Abstract
Objectives
This study examines perceived and anticipated stigma towards infected people, threat and impact appraisals of the COVID‐19 pandemic as well as distressing personal experiences related to the virus in order to determine the extent to which they directly and indirectly predict hedonic and eudaimonic well‐being. Investigated experiences included exposure to COVID‐19‐related news, having being in close proximity to people with a COVID‐19 diagnosis or with COVID‐19‐like symptoms, having being sick or having suffered COVID‐19‐like symptoms, having tested negative for COVID‐19.
Methods
Adults from northern Italy (n = 326; M age = 29.86) provided cross‐sectional data through an online survey during the nationwide lockdown period. Structural equation modelling analyses were conducted.
Results
Perceived and anticipated stigma, exposure to COVID‐19 news, perceived threat and impact on material resources access were negatively and indirectly related to both hedonic and eudaimonic well‐being via perceived COVID‐19 psychological impact which served as a mediator. Perceived stigma was also directly and negatively related to hedonic and eudaimonic well‐being, whereas having tested negative for COVID diagnosis was positively and directly associated with eudaimonic well‐being.
Conclusions
COVID‐19‐related stigma and appraisals can impair positive feelings about life as well as the pursuit of self‐realization and the search for meaning in life. The findings highlight the importance of developing psychological preventive and rehabilitative interventions to help people cope with these risk factors.
Keywords: appraisals, COVID‐19, eudaimonia, hedonia, impacts, psychological well‐being, stigma, threat
Statement of contribution.
What is already known on this subject?
Studies on the psychological implications of pandemics show a wide variety of mental health correlates.
Socio‐demographics, health status, news exposure and vulnerability perceptions are linked to COVID‐19‐related mental distress.
What does this study add?
The study focuses on both hedonic and eudaimonic well‐being during the early stages of the COVID‐19 pandemic.
It shows that a variety of factors (e.g., stigma, appraisals, personal experiences) are related to well‐being.
It was conducted in northern Italy, which was the centre of the pandemic in Europe.
Background
The novel coronavirus (SARS‐CoV‐2) has infected over 76 million individuals with 1,694,000 deaths worldwide since the beginning of 2020 (European Centre for Disease Prevention & Control, 2020). To minimize the spread of the virus, most governments have implemented quarantines and physical distancing measures, which have changed daily life in numerous ways. Many isolated and quarantined people have difficulty accessing basic necessities, are unable to work from home with subsequent loss of job‐related income, experience a sharp reduction in personal freedoms and social interactions resulting in increasing feelings of loneliness, frustration, and anger (Brooks et al., 2020; Xiang et al., 2020). Another feeling aroused by the pandemic is fear of contagion that has been shown to have an important role in motivating use of protective behaviours to avoid infection (Rubaltelli, Tedaldi, Orabona, & Scrimin, 2020). However, it can also turn into panic when individuals are affected by COVID‐19‐like symptoms or have been in close proximity with someone who has had these symptoms, as documented by cases of people who committed suicide because of the mistaken belief that they had been infected by COVID‐19 (Goyal et al., 2020; Mamun & Griffiths, 2020).
Like many other prolonged life‐threatening situations, the COVID‐19 pandemic is likely to have both short‐ and long‐effects on well‐being. A few longitudinal studies using representative adult samples have recently documented a significant increase of mental health problems in the United Kingdom and United States as a result of the COVID‐19 pandemic. Specifically, compared to pre‐COVID‐19 levels, adults (especially if females or young adults) showed higher levels of distress and depression when the pandemic broke out and the first lockdown restrictions were imposed (Daly, Sutin, & Robinson, 2020, 2021; Pierce et al., 2020). Yet, distress declined and sometimes returned to its baseline levels within a couple of months, suggesting some resilience among the sampled population (Daly & Robinson, 2020; Daly, Sutin, & Robinson, 2020). The observed effects were independent of previous mental health diagnoses (Daly & Robinsons, 2020).
A factor also likely to negatively impact psychological well‐being during the current pandemic is the stigmatization of people infected by the virus and of those who had been quarantined or simply shared social or behavioural characteristics with COVID‐19 patients (Brooks et al., 2020; Bruns, Kraguljac, & Bruns, 2020; Liu, Finch, Brenneke, Thomas, & Le, 2020; UNAIDS, 2020). Stigma can be defined as a mark of disgrace that sets a person apart from others and conveys a social identity which is devalued in a particular social context (Goffman, 1963; Link & Phelan, 2006). According to the Health Stigma and Discrimination Framework (Stangl et al., 2019), stigma associated with health conditions manifests in a wide range of experiences: The prejudice and discrimination actually experienced by stigmatized group members in their community (enacted stigma), the stigmatized group members’ endorsement of negative societal beliefs and feelings associated with their stigmatized status (internalized stigma), the perceptions about how the stigmatized group is treated in a given context (perceived stigma), and the expectations of being prejudiced, discriminated, and stereotyped by others in the future if their health condition worsens and/or becomes known (anticipated stigma).
Stigma related to physical illness often reveals itself in social avoidance and rejection, especially if illnesses are severe, contagious, caught by behaviour and avoidable (Crandall & Moriarty, 1995), as COVID‐19 is. Additionally, stigma directed at people infected by contagious and threatening diseases boosts the desire to physically and socially distance from them (Earnshaw & Quinn, 2013; Tomczyk, Rahn, & Schmidt, 2020) and can be over‐inclusive by targeting non‐diseased individuals (Park, van Leeuwen, & Chochorelou, 2013). Therefore, the perception of excessive social avoidance during the COVID‐19 pandemic can be informative of COVID‐19‐related perceived stigma. Also, given that infectious diseases are often attributed to irresponsible behaviours (Crandall & Moriarty, 1995; Logie, 2020), people may expect to be negatively judged by others and to self‐blame if they get sick with COVID‐19, thereby experiencing anticipated stigma related to COVID‐19 (Earnshaw et al., 2020).
All these COVID‐19‐related experiences can evoke intense emotional responses such as fear, perceived threat and distress, especially when they are amplified by negative cognitions and perceptions. Stress and coping theory posits that it is the perception of the event as stressful and life‐threatening, rather than the event itself, that ultimately determines its outcomes (Lazarus & Folkman, 1984). In fact, appraisals of SARS as threatening and having large negative effects on many aspects of life were associated with reports of poor health and adjustment (Cheng, Wong, & Tsang, 2006; Cheng, Chong, et al., 2006).
Appraisals of COVID‐19 are likely to be related to media exposure. According to Media Dependency Theory, people become more dependent on media to satisfy their information need when ambiguity escalates due to a threatening condition like a health crisis (Ball‐Rokeach & DeFleur, 1976). Thus, the more individuals perceive an epidemic as threatening, the more they search for accurate and up‐to‐date information regarding its spread and prevention through media sources (Tai & Sun, 2007). However, in the absence of clear information on the disease (whether because of lack of medical knowledge or because of ineffective communication of what is known) and because of appeals to change behaviour based on fear, media reports can paradoxically lead to heightened appraisals of threat, increased worry, and psychological distress (Garfin, Silver, & Holman, 2020; Olagoke, Olagoke, & Hughes, 2020).
Existing evidence regarding the impact of COVID‐19 tends to conceptualize and measure well‐being in terms of the absence of mental disorders or negative affective states. But psychological well‐being is not simply the absence of psychological distress. Despite definitional variability (Delle Fave, 2014), psychological well‐being is commonly conceptualized as a ‘combination of feeling good and functioning effectively’ (Huppert, 2009, p. 137). The concept of feeling good (or subjective well‐being) refers to experiencing positive emotions instead of negative ones (Fredrickson, 2001) and to positive judgements and satisfaction with one’s life (Diener & Ryan, 2009). The concept of functioning effectively involves the development of one’s potential, having some control over one’s life, having a sense of purpose and self‐growth, being autonomous, and experiencing positive relationships (Ryff & Singer, 2008). These two concepts reflect Deci and Ryan’s (2008) distinction between hedonic and eudaimonic approaches to well‐being (Waterman, 2008). Hedonia focuses on subjective cognitive‐affective experiences of well‐being, whereas Eudaimonia reflects positive orientation and functioning which lead to success in the face of life’s existential challenges (Huta & Waterman, 2014).
Although Zacher and Rudolph (2020) showed that hedonic well‐being decreased across the early stages of the COVID‐19 pandemic in Germany, especially among people more prone to develop negative stress appraisals, eudaimonic well‐being during the pandemic has not yet been investigated. Keyes (2007) defined mental health (or flourishing) as a combination of high hedonic and eudaimonic well‐being. Therefore, the present research investigated both hedonic and eudaimonic well‐being in the context of the COVID‐19 pandemic and several risk factors that might predict it. These included the following: perceived and anticipated stigma towards infected people, appraisals of COVID‐19 threat and impact on finances, material resources access and mental health, exposure to COVID‐19 news, having being in close proximity to people with a COVID‐19 diagnosis or with COVID‐19‐like symptoms, having being sick or having suffered COVID‐19‐like symptoms during the pandemic, and having tested negative for COVID‐19. These variables were examined in subjects who lived in northern Italy, which was the first European district to be severely affected by the COVID‐19 pandemic and is currently the European country with the first largest number of COVID‐19 deaths and the third largest number of cases.
