Abstract
Aim
We examined the impact of the COVID‐19 pandemic on how many children were admitted to Israel's largest tertiary paediatric hospital and why they were admitted.
Methods
Israel declared COVID‐19 a national emergency on 19 March 2020. This study examined daily hospital admissions to our three general paediatric wards during the COVID‐19 lockdown period from 20 March to 18 April 2020. These 258 admissions were compared with the 4217 admissions from the period immediately before this, 1 February to 19 March 2020, plus 1 February to 18 April in 2018 and 2019. We also compared why patients were admitted during the study period, and any pre‐existing conditions, with 638 children hospitalised during the same period in 2019.
Results
The mean number of daily hospitalisations during the COVID‐19 lockdown period was 8.6, which was 59% lower than the 20.9 recorded during the other three periods before COVID‐19. There was a significant decrease in the number of patients admitted with infectious (74%) and non‐infectious (44%) aetiologies from 2019 to 2020, and these occurred among patients with (58%), and without (55%), pre‐existing medical conditions.
Conclusion
The Israeli COVID‐19 lockdown had a dramatic effect on admissions to the paediatric wards of a tertiary hospital.
Keywords: coronavirus, hospital admissions, infections, paediatric wards, pre‐existing conditions
Abbreviations
- IRR
incidence rate ratio
- 95% CI
95% confidence interval
Key notes.
Mean daily admissions to Israel's largest paediatric hospital were 59% lower in the 4 weeks after the Government declared a national emergency due to COVID‐19.
The rates of hospitalisations in three general paediatric wards were compared with the immediate pre‐pandemic lockdown period and data for 2018 and 2019.
There were significant decreases in patients admitted with infectious and non‐infectious diseases and with and without pre‐existing medical conditions.
1. INTRODUCTION
COVID‐19 originated in Wuhan, China, 1 and was declared a pandemic by the World Health Organization on 11 March 2020. 2 Some studies that investigated the impact of COVID‐19 on the paediatric population have reported that most of the children who were infected were asymptomatic or had mild symptoms. 3 , 4 However, there has been considerable concern about the indirect influence of the pandemic on children with other medical conditions. 5
Protective measures against exposure to the virus have had a significant impact on daily medical practice. Much of the communication between healthcare professionals and patients has become virtual, increasing the risks for misdiagnosis or missing serious medical conditions. Moreover, the fear of contracting COVID‐19 has meant that people have avoided visiting medical facilities and this has led to delays in addressing medical problems. Delayed referrals, and their consequences, have been described in past pandemics 6 and are now being reported during the present one. 7 , 8 , 9 , 10
Another interesting aspect is the potential influence of the COVID‐19 outbreak on the incidence of other medical conditions. 11 Like many other countries, the Israeli Government has imposed numerous restrictions on the population. From 12 to 14 March 2020, all educational institutions were closed, including kindergartens and schools. Then, on 19 March a national state of emergency was declared and citizens were instructed to go into lockdown and refrain from leaving their house, except for urgent reasons. The main restrictions included forbidding group gatherings, closing all leisure venues and non‐essential stores, mandatory masks and total quarantine during a national holiday. These restrictions led to a marked decrease in physical contact between children, which could have reduced the spread of infectious diseases. As a result, we could have expected a decrease in infection‐related morbidity in Israel, in line with the reductions described by Kadambari et al in a paper on the pandemic. 12
The aim of this study was to investigate the impact of the COVID‐19 pandemic lockdown in Israel on the number of children hospitalised in three general paediatric wards and the nature of those admissions.
2. METHODS
We performed a retrospective cohort study in the largest tertiary paediatric hospital in Israel, the Schneider Children's Medical Center of Israel in Petah Tiqva, which is about 10 kilometres from Tel Aviv. The data were obtained from the hospital's electronic database.
All hospitalisations in the three general paediatric wards between 1 February and 18 April during 2018, 2019 and 2020 were studied. Hospitalisations that listed COVID‐19 as a main cause of admission (total of 20 admissions) were excluded, since the purpose of our study was to evaluate the impact of the pandemic on hospitalisations of patients with conditions other than COVID‐19 disease.
