐19 mortality cost [Color figure can be viewed at wileyonlinelibrary.com]
A question raised by the high level of pandemic‐related mortality in the United States is whether the U.S. performance is an outlier. High VSL countries should place a greater value on the promotion of health and have lower risks if they face the same marginal cost curves as other nations. To get a sense of the relative performance of the United States, I ran some simple regressions that might be viewed as the econometric equivalent of a back‐of‐the‐envelope calculation. The dependent variable is the country's COVID‐19 mortality rate per 100,000 population. The worldwide average mortality rate is 241.9 per million, and the U.S. mortality rate is 1109 per million. The explanatory variables included the country's VSL, a 0–1 indicator for the United States, the percentage of the population age 65 and older, the urban population share, the population density, the GDP change in quarter 1 and in quarter 2, the index of economic freedom (coded using indicators for 3 of the 4 quartiles on this ranking), and a World Health Organization quality of health care index (coded using indicators for 3 of the 4 quartiles on this ranking). Appendix Table A2 lists the data sources and variable definitions.
The regression results in Table 1 indicate a simple positive correlation of the VSL with the COVID‐19 mortality rate in the first column. The second column of Table 1 adds the U.S. indicator variable, and subsequent regressions in Table 1 include a more comprehensive set of variables. As expected, countries with a higher population share that is 65 and older have higher mortality rates. Given the contagious nature of the disease, COVID‐19 mortality rates are positively correlated with the urban population share variable. The final column includes the percentage change in GDP in the first two quarters, which are likely to be endogenous. The indicator variable for the United States reflects a strong positive effect irrespective of the controls. While the VSL variable is no longer statistically significant once a comprehensive set of other variables is included, the U.S. indicator continues to reflect a strong impact across all the regressions in Table 1. The magnitude of the coefficient is 57% of the total U.S. mortality rate after including all these controls. By almost any measure, the performance of the United States has fallen short of what should be expected for an affluent country in which the high VSL should foster greater protection of individual health.
TABLE 1.
Regressions of COVID‐19 mortality rate per million population
| COVID deaths per million | ||||
|---|---|---|---|---|
| Variables | (1) | (2) | (3) | (4) |
| Value of a Statistical Life | 21.28*** (6.62) | 19.71*** (6.64) | −10.32 (6.69) | −0.32 (8.87) |
| United States Indicator | 654.28* (366.65) | 540.57* (295.22) | 631.16** (267.19) | |
| Percent Age 65+ | 29.06*** (3.70) | 26.97*** (5.21) | ||
| Urban share | 4.42*** (1.31) | 3.34*** (1.28) | ||
| Pop. density (person/km sq.) | −0.01 (0.02) | |||
| Q2 GDP % change | −38.07*** (7.81) | |||
| Q1 GDP% change | −34.53* (19.83) | |||
| Econ. freedom index percentile 75–100 | −20.33 (81.79) | |||
| Econ. freedom index percentile 50–75 | 147.62** (67.00) | |||
| Econ. freedom index percentile 25–50 | −43.52 (58.93) | |||
| Health rank percentile 75–100 | −121.24 (97.13) | |||
| Health rank percentile 50–75 | −44.64 (71.06) | |||
| Health rank percentile 25–50 | 100.77 (63.49) | |||
| Constant | 197.93*** (36.71) | 200.14*** (36.51) | −206.20*** (68.01) | −526.14*** (154.82) |
| R2 | .05 | .07 | .41 | .56 |
Note: N = 180. Regressions also include indicator variables for any missing GDP data. Standard errors in parentheses.
p < .01,
p < .05,
p < .10.
2.4. Morbidity effects
The primary focus of health risk statistics is on mortality effects. Deaths are well‐defined events, although the cause of the death is not always apparent. Countries throughout the world have reported regularly on the number of deaths from COVID‐19. There are also reports of the number of positive cases by country, but these tallies depend in part on the testing rate. The focus here is on the morbidity effects for the United States, for which there is information on the distribution of the morbidity consequences.
Even if you do not die from coronavirus, for many of the victims of the disease the adverse health impacts are substantial. Based on the distribution for those who had positive tests through May 30, 2020, 14% were hospitalized and 2.3% were in the ICU (Stokes et al., 2020). The COVID‐19 symptoms are quite extensive, including: fever, cough, shortness of breath, muscle aches, headaches, loss of the sense of taste and smell, brain fog, and cardiovascular ailments. Some of these symptoms are temporary, while others, such as cardiovascular problems, may have a longer‐term impact on health.
The appropriate benefit measure is the analog of the VSL, which is based on the willingness‐to‐pay to reduce the risk of these morbidity effects. In the absence of available studies to monetize these morbidity risks, it is instructive to adopt the benefit transfer approach that government agencies use in assessing the benefits of risk and environmental regulations. Benefit transfer assessment techniques assign a unit benefit value to different health outcomes using estimates of the unit benefit values for health impacts of comparable severity. Typically, this procedure involves matching situations involving similar types of health impacts on the individual.
In constructing the calculation of morbidity costs, I break the morbidity effects into two groups—nonhospitalized cases, which tend to be less severe, and hospitalized cases. For the nonhospitalized cases, I use the unit benefit value of $3,000 for asthma risks, which is based on the estimates for asthma by O'Conor and Blomquist (1997) and Blomquist et al. (2011), after updating for inflation. Both of these studies are stated preference analyses in which the willingness‐to‐pay values were elicited for asthma risks. Despite the much greater prevalence of nonhospitalized cases, the fairly low unit benefit amount of $3,000 per case makes these impacts a relatively modest contributor to the monetized value of the COVID‐19 morbidity costs.
The more consequential component is that of hospitalized cases, which can be monetized in two different ways. The first approach is based on the estimates for the risk of chronic bronchitis developed by Viscusi et al. (1991), in which the study participants undertook a risk‐risk tradeoff involving chronic bronchitis and risks of death. The results from this study have been used in many regulatory impact analyses by the U.S. Environmental Protection Agency to value the risks of respiratory illnesses from air pollution exposures. Based on the estimated risk‐risk tradeoff coupled with the VSL, the monetized value for the risk of hospitalization for COVID‐19 is $3.4 million. Following the procedure described in Viscusi (2020), using this figure in calculating the upper bound value of morbidity costs, the morbidity cost for the hospitalized cases is 50% of the value of the mortality costs.
An alternative approach for monetizing these COVID‐19 morbidity effects involves the application of the morbidity component of the VSL. Gentry and Viscusi (2016) distinguish the valuation of the two different components of occupational fatality risks—the loss of one's life and morbidity effects before death that are associated with fatal injuries. The mean value of the morbidity loss using current estimates of the VSL is $2.75 million per expected case. I use this figure below in calculating the lower bound value of morbidity costs of the hospitalized cases. Based on this value, the morbidity cost of the hospitalized cases is 40% of the mortality costs.