Most people perceive that the COVID‐19 pandemic is causing a significant deterioration in their psychological well‐being. This perception may function as a mechanism that links the many risk factors identified earlier to hedonic and eudaimonic well‐being. The hypothesized mediational model appears in Figure 1.
Figure 1.
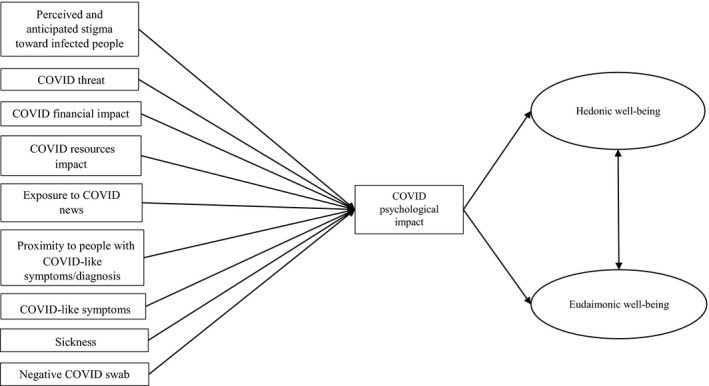
The hypothesized mediational model. Note. All the exogenous variables were correlated.
Materials and methods
Participants
Participants (n = 332) were adults from northern Italy (98.2%), 6 (1.8%) of whom had tested positive for COVID‐19 and were subsequently removed to have a homogenous sample with respect to diagnosis. The final sample consisted of 326 subjects, 248 females (76.1%) and 78 males (23.9%), aged between 19 and 73 years (M = 29.86; SD = 12.74). More than half the participants (55.5%) had a high school degree, 24.8% obtained a bachelor’s degree, 13.5% obtained a master’s degree, and 3.7% had an educational level equal to the secondary school diploma. Most participants (40.2%) were full‐time students, 26.4% were employed full‐time, 6.7 % were employed part‐time, and 16.5% were part‐time students having occasional or part‐time jobs. Among the workers (168 subjects), approximately half (51.2%) kept on working during the lockdown (60.5% of whom were telecommuting), 32.5% were temporarily unemployed (75% of whom received unemployment benefits), and 9.3% lost their job due to COVID‐19.
Procedure
Participants were contacted through an invitation message posted on social networks (e.g., Facebook, LinkedIn) and sent by instant messaging apps (e.g., WhatsApp) or messaging platform (e.g., Messenger). The invitation indicated that the purpose of the study was to examine the effects of the COVID‐19 outbreak on personal well‐being and that participants had to be Italian and at least 18 years old. Participants were then invited to complete an anonymous questionnaire, which took approximately 30 min and was implemented online using the Google Forms platform. In order to ensure that the participants did not respond more than once, the platform allowed access to the questionnaire only to subjects with a Google account, which are the large majority of people having an e‐mail account in Italy.
Data were collected in 2 weeks between April and May 2020 during the ‘lockdown’ period, when mandatory restrictive measures were applied throughout Italy. These measures mandated staying at home and leaving only for food and medical necessities, remote instruction for schools and universities, shutting business (except for food, healthcare, and IT industries) or working from home, and avoiding physical proximity to non‐cohabiting others. During the data collection period, over 21,000 Italians were diagnosed with COVID‐19 and 3,900 died after being infected.
All participants were treated according to the ethical guidelines established by the Italian Psychological Association (AIP, 2015). These guidelines include obtaining informed consent from participants, maintaining ethical treatment and respect for their rights, and ensuring the privacy of participants and their data.
Measures
Participants completed an anonymous questionnaire that measured the variables of interest.
COVID‐19 threat, impact, and experiences
COVID‐19 threat and impact appraisals and experiences were assessed using short versions of the Perceived Coronavirus Threat Questionnaire, Coronavirus Impacts Questionnaire, and Coronavirus Experiences Questionnaire (Conway, Woodard, & Zubrod, 2020). The short versions of the questionnaires were preferred over the long ones because they required less time and have equally good psychometric properties (Conway et al., 2020).
The Perceived Coronavirus Threat Questionnaire includes three items concerning how threatened or worried respondents were about COVID‐19 (e.g., ‘Thinking about COVID‐19 makes me feel threatened’). The Coronavirus Impacts Questionnaire is made up of 6 items divided into 3 scales: The Financial impact scale has 2 items (e.g., ‘From a financial point of view the COVID‐19 has had a negative impact on me’); the Resource impact scale evaluated access to material resources using 2 items (e.g., ‘I have had a hard time getting needed resources (food, toilet paper) due to the COVID‐19’); and the Psychological impact scale evaluates the impact of the virus on mental health using 2 items (e.g., ‘The COVID‐19 outbreak has impacted my psychological health negatively’). The Coronavirus Experiences Questionnaire includes three scales: The Proximity to others scale evaluates whether subjects came into contact with persons diagnosed with COVID‐19 or similar symptoms and comprised 2 items (e.g., ‘I have been in close proximity with someone who has been diagnosed with COVID‐19 in the last three months’); the 2 item News scale measured exposure to news/information related to COVID‐19 (e.g., ‘I watch a lot of news on COVID‐19’); the Personal diagnoses/symptoms scale comprises 3 items, assessing whether the participants contracted the virus, experienced symptoms similar to those of COVID‐19 or had been sick with something other than the COVID‐19 (e.g., ‘I had COVID‐19‐like symptoms at some point in the last three months), to which we added one further ad hoc item assessing whether the respondent had tested negative for COVID‐19 (e.g., ‘I have tested negative for one or more swabs for COVID‐19 diagnoses’).
The response format for all scales was a 7‐point Likert‐type scale ranging from 1 (definitely disagree) to 7 (definitely agree), except for the Personal diagnoses/symptoms and the Proximity to other scales whose response format was dichotomous (0 = no; 1 = yes).
Confirmatory factor analysis on our data replicated the original scales detected by Conway et al. (2020), with the exception of the Personal diagnoses/symptoms scale, where factor loadings were poor (item inter‐correlations ≤ .28). With the Personal diagnoses/symptoms items removed, the factorial model showed a good fit, S‐Bχ2(55) = 100.290, p = .000, R‐CFI = .963; R‐RMSEA = .050, with all factor loadings greater than .50 and factor correlations between .00 and .35. Except for the Personal diagnoses/symptoms scale, all scales showed good internal reliability in the present study (Perceived threat: α = .85; Financial impact: α = .81; Resource impact: α = .71; Psychological impact: α = .83; Proximity to others: α = .75; News exposure: α = .76). Consequently, a composite score was formed for each scale by averaging item scores, with the exception of the four Personal diagnoses/symptoms items which were not merged in an overall index.
COVID‐19 perceived and anticipated stigma
Given the lack of a validated measure of COVID‐19‐related stigma at the time of data collection, we turned to the extensive literature on HIV‐related stigma to develop measures assessing COVID‐19‐related stigma.
Perceived stigma was investigated via 3 items adapted from the Distancing subscale of the HIV Stigma Scale by Sowell et al. (1997) and Emlet (2005). The adapted items reflect the perception of being avoided and rejected during daily activities among healthy people, beyond compliance with social distancing measures (e.g., ‘Thinking back to the last months when the COVID spread in Italy, how often did you feel…I felt that people were uncomfortable being with me, even if I kept social distancing’). Response scales were anchored at 1 (not at all) and 4 (often). A composite score for Perceived social avoidance was obtained by averaging the three items (α = .88).
Nine more items assessed anticipated stigma. The items asked participants to imagine being COVID‐positive and the extent to which they would experience negative self‐image, self‐blame, disclosure, and negative social judgement concerns (for a similar procedure see Bunn, Solomon, Miller, & Forehand, 2007; Earnshaw et al., 2020; Kalichman et al., 2009). Participants were asked to answer each item on a Likert scale ranging from not at all (1) to very much (5). An Exploratory factor analysis (EFA) using principal axis factoring extraction with direct Oblimin rotation yielded a two‐factor solution, explaining 58.35% of the total variance. Factor 1 (eigenvalue = 4.7) accounted for 47.5% of total variance and included 5 items concerning anticipated negative social judgement (α = .87; e.g., ‘It would be difficult for me telling it to other people’). Factor 2, (eigenvalue = 1.29), accounted for 10.8% of total variance and included 2 items concerning anticipated self‐blame (α = .82; e.g., ‘I would feel guilty’). All factor loadings were above |.60|. We therefore computed two scores: one for ‘Anticipated negative social judgement’ and one for ‘Anticipated self‐blame’.
Psychological well‐being
Participants’ psychological well‐being was assessed using the Psychological General Well‐Being Index (PGWBI) and the Psychological Well‐Being (PWB) scales.
The PGWBI (Dupuy, 1984), used in clinical trials and epidemiological research, provides a general evaluation of self‐perceived psychological health and well‐being in the past 4 weeks. This scale measures well‐being not only in terms of absence of pain and negative affective states (e.g., being bothered by aches, being depressed, nervous, worried or tired), but also in terms of life satisfaction and presence of positive mood experiences (e.g., being happy with one’s personal life, having a daily life full of interesting things, being in good spirits, feeling full of energy and healthy, cheerful, emotionally stable), consistent with a hedonic conceptualization of well‐being.