The COVID‐19 study period was defined as 20 March to 18 April 2020. This four‐week COVID‐19 period was chosen because the Israeli Government declared a state of emergency on 19 March. Educational institutions were closed one week earlier, from 12 to 14 March. On 19 April, the Government relaxed some of the restrictions, including gradually reopening kindergartens and schools.
The comparison period comprised three time intervals before COVID‐19: the immediate pre‐COVID‐19 period from 1 February to 19 March 2020 and the periods from 1 February to 18 April in 2018 and 2019.
A comprehensive examination of our patient records was carried out to identify hospitalisations that took place during the COVID‐19 study period from 20 March to 18 April and the corresponding period in 2019. The records were divided into two major categories, according to the primary cause of hospitalisation, namely infectious and non‐infectious, and were then sub‐divided according to common disease aetiologies. In addition, we classified the patients by their medical background, as children with chronic conditions and previously healthy individuals. A chronic disease was defined as requiring a routine follow‐up by a specialist physician or needing regular medications.
This study was approved by the hospital's Institutional Research Ethics Board reference number 0363–20‐RMC.
2.1. Outcome measures
The primary outcome was a comparison between the number of daily hospitalisations during the COVID‐19 lockdown period of 20 March to 18 April and the three periods.
The secondary outcome was to compare the reasons for the admissions and the medical backgrounds of the patients between the COVID‐19 period and the corresponding four‐week period in 2019.
2.2. Statistical analysis
All analyses were performed using SPSS statistics software, version 17.0 (IBM Corp.), and a p value of <0.05 was considered statistically significant. We used negative binominal regression to examine the effect of the COVID‐19 pandemic on the number of daily hospitalisations. This model was chosen because of the over dispersed nature of the dependent variable, which was the number of daily hospitalisations.
To analyse the impact of the COVID‐19 pandemic on the number of hospitalisations for each admission category, we carried out a separate model for the causes of admission, which were organised into groups. Using the model, we calculated the incidence rate ratios (IRR) that represented the ratio of the number of patients hospitalised during the COVID‐19 period and compared that with the corresponding period in 2019.
The chi‐square test was used to compare patients with, and without, chronic conditions.
For descriptive purposes, the number of daily hospitalisations was plotted during the different research periods.
3. RESULTS
A total of 4475 hospitalisations were included in the study: 258 in the COVID‐19 study period of 20 March to 18 April 2020 and 4217 in the three comparison periods of 1 February to 19 March 2020 and 1 February to 18 April 2018 and 2019. There were 1004 hospitalisations immediately before the study period in 2020, 1661 in 2019 and 1552 in 2018. The 20 hospitalisations due to COVID‐19 were not included in the 258 children studied during the COVID‐19 period.
Figure 1 shows that the number of daily hospitalisations declined during the COVID‐19 period (8.9), compared to the combined figure for the immediate period before COVID‐19 and the comparative periods in 2018 and 2019 (20.9). This was a reduction of 59%, an incidence rate ratio (IRR) of 0.41 and a 95% confidence interval (95% CI) of 0.28–0.62 (p < 0.001).
FIGURE 1.
