Abstract
Objective
Describe a systematic approach to address advance care planning (ACP) during a COVID‐19 outbreak and its impact on the incidence of new do‐not‐hospitalize (DNH) directives among long‐term care (LTC) residents.
Design
Prospective quality improvement initiative.
Setting
Two long‐term chronic care campuses within a large academic healthcare organization.
Participants
LTC residents with activated healthcare proxies who lacked DNH directives based on documentation in the electronic medical record (EMR) as of April 13, 2020.
Intervention
Using a structured discussion guide, trained healthcare staff from various disciplines contacted the residents' proxies to conduct COVID‐19 focused ACP discussions. Residents without DNH directives with COVID‐19 were prioritized. Preferences ascertained in the discussion were communicated to the residents' primary care teams and directives were updated in the EMR accordingly.
Measurements
Residents who acquired a new DNH directive during the study initiative were determined using the EMR. Subsequent changes in DNH orders, hospitalizations, and deaths were ascertained by retrospective chart review from the date of new DNH through August 5, 2020.
Results
At baseline, 315/581 (54%) of LTC residents did not have a DNH directive. Their mean age was 87 (±9) years and 70% were female. Following ACP discussions, 124/315 (39%) of residents acquired a new DNH directive. Among residents with new DNH directives, 65/124 (52%) were diagnosed with COVID‐19 from April 2, 2020 to May 21, 2020. During follow‐up, only 6/124 (4.8%) residents had their DNH order reversed, 2/124 (1.6%) residents were hospitalized with illnesses unrelated to COVID‐19, and 29/124 (23%) died.
Conclusions
There was substantial opportunity to increase the proportion of LTC residents with DNH orders during the COVID‐19 pandemic through a systematic ACP initiative which utilized real‐time EMR data. New directives to avoid hospitalizations were sustained among the majority of residents beyond the peak of the pandemic.
Keywords: advance care planning, COVID‐19, nursing home, long‐term care
Key Point
We describe the development and implementation of a COVID‐19 advance care planning initiative that was rapidly established to promote goal‐concordant care.
Why Does this Paper Matter?
This model highlights the importance of identifying a facility champion and promoting stakeholder engagement in implementation of LTC initiatives.
1. INTRODUCTION
COVID‐19 has disproportionally affected nursing homes (NHs), accounting for 8% of cases and 41% of deaths in the United States. 1 This is attributable to the congregate housing setting in NHs which increases risk for rapid spread, as well as the vulnerability of long‐term care (LTC) residents to severe illness. 2 Mortality from COVID‐19 in LTC residents is staggering with estimates between 34% and 48%, including those who are hospitalized. 3 , 4 Hospitalization may not be clinically beneficial or concordant with the preferences of frail, LTC residents, especially when the goal of care is comfort.
Advance care planning (ACP) discussions promote care that is aligned with the preferences of LTC residents. These discussions result in enhanced quality and patient satisfaction with end‐of‐life care. 5 , 6 Given the vulnerability of LTC residents during the COVID‐19 pandemic, it is crucial to conduct efficient, compassionate ACP discussions to ensure their treatment is aligned with their goals of care. 7
We describe the structure and implementation of an ACP “SWAT Team” that used real‐time data from the electronic medical record (EMR) in a large healthcare organization to rapidly prioritize ACP discussions in LTC residents who were most vulnerable to hospitalization during the peak of the COVID‐19 pandemic. The objective of this study is to describe this initiative, and its impact on the incidence of new do‐not‐hospitalize (DNH) directives and subsequent changes in DNH orders, hospitalization, and death following the peak of the pandemic.