The validated Italian short version of the scale (Grossi et al., 2006) comprises 22 polytomous items with scores ranging from 0 to 5 and covers 6 underlying domains: Anxiety (5 items, e.g., ‘Have you been anxious, worried, or upset during the past month?’), Depressed mood (3 items, e.g., ‘Did you feel depressed during the past month?’), Positive well‐being (4 items, e.g., ‘How happy, satisfied, or pleased have you been with your personal life during the past month?’), Self‐control (3 items, e.g., ‘I was emotionally stable and sure of myself during the past month’), General health (3 items, e.g., ‘How often were you bothered by any illness, bodily disorder, aches or pains during the past month?’), and Vitality (4 items, e.g., ‘How much energy, pep, or vitality did you have or feel during the past month?’). Cronbach’s alpha was adequate in the present study, ranging from .70 to .88, for all subscales with the exception of General health (α = .38). Except for General health, whose items were kept separate, a composite score was obtained for each subscale by summing the item scores and giving them a range of 0 to 100 in order to facilitate comparison across dimensions and studies. Higher scores indicate greater psychological well‐being, mostly evaluated in regard to its hedonic components.
The PWB scales (Ryff & Keyes, 1995) investigate eudaimonic psychological well‐being and have been validated in Italy (Ruini, Ottolini, Rafanelli, Ryff, & Fava, 2003). All dimensions of the 42‐item version of the scale were used (Self‐acceptance, Self‐growth, Purpose in life, Positive relations with others, Environmental mastery), except for Autonomy. Answers were provided on a 6‐point Likert scale, ranging from 1 (definitely disagree) to 6 (definitely agree). Self‐acceptance assesses positive attitude towards oneself and the awareness of one’s positive and negative qualities (7 items, e.g., ‘In general, I feel confident and positive about myself’); self‐growth evaluates the sense of continuous growth, expansion, and open‐mindedness to experiences and fulfilment of one’s potential (7 items; e.g., ‘I have the sense that I have developed a lot as a person over time’); purpose in life evaluates the presence of a goal and a sense of direction towards life (7 items, one of which was omitted in the present study because it was not consistent with others; e.g., ‘Some people wander aimlessly through life, but I am not one of them’); positive relations with others assesses trust in people, ability to feel empathy, affection, and ability to create intimate relationships (7 item; e.g., ‘I know that I can trust my friends, and they know they can trust me’). Environmental mastery measures the ability to control the surrounding environment and the management of a wide range of activities by taking advantage of the opportunities (7 items; e.g., ‘I am quite good at managing the many responsibilities of my daily life’). Cronbach’s alpha was adequate in the present study, ranging from .75 to .87, for all subscales. A composite score was obtained for each subscale by averaging item scores so that higher scores indicate greater eudaimonic well‐being.
Data analysis
To test our mediational model, we used structural equation modelling (SEM) with latent constructs for hedonic and eudaimonic dimensions of well‐being (EQS6.2; Bentler, 2008). Composite scores served as manifest indicators for the two latent constructs; as it was not possible to summarize them in a composite score, the three PGWBI physical health items were entered as manifest indicators for the PGWBI latent construct. For all the remaining variables, we used composite scores as measured constructs.
Inspection of Mardia’s (1970) coefficients suggested significant deviations from multivariate normality; to reduce the impact of non‐normality, we relied on Satorra and Bentler (2001) scaled estimates in rescaling the standard errors and the chi‐square statistics into the Satorra–Bentler scaled chi‐square (S–B χ2) statistic. Fit indexes such as the comparative fit index (CFI; Bentler, 1990) and the root‐mean‐square error of approximation (RMSEA; Bentler, 2008) were also adjusted for non‐normality by incorporating the S–B χ2 into their calculations. We refer to them as robust estimates (i.e., R‐CFI, R‐RMSEA).
To evaluate mediation, we inspected the significance of indirect effects. We used the multivariate Lagrange multiplier (LM) test (Bentler, 2008) to test whether our full mediational model provided a better fit to the data than alternative partial mediational models, in which direct paths from exogenous measured variables to the outcome latent constructs were added. The Akaike information criterion adjusted for scaling (R‐AIC) was also used to compare the fit of competing models (Akaike, 1987). The model with the smallest AIC value among the models tested is the preferred model.
Finally, a power analysis was conducted to determine whether the study sample size was appropriate for the planned analyses. Since the sample size required for SEM depends on multiple factors not considered in rule‐of‐thumbs guidelines (i.e., the number of latent factors, the number of indicators, and the magnitude of factor loadings and correlations; Wolf, Harrington, Clark, & Miller, 2013), we used the pwrSEM app on Shiny (Wang & Rhemtulla, in press) based on Monte Carlo simulation with 10,000 repetitions to estimate the power for the regression paths in our hypothesized model. The factor loadings of PGWBI and of PWB were, respectively, set at .66 and at .80 so as to reflect the scales’ overall reliability in previous studies. When residual covariance for endogenous variables was set at .30, results revealed that, with the sample size of 326 and alpha level of .05, the test has at least 80% power to detect direct effect sizes equal to or larger than .16 and indirect effect sizes equal to or larger than .04.
Results
Preliminary analyses
All variables were normally distributed except for three: having been tested negative for COVID‐19 swab, PGWBI depression, and having felt healthy enough to do things (one of the three PGWBI physical health items), whose skewness/kurtosis was above |2|.
Descriptive statistics (see Table 1) indicated that on average participants felt quite threatened by COVID‐19 and were somewhat negatively affected by it. Repeated measures ANOVA and post‐hoc tests using the Bonferroni correction, F(1.820, 591.397) = 47.887, p = .000, revealed that participants perceived themselves to be more negatively affected by COVID‐19 financially (M = 3.52) than psychologically (M = 2.76, p = .000), and more psychologically affected than in their ability to access material necessities (M = 2.36, p = .000). Also, 26% of participants reported having had COVID‐19‐like symptoms and to have been sick since the beginning of the outbreak in Italy, 43% indicated that they had been in close proximity with someone who had COVID‐19‐like symptoms, whereas 16% stated that they had been in close proximity with someone who was diagnosed with COVID‐19 and only 5% tested negative for one or more swabs for a COVID‐19 test.
Table 1.
Descriptive statistics and Pearson’s correlations among the variables
| M | SD | Range | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | 17 | 18 | 19 | 20 | 21 | 22 | 23 | 24 | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Stigma | ||||||||||||||||||||||||||||||
| 1. Perceived social avoidance | 1.93 | 0.82 | 1–4 | – | ||||||||||||||||||||||||||
| 2. Anticipated self‐blame | 2.25 | 1.27 | 1–5 | .18 | – | |||||||||||||||||||||||||
| 3. Anticipated negative social judgement | 2.47 | 1.10 | 1–5 | .14 | .44 | – | ||||||||||||||||||||||||
| COVID | ||||||||||||||||||||||||||||||
| 4. Threat | 4.21 | 1.51 | 1–7 | .05 | .20 | .24 | – | |||||||||||||||||||||||
| 5. Financial impact | 3.52 | 2.07 | 1–7 | .17 | .14 | .10 | .17 | – | ||||||||||||||||||||||