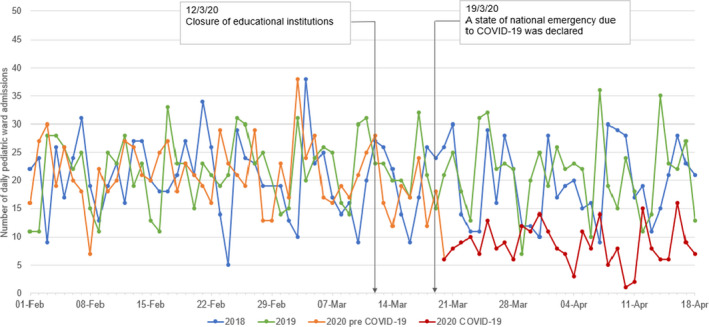
Number of hospitalisations in paediatric wards before and during the first 4 weeks of the pandemic relative to the same period in 2018 and 2019
The number of hospitalisations by cause of admission during the COVID‐19 period, and the corresponding four‐week period in 2019, is displayed in Figure 2. The total number of hospitalisations for all causes was 258 and 638, respectively. During the COVID‐19 period, patients admitted with an infectious aetiology fell by a significant 74% (IRR 0.26; 95% CI 0.15–0.46; p < 0.001) and there was a significant fall of 44% for those with a non‐infectious aetiology (IRR 0.56; 95% CI 0.33–0.96; p = 0.04). There was a significant decrease in hospitalisations due to viral infections (85%) and viral respiratory infections (76%). Hospital admissions also fell for bacterial infections (63%) and bacterial respiratory infections (67%). Most of the subgroups in the non‐infectious category did not show a significant decrease in the number of hospitalisations. The exceptions included patients with rheumatic and psychiatric diseases, the miscellaneous category and children referred for elective procedures (Figure 3). When we analysed the patients' medical backgrounds, we found a significant decrease in the number of patients admitted with (58%), and without (55%), existing conditions. There was no significant difference in the number of chronic patients hospitalised, as the percentages of total admissions, between the COVID‐19 period and the corresponding four‐week period in 2019: 44% versus 46%, respectively, p = 0.61.
FIGURE 2.
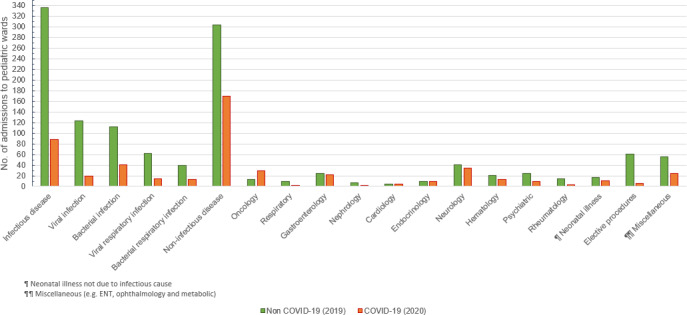
Number of hospitalisations by admission during the COVID‐19 study period and the corresponding period in 2019
FIGURE 3.
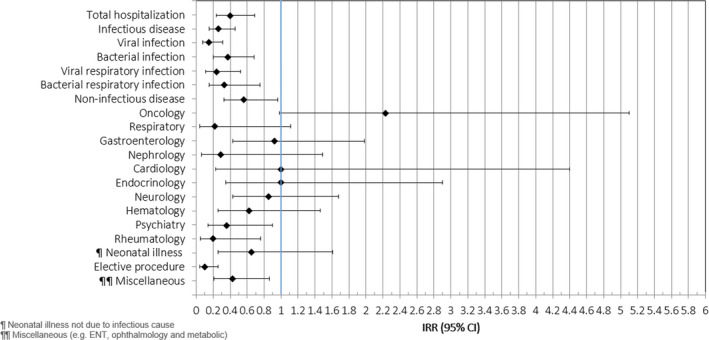
Forest plot showing the incidence rate ratios of the different reasons for hospitalisations between the COVID‐19 study period and the corresponding period in 2019
4. DISCUSSION
Our study showed that there was a drop in the total number of admissions to the three general paediatric wards of Israel's largest tertiary paediatric hospital in the four weeks after the Government declared COVID‐19 a national emergency.
The overall number of hospital admissions decreased by almost 60% during the pandemic study period, and this finding was consistent with previous reports of significant decreases in emergency department presentations. 13 The reduction in hospitalisation numbers during the COVID‐19 pandemic appears to be much greater than the lower numbers observed during the severe acute respiratory syndrome outbreak in 2009. For example, a Canadian study by Michael et al reported a reduction of only 10%–12% in the total number of admissions at that time. 14
Our findings can be explained by several factors. People were concerned about visiting hospitals because they saw them as sites where they could be exposed to COVID‐19. This stopped parents from entering hospitals and minimised referrals from primary care physicians. In addition, medical insurance companies encouraged the general public to find alternative ways to receive medical care, such as telemedicine. 15 This increased concerns about the role of medical institutions in spreading the virus. It is difficult to link missed referrals, and their consequences, directly to the pandemic, because they may be underestimated. This is because only catastrophic ones have tended to be reported. Moreover, the impact of delaying treatment may take weeks or months to become obvious, especially if children have chronic illnesses.