2. METHODS
2.1. Palliative care initiative
The first known case of COVID‐19 among Hebrew SeniorLife (HSL) LTC residents was on March 31, 2020 and brought to light the urgent need to re‐address ACP among the most vulnerable residents to ensure they received goal‐concordant care (Figure 1). The capacity to rapidly conduct ACP discussions exceeded the capacity of the usual clinical palliative care providers. Thus, allied health professionals from the HSL community were rapidly recruited and established as the ACP SWAT Team, comprised of a speech‐language pathologist, a chaplain, a nurse practitioner, and a social worker. Each member contributed 30–40 h per week and was either recruited from retirement or redeployed from a primary role in which duties were restricted due to COVID‐19 (e.g., speech therapy).
FIGURE 1.
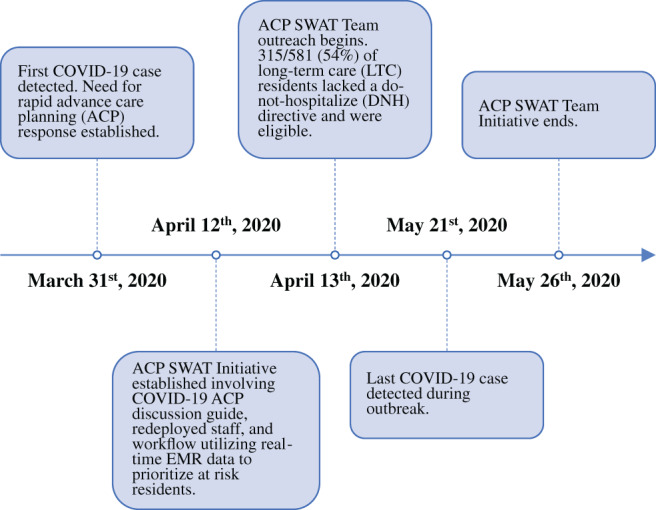
Timeline of advance care planning SWAT Team initiative
The Champion of this initiative, the Director of Palliative Care Services, was responsible for training the SWAT Team members and creating an ACP toolkit which included a structured COVID‐19 ACP discussion framework adapted from the Center toVitalTalk/VitalTalk/Respecting Choices/Ariadne Labs (Supplementary Text S1), as well as a protocol for the team's workflow. The discussion guide was designed as a framework to facilitate ACP discussions in the setting of a COVID‐19 outbreak. Compassionate language was emphasized in the guide given the challenges of these conversations. A 1‐h training session was delivered virtually and followed by 1:1 coaching with the Director of Palliative Care Services, as needed.
The SWAT Team workflow was enabled by HSL's Informatics Department and Marcus Institute for Aging Research. Every morning between April 13, 2020 and May 26, 2020 at 8:00 a.m., an automated email was sent to the team with an updated spreadsheet listing residents without DNH orders and the following information: date of last COVID‐19 test and status, unit location, healthcare proxy name and contact number, and cognitive function (i.e., surrogate for decisional capacity). The SWAT Team then called proxies to conduct a COVID‐19 focused ACP discussion, prioritizing residents with a positive COVID‐19 test. If the proxy was not available on the first call, two subsequent attempts were made. Each SWAT Team member conducted 3–7 ACP discussions per day. To track efforts, the emailed spreadsheet was linked to a Research Electronic Data Capture 8 , 9 form on which the SWAT Team could document the results of the telephone call (i.e., decided on DNH directive, decided against DNH, undecided, or could not contact). If a decision was made to initiate a DNH directive, the SWAT Team member called or emailed the resident's primary care provider so that they could write the order.
2.2. Study population and characteristics
This project was approved by the HSL Institutional Review Board. The population was drawn from LTC residents (N = 581) living in two campuses of HSL, the largest non‐profit provider of senior housing in Boston, MA. HSL employs a robust EMR (Meditech) that includes separate fields documenting individual advance directives orders (e.g., do‐not‐resuscitate [DNR], DNH) and the dates the orders were initiated. Residents without a DNH order and with an activated healthcare proxy on April 13, 2020 were identified by EMR and included (n = 315). We only targeted residents with activated healthcare proxies because the SWAT Team was not providing direct on‐site care to the residents, and thus could only conduct ACP discussions by telephone.