| 6. Resources impact | 2.36 | 1.45 | 1–7 | .14 | .13 | .12 | .18 | .18 | – | |||||||||||||||||||||
| 7. Psychological impact | 2.76 | 1.64 | 1–7 | .21 | .25 | .20 | .32 | .31 | .18 | – | ||||||||||||||||||||
| 8. Exposure to C news | 3.13 | 1.59 | 1–7 | −.01 | −.07 | .03 | .23 | .02 | .07 | .19 | – | |||||||||||||||||||
| 9. C‐like symptoms | .26 | .44 | 0–1 | .10 | −.01 | .03 | .03 | .00 | .07 | .05 | −.05 | – | ||||||||||||||||||
| 10. Sickness | .26 | .44 | 0–1 | .11 | −.01 | .03 | .12 | .00 | .00 | .02 | −.06 | .28 | – | |||||||||||||||||
| 11. Proximity to people with C. diagnosis/symptoms | .30 | .36 | 0–1 | .12 | −.04 | .05 | .04 | 04 | .07 | .12 | .06 | .25 | .06 | – | ||||||||||||||||
| 12. Negative C swab | .05 | .22 | 0 −1 | .02 | −.05 | .10 | .03 | −.01 | .01 | −.07 | .00 | .03 | .03 | .07 | – | |||||||||||||||
| PGWBI | ||||||||||||||||||||||||||||||
| 13. Lack of illness | 3.86 | 1.06 | 0–5 | −.06 | −.13 | −08 | −.12 | −.06 | −.05 | −.08 | .06 | −.11 | −.15 | −.06 | .03 | – | ||||||||||||||
| 14. Healthy enough to do things | 4.00 | .87 | 0–5 | −.17 | −.04 | .01 | .07 | −.01 | .00 | −07 | .05 | −.06 | .02 | .01 | .05 | .19 | – | |||||||||||||
| 15. Lack of health concern | 2.95 | 1.11 | 0–5 | −.11 | −07 | −.07 | −.22 | −.06 | −.02 | −.23 | −.10 | −.03 | −.05 | .03 | .04 | 19 | .09 | – | ||||||||||||
| 16. Anxiety | 59.31 | 19.91 | 0–100 | −.13 | −.15 | −.10 | −.09 | −.07 | −.07 | −.24 | −.10 | .03 | .01 | −.02 | .04 | .29 | .30 | .44 | – | |||||||||||
| 17. Depressed mood | 77.22 | 16.51 | 6.67–100 | −.17 | −.19 | −.16 | −.04 | −.11 | −.07 | −.27 | −.08 | −.01 | .02 | −.01 | .06 | .21 | .40 | .24 | .69 | – | ||||||||||
| 18. Positive well‐being | 46.99 | 16.37 | 5–100 | −.15 | −.13 | −.08 | −.06 | −.09 | −.05 | −.23 | −.14 | .01 | .02 | −.01 | .05 | 22 | .31 | .26 | .63 | .70 | – | |||||||||
| 19. Self‐control | 67.01 | 19.58 | 0–100 | −.17 | −.16 | −.09 | −.05 | −.11 | −.12 | −.23 | −.08 | .00 | .04 | −.05 | .03 | .21 | .37 | .27 | .70 | .68 | .66 | – | ||||||||
| 20. Vitality | 57.36 | 17.47 | 5–100 | −.18 | −.14 | −.05 | −.03 | −.07 | −.12 | −.25 | −.08 | −.04 | .02 | −.06 | .12 | .30 | .38 | .30 | .69 | .73 | .78 | .69 | – | |||||||
| PWB | ||||||||||||||||||||||||||||||
| 21. Environmental mastery | 4.14 | .91 | 1.29–6 | −.18 | −.25 | −.27 | −.11 | −.22 | −.09 | −.39 | −.06 | −.11 | −.10 | −.04 | .09 | .15 | .06 | .14 | .19 | .25 | .21 | .22 | .25 | – | ||||||
| 22. Personal growth | 4.67 | .73 | 2.14–6 | −.10 | −.16 | −.11 | −.09 | −.12 | .05 | −.15 | −.12 | −.09 | −.07 | .01 | .03 | .04 | −.07 | .05 | .10 | .16 | .12 | .10 | .12 | .50 | – | |||||
| 23. Positive relations | 4.63 | .83 | 1.71–6 | −.05 | −.18 | −.19 | .01 | −.11 | −.02 | −.19 | . −05 | −.09 | .02 | .02 | .12 | .10 | .04 | .04 | .07 | .17 | .18 | .06 | .19 | .59 | .47 | – | ||||
| 24. Purpose in life | 4.30 | .94 | 1.67–6 | −.15 | −.22 | −.13 | .02 | −.11 | −.02 | −.20 | −.07 | .00 | .07 | −.04 | .09 | .12 | .02 | .08 | .16 | .26 | .22 | .16 | .25 | .71 | .49 | .52 | – | |||
| 25. Self‐acceptance | 3.96 | 1.06 | 1.14–6 | −.11 | −.25 | −.27 | −.07 | −.16 | −.06 | −.35 | −.12 | −.05 | −.01 | −.11 | .13 | .12 | −.03 | .11 | .19 | .28 | .26 | .22 | .25 | .76 | .49 | .62 | .64 | |||
Values greater than |.11|, |.15|, and |.19| are significantly different from zero, with a significance level alpha equal to .05, .01, and .001, respectively; these values are reported in bold characters.
C = COVID; PGWBI = Personal General Well‐Being Index; PWB = Personal Well‐Being scale.
When testing the effects of demographic variables on COVID‐19 stigma, appraisals and experiences through general linear model analyses, a few significant effects emerged. Specifically, older subjects felt slightly more threatened by COVID‐19 than younger subjects, F(1, 278) = 5.088, p = .028, = .018. Also, compared to full‐time workers (M = 3.30) and full‐time students (M = 3.58), part‐time workers and part‐time students having occasional or part‐time jobs judged the COVID‐19 financial impact as higher, M = 5.37 and 5.06; F(4, 278) = 4.909, p = .001, = .066.
In terms of psychological well‐being, participants reported quite low levels of positivity and vitality and rather high levels of anxiety. Compared with Italian mean values reported in the PGWBI user manual (Chassany, Dimenäs, Dubois, Wu, & Dupuy, 2004), the present sample had significantly lower mean values on all well‐being dimensions assessed, anxiety: Δ = −12.77, t(1,799) = 10.804, p = .000; depressed mood: Δ = −6.30, t(1,799) = 6.094, p = .000; positive well‐being: Δ = −15.68, t(1,799) = 14.032, p = .000; self‐control: Δ = −13.26, t(1,799) = 11.801, p = .000; vitality: Δ = −11.12, t(1,799) = 10.000, p = .000. Scores on items assessing physical health were also not high, especially the one evaluating health concerns and worries. Similarly, levels of eudaimonic well‐being were moderate, especially for self‐acceptance, reflecting positive evaluations of oneself and one's past life, and environmental mastery, indicating the capacity to effectively manage one's life and surrounding world.
All stigma indicators and some indexes referring to COVID‐19 appraisals and experiences (namely its perceived impact on finances and material resources access, the exposure to news on the virus, and having been in close proximity to people sick of it) were significantly associated in the expected direction to perceived COVID‐19 psychological impact (PCPI), which in turn was negatively related to all well‐being dimensions (see Table 1). Since partial correlations revealed that, after controlling for the remaining COVID‐related indicators, the scale assessing close proximity to persons diagnosed with COVID‐19 or having COVID‐like symptoms was unrelated to PCPI as well as to any of well‐being dimensions, the proximity to other indicator was excluded from subsequent analyses.
Mediational analyses
The hypothesized full mediational model, in which perceived and anticipated stigma, threat, impacts and experiences related to COVID‐19 were assumed to predict psychological well‐being indirectly through PCPI, was tested using SEM. Examination of fit indices showed a good fit between the proposed model and the data, S‐Bχ2(205) = 349.995, p = .000, R‐CFI = .934; R‐RMSEA = .047; R‐AIC = −60.005. However, the Lagrange multiplier test indicated that the model fit could be significantly improved by adding three paths: in two of them PWB was directly predicted by anticipated negative social judgement and negative COVID test results, whereas in the third PGWBI was directly predicted by perceived social avoidance. The final mediational model is reported in Figure 2, S‐Bχ2 (202) = 327.286, p = .000, R‐CFI = .944; R‐RMSEA = .044; R‐AIC = −76.715.
Figure 2.
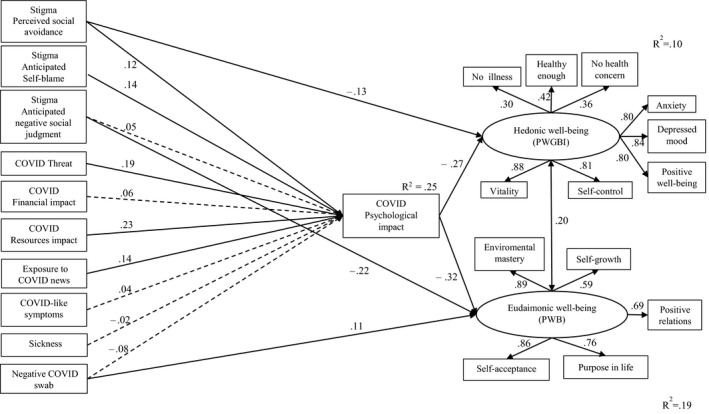
The final mediational model. Note. All the exogenous variables were correlated. Standardized coefficients are reported. All the coefficients associated with solid lines are significant, while those associated with dashed lines are not significant beyond the p < .05 level.
Direct and indirect paths were all significant and in the expected direction, except for the paths from COVID‐19 financial impact, COVID‐19‐like symptoms and sickness to PCPI (see Figure 2 and Table 2). Overall the model indicates that perceived social avoidance and anticipated self‐blame, COVID‐19 threat, COVID‐19 impact on material resources access, and exposure to COVID‐19 news uniquely predicted both hedonic and eudaimonic well‐being through the mediation of PCPI. Moreover, perceived social avoidance and fear of being judged negatively in case of COVID‐19 infection were directly and negatively related to hedonic and eudaimonic well‐being, respectively, whereas having been tested negative for one or more swabs for COVID‐19 was positively and directly associated with eudaimonic well‐being. The moderate association between PGWBI and PWB scales confirmed that the two questionnaires capture different aspects of personal well‐being.
Table 2.
