Cardiopulmonary exercise testing (CPET) before major surgery provides the best risk estimate of postoperative morbidity, mortality and consequent prognosis [1], yet is currently suspended because of the hazards associated with aerosol‐generating physical exercise and potential infective transmission [2]. While some services have transitioned to secondary, less informative assessments of cardiopulmonary function [3], novel counter‐measures are required if surgical outcomes are to be optimised. Moreover, the related effect size is such that by July 2020, COVID‐19 disease was associated with an 81‐fold increase in the number of patients (n = 83,000) waiting > 1 year for NHS treatment in England alone [4]. Despite the transmission‐reducing potential of porous microbacterial/viral filters (BVF), concerns related to water vapour saturation and increased ventilatory resistance raise barriers to implementation [2]. The aim of our study was to investigate the effect of a novel BVF on cardiorespiratory parameters during CPET, in a randomised single‐blind crossover study.
Following ethical approval as a service evaluation (Cardiff and Vale University Health Board), 12 healthy, male participants with a mean (SD) age of 45 (10) years completed two separate CPET tests (seven days apart), with BVF and without (true value) BVF, distal to the sampling line. Participants performed a standardised incremental cycling test to volitional exhaustion with online breath‐by‐breath respiratory gas analysis (MedGraphics Ultima Series, Saint Paul, MN, USA) [5]. Modified Bland‐Altman plots determined mean differences and course of bias. Interpretive implications for surgical risk stratification in a separate group of 618 patients who had previously undergone CPET before surgery for colorectal cancer were used for comparison.
A strong positive correlation was observed between the BVF and true value trials (r 2 = 0.956, p < 0.001). The BVF resulted in a systematic error and (mean) overestimation of pulmonary ventilation (, +10.2 l.min‐1, p < 0.001) and corresponding oxygen uptake (, +5.6 ml.min‐1.kg‐1, p < 0.001) (Figure 1B–D, including corrective equation). Failure to account for these differences would have meant that 2.8 % of colorectal patients would have been misleadingly classified as being unfit (anaerobic threshold < 11 mlO2.kg‐1.min‐1 [5]) compared with the authentic value of 53%.
Figure 1.
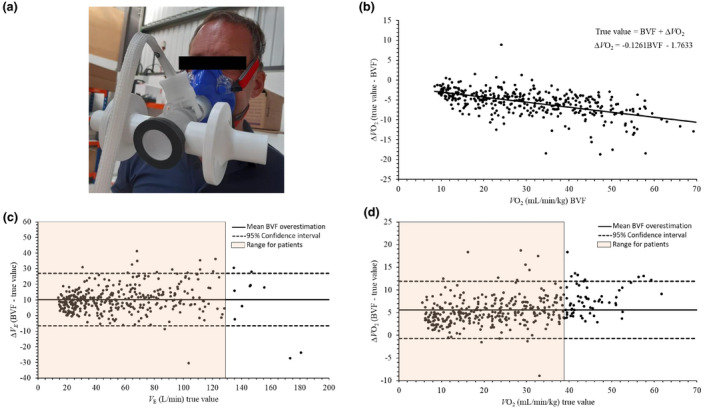
Dynamic changes in select cardiopulmonary metrics during cardiopulmonary exercise testing (CPET) with BVF and without (true value) a BVF. (a) specialist BVF; (b) provides the correction required when conducting CPET with a BVF. Modified Bland‐Altman plots display the mean difference between BVF and true values for: (c) Pulmonary ventilation (), +10.2 l.min‐1 (p < 0.001) and (d) Oxygen uptake (), +5.6 ml.min‐1.kg‐1 (p < 0.001). Data points represent the middle five of seven breaths subsequently averaged for each 10 W increment of power output. Reference ranges are from patients (n = 3168) who underwent CPET before major surgery; mean (SD) 49.8 (17.9) l.min‐1 and 16.1 (5.0) mlO2.min‐1.kg‐1.
Collectively, the findings indicate that CPET can be safely performed with a specialist BVF, minimising potential for transmission of aerosolised particles. The systematic overestimation driven by inflated measurement of gas flow across the mouthpiece pneumotach can be corrected for, allowing metrics of to be (re)calculated with accuracy and precision. These findings should help re‐establish safe CPET services in the clinical setting to guide and refine physiological stage‐directed patient care.
We acknowledge MGC Diagnostics Corporation for developing the specialist BVF and N. Chapman (Medical Graphics UK Ltd) for his co‐operation and input. The authors also acknowledge Professor S. Ward for helpful discussion. No competing interests declared.
References
- 1. Fleisher LA, Fleischmann KE, Auerbach AD, et al. 2014 ACC/AHA guideline on perioperative cardiovascular evaluation and management of patients undergoing noncardiac surgery: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines. Journal of Nuclear Cardiology 2015; 22: 162–215. [DOI] [PubMed] [Google Scholar]
- 2. Faghy MA, Sylvester KP, Cooper BG, Hull JH. Cardiopulmonary exercise testing in the COVID‐19 endemic phase. British Journal of Anaesthesia 2020; 125: 447–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Hull JH, Lloyd JK, Cooper BG. Lung function testing in the COVID‐19 endemic. Lancet Respiratory Medicine 2020; 8: 666–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Griffin S. Covid‐19: Waiting times in England reach record highs. British Medical Journal 2020; 370: m3557. [DOI] [PubMed] [Google Scholar]
- 5. Rose GA, Davies RG, Davison GW, et al. The cardiopulmonary exercise test grey zone; optimising fitness stratification by application of critical difference. British Journal of Anaesthesia 2018; 120: 1187–94. [DOI] [PubMed] [Google Scholar]


