Acute bronchiolitis is one of the most common health burdens in infants worldwide and leads to frequent hospitalisation, morbidity and mortality. 1 Children have been relatively spared by the COVID‐19 pandemic, but reports of multisystem inflammatory syndrome 2 and probable long‐term COVID 3 effects in children have started to emerge. One major concern was whether the overlap of the pandemic and seasonal bronchiolitis would put substantial pressure on healthcare systems. Bronchiolitis has a predictable seasonal pattern, primarily in autumn and winter, and in France, this is between October and February. The second COVID‐19 wave in France led to a 2‐week night curfew from 17 October 2020, followed by a full lockdown on 30 October. However, day care centres and primary and secondary schools remained open.
The aim of this study was to determine the effect on bronchiolitis of the second COVID‐19 pandemic wave in France and the public measures introduced to halt infections, namely social distancing, wearing masks, hand hygiene, curfews and lockdowns.
It was conducted at one of the largest tertiary university paediatric hospitals in the Paris region, which handles about 55,000 paediatric emergency department (PED) visits a year. We used our electronic health record system to identify all children under the age of 2 years who visited our PED with bronchiolitis. The International Classification of Diseases, 10th Revision codes J21.0, J21.1, J21.8 and J21.9 were used. We identified the number of infants visiting the PED for bronchiolitis and the number who were hospitalised during the start of the 2020–2021 bronchiolitis epidemic season, from week 41 (early October) to week 52 (end of December). These were compared with the same weeks in 2015 to 2019 using time series analysis. The data were analysed with SPSS, version 18 (SPSS Inc, Chicago, USA).
The study was approved by the Ethics Committee for Research of the Sorbonne University (CER‐2020–105).
During the five pre‐pandemic seasons, bronchiolitis epidemic curves started to rise in weeks 37–41 and peaked between weeks 47 and 49. During the pandemic season, the curve only rose slightly in week 37 and was nearly flat until week 52 (Figure S1). During the five pre‐pandemic seasons, the total number of PED visits for bronchiolitis from the beginning of the epidemic in October (week 41) to its end in February (week 8) was 6,052, with 78.9% of these visits from weeks 41 to 52. Between weeks 41 and 52, the mean and standard deviation weekly number of visits for bronchiolitis were 79.2 ± 38.5 during the pre‐pandemic seasons and only 11.6 ± 3.8 during the pandemic season (p = 0.0022). Pandemic season visits for bronchiolitis were 82.1% lower than predicted by the time series analysis which had a R‐squared of 0.8 (Figure 1). The mean and standard deviation weekly number of hospital admissions for bronchiolitis during weeks 41–52 were 30.0 ± 16.6 for the pre‐pandemic seasons and only 3.6 ± 1.8 for the pandemic season (p = 0.0022) (Figure S2). Pandemic season hospital admissions for bronchiolitis were 82.5% lower than predicted.
FIGURE 1.