The combined morbidity effect values based on the distribution of nonhospitalized cases and hospitalized cases consequently equals 40% of the mortality costs of COVID‐19 based on the VSL morbidity cost component and 50% using the chronic bronchitis values.3 Most of these costs are attributable to the hospitalized cases. Although under one‐fifth of all people with positive tests are hospitalized, the benefit values applied to each hospitalized case are almost 1,000 times as great as for the nonhospitalized cases. If the 40%–50% morbidity cost‐share remains applicable to the mix of morbidity symptoms during the year, the total morbidity cost in the United States through the end of 2020 is $1.6–2.0 trillion, and the combined mortality and morbidity costs is $5.5–5.9 trillion.
Although these estimates of the morbidity effects are substantial, some estimates may be greater. Kniesner and Sullivan (2020) present estimates of the morbidity costs using U.S. Department of Transportation benefit values for transportation accidents in their benefit transfer approach. They estimated morbidity costs ranging from $1.5 trillion to $9.6 trillion. A major consideration leading to the broad range of estimates in their analysis is that the extent of the morbidity effects may be much higher than is reflected in the positive case statistics if there is a substantial number of people who have the illness, experience morbidity effects, and are never tested.
3. THE CRITICAL ROLE OF AGE
3.1. The age distribution of COVID‐19 mortality
The fatalities resulting from COVID‐19 are not uniformly distributed throughout the population. In the initial months of the pandemic, residents in nursing homes were particularly hard hit. Through September 30, 2020, there was enormous skewness in the age distribution of these deaths.4 At that time, 31% of the deaths were to those age 85 and over, and 79% of the deaths were to those age 55 and over.
The age distribution is potentially relevant to the applicable VSL since there is substantial heterogeneity in the VSL by age. Figure 3 shows an illustrative trajectory of the VSL by age based on labor market estimates of the VSL. Other estimates based on labor market data similarly show that the life‐cycle trajectory of the VSL displays an inverted‐U shape similar to that of the life‐cycle income trajectory. The VSL rises with age, reaching a peak in the mid‐40s, after which it exhibits a decline. The decline in the VSL with age is not, however, stark, as the VSL for workers age 62 exceeds that of workers at age 20.
FIGURE 3.
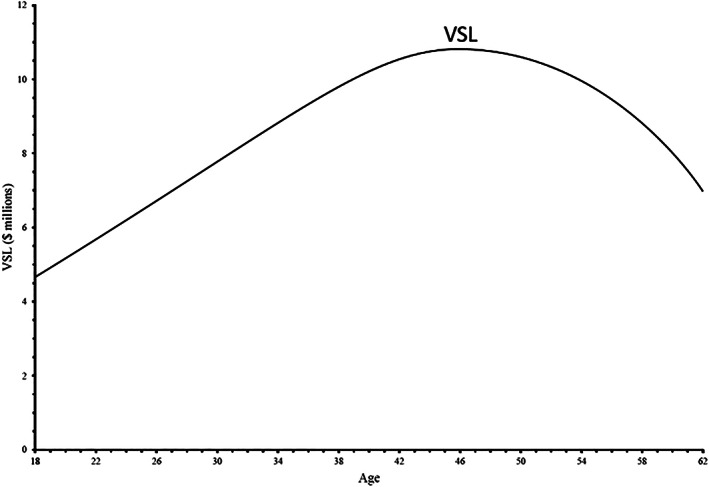
The VSL‐age trajectory
Labor market estimates of the VSL are generally restricted to those below the usual retirement age. One can construct the VSL beyond usual retirement ages using a value of a statistical life year (VSLY). For purposes of these calculations, based on my past studies reviewed in Viscusi (2020), I adopt a VSLY of $500,000. Using a discount rate of 3%, the procedure below will use the discounted value of this stream of VSLY amounts to construct the VSL for workers beyond age 55. For comparison, the undiscounted results are also presented.
Embarking on any age variation in the VSL is a controversial undertaking. In its analysis of the Clear Skies Initiative, the U.S. Environmental Protection Agency (EPA) adopted a downward age adjustment for those age 65 and older, reducing their applicable VSL by 37%. The result was a political firestorm against the “senior discount,” leading to headlines in critical articles such as “Seniors on Sale, 37% off” and “What's a Granny Worth?” EPA abandoned this approach given the public outcry.
Notwithstanding the potential controversy that arises from even considering the prospect of downward adjustments in the VSL for older people, what would the effect of adopting an age‐adjusted VSL be on the estimates of the mortality costs of COVID‐19? Instead of a VSL of $11 million for those aged 85, their VSL declines to $3 million. The average age‐adjusted VSL for the COVID‐19 age distribution is $6.3 million if there is no discounting of the VSLY stream and $5.2 million if a discount rate of 3% is applied to the stream of VSLY values.
The total effect of accounting for age adjustments to the VSL is to cut the mortality cost estimate roughly in half. For the calculations in which there is no discounting of the VSLY streams, there is a 45% reduction in mortality costs, while if there is discounting the reduction is 53%. If these estimates are incorporated into the calculations, the total mortality cost figure is $2.1 trillion in the no discounting case and $1.8 trillion if there is discounting of the VSLY effects. Based on the estimates including discounting, the overall health cost of COVID‐19 including both mortality and morbidity costs consequently is $3.4–3.8 trillion in 2020, which is still a huge cost figure.
3.2. Principles for recognizing heterogeneity in the VSL
Should policy analyses of COVID‐19 incorporate such age adjustments, notwithstanding the controversies that might arise? From the standpoint of economic efficiency, recognition of the heterogeneity simply recognizes the heterogeneity in attitudes toward risk that have been revealed in market decisions. Willingness‐to‐pay values for risk reduction do vary with age and other personal characteristics.
However, efficiency considerations are not the only drivers of assessments of the merits of considering age adjustments. Discussions of VSL heterogeneity also raise equity concerns that have arisen in the broader literature on risk equity. Some economists and ethicists have proposed notions of risk equity such as equalizing the life expectancy of all population groups, equalizing the absolute risk level, or ensuring that all people have an annual mortality risk that does not exceed a certain level. In a discussion of equity concepts in Viscusi (2018), the risk equity concept that I have found to be attractive in many contexts is what I term “equitable risk tradeoffs.” Thus, rather than equalizing an objective measure of risk or life expectancy levels, the task is to adjust policies to set the risk‐money tradeoff equal to a common population‐wide VSL. Others might advocate different approaches to achieving equitable risk tradeoffs such as equalizing the VSLY across the population, which will then be used in conjunction with the person's life expectancy. Equalizing the VSL is more protective of older age groups than is equalizing the loss based on a common VSLY. The current practice of U.S. government policies is consistent with the equitable risk tradeoffs approach based on the VSL, as agencies use a uniform VSL in regulatory impact analyses for health, safety, and environmental regulations.