Other resident characteristics that were extracted from the EMR for purposes of operationalizing the initiative and describing the cohort included: the name and contact number of their healthcare proxy, testing for SARS CoV‐2 (date and status), hospital transfers, vital status, DNR order status, age, race, and gender. In addition, cognitive impairment was determined using the C1000 scale from the Minimum Data Set (MDS) 10 immediately preceding the start of the ACP initiative, which is based on staff report of moderate–severe impairment in daily decision making. Functional characteristics were measured using the activities of daily living scale from the MDS.
2.3. Follow‐up
A retrospective chart review of residents with a reversal of DNH directive or a hospitalization through August 5, 2020 was conducted (Michelle J. Berning). Circumstances of the DNH reversal or hospitalization were gleaned from provider and nursing notes.
2.4. Analysis
Characteristics were described using proportions for categorical variables and means with standard deviations for continuous variables. The outcome of interest was the proportion of residents who acquired a DNH order. Among residents who acquired a DNH, the proportion who had the DNH reversed, were hospitalized, or who died in the follow‐up period was calculated. Resident characteristics and hospitalization rates were also described among residents with a COVID‐19 diagnosis and DNH directive either before the study period or during the study period. Descriptive statistics were computed using R version 3.6.0. 11
3. RESULTS
On April 13, 2020, 315/581 (54%) of LTC residents lacked a DNH directive. Among these 315 residents, the mean age was 87 (±9) years, 219 (70%) were female, 103 (33%) had moderate–severe cognitive impairment, and 76 (24%) had a DNR directive. During the 6‐week study period, the SWAT Team contacted an estimated 75% of resident proxies, and the remaining residents were contacted by primary care teams. Each outreach, which included preparation, call to the proxy, and subsequent documentation, took approximately 1 h to complete. A total of 124/315 (39%) of residents acquired a DNH directive between April 13, 2020 and May 26, 2020.
Among all 124 residents who acquired a DNH directive, 65 (52%) were diagnosed with COVID‐19, 2 (1.6%) were hospitalized for non‐COVID related conditions (aspiration pneumonia with urinary retention, and rectal bleeding), and 29 (23%) died during follow‐up (Table 1). Among 65 residents with a new DNH and a COVID‐19 diagnosis, only 15 residents acquired the DNH directive before the COVID‐19 diagnosis, whereas 50 acquired the DNH directive after the diagnosis.
TABLE 1.
Characteristics of residents who acquired new do‐not‐hospitalize (DNH) directives by COVID‐19 status
| All residents who acquired new DNH directives (n = 124) | COVID‐19 diagnosis (n = 65) | No COVID‐19 diagnosis (n = 59) | |
|---|---|---|---|
| Age, years | 88 (9) | 87 (10) | 89 (9) |
| Female sex | 81 (65%) | 38 (58%) | 43 (73%) |
| Caucasian | 113 (91%) | 56 (86%) | 57 (97%) |
| Cognitive impairment a | 54 (44%) | 32 (49%) | 22 (37%) |
| Activities of daily living score b | 15 (7) | 16 (7) | 14 (6) |
Note: Statistics presented: mean (SD); n (%).
Cognitive impairment defined as moderate to severe decisional impairment as described by nursing staff.
Katz activities of daily living score, range 0–28; higher scores indicate more functional impairment.
Including residents who either had a DNH directive before the outbreak or acquired a new DNH directive during the ACP initiative (n = 390), 151 residents tested positive for COVID‐19 (Table 2). Rates of hospitalization were low: one (2%) resident who acquired a DNH during the study period was hospitalized, whereas two residents (2%) with previous DNH directives were hospitalized. There were 26 (40%) deaths among residents who acquired a DNH during the study period and 41 (48%) deaths among residents with a previous DNH directive.
TABLE 2.
