Abstract
Background
Vaccine hesitancy poses serious challenges for achieving coverage for population immunity. It is necessary to achieve high COVID‐19 vaccination acceptance rates and medical students’ coverage as future health care providers. The study aimed to explore the level of COVID‐19 vaccine hesitancy and determine the factors and barriers that may affect vaccination decision‐making.
Methods
A cross‐sectional study was carried out among medical students in Tanta and Kafrelsheikh Universities, Egypt. Data collection was done via an online questionnaire during January 2021 from 2133 students.
Results
The majority of the participant students (90.5%) perceived the importance of the COVID‐19 vaccine, 46% had vaccination hesitancy, and an equal percentage (6%) either definitely accepted or refused the vaccine. Most of the students had concerns regarding the vaccine's adverse effects (96.8%) and ineffectiveness (93.2%). The most confirmed barriers of COVID‐19 vaccination were deficient data regarding the vaccine's adverse effects (potential 74.17% and unknown 56.31%) and insufficient information regarding the vaccine itself (72.76%).
Conclusion
The government, health authority decision‐makers, medical experts, and universities in Egypt need to work together and make efforts to reduce hesitancy and raise awareness about vaccinations, consequently improving the acceptance of COVID‐19 vaccines.
Keywords: COVID‐19, medical students, vaccine acceptance, vaccine hesitancy
1. INTRODUCTION
The pandemic of COVID‐19 is considered a global challenge for all countries worldwide to contain its spread. Efforts and campaigns of prevention, early diagnosis, and medical management are being led by the World Health Organization (WHO) and numerous research teams and clinical experts worldwide. There are no specific antiviral medications for COVID‐19, and among the used drugs, a few have shown potential to reduce mortality among patients with COVID‐19 (e.g., corticosteroids and antibody‐based immunotherapeutics). Also, compliance of humans with social distancing and using face masks for an extended period is unguaranteed. Thus, the best strategy to control and gradually silencing this pandemic is to develop an effective vaccine. 1 , 2 , 3 , 4
A remarkable effort has been made in the eleven months since discovering the SARS‐CoV‐2 virus and its genome. The scientific community has contributed to the creation of more than 300 vaccine projects. More than 40 new vaccines are currently undergoing clinical evaluation, a few of them obtained the Food and Drug Administration's (FDA) Emergency Use Authorization (EUA), and are now used in many countries, for example, Pfizer BioNTech and Moderna vaccines, 5 but coverage rate is an essential factor that decides successful vaccination. Vaccine development was typically taking years. So, the public acceptance for a new vaccine of COVID‐19 developed within a short period remains uncertain despite the availability. 6 , 7 Lessons learned from the previous pandemics of influenza when the vaccine was introduced, and the acceptance rate was variably low in many countries urges proper understanding of the vaccine hesitancy problem. 8 , 9 , 10 , 11
The concept of “vaccine hesitancy” means to delay accepting or refusing vaccination although the vaccination services are made available, that is, no demand for offered and available vaccines. It is a continuum between those who accept vaccines without a doubt to complete refusal without a doubt. 12 Vaccine hesitancy affects the hesitant individual and, consequently, the whole community as a high coverage rate is necessary to confer herd immunity needed to flatten the epidemic curve. 13 , 14
Vaccine hesitancy is multidimensional and specific to one's environment, fluctuating by time, setting, and vaccines themselves. It is prompted by factors like complacency, convenience, and confidence. Complacency means the low perception of disease risk; hence, vaccination seems unnecessary. Confidence denotes trust in vaccination safety, effectiveness, and competence of healthcare systems. Convenience involves availability, affordability, and delivery of vaccines in a comfy context. 15 Several determinants modify vaccination decisions and determine whether to refuse, delay, or accept some or all vaccines. These include contextual influences that arise from historical, socioeconomic, cultural, ecological, health system/institutional, and political factors. 12 Concerns about the efficacy or safety, the country of manufacture of the vaccine, the antivaccine movements, and the belief of rushed vaccine development and production, besides rumors and misinformation, were important COVID‐19 vaccination hesitancy causes. 16
There are also individual and group influences that arise from the personal perception of the vaccine, beliefs, or attitudes toward vaccination, such as perceived efficacy or benefits of vaccines, safety concerns or side effects, and social/peer environment. Besides, specific issues directly related to the vaccine or vaccination like the introduction of a new vaccine or formulation or a new recommendation for a current vaccine, method of administration, development of the vaccination program, reliability and/or source of supply, schedule, cost, the strength of recommendations, knowledge base and/or attitude. Numerous COVID‐19 vaccination studies have documented an association between some of these factors and the acceptance of the COVID‐19 vaccine. 17 , 18 , 19
World Health Organization considers vaccine hesitancy as a significant threat to global health. Reported COVID‐19 vaccine acceptance rates varied worldwide, 19 but a recent global report on COVID‐19 vaccine acceptance illustrated that nearly 30% of the investigated participants would refuse or hesitate to take a COVID‐19 vaccine when it is available. 20 The Middle East is among the regions with the lowest rates of vaccine acceptance globally. 19
As the vaccine development process progresses, it is crucial to boost the acceptance of the new vaccines. Developing effective COVID‐19 vaccination strategies necessitate a proper understanding of the factors that would impact the decision of vaccination as these factors may change for individuals who accept and be determined to take the vaccine from those who do not. 21
The Egyptian Drug Authority (EDA) has approved the Sinopharm Chinese vaccine as the first primary one. In January, Egypt began its vaccination program, starting with medical teams in quarantine hospitals to be at the top of the vaccination priority categories, then medical teams, and set up a public immunization website for registration to start with high‐risk groups. Late in January, Egypt obtained the second batch of AstraZeneca vaccine as part of the COVID‐19 Vaccines Global Access (COVAX) Facility. 22
Most of the studies were conducted among healthcare providers or the general population, and limited literature has examined these factors in other risky groups of COVID‐19. Young adults, specifically college students, are at risk of being infected with COVID‐19 and transmitting the infection to others owing to the sense of invulnerability. 24 Experience with the ongoing pandemic has demonstrated medical students’ ability to volunteer in health care assistant positions that can be of real help to healthcare systems during times of emergency. 25
A recent study was conducted to describe the existing profile of potential COVID‐19 vaccine acceptance among Egyptian health care providers (medical students constituted 39.8% of participants), reported that 45.9% accept to receive the vaccine (only 13.5% totally accept the vaccine, and 32.4% were hesitant but somewhat agree) and 40.9% refused to take the vaccine. They concluded that the intention to accept COVID‐19 vaccination among Egyptian health care workers (HCWs) is lower than in western countries but better than the African ones. Vaccine hesitancy in Egyptian HCWs could be a significant obstacle influencing the COVID‐19 acceptance decision. 26
As medical students are likely to be exposed to COVID‐19 patients, achieving high vaccination coverage rates for COVID‐19 in this group is mandatory as soon as the vaccine is widely available as they can be used as vaccination role models for the public. They are the future health care providers and the notable influencers for people and their communities. Besides, they will be responsible for making recommendations for vaccination and providing guidance to vaccine‐positive patients. Given that limited research has addressed COVID‐19 vaccine acceptance among medical students, the current study was formulated targeting medical students of Tanta and Kafrelsheikh Universities in Egypt to explore the level of COVID‐19 vaccine hesitancy and to determine the factors and barriers that may affect their vaccination decision making.