Should we choose to incorporate the heterogeneity of the VSL, analysts should not cherry‐pick particular personal attributes. The general principle I advocate for when there is the personalization of the values to those affected by the policy is that the procedure should be comprehensive and not restricted to a single attribute. The attributes that have received the most scrutiny in the literature are age and income. There are strong income‐related dependencies of the VSL. Many estimates of the income elasticity of the U.S. VSL are in the range of 0.6, and some available estimates are in excess of 1.0. Proper application of these income‐related variations in the VSL would reduce the VSL applied to the poor. Many of those most affected by COVID‐19 have below‐average income levels, including essential workers in grocery stores and other retail establishments, as well as those engaged in the production and delivery of food. Similarly, people whose jobs do not permit them to work at home and who must rely on public transit for their commute also are subject to considerable COVID‐19 risks. Policies that protect their lives would be less highly valued if there were income adjustments. Given the strong societal interest in maintaining the efforts of such individuals, it is unlikely that there would be support for applying a lower value to their lives, which in turn would lead to less policy emphasis on protecting their well‐being.
3.3. COVID‐19 ventilator rationing
Age has played a central role in discussions of optimal rationing of constrained medical resources during the COVID‐19 pandemic. Ventilators have been the chief example of medical treatments in short supply, but ICU beds and hospital facilities also have been severely constrained. If medical resources are to be rationed, who should receive them? The stakes involved are higher than in many risk regulation contexts since withholding medical treatment may lead to certain death. The provision of appropriate care may have a substantial impact on the probability of survival. Such changes in the probability of survival dwarf those encountered in most risk policy contexts by several orders of magnitude.
Medical rationing questions and advocacy of policies that disadvantage older age groups are not mere philosophical musings. During the COVID‐19 pandemic, a hospital in Italy restricted ventilators to patients under the age of 60, presumably based on their shorter remaining life expectancy.5 The economic merits of interventions may, of course, have some relationship to age. However, if the VSL is equal for all age groups, the critical factor is how effective a particular intervention is in reducing the probability of death, not the person's age. The reduction in the probability of death achieved by the intervention may depend on a variety of personal characteristics, including age, but age alone is not a sufficient determinant of the incremental change in the mortality risk provided by the use of ventilators.
The COVID‐19 pandemic has highlighted that medical resource allocations pose daunting challenges that must be resolved in a wide variety of situations. There has been a flurry of recent pronouncements by bioethicists affiliated with major medical centers on how to best allocate medical resources. Unencumbered by any economic analysis, these bioethicists often make sweeping recommendations that are inconsistent with efficient economic principles for reducing risk. The principal focus has been on triage or lifeboat scenarios in which, in their view, older people should fare badly. Weill Cornell Medical College medical ethicist Franklin G. Miller (2020) advocates a strict age criterion for rationing: “I would suggest that an initial age criterion for rationing ventilators when the demand outstrips the supply is a cut‐off of 80. Eighty is just above the average life expectancy in the United States, which is 79 years.” While he claims that older people have already had the “opportunity to live a complete life,” his age cap will shorten the lives of those affected. An average life expectancy of 79 does not mean that you die at that age. The remaining life expectancy conditional on being age 80 is 8.4 years for men and 9.8 years for women. If ventilators are in very tight supply, his age cutoff gets more stringent, as he recommends an age 70 cutoff. The remaining life expectancy at age 70 is 14.5 years for men and 16.7 years for women. Each of these groups has a substantial VSL even on an age‐adjusted basis.
A Vanderbilt University medical ethicist Larry R. Churchill similarly advocates the institution of age cutoffs. In what he designates as a “fair innings approach,” older people have already had their “turn at bat.”6 This rationale parallels that of Miller in which having past enjoyment of life years is the driving force guiding allocation decisions rather than the prospective future benefits of the intervention. A University of Pennsylvania medical ethicist and colleagues (Schmidt et al., 2020) also emphasize previous personal histories and advocate allocation of the first COVID‐19 vaccines to the poor and members of minority races since they have a lower life expectancy and have been subject to much greater disadvantages in their lives. Once again it is not the prospective benefits of interventions that is the pivotal concern in this approach but a claim that their previous welfare history has not been as advantageous. In the ethicists' view, giving them priority would create greater life expectancy parity and overcome other disadvantaged aspects of their lives, such as their lower provision of adequate retirement savings.7 The rationale for this approach is based on social justice considerations independent of any efficiency‐related rationales. The phenomenon embodied in this retrospective approach and that of the previous enjoyment‐of‐life rationales is very reminiscent of the erroneous concern with sunk costs, which should not be pertinent when making prospective economic decisions.
A final variant on the effort to diminish the protection for older people is that a Duke University social choice theorist advocates taxing older people because they benefit disproportionately from social distancing efforts given their greater vulnerability to COVID‐19. Adler's (2020) recommendation departs from the usual social justice recommendations through his advocacy of income redistribution from the old to the young, irrespective of the more conventional equity concerns based on income status. The more standard focus of equity‐based advocates is not to penalize senior citizens but to recommend that society transfer income to older people since their labor market opportunities are more limited.
The overriding theme of the various ethical pronouncements is that the high COVID‐19 mortality rate has made it open season on older people. In addition to being more severely affected by COVID‐19, older people will also receive less medical treatment in the ethicists' ideal world, and will be penalized in other ways. Remarkably, there is no attempt to ground these ethical recommendations in analyses that address the economic merits of the recommendations based on efficiency criteria for risk reduction.
Those who oppose the mistreatment of people based on age also do not base their views on economic principles. The American Geriatrics Society strongly opposes the use of age as a rationing mechanism: “Age per se should never be used as a means for a categorical exclusion from therapeutic interventions that represent the standard of care. Likewise, specific age‐based cutoffs should not be used in resource allocation strategies.”8 Restrictions on the provision of medical care based on age are also illegal. Discrimination on the basis of age is a violation of § 557 of the Affordable Care Act, which explicitly prohibits discrimination on the basis of race, color, national origin, sex, age, or disability for healthcare programs receiving federal funds. After the advent of the COVID‐19 pandemic, the U.S. Department of Health and Human Services (2020) issued a bulletin to emphasize that age and disability status cannot be used to ration health care during this pandemic. Notwithstanding these directives, there are feasible, legal ways for medical providers to sidestep the legal hurdles by relying on remaining life expectancy rather than age as the criterion for allocation. Senior citizen groups oppose all such variants in principle but do not present economic rationales in defense of older people.
Returning to first principles, it is useful to recall the economic criteria for proper assessment of the benefits of risk reduction. The value of the mortality risk reduction consists of the reduced probability of death multiplied by the VSL. Younger people have a lower probability of death than older people, but what is relevant for assessing the benefits of interventions is not the absolute probability of death but the reduction in the probability of death that can be achieved through the provision of medical care. While the absolute probability of survival is a component of this calculation, it is not sufficient to allocate treatment based on the chance of survival alone even though sometimes this is the exclusive focus.9 Even if the change in the probability of survival is the basis for allocations, there may be differences in the efficacy of treatments in which older patients may still fare badly, but at least the allocation decision will be governed appropriately by the marginal benefits associated with the care. The second component of the calculation is the VSL. If one adopts an equitable tradeoffs approach and uses the same VSL for all, then the allocation will be driven by the reduced probability of death. If one instead chooses to personalize the VSL estimate, there may be differences across patients that will vary based on age and income. However, it may be difficult to ascertain the individual willingness‐to‐pay value for the risk reduction, which is the counterpart of what the economic calculation above is intended to construct.