Characteristics and outcomes of residents who were diagnosed with COVID‐19 according to do‐not‐hospitalize (DNH) directive
| All COVID‐19+ residents with DNH directives (n = 151) | New DNH directive (n = 65) | Previous DNH directive c (n = 86) | |
|---|---|---|---|
| Age, years | 86 (9) | 87 (10) | 86 (9) |
| Female sex | 87 (58%) | 38 (58%) | 49 (57%) |
| Caucasian | 129 (85%) | 56 (86%) | 73 (85%) |
| Cognitive impairment a | 63 (42%) | 28 (43%) | 35 (41%) |
| Activities of daily living score b | 17 (8) | 16 (7) | 17 (8) |
| Hospitalization | 3 (2%) | 1 (2%) | 2 (2%) |
| Death | 67 (44%) | 26 (40%) | 41 (48%) |
Note: Statistics presented: mean (SD); n (%).
Cognitive impairment defined as moderate to severe decisional impairment as described by nursing staff.
Katz activities of daily living score, range 0–28; higher scores indicate more functional impairment.
Previous DNH directive defined as a DNH directive in place before the study period.
During follow‐up, only six residents had their DNH orders reversed. Two reversals were among the residents hospitalized for non‐COVID‐19 related conditions described above. One reversal occurred after the resident's proxy consulted additional family, whereas the other reversal was due to reconsideration of preferences once the peak of the pandemic had passed. There were two additional residents with a temporary reversal in directive to hospitalize: one was due to a guardian waiting for legal affirmation and the other was due to a proxy wavering on whether the DNH directive was appropriate. The mean (SD) time from new DNH directive to DNH reversal was 30 (±25) days.
4. DISCUSSION
We describe the creation and rapid implementation of an innovative, compassionate, and efficient process for conducting and tracking ACP discussions using real‐time EMR data to identify residents at greatest risk. This COVID‐19 specific ACP initiative resulted in a substantial increase (46%–67%) in the proportion of residents with DNH directives at two sites caring for LTC residents in a large healthcare organization. Among the 124 residents who acquired a DNH directive, approximately half were diagnosed with COVID‐19. Although mortality was considerable in this population, most residents received medical care in the facility concordant with stated preferences. Among all COVID‐19+ residents with a DNH directive, hospitalization rates were low (~2%) and similar regardless of whether the resident acquired the DNH before the initiative or during the initiative. Reversal of the DNH directive several months following the peak of the pandemic was uncommon.
We are aware of one other study on a COVID‐19 specific conversation tool for ACP discussions in the LTC setting. 12 Similar to our results, the authors reported a sharp increase in DNH directives following ACP discussions: among 16 residents with COVID‐19 who lacked DNH directives, 8 residents (50%) acquired a DNH directive. Our approach differed as we utilized redeployed staff of varied disciplines and did not rely on physicians, advanced practice professionals, or nurses, yet we found a similar increase in DNH directives. Another study of a LTC ACP initiative before the pandemic reported that over a period of 17 months, only 0.4% of directive changes involved a change in DNH status. 13
The marked increase in DNH directives over a short period of time suggests that these changes were primarily driven by the concern associated with COVID‐19. It was notable that the majority of new DNH directives occurred in residents after a COVID‐19 diagnosis. This may have been the result of proxies being more motivated to consider the ACP discussion seriously following the diagnosis of COVID‐19, or it could be because the SWAT Team prioritized residents with COVID‐19 and were unable to reach the unaffected residents quickly enough. Among all residents who acquired a DNH, approximately half were never diagnosed with COVID‐19, suggesting that reasons for updating the directive may have involved motivations beyond the risks associated with COVID‐19. Overall, we speculate that the sharp increase in DNH orders is likely attributable to the concern associated with the COVID‐19 outbreak, but it is possible that some resident care preferences had not been previously captured.
