Abstract
Background and purpose
The global COVID‐19 pandemic led many stroke centres worldwide to shift from in‐person to telemedicine consultations to assess patients with transient ischaemic attacks (TIAs). We aimed to investigate the impact of telemedicine during the COVID‐19 pandemic on the management and outcome of the patients with TIA.
Methods
We retrospectively analysed data from a registry of consecutive TIA patients assessed at the Stroke Department, Imperial College Health Care Trust, London, during the national lockdown period (between March 23 2020 and 30 June 2020). As controls, we evaluated the clinical reports and stroke quality metrics of patients presenting to the TIA clinic in the same period of 2019.
Results
Between 23 March 2020 and 30 June 2020, 136 patients were assessed using the telemedicine TIA clinic, compared to 180 patients evaluated with face‐to‐face consultation in the same period in 2019. Patients’ characteristics were similar in both groups. At 3 months after the TIA, there were no significant differences in the proportion of patients admitted to the hospital for recurrent TIA/stroke or any other cardiovascular cause from the 2020 period compared to the same period in 2019.
Conclusions
Our analysis showed that during the pandemic, our telemedicine consultations of TIA patients were not associated with an increased 3‐month rate of recurrent TIA/stroke or cardiovascular hospital admissions. More robust studies looking at this model of care will be needed to assess its long‐term effects on patients and health care systems.
Keywords: COVID‐19, telehealth, telemedicine, transient ischaemic attack
Abbreviations
- HASU
Hyperacute Stroke Unit
- NHS
National Health Service
- SSNAP
Sentinel Stroke National Audit Programme
- TIA
transient ischaemic attach
INTRODUCTION
During the global COVID‐19 pandemic, social distancing measures have been established, with the United Kingdom public being placed on lockdown from 23 March 2020 throughout June 2020 to avoid transmission of the disease. Physical attendance at outpatient clinics was discouraged in view of the risk of spreading COVID‐19, and as a result, shifts from in‐person to telemedicine or telehealth have occurred in many stroke centres worldwide to manage patients with transient ischemic attacks (TIAs) [1]. The National Health Service (NHS) and the British Association of Stroke Physicians in the United Kingdom have released new information for governance guidance for the use of telemedicine [2, 3]. However, to date, there is lack of data regarding the impact of telemedicine on the management and outcome of patients with TIAs.
The objective of this study was to assess the effects of telemedicine for patients with TIAs during the COVID‐19 pandemic on the 3‐month outcome in terms of rate of hospital admissions for recurrent TIA/stroke, any cardiovascular cause, or any nonvascular cause as compared with rates of the same period in 2019.
METHODS
This was an observational, retrospective, single‐centre study based on data of consecutive patients evaluated in the rapid outpatient TIA service of the Stroke Department, Charing Cross Hospital, Imperial College Health Care Trust, London between 23 March 2019 and 30 June 2019 and between 23 March 2020 and 30 June 2020. The Stroke Department at Charing Cross Hospital is a comprehensive tertiary stroke centre and is North West London’s (UK) regional lead referral stroke centre for mechanical thrombectomy for a population of over 2.4 million people.
This TIA service is the referral centre for TIA for the population of the boroughs of Hammersmith and Fulham, West Kensington, Hounslow, part of Ealing and Chelsea, and Westminster. The population of our catchment area includes over 700,000 residents. On average, over 900 face‐to‐face consultations are held annually in the rapid outpatient TIA service at the Charing Cross Hospital. Since the onset of the pandemic, in keeping with hospital policy, our team of stroke consultants agreed to perform remote consultations for the TIA patients and to set a target of reducing face‐to‐face clinics to 5% of the all‐outpatient attendance. We analysed the management and 3‐month outcome of the patients evaluated in our rapid outpatient TIA service between 23 March 2020 and 30 June 2020 with telemedicine. As controls, we considered the sample of patients presenting with TIA in the same period of 2019 assessed with face‐to‐face consultations.
Data source and data collection process
Consecutive enrolment of eligible patients was ensured by using a routinely collected database of TIA clinic attendees used for reporting metrics to our local clinical commissioning group and for our annual stroke‐unit assessment. Electronic medical records of eligible patients were retrieved from the Imperial College Healthcare NHS Trust online medical notes system. Data of consecutive patients were extracted using a prespecified case report file that encompassed patient characteristics including age, vascular risk factors, and relevant medical history that were recorded during the admission. Events were captured by review of medical notes of all patients admitted to the Hyperacute Stroke Unit (HASU) and referred to the rapid outpatient TIA service of the Imperial College Healthcare NHS Trust between 23 March 2020 and 30 June 2020, and between 23 March 2019 and 30 June 2019.