A recurring theme that arises in treatments of the potential triage scenarios is that it is clearly quite difficult to make such rationing decisions when medical interventions such as ventilators have an extremely high payoff, but resources are severely constrained. Unfortunately, the triage scenarios deal only with the terminal aspect of our multi‐period resource allocation problem. Given the tremendous benefits that could be derived by having more adequate medical resources, it is preferable from a benefit‐cost standpoint to make provisions before health crises arise so that severe rationing is not required for the next pandemic. In anticipation of future pandemics, it is feasible to acquire high‐quality ventilators at a cost from $25,000 to $50,000. Adding in the cost of medical support personnel would raise the annual cost to about $100,000. A reserve supply of ventilators could be a component of an anticipatory pandemic policy. Preparing for future pandemics remains a cost‐effective strategy even for annual probabilities of a pandemic on the order of 1/100. However, survey evidence by Pike et al. (2020) suggests that support for protective efforts of this type is unlikely to emerge, as there is a lack of public concern with long‐term pandemic risks. As a result, there is likely to be a continued shortfall in preparations for prospective risks, leading to future repetitions of the difficult rationing decisions posed by COVID‐19.
Similar kinds of concerns arise with respect to more modest treatment allocations, such as the priority list for receiving COVID‐19 vaccines. One could, for example, auction off priority slots for COVID‐19 vaccinations. Doing so might be an effective way of incorporating the private valuation of the risk reduction into the allocation system. Setting aside equity and feasibility concerns, the auction approach is deficient because the vaccine is not a private good. Vaccinations provide external benefits to those who will not be exposed to an infected person. Considerations of efficiency consequently also involve assessing the protective benefits that others receive. There is no reason to believe that the private values will reflect these ramifications. As a result, allocation strategies should take into account the overall risk reduction benefits, not just the benefits to the person vaccinated. The frontline workers and medical personnel would be among the groups for which the external benefits may be substantial. It should also be noted that many of these essential worker groups are minorities or lower‐income workers so that an emphasis on efficient risk reduction also promotes the well‐being of less advantaged members of society.
4. RISK COMMUNICATION FAILURES
The protective responses to the COVID‐19 pandemic require actions that the public must take on a decentralized basis. Chief among these is social distancing and all of its ramifications, including limitations on frequenting restaurants, bars, concert venues, parties, and family gatherings. Personal protective behaviors include wearing masks, washing and sanitizing your hands, avoiding unnecessary travel, and limiting public contacts. These protective activities have a risk reduction benefit for the individual as well as an external risk reduction benefit to others. Monitoring of personal behaviors is limited, and enforcement is similarly weak, though not entirely nonexistent. Airlines, for example, have refused to allow passengers who do not wear masks to travel, and some stores and restaurants enforce mask wearing except when the customer is eating or drinking.
To achieve risk reductions through these decentralized individual behaviors, the government or other institutions often must rely on establishing a social norm in lieu of regulations or mandates that can be legally enforced. The analysis of social norms has received less attention from economists than have command‐and‐control regulations. However, conceptualization of what is likely to be effective in establishing a norm often will depend on underlying economic principles. Either because of their own self‐interest in risk reduction or because of the external benefits and costs that are generated through the behavior of others, finding the protective behavior to be expected‐utility maximizing will enhance the likelihood that the person undertakes the particular precaution. Providing information to enable people to make appropriate judgments of this type is often essential.
Since the pre‐pandemic behavior did not incorporate precautions such as mask wearing, there must be some personal recognition that the pandemic poses a new level of risks meriting changes in behavior. This recognition must include both an understanding of the level of the risk and the efficacy of precautions in reducing the risk. Because COVID‐19 is a novel coronavirus, public health officials needed to develop their knowledge of which routes of exposure posed the greatest risk and the efficacy of different protective measures. That knowledge in turn suggests the most fruitful approaches for protective actions. The magnitude of the risk, the mechanisms of transmission, and the efficacy of different measures may not have been understood at the onset of the pandemic. In this situation of evolving information, maintaining the credibility of public information sources is particularly challenging since changes in the official guidance already will impede efforts to communicate credibly.
Consider a representative Bayesian citizen. The person assesses a prior risk p of illness from the pandemic. The risk that public health officials are communicating is q, which I will assume exceeds p. For both value of p and q, there is an associated informational content, which is the weight that the person places on the prior and on the new information. The informational content of p can be viewed as the number of balls that the person has drawn from a Bernoulli urn in forming prior beliefs, a fraction p of which indicates an adverse illness outcome. Similarly, the informational content of q reflects the number of balls that the person has drawn from a Bernoulli urn pertaining to the new information, where a fraction q indicates an adverse illness outcome. If the person finds the communicated risk highly credible, that will be equivalent to q being associated with a larger number of draws from the urn, so that it will receive a greater relative weight. The total amount of information is the sum of the number of balls reflected in the beliefs pertaining to p and q. It is feasible to express the Bayesian updating in terms of the fraction of the information associated with p and q.10 The posterior risk assessment s is given by
s = (fraction of information content of prior) x p + (fraction of information content of new information) x q.
The efficacy of the risk communication effort in influencing risk beliefs hinges on both the value of q and the fraction of the informational content associated with the risk information. In a series of studies of individual processing of hazard warnings and other types of risk communication, I have estimated the risk q implied by these efforts and the relative informational content of the new information. I have found that the driving force of the efficacy of risk communication efforts is usually not the value of q but whether the provided information is viewed as being highly credible, giving people an incentive to adjust their risk beliefs. In terms of lessons for the current pandemic, the persistent undermining of the credibility of information sources has been particularly destructive to risk communication efforts.
The credibility of the information depends on what risk information is being communicated as well as on the credibility of the information source. If the focus of the information is on worst case scenarios, then people may not trust the veracity of the information. In the case of some government agencies, the reported risk levels are upper bound estimates of the risk rather than mean estimates. Fortunately, in the case of COVID‐19 the emphasis seems to have been on reasonable risk assessments rather than exaggerated values intended to motivate precautions. The other aspect of credibility is the credibility of the information source. During the course of the pandemic, there was continued high level of public respect for infectious disease experts such as Dr. Anthony Fauci, the Director of the National Institute of Allergy and Infectious Diseases.
Matters became more muddled when statements by immunologists are in apparent conflict with pronouncements by prominent political figures. The principal failure of the U.S. risk communication effort has been the undercutting of scientific experts by high‐ranking government officials instead of fostering trust. Even with ideal governmental behavior, the task of having credible risk communication is challenging. The knowledge of the pandemic risks and the efficacy of steps to reduce these risks is evolving, as is the level of the outbreak in different regions and social contexts. The fluidity of the situation necessitates some changes in recommended behaviors and tailoring of these recommendations to different circumstances. Given the inherent difficulties of communicating risks effectively in this dynamic situation, communication efforts should strive to provide a coherent, scientifically accurate message.
5. VALUES THAT CANNOT BE COMPROMISED
The resistance to scientific evidence is closely entwined with opposition to infringements on personal freedom that will result from protective behaviors such as mask wearing. Perceptions of the COVID‐19 risk and the efficacy of precautions are strongly correlated with political beliefs (de Bruin et al. 2020). For some, individual freedom is an absolute right that can never be compromised. Claims of absolute rights are also made on behalf of safety. In much of my career, I have encountered those who oppose any tradeoffs involving risks to life, much less placing a dollar value on these risks.