Although feedback was not collected in a standardized manner, informal feedback was generally very positive. Only three family members expressed discomfort with the call. Reasons cited for discomfort were due to the caller being unknown to the proxy and the topic being distressing. Future studies involving new approaches to ACP should solicit more standardized feedback to assess the experience of proxies and staff.
There were several limitations to this study. First, this study was conducted under the auspices of a well‐resourced academic healthcare organization, and other facilities may be limited in emulating this model. For instance, the inclusion of informatics and biostatistics personnel allowed the team to generate real‐time EMR reports to target residents at highest risk. Although some facilities do not have an EMR system, all facilities have some form of documentation for DNH directives that could be utilized to prioritize ACP. Second, our follow‐up period was limited to 2–3 months. Ideally, it would extend beyond 6 months to understand long‐term outcomes.
In addition, we noted several barriers and facilitators to implementing this pragmatic care initiative in the LTC setting. High resident to staff ratios pose a significant barrier to implementing any new policy or care initiative in the LTC setting. To overcome this barrier, we employed a creative strategy which utilized retired and redeployed staff members. While this strategy was effective in response to a COVID‐19 outbreak, the SWAT Team was disbanded as the outbreak subsided because there was no longer an urgent need and it would not have been financially sustainable. This flexible model of staff utilization and ACP could be reengaged in the face of another COVID‐19 outbreak or other health crisis, including vaccination uptake. Facilitators to implementation of this pragmatic ACP initiative included a robust EMR, the multidisciplinary structure of the team, and strong stakeholder and Champion involvement. First, the use of a robust EMR, which included separate fields for advance directive orders, allowed the team to efficiently prioritize the most vulnerable residents. Development of new and existing EMR systems should include advance directive orders as separate fields in the EMR, especially when used in the LTC setting. Second, this initiative was successful due to the multidisciplinary structure of the team, which included experts from the clinical, informatics, and research teams. Finally, the success of this initiative was largely due to strong stakeholder and Champion involvement. The Champion of this initiative, the Director of Palliative Care Services, was engaged in every step of implementation. Other pragmatic studies in the NH setting have established that strong Champion involvement is a key factor in implementation success. 14 , 15
5. CONCLUSIONS AND IMPLICATIONS
In this report, we described a pragmatic COVID‐19 ACP SWAT Team that was successfully developed and integrated into a healthcare system to care for LTC residents during the pandemic. This ACP initiative highlights the roles of a robust EMR system in the LTC setting, telephone evaluation and management, and a creative model of staff redeployment in expanding access to ACP during a time of unprecedented need for palliative services. Feedback from stakeholders was generally positive and few DNH directives were reversed during follow‐up. As the COVID‐19 pandemic continues, we hope this model for ACP may be adapted to other LTC facilities to target vulnerable residents and promote goal‐concordant care.
Beyond the response to the COVID‐19 outbreak, this model highlights the importance of strong Champion and stakeholder involvement in the successful implementation of a LTC initiative. We encourage any facility that wishes to employ a similar model, whether the objective is to increase access to ACP or to institute a COVID‐19 vaccination plan, to ensure stakeholder and Champion engagement to enhance uptake.
FINANCIAL DISCLOSURE
This work was supported by the National Institute of Health (NIH), National Institute on Aging (NIA), 5T35AG038027‐0 and K24 AG070106. Dr. Susan L. Mitchell was supported by the NIA of the National Institutes of Health under Award Number U54AG063546, which funds NIA Imbedded Pragmatic Alzheimer's Disease and AD‐Related Dementias Clinical Trials Collaboratory (NIA IMPACT Collaboratory). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
CONFLICT OF INTEREST
None to declare.
AUTHOR CONTRIBUTIONS
Study concept: Sarah D. Berry, Emily Palmer, and Susan L. Mitchell. Data acquired: Timothy Tsai and Michelle J. Berning. Analysis and verification of data accuracy: Timothy Tsai. Drafting of the manuscript: Michelle J. Berning and Sarah D. Berry. All authors participated in interpretation of results and revision of manuscript.