This study is exempt from ethical committee approval, as decided by the Department of Stroke Medicine, Imperial College Healthcare NHS Trust. This health service evaluation is exempt because all clinical data were extracted from a routinely collected source as part of an ongoing national audit program (Sentinel Stroke National Audit Programme [SSNAP]; www.strokeaudit.org). No new intervention was used or tested. Informed consent was not a legal requirement, because the research was carried out using data collected as part of routine care, and any researchers outside the direct care team only had access to anonymised data.
We evaluated the rate of hospital admission for recurrent stroke/TIA, cardiovascular, and any nonvascular cause at 3 months. Follow‐up information on occurrence of these events was obtained by stroke physicians in the follow‐up clinics during face‐to‐face interviews or by nurses through telephone calls. If the patient could not be contacted, a close relative or their family doctor was interviewed. Patients were informed that they might receive a telephone call.
Hospital admission for recurrent stroke/TIA, cardiovascular, and any nonvascular cause were also identified by overlapping methods of hot and cold pursuit [4]. These events were reviewed by an independent stroke physician who was blind to the phase of the study in which the event occurred and who decided which events were definite recurrent stroke/TIA.
Definition of study variables
Ischaemic stroke was defined as an episode of neurological dysfunction caused by focal cerebral, spinal, or retinal infarction [5]. TIA was defined as a brief episode of neurological dysfunction caused by focal brain or retinal ischaemia, with clinical symptoms typically lasting <1 hour, and without evidence of acute infarction [6]. TIA mimics included migraine aura, seizures, syncope, peripheral vestibular disturbance, transient global amnesia, functional/anxiety disorder, amyloid spells, subarachnoid haemorrhage, structural brain lesion, and paroxysmal symptoms due to demyelination [7]. Data on known stroke risk factors were collected as follows: age, sex, history of hypertension (blood pressure >140/90 mm Hg at least twice before acute stroke or if already under treatment with antihypertensive drugs), history of diabetes mellitus (a random venous plasma glucose concentration of >11.1 mmol/L or a fasting plasma glucose concentration of >7.0 mmol/L or 2‐h plasma glucose concentration of >11.1 mmol/L 2 h after 75 g anhydrous glucose in an oral glucose tolerance test, or haemoglobin A1c of >48 mmol/mol or under antidiabetic treatment), history of dementia, history of symptomatic ischaemic heart disease (myocardial infarction, history of angina or previous diagnosis of multiple lesions on thallium heart isotope scan or evidence of coronary disease on coronary angiography), previous stroke/TIA.
Brief description of the workflow
Local general practitioners in primary care or emergency departments can refer any patient they suspect had a TIA, but whom they did not consider required immediate hospital admission, to our rapid outpatient TIA service. These patients or the caregiver at home are then contacted by our team to arrange a clinic appointment within 24 h of referral received. Our TIA clinic is organised to provide a standardised assessment to all our patients. On the same day, blood tests, electrocardiography, brain imaging (usually computed tomography), and carotid ultrasound imaging are obtained. Because of the COVID‐19 pandemic, stroke physicians performed telephone consultations for the TIA patients rather than the usual clinical face‐to‐face assessment. During these virtual consultations, stroke physicians collected the patient's clinical history and reviewed remotely the results of the investigations. Patients were discharged home immediately after the assessment, unless the treating physician believed the patient required urgent admission to our HASU.
Study outcomes and statistical analysis
Continuous variables are presented as mean with standard deviation if values are normally distributed or as median with interquartile range when they do not follow the normal distribution. We compared the distribution of continuous variables between groups with a t test or Wilcoxon rank sum test as appropriate, whereas categorical values were compared with χ2 tests. Statistical significance was set at 0.05. All analyses were conducted with Stata 15.1 (StataCorp).
RESULTS
Between the 23 March 2019 and 30 June 2019, 180 patients were evaluated in our rapid TIA outpatient service with face‐to‐face consultation, whereas 136 patients were assessed in the same period in 2020 with telemedicine. Patients’ characteristics were similar in both groups, apart from less dementia in the 2020 cohort (p = 0.027) (Table 1). During the COVID‐19 period, 55.15% of the patients evaluated with a remote consultation had a final diagnosis of TIA, whereas it was 46.11% during the same period of 2019. Of note, the percentage of patients with a final diagnosis of a TIA mimic dropped from 48.89% to 35.29% during the COVID‐19 period compared to the 2019 period. The rate of ischaemic stroke diagnosed through the TIA clinic also doubled from 5% to 9.56% from 2019 to the 2020 period.