2. MATERIALS AND METHODS
2.1. Study settings
A cross‐sectional study was conducted during January 2021 in Tanta and Kafrelsheikh Universities, two central public universities in the Delta region that recruit students from lower Egyptian governorates. Our target population was medical students at both universities (a total of 27715 students). 27 distributed through faculties of Medicine, Pharmacy, Dentistry, Nursing, and Physiotherapy. The Egyptian medical educational system varies according to the college's type; the faculty of medicine consisted of 6 years of university education, followed by one year of internship, and was modified in 2019 to be five years, followed by two internships. Dentistry education consists of five years, followed by 1 year of internships which is the same in the pharmacy but without training. The nursing and physiotherapy faculties comprised four years of education, followed by one year of internship. The students' groups are freshmen in 1st year, sophomores in 2nd year, juniors in 3rd and seniors in 4th, 5th, or 6th years—according to the college type—and graduates in the internship.
2.2. Study sample
Using Epi‐Info 7.2.3.0 software statistical package created by Center for Disease Control and Prevention, Atlanta, Georgia, USA and based on the expected frequency of 50%, an acceptable margin of error of 2.5%, level of confidence of 95%, the minimum required sample size was calculated to equal 1456 student. They were approached by convenience sampling using a self‐administered online questionnaire hosted in Microsoft form and distributed through official university platforms and informal students’ groups on social media like Facebook. Some students' representatives from each faculty were also engaged in distributing the questionnaire's link directly to their colleagues. The form was open for one week from 8th to 15th January 2021 and then closed when not receiving any new responses for 24 h.
2.3. Study tool
The questionnaire was designed and pretested by the researchers after an extensive literature review. 24 , 28 , 29 , 30 It addressed the following data: Personal characteristics; gender, age, residence, college, academic year, family income, and socioeconomic status. It also included questions about self‐perception of own health status, risk perception percentage of getting COVID‐19 infection, previous infection with COVID‐19 or infection in a close social network, seasonal influenza vaccination, and knowledge and information sources COVID‐19. Lastly, level of acceptance or hesitancy about COVID‐19 vaccine, beliefs regarding COVID‐19 vaccination (16 questions), perceived barriers and motivators of COVID‐19 vaccination (13 questions), and type of COVID‐19 vaccine preference. The questionnaire form was pretested on 20 students who were not included in the final analysis; its internal consistency was assessed by calculating the Cronbach's alpha as 0.790. Most of the questions were assigned to be mandatory answered items to avoid incompleteness and missing data.
2.4. Statistical analysis of data
Data were extracted from the form to Excel sheet and statistically analyzed using IBM SPSS software version 26. Qualitative data were presented as frequencies and percentages, and a chi‐square test was used for analysis. Quantitative variables were presented as mean and standard deviation, and ANOVA was used for analysis. Multivariate logistic regression was applied to predict factors affecting vaccine acceptance among respondents. The adopted significance level is p < .05.
2.5. Ethical consideration
Research ethical approval from the Tanta Faculty of Medicine Research Ethical Committee (REC) was obtained (code:34400/1/21). An informative statement was added at the beginning of the anonymous online questionnaire, and the participants were provided with informed consent to be digitally signed before starting the survey. Confidentiality and privacy of data were guaranteed during the study, and the collected personal information was stored in secure folders that could only be accessed by the researchers and protected from any unauthorized access.
3. RESULTS
3.1. Participant characteristics in relation to COVID‐19 vaccination acceptance status
The study included 2133 participants from five medical colleges in Tanta and Kafrelsheikh universities; their mean age was 20.24 ± 1.8 years. The acceptance group represented 34.9% of students (746 out of 2133), the hesitant group was 45.7% (974 out of 2133), and the refusal group constituted only 19.4% (413 out of 2133).
Regarding factors associated with COVID‐19 vaccine acceptance among the respondent medical students: The majority (65.2%) of surveyed students were females, 68.4% were students in Medicine and Physiotherapy (34.1% and 34.3%, respectively), more than half had just enough income (57.3%), and most of them had average socioeconomic status (77.5%). However, there was no statistically significant difference between the groups of students accepting, hesitating, or refusing the vaccine regarding those variables. The highest percentage, 47% (38 out of 81), of vaccine acceptance, was reported among graduate respondents, while the highest percentage of hesitancy and refusal was reported among juniors 50.5% (140 out of 277) and 22.0% (61 out of 277), respectively, with a statistically significant difference (p = .011).
Most of the respondents reported average to very good health status (95.4%). Of the small percentage who reported bad health status, more than half were hesitant about the vaccine (53.8%; 42 out of 78), and one‐third (33.3%; 6 out of 18) of the students with very bad health status accepted the vaccination, and the difference between the groups was statistically significant (p = .001). Overall, 38.7% of respondents reported ˃80% risk of infection with COVID‐19, 26.2% reported ˃60% risk, 25.6% reported ˃40% risk. More than half of respondents (56.4%) were not infected with COVID‐19, and only 4.4% had confirmed infection with no statistically significant difference between different groups of students. On the other hand, 51.5% of respondents had confirmed COVID‐19 infection in their close social network, and of those, 35.4% accepted the vaccine, 46.1% (507 out of 1099) were hesitant, and 18.5% (203 out of 1099) refused the vaccine with a statistically significant difference (p = .001). Most respondents (89.7%) never received the seasonal influenza vaccine compared to only 2.6% who used to receive it annually, but the difference between groups was not statistically significant. Most respondents (91.3%) reported inadequacy of the available safety data for the new vaccines, and of the 8.7% who reported adequacy of safety data, 69.4% (129 out of 186) accepted the vaccine compared to 25.8% (48 out of 186) were hesitant, and 4.8% (9 out of 186) refused the vaccine (p = .0001). Other characteristics are shown in Table 1.
Table 1.