Significant total effects (outside parentheses) and indirect effects (inside parentheses) resulting from the final mediational model
| Outcome variables | PGWBI | PWB | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Predictor variables | Overall (latent variable) | Lack of illness | Healthy enough to do things | Lack of health concern | Anxiety | Depressed mood | Positive well‐being | Self‐control | Vitality | Overall (latent variable) | Environmental mastery | Personal growth | Positive relations | Purpose in life | Self‐acceptance |
| Stigma | |||||||||||||||
| Perceived social avoidance | −.16 (−.03) | −.05 (−.05) | .07 (.07) | −.06 (−.06) | −.13 (−.13) | −.14 (−.14) | −.14 (−.14) | −.13 (−.13) | −.14 (−.14) | −.04 (−.04) | −.03 (−.03) | −.02 (−.02) | −.03 (−.03) | −.03 (−.03) | −.03 (−.03) |
| Anticipated self‐blame | −.04 (−.04) | −.01 (−.01) | .02 (.02) | −.01 (−.01) | −.03 (−.03) | −.03 (−.03) | −.03 (−.03) | −.03 (−.03) | −.03 (−.03) | −.05 (−.05) | −.04 (−.04) | −.03 (−.03) | −.03 (−.03) | −.04 (−.04) | −.04 (−.04) |
| Anticipated negative social judgement | – | – | – | – | – | – | – | – | – | −.23 | −.21 (−.21) | −.14 (−.14) | −.16 (−.16) | −.18 (−.18) | −.20 (−.20) |
| COVID | |||||||||||||||
| Threat | −.05 (−.05) | −.02 (−.02) | .02 (.02) | −.02 (−.02) | −.04 (−.04) | −.04 (−.04) | −.04 (−.04) | −.04 (−.04) | −.05 (−.05) | −.06 (−.06) | −.06 (−.06) | −.04 (−.04) | −.04 (−.04) | −.05 (−.05) | −.05 (−.05) |
| Financial impact | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – |
| Resources impact | −.06 (−.06) | −.02 (−.02) | .03 (.03) | −.02 (−.02) | −.05 (−.05) | −.05 (−.05) | −.05 (−.05) | −.05 (−.05) | −.05 (−.05) | −.07 (−.07) | −.07 (−.07) | −.04 (−.04) | −.05 (−.05) | −.06 (−.06) | −.06 (−.06) |
| Psychological impact | −.27 | −.08 (−.08) | .11 (.11) | −.09 (−.09) | −.21 (−.21) | −.22 (−.22) | −.22 (−.22) | −.21 (−.21) | −.23 (−.23) | −.32 | −.29 (−.29) | −.19 (−.19) | −.22 (−.22) | −.25 (−.25) | −.28 (−.28) |
| Exposure to C news | −.04 (−.04) | −.01 (−.01) | .02 (.02) | −.01 (−.01) | −.03 (−.03) | −.03 (−.03) | −.03 (−.03) | −.03 (−.03) | −.03 (−.03) | −.05 (−.05) | −.04 (−.04) | −.03 (−.03) | −.03 (−.03) | −.04 (−.04) | −.04 (−.04) |
| C‐like symptoms | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – |
| Sickness | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – |
| Negative C swab | – | – | – | – | – | – | – | – | – | .14 | .12 (.12) | .08 (.08) | .09 (.09) | .11 (.11) | .12 (.12) |
Values reported refer to standardized effects significant at p < .05.
When total effects (indirect + direct effects) on well‐being outcomes were considered (see Table 2), hedonic psychological well‐being was more strongly and negatively predicted by PCPI and by perceived social avoidance. In comparison, eudaimonic well‐being was more strongly and negatively predicted by PCPI and by the fear of being socially reproached, but was positively related to having been tested negative for COVID‐19. The propensity to self‐blame in case of COVID‐19 infection, COVID‐19 threat, COVID impact on resources access, and exposure to COVID‐19 news were also uniquely and significantly related to hedonic and eudaimonic well‐being dimensions, but their effects were weaker.
The above findings were unaffected by subjects’ age and occupation, which preliminary descriptive analyses had shown to relate to COVID‐19 threat and financial impact. In fact, when age and occupation where entered in our final mediational model as exogenous variables predicting PCPI, the model fit was equally good, S‐Bχ2(267) = 417.184, p = .000, R‐CFI = .951; R‐RMSEA = .042; R‐AIC = −116.816, and all the direct and indirect paths which were previously significant remained unchanged in their strength. Although it should be interpreted with caution due to the low ratio of parameters to subjects, this new model controlling for age and occupation also indicated that, compared to people in other working conditions, full‐time employees reported significantly lower PCPI (β = −.18) and indirectly experienced higher hedonic and eudaimonic well‐being (β = .05 and .06).
Discussion
Informed by stigma and appraisal literatures, this study investigated COVID‐19 stigma, appraisals, and distressing personal experiences related to the virus and their relations to hedonic and eudaimonic psychological well‐being, among adults from northern Italy, one of the areas in Europe most stricken by COVID‐19. Participants indicated that they felt quite threatened by COVID‐19 (especially if middle‐aged and older), were somewhat negatively affected by it and quite exposed to news on it. They also expected to be somewhat negatively judged and to blame themselves in the event of contracting COVID‐19.
Structural equation modelling showed that the more subjects expected to be avoided and to self‐blame in case of COVID‐19 diagnosis, felt the pandemic threatened them and prevented them from finding basic necessities and were exposed to news on it, the more they perceived the pandemic had a negative impact on their psychological health which, in turn, was negatively related to their hedonic and eudaimonic psychological well‐being. However, contrary to our predictions, the perceived impact of COVID‐19 on finances, and potentially distressing experiences, like having been sick or affected by COVID‐19‐like symptoms or having been physically proximate to people diagnosed with COVID‐19 or having COVID‐19‐like symptoms, were not uniquely related to psychological well‐being, either directly or through the mediation of PCPI. The lack of significant relations between perceived financial impact and psychological well‐being might be due to the fact that participants were mostly full‐time university students living with their family of origin without burdensome financial responsibilities or full‐time workers who went on working during the quarantine period (telecommuting) or, if not, received unemployment benefits, and therefore experiencing small reductions in income. Accordingly, our analyses indicated that full‐time students and full‐time employees were less negatively impacted by the pandemic from a financial point of view.
As regards potentially threatening experiences related to being sick or in close proximity to sick people, these factors might be more distal predictors of psychological well‐being compared to COVID‐19 perceived threat or stigma for being infected; even though not particularly strong, the correlations found between these variables are in line with this possible explanation.
In addition, structural equation modelling indicated that perceived social avoidance and fear of being judged negatively in the event of COVID‐19 infection were directly and negatively related to hedonic and eudaimonic well‐being, respectively. In contrast, having tested negative for COVID was positively and directly associated with eudaimonic well‐being. The existence of these direct links suggests that there are aspects of the COVID‐19 pandemic whose impacts on psychological well‐being are not commonly perceived. Specifically, the negative effects of perceived stigma towards potentially infected people and the positive effects of testing negative for COVID‐19 on psychological well‐being seem undervalued. Although the effects of stigma on eudaimonic well‐being have so far rarely been investigated, our results are consistent with some evidence showing that perceived stigma and discrimination are inversely related to eudaimonic dimensions of well‐being, like mastery, meaning in life, and self‐acceptance (Brown, 2017; Ehrlich‐Ben Or et al., 2013; Ryff, Keyes, & Hughes, 2003). The results are also in line with a meta‐analysis showing that stigma does have an observable association with the stigmatized groups’ mental health (Mak, Poon, Pun, & Cheung, 2007). Specifically, the meta‐analysis indicated that, across stigmatized conditions, stigma had a stronger relationship with positive mental health indicators than with negative indicators. Given that mental health is not merely the absence of mental illness or distress, this pattern of relationships suggested that stigma has a stronger negative effect on adjustment and growth than an exacerbating effect on psychological distress.
Overall, the present results provide initial evidence that COVID‐19‐related stigma, appraisals and experiences can negatively influence not only positive feelings about life, but also the pursuit of self‐realization and the search for meaning (Deci & Ryan, 2008).
Limitations and future directions
This study recruited participants through online communities and messaging platforms and collected self‐report data using an online survey. These methods, which allow collection of data from a large number of people in a short time, were preferred to reduce the risk that changes in the containment measures and in the evolution of the epidemic could occur during the data collection and affect our results. However, they have several limitations, including the inaccurate reporting, social desirability biases and the underrepresentation of people not familiar with social media, like elders or those suffering severe mental disturbance. Even if statistical power analysis showed that our sample was large enough to capture quite small direct and indirect effects, bigger samples are needed to replicate the current findings, given the complexity of the mediational model estimated.
Second, given the lack of validated measures on COVID‐19‐related stigma at the time the data were collected, we used prior research on stigma towards people with HIV/AIDS to inform our measures of stigma. However, it must be acknowledged that SARS and HIV viruses are very different in terms of vehicle of transmission and related stigma. Specifically, HIV is transmitted by sexual contact across mucosal surfaces, by maternal‐infant exposure, and by percutaneous inoculation (Shaw & Hunter, 2012), while transmission of SARS‐CoV‐2 occurs primarily via respiratory droplets from face‐to‐face contact and, to a lesser degree, via contaminated surfaces (Wiersinga, Rhodes, Cheng, Peacock, & Prescott, 2020). In this sense, people cannot control transmission of SARS‐CoV‐2 at the same level as they can control HIV transmission. Moreover, due to HIV transmission modes, on the onset of HIV epidemic many infected women were labelled as drug users or prostitutes and stigmatizing attitudes were developed towards specific groups that were believed to be disproportionately affected by the epidemic, such as gay and bisexual men, injecting drug users or sex workers (Bunting, 1996; Herek, Capitanio, & Widaman, 2002). Of course, this is not the case of COVID‐19‐related stigma.