The statement on COVID‐19 treatments by New York Governor Andrew Cuomo reflects such a refusal to engage in tradeoffs: “My mother is not expendable. And your mother is not expendable. And our brothers and sisters are not expendable…We're not going to put a dollar figure on human life.”11 An uncompromising risk reduction approach is not feasible generally. If human life is accorded an appropriate monetized value, the application of VSL and efficient principles for controlling risks will lead to greater levels of protection than will result if medical personnel follow the guidance provided by many prominent medical ethicists.
In the case of COVID‐19 policies, absolutes can conflict with each other. Society confronted similar conflicts after the 9/11 attack (Viscusi and Zeckhauser, 2005). To reduce terrorism risks, we accepted more intrusion on personal liberties, including airport screening and additional surveillance efforts. Parallel conflicts between values that purportedly cannot be compromised occurs with respect to COVID‐19 policies, where the values at stake here are the expected health impacts and personal freedom.
Figure 4 illustrates the nature of the societal decision. The horizontal axis is a measure of personal freedom, and the vertical axis is the expected health losses from the pandemic. Because personal freedom is valued positively, and lower values of health losses are preferable, the direction of preference is in the southeastern direction. For the dashed line indifference cures in the diagram—I1, I2, I3, and I4—the lowest curve I4 reflects the highest expected utility level and I1 reflects the lowest level. Before the pandemic, the opportunity locus was the lower solid curve xx. The optimal combination of freedom and health is at point A, which has health losses at point a and the indicated pre‐pandemic optimal level of personal freedom.
FIGURE 4.
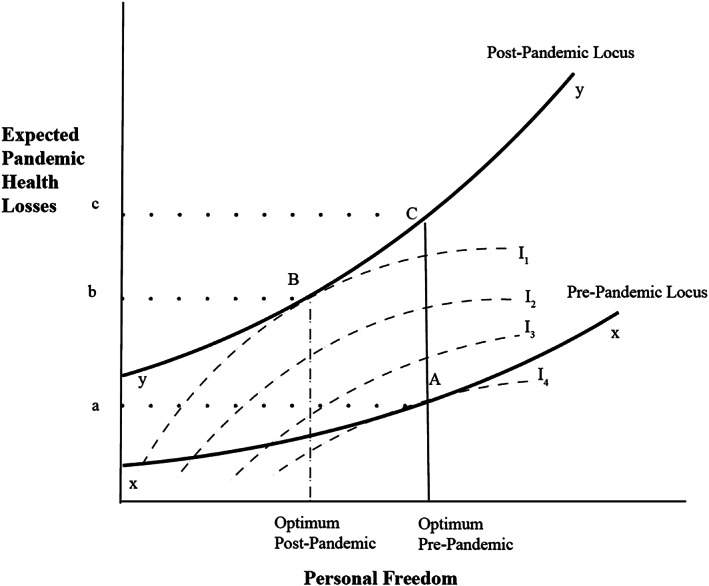
The personal freedom‐health risk tradeoff
After the pandemic, the opportunities locus shifts upward to the curve yy. For any given level of personal freedom, the expected health losses have risen. If there is no restriction on personal freedom, the outcome will be at point C, with expected health losses c. For the curves shown in Figure 4, the new optimum is at point B. Choosing an outcome at point B leads to less personal freedom than before, but there are benefits in terms of lower health costs. Taking precautions reduces the adverse health effects from c to b. Failure to recognize that some sacrifice in personal freedom is desirable leads to a welfare loss. It should be noted that personal freedoms are limited but not eliminated in Figure 4. The practical policy task is to ascertain which restrictions yield benefits sufficient to warrant the costs.
6. ECONOMIC LESSONS
Coronavirus is a novel disease, but we remain on familiar economic turf. The kinds of policy choices that are encountered bear many similarities to those posed by health, safety, and environmental policies. Just as economic frameworks are instrumental in conceptualizing the competing effects and optimal decisions in those contexts, economic insights also provide valuable guidance for pandemic policies with respect to valuing risks, communicating risks effectively, and thinking about tradeoffs in order to promote efficient outcomes.
The risk valuation component is central to all choices as it sets the price for the health risk reductions, which in turn provides the justification for incurring a variety of costs, including economic dislocations. Monetizing mortality costs based on the VSL indicated that COVID‐19 imposed substantial U.S. mortality costs in 2020 of $3.9 trillion, and a total mortality and morbidity cost of $5.5–5.9 trillion. By March 2021, the U.S. death toll will have reached 500,000.12 Extrapolating the results to this mortality level implies an associated mortality cost of $5.5 trillion and a combined mortality and morbidity cost of $7.8–8.3 trillion. The magnitude of these costs makes it clear that vigorous efforts to control the virus are clearly desirable.
The targeting of these efforts can be assisted by proper understanding of economic guidelines for valuing risks. Whether older people should be placed on ventilators and determining who should be provided the vaccine are all matters that can be structured in a sensible manner. In the absence of economic frameworks, there is a tendency to resort to purported ethical principles that sometimes represent arbitrary judgments devoid of any recognition of the economic value of the mortality reduction benefits.
The decentralized nature of precautionary behavior makes it essential that risks be communicated effectively. To do so, the risks that are communicated must be credible. A critical aspect of credibility is that the information source must be trustworthy. A principal deficiency of the risk communication effort for COVID‐19 has been the undercutting of efforts by scientists to communicate the risk, which has created a highly fragmented and often inconsistent informational environment.
The final overriding economic lesson is that it is essential to consider tradeoffs, even for those attributes that some may view as absolute. It is not feasible to live in a risk‐free world or to have complete freedom. Unlimited personal freedoms will lower our well‐being, particularly when confronting crises for which collective, responsible behavior is desirable. Recognition and proper valuation of what is at stake will enable us to strike an appropriate balance between these competing concerns.
TABLE A1.