Another possible contributing factor to the decrease in the number of hospitalisations could have been the reduction in the transmission of infectious disease due to COVID‐19 restrictions. When we analysed the number of hospitalisations by diagnosis, we found a substantial reduction in cases with an infectious aetiology, of both viral and bacterial origins. A 2020 paper by Li et al reported similar observations in Hangzhou, China. 11 We believe that the most plausible explanation for these findings lies in the restrictions imposed to minimise the spread of the virus. The main measures taken in Israel were closing educational facilities and telling people to stay at home. These restrictions prevented regular contact between people in general and among children in particular. As a result, the risk of infection transmission was reduced, as reported by another Israeli paper. 16
An exceptional decrease in the number of hospitalisations was observed among children with rheumatic and psychiatric diseases and in patients admitted for elective procedures and miscellaneous aetiologies. The reduction in hospitalisations for elective procedures was directly related to the closure of the hospital's ambulatory services and cessation of elective activities, as instructed by the Israel Ministry of Health. The miscellaneous group included patients with less common causes for hospitalisation, such as ear, nose and throat, ophthalmology and metabolic diseases. The small numbers did not allow us to create specific sub‐analyses for each category. It is difficult to draw any clear conclusions about the reduction in hospitalisations of children with rheumatic diseases, because the sample was small. However, the fact that infectious diseases are known to play a role in triggering autoimmune diseases may explain this finding. 17 Lastly, we found a significant reduction in hospital admissions of patients with psychiatric conditions. Although we expected the stress of the pandemic and lockdown to aggravate these illnesses, patients may have been scared of getting infected with COVID‐19 and avoided coming to the hospital.
We do wonder whether the reduced number of hospitalised children during the outbreak reflects the true number of patients who actually needed inpatient care. It may well be that the reasons why physicians hospitalise patients need to be re‐examined. Scaramuzza et al raised a similar question regarding the use of the emergency departments in Italy. 13
Another interesting finding was the lack of any significant difference between the percentages of patients with and without chronic diseases. We expected to find that a larger percentage of chronic patients had been admitted, because many of them cannot be treated in outpatient settings. One of the most common causes of deterioration in patients with chronic conditions is developing an infectious disease. Therefore, the reduction in the prevalence of infectious diseases might be explained by the decreased need for hospitalisation in this population. Another explanation is that these high‐risk patients avoided being hospitalised because of considerable concerns about acquiring the virus that causes COVID‐19.
Our study had several limitations. First, it was conducted in a single, urban, paediatric tertiary hospital and this means that the generalisability of these findings is limited to comparable institutions. Second, we only observed a short period, which covered the first four weeks at the start of the pandemic in Israel, and it may not reflect the real long‐term impact of the COVID‐19 outbreak. Lastly, we lacked information about patients who did not seek medical help or were not referred to our hospital. This additional information might have provided greater clarity about all the factors that drove the decrease in the number of hospitalisations during the COVID‐19 pandemic period.
5. CONCLUSION
Our results show that the first four weeks of the COVID‐19 pandemic in Israel led to a dramatic reduction in the number of patients admitted to the general paediatric wards of the country's largest paediatric hospital. It also had an impact on the distribution of the reasons for those admissions. Further studies are needed to identify the factors that may have affected this trend, which has also been reported in other countries. There is a need to re‐examine the indications for hospitalisation and to find out whether reduced admissions are damaging the health of paediatric patients due to late diagnoses and referrals.
CONFLICT OF INTEREST
The authors have no conflicts of interest to declare.