Moreover, in this paper we did not take the viewpoint of infected people and investigate perceived stigma from their own words, rather we focused on healthy people’s perspective. In order to evaluate their anticipated stigma, participants were asked to ‘imagine/pretend’ to be infected. We acknowledge the difficulty of imagining being positive to SARS‐CoV‐2 for a healthy participant; however, this is a common practice in social sciences (Pivetti & Melotti, 2013), already used in COVID‐19 research (Earnshaw et al., 2020). Further studies are needed to support the content validity of our stigma measures as well as to replicate and extend the present results with samples of COVID‐19‐infected people.
Third, since the present study reports correlational data, longitudinal research is needed to provide stronger evidence not only on direction of effects, but also of their persistence over time. Chen and Bonanno (2020, p. 1) encourage researchers ‘to investigate long‐term patterns of mental health’ to better understand the psychological impact of the COVID‐19 pandemic. In fact, large‐scale social and life threats also provide an opportunity to examine long‐term effects on post‐traumatic relational and personal growth, such as potential increases in social cohesion and connections and in self‐efficacy for handling difficulties (Bonanno, Brewin, Kaniasty, & Greca, 2010; Cheng, Wong, et al., 2006; Cheng, Chong, et al., 2006). Therefore, future longitudinal research might examine whether some negative effects of the COVID‐19 pandemic on hedonic and eudaimonic psychological well‐being diminish or even turn into positive effects over time. As PeConga et al. (2020) have recently pointed out, despite the COVID‐19 pandemic undoubtedly posing risks for mental health, resilience is an equally likely outcome particularly in the long‐term (see also Daly & Robinson, 2020).
Given the above observation, an important direction for future research might be to identify factors that promote resilience in the face of the COVID‐19 pandemic. As a large literature on stress and coping has shown, the perceived availability of individual and situational resources (e.g., self‐efficacy, optimism, social support, cohesive neighbourhood) buffers the negative effects of stressors on psychological well‐being (Biggs, Brough, & Drummond, 2017). Similarly, research on post‐traumatic growth indicates that both personality traits and social factors contribute to resilience in the face of extreme stressors (Masten & Reed, 2002). With regard to individual factors affecting resilience in the COVID‐19 pandemic, Rubaltelli et al. (2020) have recently shown that greater ability to regulate emotions is predictive of a higher number of protective behaviours regardless of a person’s risk perception. There is also evidence that people scoring high on agreeableness and low on the Dark Triad traits are more likely to comply with governmental restrictions imposing personal costs in hopes of protecting others, because they tend to be more compassionate and caring people (Zajenkowski, Jonason, Leniarska, & Kozakiewicz, 2020). With regard to social factors, Prime, Wade, and Browne (2020) have suggested that family processes, organization, and family belief systems might be an important source of resilience. Sense of community and broader social connectedness also have been identified as possible protective factors in a recent study on the effects of a nationwide lockdown during COVID‐19 on New Zealanders’ well‐being (Sibley et al., 2020).
Practical implications and conclusion
Although our study provides only initial evidence which needs further empirical support, it has interesting implications for preventive and rehabilitative interventions. For instance, people suffering low well‐being from the pandemic could be helped to cognitively reframe it in more positive ways, by finding benefits in adversity. Previous research indicates that there are general beneficial qualities prevalent across a variety of traumatic circumstances, such as personal growth and interpersonal appreciation, but also benefits that appear to be relatively specific to virus outbreaks like the development of healthy behaviours and a heightened sense of solidarity (Cheng, Wong, et al., 2006; Cheng, Chong, et al., 2006). Finding benefits in adversity is predictive of greater psychological well‐being, especially among individuals who also perceive costs, probably because such costs are not denied, but acknowledged and worked through (Lehman et al., 1993; Taylor, 1983). Positive reframing associated with spiritual activities, like praying or searching for meaning, also has been shown to promote psychological adaptation to life‐threatening events (McIntosh & Rosselli, 2012).
As there is a tremendous amount of variability in the ways stigmatized individuals and groups respond to experiences of stigma‐related stress, classic coping models suggest that individual‐level coping strategies such as focusing on emotional aspects of the stress experience (e.g., meditation, expressive writing) or focusing on changing the circumstances relating to the stress (e.g., spending less time at work) can mitigate the consequences of stigma (Carver & Connor‐Smith, 2010; Coyne & Downey, 1991). Further, according to Frost (2011), meaning‐making strategies that focus on (re)defining the meaning of stigma‐related stressors can potentially result in positive outcomes for marginalized individuals and groups in various forms, such as social creativity and social change in the face of stigma (Jewkes, 2006; Riggle, Whitman, Olson, Rostosky, & Strong, 2008). Thus, through individual and group‐level meaning (re)making processes of stigma‐related stressors, social stigma can, indirectly, result in positive outcomes.
In order to reduce the psychological impact of the COVID‐19 outbreak, it is also advisable for the media to convey information to promote appropriate health protective behaviours ‘without sensationalism or disturbing images’ (Garfin et al., 2020, p. 356). In addition, healthcare systems need to make swab tests easily accessible to provide people with individualized information about their real health conditions. Policies to support work and income promise to be equally important in limiting the psychological impact of the COVID‐19 outbreak.
As our data suggest, the ongoing pandemic involves different levels of perceived risks, which to be adequately addressed require the synergistic intervention of several agencies and actors. Among these risks, the impairment of the subjects' well‐being is crucial, which merits further intensive investigation.
Conflicts of interest
All authors declare no conflict of interest.
Author contributions
F. Giorgia Paleari (Conceptualization; Data curation; Formal analysis; Methodology; Supervision; Writing – original draft; Writing – review & editing). Monica Pivetti (Conceptualization; Formal analysis; Methodology; Writing – original draft). Desirée Galati (Conceptualization; Data curation; Investigation; Methodology; Writing – original draft). Frank D. Fincham (Investigation; Supervision; Writing – review & editing).
Data availability statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
- AIP (2015). Code of ethics of the Italian psychological association. Retrieved from http://www.aipass.org/node/11560
- Akaike, H. (1987). Factor analysis and AIC. Psychometrika, 52, 317–332. 10.1007/BF02294359 [DOI] [Google Scholar]
- Ball‐Rokeach, S. J. , & DeFleur, M. L. (1976). A dependency model of mass‐media effects. Communication Research, 3(1), 3–21. 10.1177/009365027600300101 [DOI] [Google Scholar]
- Bentler, P. M. (1990). Comparative fit indexes in structural models. Psychological Bulletin, 107, 238–246. 10.1037/0033-2909.107.2.238 [DOI] [PubMed] [Google Scholar]
- Bentler, P. M. (2008). EQS 6 structural equations program manual. Encino, CA: Multivariate Software. Retrieved from www.mvsoft.com [Google Scholar]
- Biggs, A. , Brough, P. , & Drummond, S. (2017). Lazarus and Folkman's psychological stress and coping theory. In Cooper C. L. & Quick J. C. (Eds.), The handbook of stress and health: A guide to research and practice (pp. 349–364). Chichester, West Sussex, UK: Wiley‐Blackwell. [Google Scholar]
- Bonanno, G. A. , Brewin, C. R. , Kaniasty, K. , & Greca, A. M. L. (2010). Weighing the costs of disaster: Consequences, risks, and resilience in individuals, families, and communities. Psychological Science in the Public Interest, 11(1), 1–49. 10.1177/1529100610387086 [DOI] [PubMed] [Google Scholar]