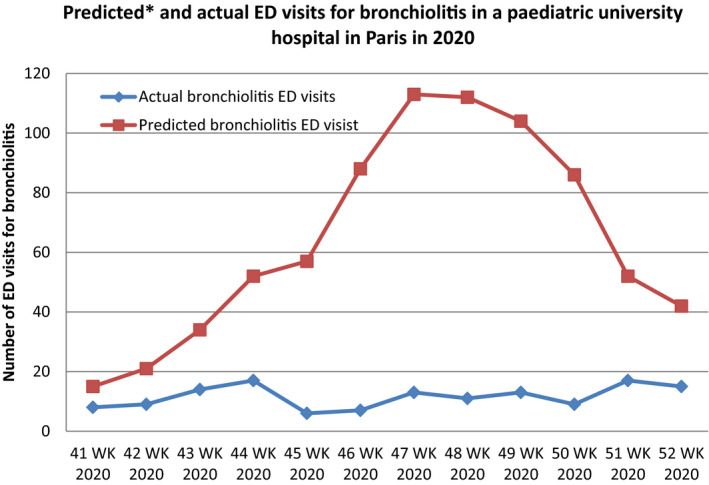
Comparison of predicted and actual paediatric emergency department visits for bronchiolitis in one university paediatric hospital in Paris during the COVID‐19 outbreak. Pandemic season visits for bronchiolitis between weeks 41 and 52 were 82.1% lower than predicted. *Time series analysis was used to predict the pandemic season visits using the 2015–2019 bronchiolitis epidemic seasons data. R‐square of the model was 0.8
The bronchiolitis burden dramatically decreased during the second COVID‐19 wave in France and reports from the Southern Hemisphere indicated similar reductions during the first COVID‐19 wave. 4 It is very likely that decreased human contacts had a major impact on the spread of bronchiolitis viruses, especially the respiratory syncytial virus. It is important to note that, while adults have been partially restricted in France, children have continued to attend day care centres and schools. Our findings challenge the widely accepted notion that children are the main vectors of bronchiolitis viruses and suggest that adults may play an important role in spreading the bronchiolitis virus. For example, there was a marked decline in bronchiolitis in 1995–1996 in the Paris region during a major 3‐week public transport workers strike, which forced many people to stay at home. 5 The COVID‐19 measures have had a striking beneficial effect on infants, and it is very likely that lives have been saved. This prompts us to ask whether we should change our habits in future and advise people to wear masks, increase social distancing and reinforce hand hygiene when they have respiratory tract infections. Within this context, we could also underline that during bronchiolitis seasons young infants should not be taken to mass gatherings in order to reduce contacts with adults.
This study had some limitations. First, the 2020–2021 season we observed on went up to week 52 and did not encompass the whole bronchiolitis season. However, weeks 41–52 accounted for 78.9%, of PED visits for bronchiolitis in the five pre‐pandemic seasons and we feel our results were fairly representative of the 2020–2021 bronchiolitis epidemic. Moreover, our predictive model was very strong as it had an R‐squared of 0.8. Second, this was a single centre study and it did not necessarily represent visits for bronchiolitis to other French PEDs. However, the study centre is one of the largest paediatric centres in France and is very likely to have similar patterns to other French PEDs. Third, during the partial lockdown, Parisian children still attended day care centres and schools. Many areas of the world did not follow this strategy which could make our results less generalisable to other countries. However, we could still have expected large bronchiolitis transmission in France, as children were not locked down like adults.
We believe that the remarkable reduction in bronchiolitis observed, which extended beyond its expected peak in this country in the Northern Hemisphere, provides an important public health message. It can also help health systems to understand future bronchiolitis epidemics better.
CONFLICT OF INTEREST
The authors have no conflicts of interest to declare.
Supporting information
App S1
Funding information
No external funding.
REFERENCES
- 1. American Academy of Pediatrics Subcommittee on D, Management of B . Diagnosis and management of bronchiolitis. Pediatrics. 2006;118(4):1774‐1793. [DOI] [PubMed] [Google Scholar]
- 2. Carbajal R, Lorrot M, Levy Y, et al. Multisystem inflammatory syndrome in children rose and fell with the first wave of the COVID‐19 pandemic in France. Acta Paediatr. 2020. https://doi.org.10.1111/apa.15667 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Ludvigsson JF. Case report and systematic review suggest that children may experience similar long‐term effects to adults after clinical COVID‐19. Acta Paediatr. 2020. https://doi.org.10.1111/apa.15673 [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Vasquez‐Hoyos P, Diaz‐Rubio F, Monteverde‐Fernandez N, et al. Reduced PICU respiratory admissions during COVID‐19. Arch Dis Child. 2020. https://doi.org.10.1136/archdischild‐2020‐320469 [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 5. Thelot B, Bourrillon A. Coincidence of public transport strike with bronchiolitis epidemic. Lancet. 1996;348(9043):1743‐1744. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
App S1