Factors associated with COVID‐19 vaccine acceptance among respondent medical students
| Factors | Overall respondents (n = 2133) | COVID‐19 vaccine acceptance group (n = 746)a | COVID‐19 vaccine hesitant group (n = 974) | COVID‐19 vaccine refusal group (n = 413)b | p | ||||
|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | ||
| Age (years), mean ± SD | 20.24 | ± 1.78 | 20.24 | ± 1.853 | 20.26 | ± 1.77 | 20.20 | ± 1.67 | .232 |
| Sex | |||||||||
| Men | 742 | 34.8 | 276 | 37.2 | 331 | 44.6 | 135 | 18.2 | .263 |
| Women | 1391 | 65.2 | 470 | 33.8 | 643 | 46.2 | 278 | 20.0 | |
| College | |||||||||
| Medicine | 727 | 34.1 | 261 | 35.9 | 340 | 46.8 | 126 | 17.3 | .725 |
| Physical medicine | 732 | 34.3 | 245 | 33.5 | 330 | 45.1 | 157 | 21.4 | |
| Dentistry | 256 | 12.0 | 71 | 27.7 | 137 | 53.5 | 48 | 18.8 | |
| Nursing | 274 | 12.8 | 130 | 47.4 | 98 | 35.8 | 46 | 16.8 | |
| Pharmacy | 144 | 6.8 | 39 | 27.1 | 69 | 47.9 | 36 | 25.0 | |
| Academic year | |||||||||
| Freshman | 496 | 23.3 | 165 | 33.3 | 235 | 47.4 | 96 | 19.4 | .011c |
| Sophomore | 676 | 31.7 | 266 | 39.3 | 283 | 41.9 | 127 | 18.8 | |
| Junior | 277 | 13.0 | 76 | 27.4 | 140 | 50.5 | 61 | 22.0 | |
| Senior | 603 | 28.3 | 201 | 33.3 | 284 | 47.1 | 118 | 19.6 | |
| Graduate | 81 | 3.8 | 38 | 46.9 | 32 | 39.5 | 11 | 13.6 | |
| Family income | |||||||||
| Not enough | 195 | 9.1 | 68 | 34.9 | 85 | 43.6 | 42 | 21.5 | .762 |
| Enough but no saving | 1223 | 57.3 | 437 | 35.7 | 559 | 45.7 | 227 | 18.6 | |
| Enough and saving | 715 | 33.5 | 241 | 33.7 | 330 | 46.2 | 144 | 20.1 | |
| Socioeconomic status | |||||||||
| Low | 69 | 3.2 | 27 | 39.1 | 132 | 43.9 | 14 | 20.3 | .093 |
| Average | 1654 | 77.5 | 585 | 35.4 | 28 | 40.6 | 299 | 18.1 | |
| High | 109 | 5.1 | 41 | 37.6 | 770 | 46.6 | 24 | 22.0 | |
| Prefer Not to disclose | 301 | 14.1 | 93 | 30.9 | 44 | 40.4 | 76 | 25.2 | |
| Self‐perception of own health status | |||||||||
| Very bad | 18 | 0.8 | 6 | 33.3 | 3 | 16.7 | 9 | 50.0 | .001b |
| Bad | 78 | 3.7 | 15 | 19.2 | 42 | 53.8 | 21 | 26.9 | |
| Average | 536 | 25.1 | 123 | 22.9 | 242 | 45.1 | 171 | 31.9 | |
| Good | 1129 | 52.9 | 210 | 18.6 | 535 | 47.4 | 384 | 34.0 | |
| Very good | 372 | 17.4 | 6 | 33.3 | 152 | 40.9 | 161 | 43.3 | |
| Risk perception percentage of getting COVID‐19 infection | |||||||||
| 0% ‐ | 70 | 3.3 | 20 | 28.6 | 26 | 37.1 | 24 | 34.3 | .095 |
| 20% ‐ | 135 | 6.3 | 40 | 29.6 | 65 | 48.1 | 30 | 22.2 | |
| 40% ‐ | 545 | 25.6 | 200 | 36.7 | 241 | 44.2 | 104 | 19.1 | |
| 60% ‐ | 558 | 26.2 | 193 | 34.6 | 260 | 46.6 | 105 | 18.8 | |
| ˃ 80% | 825 | 38.7 | 293 | 35.5 | 382 | 46.3 | 150 | 18.2 | |
| Previous infection with COVID‐19 | |||||||||
| I do not know | 470 | 22.0 | 155 | 33.0 | 225 | 47.9 | 90 | 19.1 | .259 |
| Yes & confirmed | 94 | 4.4 | 29 | 30.9 | 46 | 48.9 | 19 | 20.2 | |
| Yes, but not confirmed | 367 | 17.2 | 118 | 32.2 | 164 | 44.7 | 85 | 23.2 | |
| Not infected | 1202 | 56.4 | 444 | 36.9 | 539 | 44.8 | 219 | 18.2 | |
| COVID‐19 infection in close social network | |||||||||
| Do not know | 208 | 9.8 | 53 | 25.5 | 103 | 49.5 | 52 | 25.0 | .001b |
| Yes & confirmed | 1099 | 51.5 | 389 | 35.4 | 507 | 46.1 | 203 | 18.5 | |
| Yes, but not confirmed | 364 | 17.1 | 114 | 31.3 | 184 | 50.5 | 66 | 18.1 | |
| Not infected | 462 | 21.7 | 190 | 41.1 | 180 | 39.0 | 92 | 19.9 | |
| Seasonal influenza vaccination | |||||||||
| Never | 1914 | 89.7 | 647 | 33.8 | 890 | 46.5 | 377 | 19.7 | .078 |
| Last year | 112 | 5.3 | 50 | 44.6 | 44 | 39.3 | 18 | 16.1 | |
| Current flu season (2020–2021) | 51 | 2.4 | 23 | 45.1 | 19 | 37.3 | 9 | 17.6 | |
| Annually | 56 | 2.6 | 26 | 46.4 | 21 | 37.5 | 9 | 16.1 | |
| Adequacy of the available safety data for the new vaccine | |||||||||
| No | 1947 | 91.3 | 617 | 31.7 | 926 | 47.6 | 404 | 20.7 | .0001b |
| Yes | 186 | 8.7 | 129 | 69.4 | 48 | 25.8 | 9 | 4.8 | |
Vaccine acceptance = definitely accept + accept with some hesitancy.
Vaccine refusal = definitely refuse + refuse with some hesitancy.
Significant.
3.2. COVID‐19 vaccine acceptance and hesitancy among respondents
Near half (46%) of respondents showed hesitancy, and 6% either accepted the vaccine or refused it definitely (Figure 1A). Despite the reported hesitancy, most respondents (71%) intend to receive the vaccine but will postpone this for a while, and only 13% intend to receive it as soon as possible (Figure 1B). Approximately 46% (83 out of 181) of respondents who self‐rated their level of knowledge about COVID‐19 as very good were vaccine acceptors, while 45.5% (10 out of 22) of respondents with a very bad level of knowledge refused it (Figure 1C). Social media, scientific websites, and healthcare providers were the primary sources of information about COVID‐19. Meanwhile, magazines and newspapers were the least (Figure 1D).
Figure 1.