- Brooks, S. K. , Webster, R. K. , Smith, L. E. , Woodland, L. , Wessely, S. , Greenberg, N. , & Rubin, G. J. (2020). The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet, 395, 912–920. 10.1016/S0140-6736(20)30460-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown, R. L. (2017). Functional limitation and depressive symptomatology: Considering perceived stigma and discrimination within a stress and coping framework. Stigma Health, 2(2), 98–109. 10.1037/sah0000042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bruns, D. P. , Kraguljac, N. V. , & Bruns, T. R. (2020). COVID‐19: Facts, cultural considerations, and risk of stigmatization. Journal of Transcultural Nursing, 31, 326–332. 10.1177/1043659620917724 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bunn, J. Y. , Solomon, S. E. , Miller, C. , & Forehand, R. (2007). Measurement of stigma in people with HIV: A reexamination of the HIV Stigma Scale. AIDS Education and Prevention, 19(3), 198–208. 10.1521/aeap.2007.19.3.198 [DOI] [PubMed] [Google Scholar]
- Bunting, S. M. (1996). Sources of stigma associated with women with HIV. Advances in Nursing Science, 19(2), 64–73. 10.1097/00012272-199612000-00008 [DOI] [PubMed] [Google Scholar]
- Carver, C. S. , & Connor‐Smith, J. (2010). Personality and coping. Annual Review of Psychology, 61(1), 679–704. 10.1146/annurev.psych.093008.100352 [DOI] [PubMed] [Google Scholar]
- Chassany, O. , Dimenäs, E. , Dubois, D. , Wu, A. , & Dupuy, H. (2004). The Psychological General Well‐Being Index (PGWBI) user manual. France: MAPI Research Institute. [Google Scholar]
- Chen, S. , & Bonanno, G. A. (2020). Psychological adjustment during the global outbreak of COVID‐19: A resilience perspective. Psychological Trauma: Theory, Research, Practice and Policy, 12(S1), S51–S54. 10.1037/tra0000685 [DOI] [PubMed] [Google Scholar]
- Cheng, C. , Wong, W. M. , & Tsang, K. W. (2006). Perception of benefits and costs during SARS outbreak: An 18‐month prospective study. Journal of Consulting and Clinical Psychology, 74, 870–879. 10.1037/0022-006X.74.5.870 [DOI] [PubMed] [Google Scholar]
- Cheng, S. K. W. , Chong, G. H. C. , Chang, S. S. Y. , Wong, C. W. , Wong, C. S. Y. , Wong, M. T. P. , & Wong, K. C. (2006). Adjustment to severe acute respiratory syndrome (SARS): Roles of appraisal and post‐traumatic growth. Psychology & Health, 21, 301–317. 10.1080/14768320500286450 [DOI] [Google Scholar]
- Conway, L. G. , Woodard, S. R. , & Zubrod, A. (2020). Social psychological measurements of COVID 19: Coronavirus perceived threat, government response, impacts, and experiences questionnaires. PsyArXiv Preprints [Preprint]. 10.31234/osf.io/z2x9a [DOI] [Google Scholar]
- Coyne, J. C. , & Downey, G. (1991). Social factors and psychopathology: Stress, social support, and coping processes. Annual Review of Psychology, 42, 401–425. 10.1146/annurev.ps.42.020191.002153 [DOI] [PubMed] [Google Scholar]
- Crandall, C. S. , & Moriarty, D. (1995). Physical illness stigma and social rejection. British Journal of Social Psychology, 34, 67–83. 10.1111/j.2044-8309.1995.tb01049.x [DOI] [PubMed] [Google Scholar]
- Daly, M. , & Robinson, E. (2020). Psychological distress and adaptation to the COVID‐19 crisis in the United States. Journal of Psychiatric Research, S0022‐3956(20)31038‐4. Advance online publication. 10.1016/j.jpsychires.2020.10.035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daly, M. , Sutin, A. R. , & Robinson, E. (2020). Longitudinal changes in mental health and the COVID‐19 pandemic: Evidence from the UK Household Longitudinal Study. Psychological Medicine, 1–10. Advance online publication. 10.1017/S0033291720004432 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daly, M. , Sutin, A. R. , & Robinson, E. (2021). Depression reported by US adults in 2017–2018 and March and April 2020. Journal of Affective Disorders, 278, 131–135. 10.1016/j.jad.2020.09.065 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deci, E. L. , & Ryan, R. M. (2008). Self‐determination theory: A macrotheory of human motivation, development, and health. Canadian Psychology/Psychologie Canadienne, 49(3), 182–185. 10.1037/a0012801 [DOI] [Google Scholar]
- Delle Fave, A. (2014). Eudaimonic and hedonic happiness. In Michalos C. (Ed.), Encyclopedia of quality of life and well‐being research (pp. 1999–2003). Dordrecht, the Netherlands: Springer. 10.1007/978-94-007-0753-5 [DOI] [Google Scholar]
- Diener, E. , & Ryan, K. (2009). Subjective well‐being: A general overview. South African Journal of Psychology, 39, 391–406. 10.1177/008124630903900402 [DOI] [Google Scholar]
- Dupuy, H. J. (1984). The psychological general wellbeing (PGWB) index. In Wenger N. K., Mattson M. E., Furburg C. D., & Elinson J. (Eds.), Assessment of quality of life in clinical trials of cardiovascular therapies (pp. 170–183). New York, NY: Le Jacq Publishing. [Google Scholar]
- Earnshaw, V. A. , Brousseau, N. M. , Hill, E. C. , Kalichman, S. C. , Eaton, L. A. , & Fox, A. B. (2020). Anticipated stigma, stereotypes, and COVID‐19 testing. Stigma and Health, 5, 390–393. 10.1037/sah0000255 [DOI] [Google Scholar]
- Earnshaw, V. A. , & Quinn, D. M. (2013). Influenza Stigma during the 2009 H1N1 pandemic. Journal of Applied Social Psychology, 43(1), 109–114. 10.1111/jasp.12049 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ehrlich‐Ben Or, S. , Hasson‐Ohayon, I. , Feingold, D. , Vahab, K. , Amiaz, R. , Weiser, M. , & Lysaker, P. H. (2013). Meaning in life, insight and self‐stigma among people with severe mental illness. Comprehensive Psychiatry, 54(2), 195–200. 10.1016/j.comppsych.2012.07.011 [DOI] [PubMed] [Google Scholar]
- Emlet, C. A. (2005). Measuring stigma in older and younger adults with HIV/AIDS: An analysis of an HIV stigma scale and initial exploration of subscales. Research on Social Work Practice, 15(4), 291–300. 10.1177/1049731504273250 [DOI] [Google Scholar]
- European Centre for Disease Prevention and Control (2020). COVID‐19 situation update for the EU/EEA and the UK. Retrieved from https://www.ecdc.europa.eu/en
- Fredrickson, B. L. (2001). The role of positive emotions in positive psychology. The broaden‐and‐build theory of positive emotions. The American Psychologist, 56(3), 218–226. 10.1037//0003-066x.56.3.218 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garfin, D. R. , Silver, R. C. , & Holman, E. A. (2020). The novel coronavirus (COVID‐2019) outbreak: Amplification of public health consequences by media exposure. Health Psychology, 39, 355–357. 10.1037/hea0000875 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goffman, E. (1963). Stigma: Notes on the management of spoiled identity. New York, NY: Simon and Schuster. [Google Scholar]
- Goyal, P. , Choi, J. J. , Pinheiro, L. C. , Schenck, E. J. , Chen, R. , Jabri, A. , … Safford, M. M. (2020). Clinical characteristics of COVID‐19 in New York City. The New England Journal of Medicine, 382, 2372–2374. 10.1056/nejmc2010419 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grossi, E. , Groth, N. , Mosconi, P. , Cerutti, R. , Pace, F. , Compare, A. , & Apolone, G. (2006). Development and validation of the short version of the Psychological General Well‐Being Index (PGWB‐S). Health and Quality of Life Outcomes, 4, 88. 10.1186/1477-7525-4-88 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herek, G. M. , Capitanio, J. P. , & Widaman, K. F. (2002). HIVrelated stigma and knowledge in the United States: Prevalence and trends, 1991–1999. American Journal of Public Health, 92, 371–377. 10.2105/AJPH.92.3.371 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huppert, F. A. (2009). Psychological well‐being: Evidence regarding its causes and consequences. Applied Psychology: Health and Well‐Being, 1(2), 137–164. 10.1111/j.1758-0854.2009.01008.x [DOI] [Google Scholar]
- Huta, V. , & Waterman, A. S. (2014). Eudaimonia and its distinction from hedonia: Developing a classification and terminology for understanding conceptual and operational definitions. Journal of Happiness Studies, 15, 1425–1456. 10.1007/s10902-013-9485-0 [DOI] [Google Scholar]
- Jewkes, R. (2006). Beyond stigma: Social responses to HIV in South Africa. Lancet, 368, 430–431. 10.1016/S0140-6736(06)69130-7 [DOI] [PubMed] [Google Scholar]
- Kalichman, S. C. , Simbayi, L. C. , Cloete, A. , Mthembu, P. P. , Mkhonta, R. N. , & Ginindza, T. (2009). Measuring AIDS stigmas in people living with HIV/AIDS: The internalized AIDS‐related stigma scale. AIDS Care: Psychological and Socio‐medical Aspects of AIDS/HIV, 21(1), 87–93. 10.1080/09540120802032627 [DOI] [PubMed] [Google Scholar]
- Keyes, C. L. M. (2007). Promoting and protecting mental health as flourishing: A complementary strategy for improving national mental health. American Psychologist, 62(2), 95–108. 10.1037/0003-066X.62.2.95 [DOI] [PubMed] [Google Scholar]
- Lazarus, R. S. , & Folkman, S. (1984). Stress, appraisal, and coping. New York, NY: Springer. [Google Scholar]
- Lehman, D. , Davis, C. , DeLongis, A. , Wortman, C. B. , Bluck, S. , Mandel, D. , & Ellard, G. H. (1993). Positive and negative life changes following bereavement and their relations to adjustment. Journal of Social and Clinical Psychology, 12, 90–112. 10.1521/jscp.1993.12.1.90 [DOI] [Google Scholar]
- Link, B. G. , & Phelan, J. C. (2006). Stigma and its public health implications. Lancet, 367, 528–529. 10.1016/s0140-6736(06)68184-1 [DOI] [PubMed] [Google Scholar]