SPONSOR'S ROLE
The funding agency played no role in the analysis or preparation of the manuscript.
Supporting information
Data S1. COVID‐19 advance care planning conversation guide.
ACKNOWLEDGMENTS
Berning MJ, Palmer E, Tsai T, Mitchell SL, Berry SD. An advance care planning long‐term care initiative in response to COVID‐19. J Am Geriatr Soc. 2021;69:861–867. 10.1111/jgs.17051
Funding information NIA of the National Institutes of Health, Grant/Award Numbers: U54AG063546, K24 AG070106, 5T35AG038027‐0
REFERENCES
- 1. Conlen M. More than 40% of US coronavirus deaths are linked to nursing homes. New York Times . https://www.nytimes.com/interactive/2020/us/coronavirus-nursing-homes.html. Accessed August 13, 2020.
- 2. Mueller AL, McNamara MS, Sinclair DA. Why does COVID‐19 disproportionately affect older people? Aging. 2020;12(10):9959‐9981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. McMichael TM, Currie DW, Clark S, et al. Epidemiology of Covid‐19 in a long‐term care facility in King County, Washington. N Engl J Med. 2020;382(21):2005‐2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Brouns SH, Brüggemann R, Linkens A, et al. Mortality and the use of antithrombotic therapies among nursing home residents with COVID‐19. J Am Geriatr Soc. 2020;68:1647‐1652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Martin RS, Hayes B, Gregorevic K, Lim WK. The effects of advance care planning interventions on nursing home residents: a systematic review. J Am Med Dir Assoc. 2016;17(4):284‐293. [DOI] [PubMed] [Google Scholar]
- 6. Bischoff KE, Sudore R, Miao Y, Boscardin WJ, Smith AK. Advance care planning and the quality of end‐of‐life care in older adults. J Am Geriatr Soc. 2013;61(2):209‐214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Curtis JR, Kross EK, Stapleton RD. The importance of addressing advance care planning and decisions about do‐not‐resuscitate orders during novel coronavirus 2019 (COVID‐19). JAMA. 2020;323(18):1771‐1772. [DOI] [PubMed] [Google Scholar]
- 8. Harris PA, Taylor R, Minor BL, et al. The REDCap consortium: building an international community of software partners. J Biomed Inform. 2019;95:103208. 10.1016/j.jbi.2019.103208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap) – a metadata‐driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377‐381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Morris JN, Hawes C, Fries BE, et al. Designing the national resident assessment instrument for nursing homes. Gerontologist. 1990;30(3):293‐307. [DOI] [PubMed] [Google Scholar]
- 11. R Core Team . R: A Language and Environment for Statistical Computing. Vienna, Austria: R Foundation for Statistical Computing; 2019. https://www.R-project.org/. [Google Scholar]
- 12. Gaur S, Pandya N, Dumyati G, Nace DA, Pandya K, Jump RL. A structured tool for communication and care planning in the era of the COVID‐19 pandemic. J Am Med Dir Assoc. 2020;21:943‐947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Hickman SE, Unroe KT, Ersek MT, Buente B, Nazir A, Sachs GA. An interim analysis of an advance care planning intervention in the nursing home setting. J Am Geriatr Soc. 2016;64(11):2385‐2392. [DOI] [PubMed] [Google Scholar]
- 14. Loomer L, McCreedy E, Belanger E, et al. Nursing home characteristics associated with implementation of an advance care planning video intervention. J Am Med Dir Assoc. 2019;20(7):804‐809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Tappen R, Wolf D, Rahemi Z, et al. Barriers and facilitators to implementing a change initiative in long‐term care utilizing the INTERACT™ quality improvement program. Health Care Manag (Frederick). 2017;36(3):219‐230. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data S1. COVID‐19 advance care planning conversation guide.