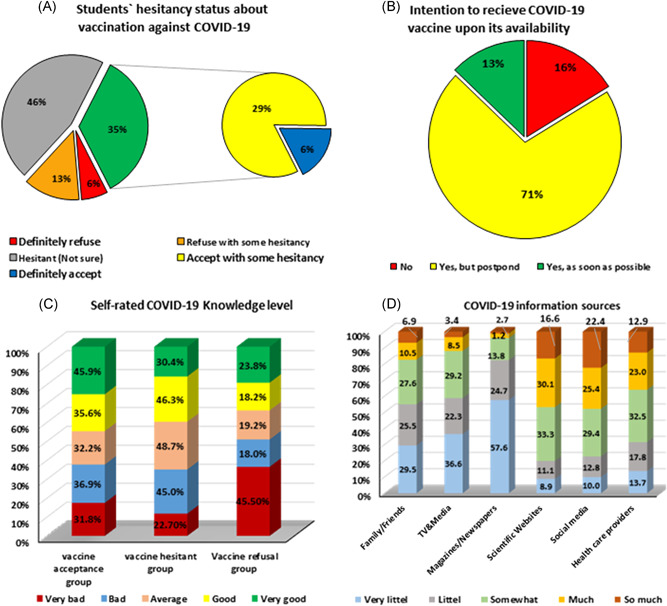
COVID‐19 vaccine acceptance and hesitancy among respondents
3.3. Participants' beliefs regarding COVID‐19 vaccination
Most participants believe that COVID‐19 vaccination is important (90.5%), everyone in the community should get it once available (92.6%), vaccination should be compulsory for the general population (69.7%), especially for health care workers (HCWs; 92.1%). Despite that good percentage of students believed that the way to overcome the COVID‐19 pandemic is mass vaccination (67.9%) and that getting vaccinated is the best preventive measure (56.5%), most of them had concerns regarding the adverse effects of the vaccine (96.8%), its ineffectiveness (93.2%) and enough testing (80.2%), safety (54.0%), and 63.3% had concerns for the acquisition of COVID‐19 from the vaccine itself. Most students were not against vaccination in general (95.1%), and 76.4% had no prior bad experience with any vaccines or their adverse reactions. Students perceived themselves at elevated risk to acquire COVID‐19 (77.6%) and at a considerable risk of developing complications if they have been infected (75.9%; Table 2).
Table 2.
Study participants' beliefs regarding COVID‐19 vaccination
| Statement | Perceived importance | |||
|---|---|---|---|---|
| Not important | Important | |||
| n | % | n | % | |
| How important do you perceive the COVID‐19 vaccine to be? | 202 | 9.5 | 1931 | 90.5 |
| How important you think that everyone in the community should get the COVID‐19 vaccine once available? | 158 | 7.4 | 1975 | 92.6 |
| Vaccination of COVID‐19 should always be compulsory once it is available | 646 | 30.3 | 1487 | 69.7 |
| Your concerns regarding the COVID‐19 vaccination? | 282 | 13.2 | 1851 | 86.8 |
| Vaccination of COVID‐19 should always be compulsory for HCWs once it is available | 169 | 7.9 | 1964 | 92.1 |
| Statement | Disagree | Agree | ||
| n | % | n | % | |
| I think that approval of the vaccine guarantees its safety | 1151 | 54.0 | 982 | 46.0 |
| Do you believe that the way to overcome the COVID‐19 pandemic is mass vaccination? | 684 | 32.1 | 1449 | 67.9 |
| The best preventive measure for COVID‐19 is getting vaccinated | 927 | 43.5 | 1206 | 56.5 |
| I think that the vaccine was not tested for enough time | 422 | 19.8 | 1711 | 80.2 |
| Concern regarding the adverse effects of the vaccine | 68 | 3.2 | 2065 | 96.8 |
| Concern about the ineffectiveness of the vaccine | 145 | 6.8 | 1988 | 93.2 |
| having a prior bad experience with any vaccines and their adverse reactions | 1629 | 76.4 | 504 | 23.6 |
| I am against vaccination in general | 2028 | 95.1 | 105 | 4.9 |
| Concern for the acquisition of Covid‐19 from the vaccine | 782 | 36.7 | 1351 | 63.3 |
| I think that I am not at a considerable risk of developing complications if I have been infected with Covid‐19 | 1618 | 75.9 | 515 | 24.1 |
| I perceive myself not at elevated risk to acquire Covid‐19 | 1655 | 77.6 | 478 | 22.4 |
3.4. Reported barriers and motivators of COVID‐19 vaccination
The most‐reported barriers of COVID‐19 vaccination were insufficient information regarding adverse effects of the vaccine (potential 74.2% and unknown 56.3%), insufficient information regarding the vaccine itself (72.8%), financial cost hindrance if the vaccine is not free (68.0%), and insufficient trust in the vaccination source (55.1%). On the other hand, fear of infecting their family, especially parents, or being infected themselves were the most reported motivators (77.7% and 35.1%, respectively; Table 3).
Table 3.
The perceived barriers and motivators of COVID‐19 vaccination among the study participants
| Factors | n (n = 2133) | % |
|---|---|---|
| The barriers to receiving the COVID‐19 vaccine | ||
| Doubt in vaccine safety | 844 | 39.57 |
| Doubt in vaccine effectiveness | 501 | 23.49 |
| Fear of unknown adverse effects | 1201 | 56.31 |
| Fear of long‐term genetic effects of some vaccine types | 488 | 22.88 |
| Fear of (nanochips) implantation via the vaccine | 332 | 15.56 |
| Insufficient trust in the vaccination source (producer) | 1175 | 55.09 |
| Insufficient information regarding the vaccine | 1552 | 72.76 |
| Insufficient information regarding the potential adverse effects | 1582 | 74.17 |
| The financial cost hindrance if the vaccine is not free | 1451 | 68.0 |
| The motivators for receiving the COVID‐19 vaccine | ||
| Fear of being infected with COVID‐19 | 749 | 35.11 |
| Fear of infecting my family with COVID‐19, especially my parents | 1658 | 77.73 |
| Belief in the effectiveness and safety of the vaccine | 302 | 14.16 |
| Availability of free vaccines | 250 | 11.72 |
Figure 2 portrays that 65.6% of respondents did not know the difference between types of available COVID‐19 vaccines, while 22% preferred Pfizer‐BionNTech one.
Figure 2.
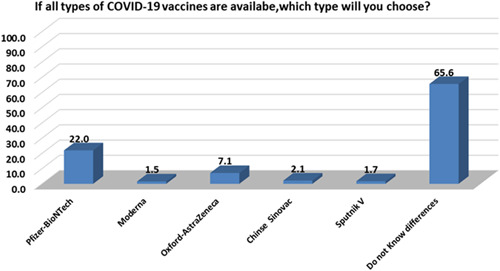
Type of COVID‐19 vaccine preference among respondents
3.5. Predictors associated with vaccine acceptance among medical students
Table 4 illustrates that being a pharmacy student, higher academic year and graduates, average to very good self‐perception of own health status, good self‐rated COVID‐19 knowledge level, and presence of confirmed COVID‐19 infection in close social network were the significant predictors of COVID‐19 vaccine acceptance among studied medical students (p < .05).