- Liu, Y. , Finch, B. K. , Brenneke, S. G. , Thomas, K. , & Le, P. D. (2020). Perceived discrimination and mental distress amid the COVID‐19 pandemic: Evidence from the understanding America study. American Journal of Preventive Medicine, 59, 481–492. 10.1016/j.amepre.2020.06.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Logie, C. H. (2020). Lessons learned from HIV can inform our approach to COVID‐19 stigma. Journal of the International AIDS Society, 23(5), e25504. 10.1002/jia2.25504 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mak, W. W. , Poon, C. Y. , Pun, L. Y. , & Cheung, S. F. (2007). Meta‐analysis of stigma and mental health. Social Science & Medicine, 65(2), 245–261. 10.1016/j.socscimed.2007.03.015 [DOI] [PubMed] [Google Scholar]
- Mamun, M. A. , & Griffiths, M. D. (2020). COVID‐19 suicidal behavior among couples and suicide pacts: Case study evidence from press reports. Psychiatry Research, 289, 113105. 10.1016/2Fj.psychres.2020.113105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mardia, K. V. (1970). Measures of multivariate skewness and kurtosiswith applications. Biometrika, 57, 519–530. 10.1093/biomet/57.3.519 [DOI] [Google Scholar]
- Masten, A. S. , & Reed, M.‐G.‐J. (2002). Resilience in development. In Snyder C. R. & Lopez S. J. (Eds.), Handbook of positive psychology (pp. 74–88). New York: Oxford University Press. [Google Scholar]
- McIntosh, R. C. , & Rosselli, M. (2012). Stress and coping in women living with HIV: A meta‐analytic review. AIDS and Behavior, 16, 2144–2159. 10.1007/s10461-012-0166-5 [DOI] [PubMed] [Google Scholar]
- Olagoke, A. A. , Olagoke, O. O. , & Hughes, A. M. (2020). Exposure to coronavirus news on mainstream media: The role of risk perceptions and depression. British Journal of Health Psychology, 25, 865–874. 10.1111/bjhp.12427 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park, J. H. , van Leeuwen, F. , & Chochorelou, Y. (2013). Disease‐avoidance processes and stigmatization: Cues of substandard health arouse heightened discomfort with physical contact. The Journal of Social Psychology, 153(2), 212–228. 10.1080/00224545.2012.721812 [DOI] [PubMed] [Google Scholar]
- PeConga, E. K. , Gauthier, G. M. , Holloway, A. , Walker, R. , Rosencrans, P. L. , Zoellner, L. A. , & Bedard‐Gilligan, M. (2020). Resilience is spreading: Mental health within the COVID‐19 pandemic. Psychological Trauma: Theory, Research, Practice and Policy, 12(S1), S47–S48. 10.1037/tra0000874 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pierce, M. , Hope, H. , Ford, T. , Hatch, S. , Hotopf, M. , John, A. , … Abel, K. M. (2020). Mental health before and during the COVID‐19 pandemic: A longitudinal probability sample survey of the UK population. The Lancet Psychiatry, 7, 883–892. 10.1016/S2215-0366(20)30308-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pivetti, M. , & Melotti, G. (2013). Prenatal genetic testing: an investigation of determining factors affecting the decision‐making process. Journal of Genetic Counseling, 22(1), 76–89. 10.1007/s10897-012-9498-6 [DOI] [PubMed] [Google Scholar]
- Prime, H. , Wade, M. , & Browne, D. T. (2020). Risk and resilience in family well‐being during the COVID‐19 pandemic. American Psychologist, 75, 631–643. 10.1037/amp0000660 [DOI] [PubMed] [Google Scholar]
- Riggle, E. B. , Whitman, J. S. , Olson, A. , Rostosky, S. , & Strong, S. (2008). The positive aspects of being a lesbian or gay man. Professional Psychology: Research and Practice, 39(2), 210–217. 10.1037/0735-7028.39.2.210 [DOI] [Google Scholar]
- Rubaltelli, E. , Tedaldi, E. , Orabona, N. , & Scrimin, S. (2020). Environmental and psychological variables influencing reactions to the COVID‐19 outbreak. British Journal of Health Psychology, 25, 1020–1038. 10.1111/bjhp.12473 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruini, C. , Ottolini, F. , Rafanelli, C. , Ryff, C. , & Fava, G. A. (2003). Italian validation of Psychological Well‐being Scales (PWB). Rivista Di Psichiatria, 38(3), 117–130. [Google Scholar]
- Ryff, C. D. , & Keyes, C. L. M. (1995). The structure of psychological well‐being revisited. Journal of Personality and Social Psychology, 69, 719–727. 10.1037//0022-3514.69.4.719 [DOI] [PubMed] [Google Scholar]
- Ryff, C. D. , Keyes, C. L. , & Hughes, D. L. (2003). Status inequalities, perceived discrimination, and eudaimonic well‐being: Do the challenges of minority life hone purpose and growth? Journal of Health and Social Behavior, 44(3), 275–291. 10.2307/1519779 [DOI] [PubMed] [Google Scholar]
- Ryff, C. D. , & Singer, B. H. (2008). Know thyself and become what you are: A eudaimonic approach to psychological well‐being. Journal of Happiness Studies, 9, 13–39. 10.1007/s10902-006-9019-0 [DOI] [Google Scholar]
- Satorra, A. , & Bentler, P. M. (2001). A scaled difference chi‐square test statistic for moment structure analysis. Psychometrika, 66, 507–514. 10.1007/BF02296192 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shaw, G. M. , & Hunter, E. (2012). HIV transmission. Cold Spring Harbor Perspectives in Medicine, 2(11), a006965. 10.1101/cshperspect.a006965 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sibley, C. G. , Greaves, L. M. , Satherley, N. , Wilson, M. S. , Overall, N. C. , Lee, C. H. J. , … Barlow, F. K. (2020). Effects of the COVID‐19 pandemic and nationwide lockdown on trust, attitudes toward government, and well‐being. American Psychologist, 75, 618–630. 10.1037/amp0000662 [DOI] [PubMed] [Google Scholar]
- Sowell, R. L. , Lowenstein, A. , Moneyham, L. , Demi, A. , Mizuno, Y. , & Seals, B. F. (1997). Resources, stigma, and patterns of disclosure in rural women with HIV infection. Public Health Nursing, 14, 302–312. 10.1111/j.1525-1446.1997.tb00379.x [DOI] [PubMed] [Google Scholar]
- Stangl, A. L. , Earnshaw, V. A. , Logie, C. H. , van Brakel, W. , C Simbayi, L. , Barré, I. , & Dovidio, J. F. (2019). The Health Stigma and Discrimination Framework: a global, crosscutting framework to inform research, intervention development, and policy on health‐related stigmas. BMC Medicine, 17(1), 31. 10.1186/s12916-019-1271-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tai, Z. , & Sun, T. (2007). Media dependencies in a changing media environment: the case of the 2003 SARS epidemic in China. New Media & Society, 9, 987–1009. 10.1177/1461444807082691 [DOI] [Google Scholar]
- Taylor, S. E. (1983). Adjustment to threatening events: A theory of cognitive adaptation. American Psychologist, 38, 1161–1173. 10.1037/0003-066X.38.11.1161 [DOI] [Google Scholar]
- Tomczyk, S. , Rahn, M. , & Schmidt, S. (2020). Social distancing and stigma: Association between compliance with behavioral recommendations, risk perception, and stigmatizing attitudes during the COVID‐19 outbreak. Frontiers in Psychology, 11, 1821. 10.3389/fpsyg.2020.01821 [DOI] [PMC free article] [PubMed] [Google Scholar]
- UNAIDS . (2020). Rights in the time of COVID‐19—Lessons from HIV for an effective, community‐led response. Retrieved from https://www.unaids.org/en/resources/documents/2020/human‐rights‐and‐covid‐19
- Wang, Y. A. , & Rhemtulla, M. (in press). Power analysis for parameter estimation in structural equation modeling: A discussion and tutorial. Advances in Methods and Practices in Psychological Science. 10.31234/osf.io/pj67b [DOI] [Google Scholar]
- Waterman, A. (2008). Reconsidering happiness: A eudaimonist’s perspective. J. Positive Psycholology, 3, 234–252. 10.1080/17439760802303002 [DOI] [Google Scholar]
- Wiersinga, W. J. , Rhodes, A. , Cheng, A. C. , Peacock, S. J. , & Prescott, H. C. (2020). Pathophysiology, transmission, diagnosis, and treatment of coronavirus disease 2019 (COVID‐19): A review. JAMA, 324, 782–793. 10.1001/jama.2020.12839 [DOI] [PubMed] [Google Scholar]
- Wolf, E. J. , Harrington, K. M. , Clark, S. L. , & Miller, M. W. (2013). Sample size requirements for structural equation models: An evaluation of power, bias, and solution propriety. Educational and Psychological Measurement, 73, 913–934. 10.1177/0013164413495237 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xiang, Y. T. , Yang, Y. , Li, W. , Zhang, L. , Zhang, Q. , Cheung, T. , & Chee, H. N. (2020). Timely mental health care for the 2019 novel coronavirus outbreak is urgently needed. Lancet, 7(3), 228–229. 10.1016/S2215-0366(20)30046-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zacher, H. , & Rudolph, C. W. (2020). Individual differences and changes in subjective wellbeing during the early stages of the COVID‐19 pandemic. American Psychologist. 10.1037/amp0000702. Advance online publication. [DOI] [PubMed] [Google Scholar]
- Zajenkowski, M. , Jonason, P. K. , Leniarska, M. , & Kozakiewicz, Z. (2020). Who complies with the restrictions to reduce the spread of COVID‐19? Personality and perceptions of the COVID‐19 situation. Personality and Individual Differences, 166, 110199. 10.1016/j.paid.2020.110199 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.