TABLE 1.
Baseline characteristics of the patients evaluated in the rapid outpatient TIA service during the two study periods
| 23 March to 30 June 2020, n = 136 | 23 March to 30 June 2019, n = 180 | p | |
|---|---|---|---|
| Demographics | |||
| Age, years, median, IQR | 65, 23–96 | 68.5, 20–28 | 0.087 |
| Male, sex, n (%) | 99 (72.79%) | 121 (67.22%) | 0.227 |
| Clinical characteristics | |||
| Hypertension, n (%) | 71 (52.21%) | 95 (52.78%) | 0.442 |
| Diabetes mellitus, n (%) | 27 (19.85%) | 37 (20.56%) | 0.645 |
| Hypercholesterolemia, n (%) | 65 (47.79%) | 76 (42.22%) | 0.638 |
| Coronary artery disease, n (%) | 19 (13.97%) | 21 (11.67%) | 0.695 |
| Previous TIA/stroke, n (%) | 23 (16.91%) | 39 (21.67%) | 0.186 |
| Carotid stenosis, n (%) | 3 (2.21%) | 9 (5.0%) | 0.164 |
| AF, n (%) | 15 (11.03%) | 25 (13.89%) | 0.334 |
| Dementia, n (%) | 6 (4.41%) | 18 (10%) | 0.027 |
| ABCD2 score, median, IQR | 3, 0–6 | 3, 0–6 | 0.929 |
| Symptom onset to first medical review time, days, median, IQR | 3, 0–90 | 0, 0–133 | 0.002 |
| Final diagnosis | |||
| TIA, n (%) | 75 (55.15%) | 83 (46.11%) | |
| Ischaemic stroke, n (%) | 13 (9.56%) | 9 (5.0%) | |
| TIA mimic, n (%) | 48 (35.29%) | 88 (48.89%) | 0.020 |
Abbreviations: ABCD2, age ≥ 60 years, BP ≥ 140/90 mmHg, clinical features of the TIA, duration of symptoms, history of diabetes; AF, atrial fibrillation; IQR, interquartile range; TIA, transient ischaemic attack.
Table 2 and Figure 1 show all of the causes of hospital admission during the 3‐month follow‐up after the TIA. There were no significant differences in the proportion of patients admitted in the hospital for recurrent TIA/stroke (p = 0.445) and for cardiovascular cause (p = 0.367) between the COVID‐19 period and the same period in 2019. However, a significantly lower proportion of patients were admitted to the hospital for any nonvascular cause during the COVID‐19 period compared to the same period of 2019 (p = 0.048).
TABLE 2.
All‐cause hospital admission during the 3‐month follow‐up
| 23 March to 30 June 2020, n = 136 | 23 March to 30 June 2019, n = 180 | p | |
|---|---|---|---|
| Admission to hospital for recurrent TIA/stroke, n (%) | 2 (1.47%) | 3 (1.67%) | 0.445 |
| Cardiovascular admission to hospital, n (%) | 1 (0.74%) | 2 (1.11%) | 0.367 |
| Nonvascular admission to hospital, n (%) | 4 (2.94%) | 13 (7.22%) | 0.048 |
Abbreviation: TIA, transient ischaemic attack.
FIGURE 1.
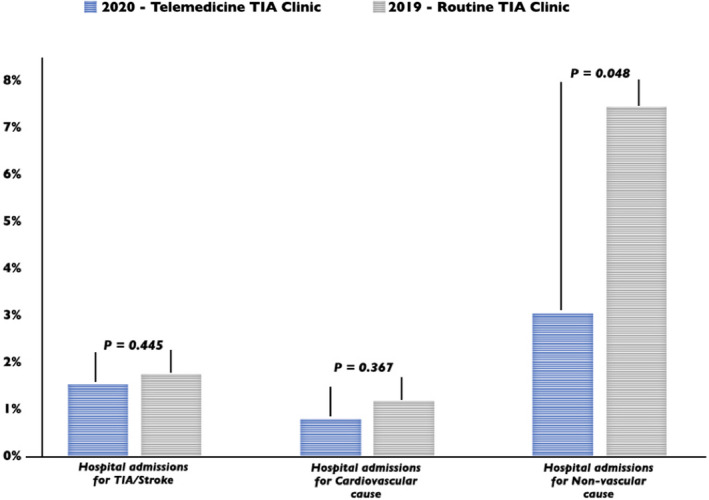
Rate of all‐cause hospital admission during the 3‐month follow‐up. TIA, transient ischaemic attack [Colour figure can be viewed at wileyonlinelibrary.com]
DISCUSSION
Our analysis showed that during the pandemic, our telemedicine TIA clinic was not associated with an increased rate of recurrent TIA/stroke and cardiovascular hospital admissions up to the 3‐month follow‐up. Therefore, the virtual TIA clinic may provide a means to treat patients remotely using agreed‐upon protocols [2, 3] as it was shown to be noninferior to the routine face‐to‐face encounter in our two assessment periods.