Table 4.
Predictors of COVID‐19 vaccine acceptance among medical students by logistic regression analysis
| Predictor Variable | B | Wald | Sig. | Exp(B) | 95% CI for EXP (B) | |
|---|---|---|---|---|---|---|
| Lower | Upper | |||||
| Age | −0.064 | 1.057 | 0.304 | 0.938 | 0.831 | 1.060 |
| Sex: Men #Ref. | ||||||
| Women | 0.140 | 1.821 | 0.177 | 1.150 | 0.939 | 1.409 |
| College: Medicine #Ref. | ||||||
| Physical medicine | 0.323 | 2.249 | 0.134 | 1.381 | 0.906 | 2.105 |
| Dentistry | 0.269 | 1.501 | 0.221 | 1.308 | 0.851 | 2.010 |
| Nursing | 0.030 | 0.015 | 0.903 | 1.030 | 0.639 | 1.661 |
| Pharmacy | 0.817 | 9.470 | 0.002* | 2.264 | 1.345 | 3.809 |
| Year: Freshman #Ref. | ||||||
| Sophomore | −1.025 | 5.124 | 0.024* | 0.359 | 0.148 | 0.872 |
| Junior | −0.874 | 4.747 | 0.029* | 0.417 | 0.190 | 0.916 |
| Senior | −1.034 | 7.816 | 0.005* | 0.356 | 0.172 | 0.734 |
| Graduate | −0.733 | 6.397 | 0.011* | 0.480 | 0.272 | 0.848 |
| Socioeconomic status: Low #Ref. | ||||||
| Average | −0.242 | 0.881 | 0.348 | 0.785 | 0.474 | 1.301 |
| High | −0.001 | 0.000 | 0.998 | 0.999 | 0.487 | 2.049 |
| Prefer not to disclose | −0.029 | 0.016 | 0.900 | 0.972 | 0.620 | 1.523 |
| Family income: Not enough #Ref. | ||||||
| Enough but no saving | 0.085 | 0.181 | 0.671 | 1.089 | 0.736 | 1.611 |
| Enough and saving | 0.161 | 2.073 | 0.150 | 1.174 | 0.944 | 1.462 |
| Self‐perception of own health status: Very bad #Ref. | ||||||
| Bad | 0.179 | 0.121 | 0.728 | 1.196 | 0.436 | 3.279 |
| Average | −0.681 | 5.196 | 0.023* | 0.506 | 0.282 | 0.909 |
| Good | −0.392 | 6.488 | 0.011* | 0.675 | 0.499 | 0.913 |
| Very good | −0.310 | 5.507 | 0.019* | 0.733 | 0.566 | 0.950 |
| Self‐rated COVID‐19 knowledge level: Very bad #Ref. | ||||||
| Bad | −0.486 | 0.887 | 0.346 | 0.615 | 0.224 | 1.691 |
| Average | −0.150 | 0.324 | 0.569 | 0.861 | 0.514 | 1.442 |
| Good | −0.459 | 6.532 | 0.011* | 0.632 | 0.444 | 0.898 |
| Very good | −0.339 | 3.651 | 0.056 | 0.713 | 0.504 | 1.009 |
| Previous infection with COVID‐19: I do not know #Ref. | ||||||
| Yes & confirmed | −0.003 | 0.001 | 0.981 | 0.997 | 0.778 | 1.278 |
| Yes, but not confirmed | −0.164 | 0.430 | 0.512 | 0.849 | 0.521 | 1.384 |
| Not infected | −0.141 | 0.994 | 0.319 | 0.868 | 0.658 | 1.146 |
| COVID‐19 infection in close social network: I do not know #Ref. | ||||||
| Yes & confirmed | −0.618 | 9.616 | 0.002* | 0.539 | 0.365 | 0.797 |
| Yes, but not confirmed | −0.110 | 0.740 | 0.390 | 0.895 | 0.696 | 1.152 |
| Not infected | −0.296 | 3.357 | 0.067 | 0.744 | 0.542 | 1.021 |
| Previous seasonal influenza vaccination: Never #Ref. | ||||||
| Last year | −0.480 | 2.822 | 0.093 | 0.619 | 0.354 | 1.083 |
| Current flu season (2020–2021) | −0.168 | 0.235 | 0.628 | 0.845 | 0.428 | 1.669 |
| Annually | 0.015 | 0.001 | 0.970 | 1.016 | 0.456 | 2.263 |
| Risk perception percentage of getting COVID‐19 infection: 0‐#Ref. | ||||||
| 20 | −0.402 | 1.948 | 0.163 | 0.669 | 0.380 | 1.177 |
| 40 | −0.315 | 2.156 | 0.142 | 0.730 | 0.479 | 1.111 |
| 60 | 0.027 | 0.047 | 0.829 | 1.027 | 0.805 | 1.311 |
| >80 | −0.025 | 0.042 | 0.837 | 0.975 | 0.767 | 1.239 |
Significant.
The dependent variable is vaccine acceptance (definitely accept and accept with some hesitancy) versus (definitely refuse, refuse with some hesitancy and hesitant responses) #Ref. Reference category.
4. DISCUSSION
Vaccine hesitancy is a limiting step in global attempts to control the current pandemic with its adverse health and socioeconomic consequences. Understanding the student's attitude upon the COVID‐19 vaccine and raising their acceptance is essential in planning an appropriate post‐pandemic strategy. 31
In the present study, 35% of the students accepted the COVID‐19 vaccination, 46% were hesitant, and 19% refused (Figure 1A). A lower percentage of hesitancy (32.4%) and a higher level of acceptance (45.9%) were reported among some Egyptian HCWs. 26 The difference may be attributed to the higher age of health care staff (older participants seem to accept more) and the prevalence of co‐morbidities or chronic diseases among them. Tam et al., 2020 23 reported 15.1% as hesitant, 60.6% as acceptance group, and 24.3% as refusal group among college students in South Carolina. In comparison, Lucia et al., 2020, 28 nearly one‐quarter of the allopathic medical students in Southeast Michigan were vaccine‐hesitant. Our findings are supported by a systematic review of COVID‐19, which reported wide variability in COVID‐19 vaccine acceptance rates in different countries with low rates in the Middle East. 32 This issue poses a significant problem for ongoing efforts to contain the current pandemic of COVID‐19.