REFERENCES
- 1. Zhou P, Yang XL, Wang XG, et al. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature. 2020;579(7798):270‐273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. World Health Organization (WHO) . WHO Director‐General's opening remarks at the media briefing on COVID‐19. 11 March 2020. Published March 11, 2020. https://www.who.int/dg/speeches/detail/who‐directorgeneral‐s‐opening‐remarks‐at‐the‐media‐briefingon‐covid‐19–‐11‐march‐2020. Accessed March 11, 2020.
- 3. Ludvigsson JF. Systematic review of COVID‐19 in children shows milder cases and a better prognosis than adults. Acta Paediatr. 2020;109(6):1088‐1095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Castagnoli R, Votto M, Licari A, et al. Severe Acute Respiratory Syndrome Coronavirus 2 (SARS‐CoV‐2) infection in children and adolescents. JAMA Pediatr. 2020;174(9):882‐889. [DOI] [PubMed] [Google Scholar]
- 5. Isba R, Edge R, Jenner R, Broughton E, Francis N, Butler J. Where have all the children gone? Decreases in paediatric emergency department attendances at the start of the COVID‐19 pandemic of 2020. Arch Dis Child. 2020;105(7):704. [DOI] [PubMed] [Google Scholar]
- 6. Chang HJ, Huang N, Lee CH, Hsu YJ, Hsieh CJ, Chou YJ. The impact of the SARS epidemic on the utilization of medical services: SARS and the fear of SARS. Am J Public Health. 2004;94(4):562‐564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Roland D, Harwood R, Bishop N, Hargreaves D, Patel S, Sinha I. Children's emergency presentations during the COVID‐19 pandemic. Lancet Child Adolesc Health. 2020;4(8):e32‐e33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Lazzerini M, Barbi E, Apicella A, Marchetti F, Cardinale F, Trobia G. Delayed access or provision of care in Italy resulting from fear of COVID‐19. Lancet Child Adolesc Health. 2020;4(5):e10‐e11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Snapiri O, Danziger CR, Krause I, et al. Delayed diagnosis of paediatric appendicitis during the COVID‐19 pandemic. Acta Paediatr. 2020;109(8):1672‐1676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Danziger CR, Krause I, Scheuerman O, et al. Pediatrician, watch out for corona‐phobia. Eur J Pediatr. 2020;13:1‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Li H, Yu G, Duan H, Fu J, Shu Q. Changes in children's healthcare visits during coronavirus disease‐2019 pandemic in Hangzhou. China. J Pediatr. 2020;224:146‐149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Kadambari S, Abo YN, Phuong LK, Osowicki J, Bryant PA. Decrease in infection related hospital admissions during COVID‐19: why are parents avoiding the doctor? Pediatr Infect Dis J. 2020;39(11):e385‐e386. [DOI] [PubMed] [Google Scholar]
- 13. Scaramuzza A, Tagliaferri F, Bonetti L, et al. Changing admission patterns in paediatric emergency departments during the COVID‐19 pandemic. Arch Dis Child. 2020;105(7):704‐706. [DOI] [PubMed] [Google Scholar]
- 14. Schull MJ, Stukel TA, Vermeulen MJ, et al. Effect of widespread restrictions on the use of hospital services during an outbreak of severe acute respiratory syndrome. CMAJ. 2007;176(13):1827‐1832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Smith AC, Thomas E, Snoswell CL, et al. Telehealth for global emergencies: Implications for coronavirus disease 2019 (COVID‐19). J Telemedicine Telecare. 2020;26(5):309‐313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Keshet A, Gavrieli A, Rossman H, et al. The effect of a national lockdown in response to COVID‐19 pandemic on the prevalence of clinical symptoms in the population. 10.1101/2020.04.27.20076000 [DOI]
- 17. Berkun Y, Padeh S. Environmental factors and the geoepidemiology of juvenile idiopathic arthritis. Autoimmun Rev. 2010;9(5):A319‐A324. [DOI] [PubMed] [Google Scholar]