The global mortality costs of COVID‐19 as of January 1, 2021
| Country | Number of deaths | VSL ($ millions) | VSL x deaths ($ millions) |
|---|---|---|---|
| Total | 1,829,126 | – | 10,116,632 |
| United States | 355,631 | 11 | 3,911,941 |
| United Kingdom | 74,125 | 7.8188 | 579,569 |
| Brazil | 195,152 | 2.8776 | 561,569 |
| Italy | 74,621 | 7.0796 | 528,287 |
| France | 64,632 | 7.9684 | 515,014 |
| Mexico | 125,807 | 3.223 | 405,476 |
| Spain | 50,837 | 6.6682 | 338,991 |
| Germany | 34,388 | 9.3841 | 322,700 |
| Russia | 57,555 | 4.5441 | 261,536 |
| Iran | 55,337 | 3.487 | 192,960 |
| India | 149,205 | 1.1528 | 172,004 |
| Belgium | 19,528 | 8.7285 | 170,450 |
| Argentina | 43,245 | 3.8258 | 165,447 |
| Poland | 28,956 | 4.9566 | 143,523 |
| Canada | 15,606 | 8.3919 | 130,964 |
| Colombia | 43,213 | 2.5905 | 111,943 |
| Netherlands | 11,529 | 9.4457 | 108,899 |
| Switzerland | 7662 | 12.254 | 93,890 |
| Peru | 37,680 | 2.3056 | 86,875 |
| Sweden | 8727 | 9.3104 | 81,252 |
| Turkey | 21,093 | 3.7741 | 79,607 |
| Chile | 16,660 | 4.3516 | 72,498 |
| South Africa | 28,887 | 2.4607 | 71,082 |
| Czech Republic | 11,711 | 6.0313 | 70,633 |
| Romania | 15,841 | 4.1316 | 65,449 |
| Saudi Arabia | 6230 | 10.4841 | 65,316 |
| Austria | 6261 | 9.3984 | 58,843 |
| Hungary | 9667 | 4.8257 | 46,650 |
| Indonesia | 22,329 | 2.046 | 45,685 |
| Portugal | 6972 | 5.555 | 38,729 |
| Iraq | 12,824 | 2.9326 | 37,608 |
| Ecuador | 14,051 | 2.1549 | 30,278 |
| Ukraine | 18,680 | 1.4993 | 28,007 |
| Japan | 3460 | 8.0883 | 27,986 |
| Bulgaria | 7576 | 3.4177 | 25,892 |
| Greece | 4881 | 5.0721 | 24,757 |
| Ireland | 2248 | 10.4401 | 23,469 |
| Israel | 3356 | 6.8893 | 23,120 |
| Croatia | 3961 | 4.2779 | 16,945 |
| Slovenia | 2728 | 5.9609 | 16,261 |
| Philippines | 9248 | 1.7094 | 15,809 |
| Panama | 4022 | 3.9116 | 15,732 |
| Egypt | 7631 | 2.0471 | 15,621 |
| Kuwait | 936 | 16.1271 | 15,095 |
| China | 4634 | 2.7511 | 12,749 |
| Slovakia | 2250 | 5.6276 | 12,662 |
| Denmark | 1322 | 9.4138 | 12,445 |
| Bolivia | 9165 | 1.2826 | 11,755 |
| Oman | 1499 | 7.3887 | 11,076 |
| Morocco | 7425 | 1.4696 | 10,912 |
| Pakistan | 10,176 | 1.0175 | 10,354 |
| Kazakhstan | 2262 | 4.4891 | 10,154 |
| Tunisia | 4730 | 2.1219 | 10,037 |
| United Arab Emirates | 671 | 13.3859 | 8982 |
| Azerbaijan | 2670 | 3.2824 | 8764 |
| Bosnia and Herzegovina | 4086 | 2.0834 | 8513 |
| Lithuania | 1589 | 5.2701 | 8374 |
| Serbia | 3250 | 2.5652 | 8337 |
| Jordan | 3851 | 2.057 | 7922 |
| Australia | 909 | 8.6636 | 7875 |
| Algeria | 2756 | 2.7357 | 7540 |
| Guatemala | 4820 | 1.4399 | 6940 |
| Luxembourg | 501 | 13.7797 | 6904 |
| Macedonia | 2510 | 2.6246 | 6588 |
| Qatar | 245 | 26.4737 | 6486 |
| Dominican Republic | 2416 | 2.6004 | 6283 |
| Costa Rica | 2185 | 2.8501 | 6227 |
| Korea, Rep. | 917 | 6.655 | 6103 |
| Norway | 436 | 12.5081 | 5454 |
| Bangladesh | 7576 | 0.6809 | 5158 |
| Armenia | 2828 | 1.6764 | 4741 |
| Belarus | 1433 | 3.2351 | 4636 |
| Finland | 561 | 8.1444 | 4569 |
| Georgia | 2528 | 1.7853 | 4513 |
| Lebanon | 1479 | 2.629 | 3888 |
| Paraguay | 2262 | 1.6599 | 3755 |
| Venezuela | 1028 | 3.2285 | 3319 |
| Moldova | 3004 | 1.0318 | 3100 |
| Latvia | 644 | 4.7487 | 3058 |
| Honduras | 3141 | 0.9086 | 2854 |
| Bahrain | 352 | 7.3909 | 2602 |
| Albania | 1181 | 2.1626 | 2554 |
| Myanmar | 2697 | 0.9427 | 2542 |
| Malaysia | 474 | 5.0072 | 2373 |
| Montenegro | 682 | 3.1471 | 2146 |
| El Salvador | 1336 | 1.5752 | 2104 |
| Hong Kong | 148 | 11.0616 | 1637 |
| Nigeria | 1289 | 1.111 | 1432 |
| Malta | 219 | 6.3415 | 1389 |
| West Bank and Gaza | 1418 | 0.9691 | 1374 |
| Estonia | 234 | 5.4274 | 1270 |
| Sudan | 1468 | 0.7623 | 1119 |
| Kenya | 1681 | 0.5874 | 987 |
| Nepal | 1864 | 0.4774 | 890 |
| Kyrgyzstan | 1356 | 0.6325 | 858 |
| Afghanistan | 2211 | 0.3707 | 820 |
| Trinidad and Tobago | 127 | 6.1523 | 781 |
| Uzbekistan | 614 | 1.1858 | 728 |
| Cyprus | 119 | 6.0522 | 720 |
| Bahamas | 170 | 4.1998 | 714 |
| Uruguay | 181 | 3.8995 | 706 |
| Cuba | 146 | 4.3637 | 637 |
| Ethiopia | 1937 | 0.3102 | 601 |
| Jamaica | 303 | 1.6599 | 503 |
| Angola | 405 | 1.2364 | 501 |
| Sri Lanka | 208 | 2.1989 | 457 |
| Singapore | 29 | 15.554 | 451 |
| Equatorial Guinea | 86 | 5.1997 | 447 |
| Namibia | 208 | 1.9844 | 413 |
| Suriname | 122 | 3.1757 | 387 |
| Belize | 248 | 1.5334 | 380 |
| Yemen | 610 | 0.5203 | 317 |
| Zambia | 390 | 0.6963 | 272 |
| Cameroon | 448 | 0.5874 | 263 |
| Iceland | 29 | 9.0156 | 261 |
| Ghana | 335 | 0.7799 | 261 |
| Mauritania | 349 | 0.726 | 253 |
| Guyana | 164 | 1.441 | 236 |
| Gabon | 64 | 3.6091 | 231 |
| Thailand | 63 | 2.9667 | 187 |
| Senegal | 410 | 0.4554 | 187 |
| New Zealand | 25 | 6.9113 | 173 |
| Nicaragua | 165 | 0.9669 | 160 |
| Cabo Verde | 113 | 1.2078 | 136 |
| Congo, Rep. | 108 | 1.2078 | 130 |
| Bermuda | 10 | 12.5664 | 126 |
| Botswana | 42 | 2.9656 | 125 |
| Zimbabwe | 369 | 0.3267 | 121 |
| Maldives | 48 | 2.1945 | 105 |
| Mali | 269 | 0.3762 | 101 |
| Uganda | 265 | 0.3476 | 92 |
| Cote d'Ivoire | 138 | 0.6237 | 86 |
| Congo, Dem. Rep. | 591 | 0.1375 | 81 |
| Haiti | 236 | 0.3366 | 79 |
| Madagascar | 261 | 0.2695 | 70 |
| Tajikistan | 90 | 0.6611 | 59 |
| Brunei | 3 | 15.7025 | 47 |
| Chad | 104 | 0.4037 | 42 |
| Malawi | 191 | 0.2178 | 42 |
| Vietnam | 35 | 1.0934 | 38 |
| Mauritius | 10 | 3.8115 | 38 |
| Mozambique | 167 | 0.2233 | 37 |