The majority of the participants had the intention of the vaccination, and only 16% had no intention (Figure 1B). Similar results were stated by Barello et al., 2020 29 as they found the Italian university students' intention to get the COVID‐19 vaccine as 86.1%, and on the other side, 13.9% of them reported no intention. However, the estimated intention to vaccinate is higher among medical students due to higher literacy on health‐related issues. 33
Considerably high level (47.1%) of vaccine hesitancy was found among the senior students (Table 2). Seniors could help control the current pandemic in multiple ways and be prepared for future waves or peaks. Medical schools in some countries as the United States and England prepare students to help medical teams 34 efficiently, so they should be protected and vaccinated as vaccination of healthcare staff and students is a crucial measure in preventing health‐related infections resulting from close interaction with high‐risk patients. 29
The high level of vaccine hesitancy among the students was surprisingly associated with a similarly high level of perception of elevated risk of getting COVID‐19 infection (Table 1). This finding was in line with Lucia et al., 2020, 28 who reported that more than 2 out of 10 students were vaccine‐hesitant despite self‐perception of increased risk of exposure to COVID‐19 infection. At the same time, this finding contrasts with previous studies, which showed the perception of risk as a key predictor of the intention of prevention and protective health behaviors. 30
Near half of the vaccine, acceptors rated their COVID‐19 related knowledge as good (Table 1; Figure 1C). Similarly, Barello et al. 2020 concluded that the vaccination attitude is affected by students’ knowledge regarding health issues. 29
Most of the study participants perceived COVID‐19 vaccination as important, especially for HCWs, and that it should be compulsory once widely available (Table 2). Corresponding findings were reported by Lucia et al., 2020. 28 CDC, 2020, recommends that healthcare personnel, including medical students, receive the first doses of COVID‐19 vaccines due to their high risk of exposure. 35
In this study, most participants reported having concerns regarding vaccine effectiveness, safety, and adverse effects (Table 2 & 3). Similar concerns were reported among Egyptian HCWs. 26 These findings may explain that although the students perceive the importance of the COVID‐19 vaccine and agree to make the vaccination mandatory, they still have a significant hesitancy due to a lack of certainty on the safety of vaccinations and unknown potential adverse effects, in addition to misinformation from social media as a source of their knowledge.
Evidence suggests the importance of concentrating on building trust in COVID‐19 vaccines. This includes the use of trusted messengers to navigate the COVID‐19 information paradigm and confidence‐building in vaccines through transparency and expectation management. Communities should be engaged early to listen to concerns, answer questions, and counter misinformation. 36 As public confidence in vaccination is weak; COVID‐19 vaccination programs can only succeed if there is a common belief that the provided vaccines are safe and effective. 37 Lucia et al., 28 emphasized the need for transparency and to answer concerns about vaccine development's speed and safety. Supporting COVID‐19 vaccination through public messages and news releases and monitoring and tacking false news is crucial.
In This study, “Fear of being infected or infecting family with, especially parents” was highly reported among COVID‐19 vaccination motivators (Table 3). This finding is supported by Brewer et al. 38 who reported that anticipated regret for lack of action (i.e., not getting a vaccination and being infected and/or infecting loved ones) is correlated with a higher likelihood of vaccination. However, a study on Saudi HCWs’ willingness for COVID‐19 vaccination concluded that the level of concern regarding contracting COVID‐19 and infecting household members did not correlate significantly with their likelihood of being vaccinated. 39
In this study, the main vaccination barriers were insufficient information regarding the vaccine and its potential adverse effects, the accelerated pace of the vaccine production, fear of high financial costs (Tables 2 and 3). Similarly, Lucia et al., 2020 28 stated that concerns about the vaccine's serious side effects and lack of trusted information contributed to the hesitancy of vaccines. Also, Tam et al. 23 concluded that the adverse outcomes of COVID‐19 vaccines as long‐term side effects, safety issues, and distrust of vaccines lead to vaccine hesitancy. Misinformation regarding the vaccines and lack of advanced vaccination knowledge can contribute to anxiety, leading to overestimating possible side effects. 40 It is anticipated that many hesitant individuals may accept vaccination if reassured and provided with trustable information that the vaccine is safe and effective.
Gautam et al. 41 checked the responder's affordability and concluded that most responders wish a cheap or a free vaccine from the government. Vaccine cost and effectiveness appear as essential factors to accept vaccination. 42 A study on South Carolina college students reported vaccination costs as one factor that directly affects the students' vaccination behaviors. 23
Some of the vaccination barriers and beliefs in the present study were false and related to the students’ misinformation as genetic effects, acquisition of COVID‐19 from the vaccine, and nanochips’ implantation (Tables 3 and 4), and this could be attributed to lack of information concerning COVID‐19 vaccination in their current curricula, so future inclusion of such topic into medical education could help them to evaluate the risks and benefits of vaccination. The World Health Organization warned that the world is fighting another kind of epidemic called “infodemic” that rapidly spreads fake news, misleading information, and false scientific claims. 43 Lessons learned from past outbreaks of SARS, H1N1, and Ebola illustrated the essential role of health information in disease prevention and vaccine acceptance. 44
College students use various sources to know about COVID‐19 vaccines, including health authorities, personal networks, and social media. 30 Hesitancy is exacerbated by social media, conspiracy theories, and misinformation. 45
The study participants' reported social media, scientific websites, then health care providers as the most extensive sources to obtain their COVID‐19 and vaccine information (Figure 1D). Vaccination decision‐making is often affected by social networks’ impacts, including family members, colleagues, and healthcare professionals. 38 Harapan et al. 46 asserted that most of the information about COVID‐19 is disseminated via social or online media. This information influences perceptions 47 ; these sources are not a preferred knowledge source due to the public's misinformation (conspiracy theory). So, improved information on vaccines has been shown to increase vaccines’ acceptance. 48
Health professionals as a reliable source of COVID‐19 information were a higher percentage (75%) in Malik et al. 49 but their study was among the USA's general population. However, it is recommended to organize expert groups for communicating with the public, including health officials and health practitioners, including nurses and ancillary health personnel, to conduct the community messaging to boost trust and increase the acceptance of the COVID‐19 vaccine. 50
Most participants did not know the available types of COVID‐19 vaccines, so they do not have a preferred one (Figure 2). However, 46.2% of Egyptian HCWs reported preferring (Pfizer‐BioNTech) vaccine due to trust in this brand and the transparency of their vaccine details and information presented to the public. 26 The type of vaccine may affect the individual's attitudes toward vaccination, though Pogue et al. 51 found that the vaccine type did not make a difference to the respondents, as they detected no significant difference in comfort to vaccination.
5. CONCLUSIONS
This is the first study of vaccine hesitancy among university students—particularly medical students—in Egypt. This study highlighted the following:
-
▪
The COIVD‐19 vaccine acceptance was only 35%, with considerably high hesitancy and refusal. Notably, the baseline acceptance for vaccination is not high enough in many countries, and the public confidence in vaccination is still weak.
-
▪
COIVD‐19 vaccine acceptance's key barriers were concerns regarding safety, efficacy, and potential adverse effects, consistent with studies in other countries among different population groups.
-
▪
Social media was the commonest knowledge source for COVID‐19 and vaccine. Misinformation and false claims led to vaccine hesitancy. Worldwide, online social media facilitate the uncontrolled spread of fake news and misinformation, leading to infodemic.