It was interesting to note that hospital admissions for nonvascular causes were reduced in the 2020 cohort compared to 2019. This may be related to patient reluctance to attend hospitals during the pandemic. Another interesting finding of our analysis was that our ambulatory rapid access TIA clinic registered a marked decrease in mimic diagnoses during the pandemic. This is in keeping with the hypothesis that patients, especially those with milder symptoms, may have intentionally avoided hospitals during the COVID‐19 pandemic.
The general terms for non–face‐to‐face care services are telehealth or telemedicine, from the Greek word for “far.” Remote or non–face‐to‐face care models, in which patients are geographically separated from the physicians, have existed for decades, but the COVID‐19 crisis stimulated policy makers, regulators, and physicians to expand the use of remote health care. As the global pandemic will have a lasting effect on society, neurologists should consider incorporating telehealth into their practice. The utilization of telemedicine requires an authentic patient engagement and different communication strategies from the physicians [8]. Moreover, workflow and staff functions need to adapt to ensure that this model can improve patient care at lower costs. It is worth noting that physicians may not be comfortable performing virtual consultations for all patients due to lack of physical examination, and this will need to be taken into account when developing services.
In conclusion, despite the fact that TIA virtual clinics have an important role in the current COVID‐19 pandemic, due to the possibility to provide ongoing care in an otherwise challenging setting, more robust studies looking at this model of care will be needed to assess its long‐term effects on patients and health care systems.
CONFLICT OF INTEREST
The authors declare no financial or other conflicts of interest.
AUTHOR CONTRIBUTIONS
Lucio D'Anna: Conceptualization (equal); data curation (equal); formal analysis (equal); funding acquisition (equal); investigation (equal); methodology (equal); project administration (equal); resources (equal); software (equal); supervision (equal); validation (equal); visualization (equal); writing–original draft (equal); writing–review & editing (equal). Natalya Ellis: Data curation (equal). Harri Jenkins, Paul Bentley, Zoe Brown, Omid Halse, Sohaa Jamil, Abid Malik, Dheeraj Kalladka, Joseph Kwan, Marius Venter, Soma Banerjee: Data curation (equal); writing–review & editing (equal).
ACKNOWLEDGEMENTS
The authors would like to thank the following healthcare staff for their contributions: Tsering Dolkar and Siji Joy (stroke clinical nurse specialists), and Riann Kruger and Brooke Hall (data analysts for SSNAP).
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.
REFERENCES
- 1. Furlanis G, Ajčević M, Naccarato M, et al. e‐Health vs COVID‐19: home patient telemonitoring to maintain TIA continuum of care. Neurol Sci. 2020;41:2023‐2024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. NHS England . Clinical guide for the management of stroke patients during the coronavirus pandemic; 2020.
- 3. Ford GA, Hargroves D, Lowe D, Harston G, Rooney G, Oatley H, Lough J.Developing virtual clinics for managing TIA and minor stroke during the COVID‐19 pandemic; 2020.
- 4. Coull AJ, Silver LE, Bull LM, Giles MF, Rothwell PM. Direct assessment of completeness of ascertainment in a stroke incidence study. Stroke. 2004;35(9):2041‐2045. 10.1161/01.STR.0000137605.48864.2f [DOI] [PubMed] [Google Scholar]
- 5. Sacco RL, Kasner SE, Broderick JP, et al. An updated definition of stroke for the 21st century. Stroke. 2013;44(7):2064‐2089. 10.1161/str.0b013e318296aeca [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Easton JD, Saver JL, Albers GW, et al. Definition and evaluation of transient ischemic attack. Stroke. 2009;40(6):2276‐2293. 10.1161/strokeaha.108.192218 [DOI] [PubMed] [Google Scholar]
- 7. Nadarajan V, Perry RJ, Johnson J, Werring DJ. Transient ischaemic attacks: Mimics and chameleons. Pract Neurol. 2014;14(1):23‐3;. 10.1136/practneurol-2013-000782 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Klein BC, Busis NA. COVID‐19 is catalyzing the adoption of teleneurology. Neurology. 2020;94(21):903‐904. 10.1212/WNL.0000000000009494 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.