| Gambia | 124 | 0.2959 | 37 |
| Lesotho | 51 | 0.6292 | 32 |
| Rwanda | 94 | 0.3289 | 31 |
| Burkina Faso | 85 | 0.3168 | 27 |
| Sierra Leone | 76 | 0.2981 | 23 |
| Antigua and Barbuda | 5 | 4.2592 | 21 |
| Barbados | 7 | 2.9843 | 21 |
| South Sudan | 63 | 0.3113 | 20 |
| Niger | 104 | 0.1815 | 19 |
| Guinea | 81 | 0.2145 | 17 |
| Togo | 68 | 0.2541 | 17 |
| Benin | 44 | 0.3916 | 17 |
| Guinea‐Bissau | 45 | 0.2772 | 12 |
| Liberia | 83 | 0.1375 | 11 |
| Sao Tome and Principe | 17 | 0.6215 | 11 |
| Tanzania | 21 | 0.5027 | 11 |
| St. Lucia | 5 | 2.0603 | 10 |
| Central African Republic | 63 | 0.1188 | 7 |
| Papua New Guinea | 9 | 0.5852 | 5 |
| Fiji | 2 | 1.6918 | 3 |
| Comoros | 10 | 0.2849 | 3 |
| Mongolia | 1 | 2.145 | 2 |
| Eritrea | 3 | 0.3619 | 1 |
| Burundi | 2 | 0.1397 | 0 |
| Bhutan | – | 1.4586 | – |
| Cambodia | – | 0.6314 | – |
| Dominica | – | 2.0075 | – |
| Grenada | – | 2.5025 | – |
| Laos | – | 1.0318 | – |
| Macao | – | 19.591 | – |
| Seychelles | – | 4.9071 | – |
| St. Kitts and Nevis | – | 4.6585 | – |
| St. Vincent Grenadines | – | 2.1197 | – |
| Timor‐Leste | – | 0.8701 | – |
| Marshall Islands | – | 1.0384 | – |
| Samoa | – | 1.0978 | – |
| Solomon Islands | – | 0.4191 | – |
| Vanuatu | – | 0.5984 | – |
| Kiribati | – | 0.8085 | – |
| Kosovo | – | 1.8865 | – |
| Micronesia | – | 0.7876 | – |
| Palau | – | 2.816 | – |
| Swaziland | – | 1.5796 | – |
| Tonga | – | 1.0681 | – |
| Turkmenistan | – | 3.0129 | – |
| Tuvalu | – | 1.2793 | – |
Note: VSL figures are based on Viscusi (2019), updated for inflation. Mortality figures are from Worldometer, January 1, 2021: https://web.archive.org/web/20210101203833/https://www.worldometers.info/coronavirus/.
TABLE A2.
Data sources for regressions
| COVID deaths data: | Worldometer, coronavirus update (September 26, 2020), https://web.archive.org/web/20200927003841/ https://www.worldometers.info/coronavirus/ |
|---|---|
| Value of a statistical life: | Viscusi, W. K. (2019). Risk guideposts for a safer society: Introduction and overview. Journal of Risk and Uncertainty, 58(2–3), 101–119. |
| Population density & urban share: |
Worldometer, Countries in the World by Population (September 26, 2020), https://web.archive.org/web/20200929130113/https://www.worldometers.info/world‐population/population‐by‐country/ (Urban share data come from the United Nations Population estimates and is the de facto population living in areas classified as urban according to the criteria used by each country divided by the country's total population. Population density is the number of people per square kilometer). |
| GDP‐quarterly percentage change: | OECD, Quarterly Data (September 26, 2020), https://data.oecd.org/gdp/quarterly‐gdp.htm. (Real GDP data as a percentage change from the previous quarter. Includes 47 countries for both Q1 and Q2 GDP data and not limited to just OECD countries. Some GDP data are provisional or an estimate as of the time of reporting. For countries without GDP data, their GDP values are set to zero and an indicator variable is included as “Missing GDP data”). |
| Percent Age 65+: |
United Nations, World Population Prospects 2019, https://population.un. org/wpp/Download/Standard/Population/ (download table: Population by Age Groups – Both Sexes). |
| Economic freedom index: |
Heritage Foundation, 2020 Index of Economic Freedom Country Rankings, https://www.heritage.org/index/ranking (Each country is assigned to a quartile based on their relative rank in the Heritage Foundation's Economic Freedom Index. Results are relative to countries in the lowest quartile, the omitted category.) |
| Health Rank: | Tandon, A. et al., Measuring Overall Health System Performance for 191 Countries. World Health Organization, GPE Discussion Paper Series: No. 30, 18–21. (Each country is assigned to a quartile based on their relative rank of overall health efficiency. Results are relative to countries in the lowest health quartile, the omitted category.) |
Viscusi WK. Economic lessons for COVID‐19 pandemic policies. South Econ J. 2021;87:1064–1089. 10.1002/soej.12492
This article is based on the author's Southern Economic Association Presidential Address on November 22, 2020. Scott Jeffrey provided excellent research assistance.
Footnotes
Unless indicated otherwise, all mortality figures are from Table A1 for January 1, 2021.
The mortality cost of the pandemic serves as a central benefit component in benefit‐cost assessments of COVID‐19 policies, such as that in Thunström et al. (2020).
Viscusi (2020) provides details regarding data sources and the construction of this estimate.
The death counts by age reflect deaths in the United States from February 1, 2020, to September 26, 2020, updated on September 30. Centers for Disease Control 2020: https://data.cdc.gov/NCHS/Provisional-COVID-19-Death-Counts-vy-Sex-Age-andS/9bhg-hcku.
See McGrath (2020).
See Churchill's comments in Span (2020).
See Farrell et al. (2020).
For a COVID‐19 example of rationing based on the chance of survival, see Meeks and Maxouris (2021). Also see Grace Houck, “‘Care Now Has to Be Rationed:’ Los Angeles COVID‐19 Spike Is Crushing Hospitals,” USA Today, January 5, 2021.
Among the analyses in which I use this format is that in Viscusi (1997), which considers the public's response to multiple, conflicting risk communication efforts.
See Jones (2020).
See Cameron (2021).