6. RECOMMENDATIONS
Since the hesitancy of COVID‐19 vaccination negatively affects the implementation of mass vaccination programs hence the control of the current pandemic, the following measures are recommended to increase vaccine acceptance:
-
▪
Provision of evidence‐based information for COIVID‐19 vaccines with effective and proactive initiatives that keep a vigilant eye to fight misinformation.
-
▪
Organizing expert groups from health professionals and scientists for scientific engagement on COVID‐19 vaccines to provide truthful and understandable information for reducing confusion and doubt and reconstructing a trusting relationship with the public utilizing social and traditional media.
-
▪
Monitoring and confronting misinformation and fake news on COVID‐19 Vaccines, especially on the social media platforms.
7. LIMITATIONS
The current study sample was from medical colleges in only two universities and done on only medically‐oriented students, which may affect generalizability to other college populations elsewhere. The online reaching of the participants within a short time. Respondents may also have been predominantly affected by media attention to the COVID‐19 vaccine, as this topic has not been formally integrated into their curricula.
CONFLICT OF INTEREST
Authors declare no known competing conflicts of interest.
AUTHORS’ CONTRIBUTIONS
All authors contributed significantly to this study. Conceptualization and proposal writing was done by SS, IK, and SA. SS and ES supervised data collection. SS and SA managed the data and wrote the manuscript. All authors have read and approved the manuscript.
PEER REVIEW
The peer review history for this article is available at https://publons.com/publon/10.1002/jmv.26910
Saied SM, Saied EM, Kabbash IA, Abdo SAE.. Vaccine hesitancy: Beliefs and barriers associated with COVID‐19 vaccination among Egyptian medical students. J Med Virol. 2021;93:4280–4291. 10.1002/jmv.26910
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.
REFERENCES
- 1. Callaway E. The race for coronavirus vaccines: a graphical guide. Nature. 2020;580:576‐577. [DOI] [PubMed] [Google Scholar]
- 2. Sharun K, Dhama K, Patel SK, et al. Ivermectin, a new candidate therapeutic against SARSCoV‐2/COVID‐19. Ann Clin Microbiol Antimicrob. 2020b;19(1):23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Sharun K, Tiwari R, Iqbal Yatoo M, et al. Antibodybased immunotherapeutics and use of convalescent plasma to counter COVID‐19: advances and prospects. Expert Opin Biol Ther. 2020d;20(9):1033‐1046. [DOI] [PubMed] [Google Scholar]
- 4. Sharun K, Tiwari R, Dhama J, Dhama K. Dexamethasone to combat cytokine storm in COVID‐19: Clinical trials and preliminary evidence. Int J Surg. 2020c;82:179‐181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Forni G, Mantovani A. COVID‐19 Commission of Accademia Nazionale dei Lincei, Rome. COVID‐19 vaccines: where we stand and challenges ahead. Cell Death Differ. 2021;28(2):626‐639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Dubé E, MacDonald NE. Vaccine Acceptance: Barriers, Perceived Risks, Benefits, and Irrational Beliefs. In the Vaccine Book, Academic Press. 2016:507‐528. [Google Scholar]
- 7. Godlee F. What should we do about vaccine hesitancy? BMJ. 2019;365:l40‐l44. [Google Scholar]
- 8. Larson HJ, Clarke RM, Jarrett C, et al. Measuring trust in vaccination: a systematic review. Hum Vaccin Immunother. 2018;14(7):1599‐1609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Xiao X, Wong RM. Vaccine hesitancy and perceived behavioral control: a meta‐analysis. Vaccine. 2020;38(33):5131‐5138. [DOI] [PubMed] [Google Scholar]
- 10. Chan E‐Y‐Y, Cheng CK‐Y, Tam GC‐H, Huang Z, Lee PY. Willingness of future A/H7N9 influenza vaccine uptake: a cross‐sectional study of Hong Kong community. Vaccine. 2015;33(38):4737‐4740. [DOI] [PubMed] [Google Scholar]
- 11. Abbas KM, Kang GJ, Chen D, Werre SR, Marathe A. Demographics, perceptions, and socioeconomic factors affecting influenza vaccination among adults in the United States. PeerJ. 2018;6:e5171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. MacDonald NE. Vaccine hesitancy: definition, scope and determinants. Vaccine. 2015;32(34):4161‐4164. [DOI] [PubMed] [Google Scholar]
- 13. Padhi BK, Almohaithef MA. Determinants of intent to uptake Coronavirus vaccination among respondents in Saudi Arabia: a web‐based national survey. medRxiv. 2020. [Google Scholar]
- 14. Adebisi YA, Alaran AJ, Bolarinwa OA, Akande‐Sholabi W, Lucero‐Prisno DE. When it is available, will we take it? Public perception of hypothetical COVID‐19 vaccine in Nigeria. medRxiv. Cold Spring Harbor Laboratory Press; 2020. 10.1101/2020.09.24.20200436 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. SAGE Working Group on Vaccine Hesitancy . Report of the SAGE Working Group on Vaccine Hesitancy. Availabe online: https://www.who.int/immunization/sage/meetings/2014/october/1_Report_WORKING_GROUP_vaccine_hesitancy_final.Pdf
- 16. Schwarzinger M, Watson V, Arwidson P, Alla F, Luchini S. COVID‐19 vaccine hesitancy in a representative working‐age population in France: a survey experiment based on vaccine characteristics. Lancet Public Health. 2021;S2468‐2667(21):00012‐00018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Head KJ, Kasting ML, Sturm LA, Hartsock JA, Zimet GD. A National Survey Assessing SARS‐CoV‐2 Vaccination Intentions: Implications for Future Public Health Communication Efforts. Sci Commun. 2020;42(5):698‐723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Reiter PL, Pennell ML, Katz ML. Acceptability of a COVID‐19 vaccine among adults in the United States: How many people would get vaccinated? Vaccine. 2020;38(42):6500‐6507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. World Health Organization . Behavioral considerations for acceptance and uptake of COVID‐19 vaccines: WHO Technical Advisory Group on Behavioral Insights and Sciences for Health, meeting report, 15 October 2020. Geneva: World Health Organization. 2020. https://apps.who.int/iris/handle/10665/337335 [Google Scholar]
- 20. Malik S. COVID‐19 vaccine hesitancy worldwide: a systematic review of vaccine acceptance rates. Preprints. 2020:0717.v1. www.preprints.org [Google Scholar]
- 21. Lazarus JV, Ratzan SC, Palayew A, et al. A global survey of potential acceptance of a COVID‐19 vaccine. Nature Med. 2020:1‐4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. WHO (EMRO) . News: Media center. Available at http://www.emro.who.int/media/news/glimmer-of-hope-covid-19-vaccines-roll-out-in-countries-of-the-eastern-mediterranean-region.html. Last accessed on 21‐2‐2021.