REFERENCES
- Adler, M.D. (2020) What should we spend to save lives in a pandemic: A critique of the value of statistical life. Center for Economic Policy Research, COVID‐19 Economics, 33, 1–45. [Google Scholar]
- Blomquist, G. , Dickie, M. & O'Conor, R.M. (2011) Willingness‐to‐pay for improving fatality risks and asthma symptoms: Values for children and adults of all ages. Resource and Energy Economics, 33(2), 410–425. [Google Scholar]
- Broughel, J. & Viscusi, W.K. (2021) The mortality cost of expenditures. Contemporary Economic Policy, 39(1), 156–167. [Google Scholar]
- Bruine de Bruin, W. , Saw, H.W. & Goldman, D. (2020) Political polarization in US residents' COVID‐19 responses, policy preferences, and protective behaviors. Journal of Risk and Uncertainty, 61(2), 177–194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cameron, C . (2021). Biden official predicts a toll of 500,000 before March. New York Times, January 18, 2021. https://www.nytimes.com/2021/01/17/world/Covid-deaths-Biden.html.
- Centers for Disease Control . (2020). Provisional COVID‐19 death counts by sex, age, and state. https://data.cdc.gov/NCHS/Provisional-COVID-19-Death-Counts-by-Sex-Age-and-S/9bhg-hcku . Accessed January 21, 2021.
- Farrell, T.W. , Ferrante, L.E. , Brown, T. , Francis, L. , Widera, E. , Rhodes, R. , et al. (2020) AGS position statement: Resource allocation strategies and age‐related considerations in the COVID‐19 era and beyond. Journal of the American Geriatrics Society, 68, 1136–1138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gentry, E.P. & Viscusi, W.K. (2016) The fatality and morbidity component of the value of a statistical life. Journal of Health Economics, 46(2), 90–99. [DOI] [PubMed] [Google Scholar]
- Goodnough, A. & Hoffman, J . (2020) The elderly vs. essential workers: who should get the coronavirus vaccine first? New York Times, December 6, 2020. https://www.nytimes.com/2020/12/05/health/covid-vaccine-first.html. Accessed January 21, 2021.
- Hammitt, J.K. (2020) Valuing the mortality risk in the time of COVID‐19. Journal of Risk and Uncertainty, 61(2), 129–154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones, J . (2020). NY governor on conservatives who want to end social distancing: life is not ‘disposable.’ Huffington Post. https://www.huffpost.com/entry/andrew-cuomo-trump-social-distancing-coronavirus_n_5e7a4a27c5b62f90bc525564. Accessed January 22, 2021.
- Kniesner, T.J. & Sullivan, R. (2020) The forgotten numbers: A closer look at COVID‐19 non‐fatal valuations. Journal of Risk and Uncertainty, 61(2), 155–176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Masterman, C.J. & Viscusi, W.K. (2018) The income elasticity of global values of a statistical life: Stated preference evidence. Journal of Benefit‐Cost Analysis, 9(3), 407–434. [Google Scholar]
- McGrath, C. (2020) Italian hospital makes heartbreaking decision not to intubate anyone over the age of 60. Express, March 20, 2020. https://www.express.co.uk/news/world/1257852/Italy-coronavirus-intubating-elderly-pandemic-china-hospitals-Nadine-Dorries. Accessed January 21, 2021.
- Meeks, A. , & Maxouris, C . (2021) ‘Human disaster’ unfolding in LA will get worse, experts say. CNN News, January 5, 2021. https://www.cnn.com/2021/01/05/us/los-angeles-county-california-human-disaster-covid/index.html . .
- Miller, F.G . (2020) Why I support age‐related rationing of ventilators for COVID‐19 patients. The Hastings Center, April 9, 2020. https://www.thehastingscenter.org/why-i-support-age-related-rationing-of-ventilators-for-covid-19-patients/. Accessed January 21, 2021.
- O'Conor, R.M. & Blomquist, G. (1997) Measurement of consumer‐patient preferences using a hybrid contingent valuation method. Journal of Health Economics, 19(6), 667–683. [DOI] [PubMed] [Google Scholar]
- Pike, J. , Shogren, J.F. , Adland, D. , Viscusi, W.K. , Finnoff, D. , Skiba, A. , et al. (2020) Waking up to the reality of a pandemic. EcoHealth, 17(2), 217–221. 10.1007/s10393-020-01479-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schmidt, H. , Gostin, L.O. & Williams, M.A. (2020) Is it lawful and ethical to prioritize racial minorities for COVID‐19 vaccines? Journal of the American Medical Association, 324(20), 2023–2024. [DOI] [PubMed] [Google Scholar]
- Span, P . (2020) Should youth come first in coronavirus care? New York Times, July 31, 2020. https://www.nytimes.com/2020/07/31/health/coronavirus-ethics-rationing-elderly.html. Accessed January 21, 2021.
- Stokes, E.K. , Zamrano, L.D. , Anderson, K.N. , Marder, E.P. , Raz, K.M. , Felix, S.E.B. , et al. (2020) Coronavirus disease 2019 case surveillance—United States, Jan. 22–May 30, 2020. Morbidity and Mortality Weekly Report, 69, 759–765. 10.15585/mmwr.mm6924e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thunström, L. , Newbold, S.C. , Finnoff, D.C. , Ashworth, M. & Shogren, J.F. (2020) The benefits and cost of flattening the curve for COVID‐19. Journal of Benefit‐Cost Analysis, 11(2), 179–195. [Google Scholar]
- U.S. Department of Health and Human Services, Office for Civil Rights . (2020) Action, bulletin: Civil rights, HIPAA, and the coronavirus disease 2019 (COVID‐19), March 28, 2020. https://www.hhs.gov/sites/default/files/ocr-bulletin-3-28-20.pdf.
- Viscusi, W.K. (1994) Mortality effects of regulatory costs and policy evaluation criteria. RAND Journal of Economics, 25(1), 94–109. [Google Scholar]
- Viscusi, W.K. (1997) Alarmist decisions with divergent information. Economic Journal, 107(445), 1657–1670. [Google Scholar]
- Viscusi, W.K. (2010) Policy challenges of the heterogeneity of the value of a statistical life. Foundations and Trends in Microeconomics, 6(2), 99–172. [Google Scholar]
- Viscusi, W.K. (2018) Pricing lives: guideposts for a safer society. Princeton: Princeton University Press. [Google Scholar]
- Viscusi, W.K. (2020) Pricing the global health risks of the COVID‐19 pandemic. Journal of Risk and Uncertainty, 61(1), 101–128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Viscusi, W.K. , Magat, W.A. & Huber, J. (1991) Pricing environmental health risks: survey assessments of risk‐risk and risk‐dollar trade‐offs for chronic bronchitis. Journal of Environmental Economics and Management, 21(1), 32–51. [Google Scholar]
- Viscusi, W.K. & Masterman, C.J. (2017) Income elasticities and global values of a statistical life. Journal of Benefit‐Cost Analysis, 8(2), 226–250. [Google Scholar]
- Viscusi, W.K. & Zeckhauser, R.J. (2005) Recollection bias and the combat of terrorism. The Journal of Legal Studies, 34(1), 27–55. [Google Scholar]
- Worldometer . (2021). COVID‐19 Coronavirus Pandemic. https://www.worldometers.info/coronavirus/.