- 23. Tam CC, Qiao S, Li X. Factors associated with decision making on COVID‐19 vaccine acceptance among college students in South Carolina. medRxiv. 2020. 10.1101/2020.12.03.20243543 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Guilamo‐Ramos V, Benzekri A, Thimm‐Kaiser M, Hidalgo A, Perlman DC. Reconsidering assumptions of adolescent and young adult SARS‐CoV‐2 transmission dynamics. Clin Infect Dis. 2020:ciaa1348. https://academic.oup.com/cid/advance-article/doi/10.1093/cid/ciaa1348/5902518 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Bazan D, Nowicki M, Rzymski P. Medical students as the volunteer workforce during the COVID‐19 pandemic: Polish experience. Int J Disaster Risk Reduct. 2021;55:102109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Mohamed‐Hussein AA, Makhlouf H, Abd El Aal H, Kholief K, Saad MM, Abdellal DA. A national survey of potential acceptance of COVID‐19 vaccines in healthcare workers in Egypt. medRxiv. 2021. 10.1101/2021.01.11.21249324 [DOI] [Google Scholar]
- 27. Central Agency for Public Mobilization and Statistics (CAPMAS) . Annual Bulletin of Students Enrolled in the Faculty of Higher Education 2019/2020. https://www.capmas.gov.eg/Pages/Publications.aspx?page_id%A0=%A05104%26YearID%A0=%A023452
- 28. Lucia VC, Kelekar A, Afonso NM. COVID‐19 vaccine hesitancy among medical students. J Public Health (Bangkok). 2020:42(4):fdaa230 10.1093/pubmed/fdaa230 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Barello S, Nania T, Dellafiore F, Graffigna G, Caruso R. Vaccine hesitancy among university students in Italy during the COVID‐19 pandemic. Eur J Epidemiol. 2020;35(8):781‐783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Betsch C, Wicker S. E‐health use, vaccination knowledge and perception of own risk: drivers of vaccination uptake in medical students. Vaccine. 2012;130(6):1143‐1148. [DOI] [PubMed] [Google Scholar]
- 31. Qiao S, Friedman DB, Tam CC, Zeng C, Li X. Vaccine acceptance among college students in South Carolina: Do information sources and trust in information make a difference? medRxiv [Preprint]. 2020. 10.1101/2020.12.02.20242982. PMID: 33300004; PMCID: PMC7724671. [DOI] [PubMed] [Google Scholar]
- 32. Sallam M, Dababseh D, Eid H, et al. High rates of COVID‐19 vaccine hesitancy and its association with conspiracy beliefs: a study in Jordan and Kuwait among other Arab countries. Vaccines. 2021;9(1):42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Talbot TR, Bradley SE, Cosgrove SE, Ruef C, Siegel JD, Weber DJ. Influenza vaccination of healthcare workers and vaccine allocation for healthcare workers during vaccine shortages. Infect Control Hosp Epidemiol. 2005;26(11):882‐890. [DOI] [PubMed] [Google Scholar]
- 34. Stokes DC. Senior medical students in the COVID‐19 response: an opportunity to be proactive. Acad Emerg Med. 2020;27(4):343‐345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. CDC . The Importance of COVID‐19 Vaccination for Healthcare Personnel. 2020. https://www.cdc.gov/coronavirus/2019-cov/vaccines/recommendations/hcp.html
- 36. Humanitarian programme recommendations for COVID‐19 based on social sciences evidence from the DRC Ebola outbreak response . Social science support for COVID‐19: lessons learned brief 3. Cellule d'Analyse en Sciences Sociales (CASS); 2020. https://www.unicef.org/drcongo/media/4131/file/CASS-Brief3-recommendations.pdf. Accessed 29 January 2021
- 37. Schwartz JL. Evaluating and deploying covid‐19 vaccines—the importance of transparency, scientific integrity, and public trust. N Engl J Med. 2020;383(18):1703‐1705. [DOI] [PubMed] [Google Scholar]
- 38. Brewer NT, DeFrank JT, Gilkey MB. Anticipated regret and health behavior: a meta‐analysis. Health Psychol. 2016;35(11):1264‐1275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Behavioural considerations for acceptance and uptake of COVID‐19 vaccines: WHO Technical Advisory Group on Behavioural Insights and Sciences for Health, meeting report, 15 October 2020. Geneva: World Health Organization; 2020. [Google Scholar]
- 40. Karafillakis E, Dinca I, Apfel F, et al. Vaccine hesitancy among healthcare workers in Europe: A qualitative study. Vaccine. 2016;34(41):5013‐5020. [DOI] [PubMed] [Google Scholar]
- 41. Gautam A, Dhara B, Mukherjee D, et al. A digital survey on the acceptance and affordability of COVID 19 vaccine among the people of West Bengal, India‐a survey based study. medRxiv. 2020. [Google Scholar]
- 42. Wang J, Peng Y, Xu H, Cui Z, Williams RO 3rd. The COVID‐19 vaccine race: challenges and opportunities in vaccine formulation. AAPS PharmSciTech. 2020;21(6):225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Naeem SB, Bhatti R, Khan A. An exploration of how fake news is taking over social media and putting public health at risk [published online ahead of print July 12, 2020]. Health Inf Libr J. 2020. 10.1111/hir.12320 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Siegrist M, Zingg A. The role of public trust during pandemics: Implications for crisis communication. European Psychologist. 2014;19(1):23‐32. [Google Scholar]
- 45. Puri N, Coomes EA, Haghbayan H, Gunaratne K. Social media and vaccine hesitancy: new updates for the era of COVID‐19 and globalized infectious diseases. Hum Vaccin Immunother. 2020;16(11):2586‐2593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Harapan H, Wagner AL, Yufika A, et al. Acceptance of a COVID‐19 vaccine in southeast Asia: A cross‐sectional study in Indonesia [published online ahead of print July 14, 2020]. Front Public Health. 2020:8:381. 10.3389/fpubh.2020.00381 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Millner VS, Eichold BH 2nd, Franks RD, Johnson GD. Influenza vaccination acceptance and refusal rates among health care personnel. South Med J. 2010;103(10):993‐998. [DOI] [PubMed] [Google Scholar]
- 48. Synnott Kevin. College Students' COVID‐19 Vaccine Hesitancy. 2020. Available at SSRN: 10.2139/ssrn.3753756 https://ssrn.com/abstract=3753756 [DOI] [Google Scholar]
- 49. Malik AA, McFadden SM, Elharake J, Omer SB. Determinants of COVID‐19 vaccine acceptance in the US. EClinicalMedicine. 2020;26:100495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Rzymski P, Borkowski L, Drąg M, et al. The strategies to support the COVID‐19 vaccination with evidence‐based communication and tackling misinformation. Vaccines (Basel). 2021;9:109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Pogue K, Jensen JL, Stancil CK, et al. Influences on attitudes regarding potential COVID‐19 vaccination in the United States. Vaccines (Basel). 2020;8:582. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.


