Abstract
The novel coronavirus disease 2019 (COVID‐19) pandemic and its unprecedented social restrictions may have serious mental health implications, especially in individuals who have experienced childhood traumatic experiences (CTEs). This prospective study aimed to investigate whether general psychopathology and posttraumatic stress disorder (PTSD) symptom severity increased during the pandemic as compared to prepandemic baseline data collected approximately 1 year earlier. Furthermore, we investigated whether an increase in symptomatology was linked to CTEs and mediated by a lack of perceived social support and fear of COVID‐19. An online survey was administered to 85 individuals, including both participants with PTSD, major depression, or somatic symptom disorder (n = 63) and healthy volunteers (n = 22), during a period of the most severe social restrictions in Germany. The survey included the Childhood Trauma Questionnaire, Brief Symptom Inventory, PTSD Checklist for DSM‐5, ENRICHD Social Support Inventory, and Fear of COVID‐19 Scale. In the whole sample, we found significant increases in general psychopathology and PTSD symptom severity, ω2 = .07–.08, during as compared to before the COVID‐19 pandemic, with CTEs predicting increased PTSD symptom severity, β = .245, p = .042. This effect was mediated by a lack of perceived social support, indirect effect = .101, 95% CI [.013, .209], but not fear of COVID‐19, indirect effect = .060, 95% CI [−.035, .167]. These findings emphasize the importance of interventions that promote social inclusion to mitigate the potentially detrimental effects of public health actions implemented against the COVID‐19 pandemic in individuals with CTEs.
簡體及繁體中文撮要由亞洲創傷心理研究學會翻譯
JOTS‐20‐0330.R2_Seitz_Cantonese
Traditional Chinese
新冠疫症大流行期間兒童創傷暴露個體心理健康的前瞻性研究: 社會支持問題
摘要: 2019年新型冠狀病毒(COVID‐19)大流行及其前所未有的社會限制可能會對心理健康產生嚴重影響, 特別是對那些經歷過童年創傷經歷(CTE)的臨床治療者。這項前瞻性研究旨在調查與大約1年前收集的大流行前的基線數據相比, 疫症期間一般心理病理學和創傷後壓力症(PTSD)症狀嚴重程度是否增加。此外, 我們還調查了症狀的增加是否與CTE有關, 以及是否由缺乏感知的社會支持和對新冠疫症的恐懼所調解。在德國社會限制最嚴重的時期, 我們對85人進行了在線調查, 包括患有創傷後壓力症、嚴重抑鬱症或軀體症狀障礙的參與者(n = 63)和健康志願者(n = 22)。調查包括《兒童創傷問卷》、《簡易症狀表》、《第五版創傷後壓力症調查表》、《充實社會支持量表》和《新冠疫症恐懼調查表》。在整個樣本中, 我們發現在新冠疫症大流行期間, 一般心理病理學和創傷後壓力症症狀嚴重程度比之前有明顯的增加, ω2=0.07‐0.08, 其中CTE預測創傷後壓力症症狀嚴重程度增加, β=0.245, p=0.042。這一效應是由缺乏感知的社會支持所調解的, 間接效應=0.101, 95%CI[.013, .209], 但不是對新冠疫症的恐懼, 間接效應=0.060, 95%CI[‐.035, .167]。這些發現強調了促進社會包容的干預措施的重要性, 以減輕針對新冠疫症大流行病實施的公共衛生行動對童年創傷經歷臨床治療者的潛在不利影響。
Simplified Chinese
新冠疫症大流行期间儿童创伤暴露个体心理健康的前瞻性研究: 社会支持问题
摘要: 2019年新型冠状病毒(COVID‐19)大流行及其前所未有的社会限制可能会对心理健康产生严重影响, 特别是对那些经历过童年创伤经历(CTE)的临床治疗者。这项前瞻性研究旨在调查与大约1年前收集的大流行前的基线数据相比, 疫症期间一般心理病理学和创伤后压力症(PTSD)症状严重程度是否增加。此外, 我们还调查了症状的增加是否与CTE有关, 以及是否由缺乏感知的社会支持和对新冠疫症的恐惧所调解。在德国社会限制最严重的时期, 我们对85人进行了在线调查, 包括患有创伤后压力症、严重抑郁症或躯体症状障碍的参与者(n = 63)和健康志愿者(n = 22)。调查包括《儿童创伤问卷》、《简易症状表》、《第五版创伤后压力症调查表》、《充实社会支持量表》和《新冠疫症恐惧调查表》。在整个样本中, 我们发现在新冠疫症大流行期间, 一般心理病理学和创伤后压力症症状严重程度比之前有明显的增加, ω2=0.07‐0.08, 其中CTE预测创伤后压力症症状严重程度增加, β=0.245, p=0.042。这一效应是由缺乏感知的社会支持所调解的, 间接效应=0.101, 95%CI[.013, .209], 但不是对新冠疫症的恐惧, 间接效应=0.060, 95%CI[‐.035, .167]。这些发现强调了促进社会包容的干预措施的重要性, 以减轻针对新冠疫症大流行病实施的公共卫生行动对童年创伤经历临床治疗者的潜在不利影响。
Recent literature has proposed that investigations of the effects of the novel coronavirus disease 2019 (COVID‐19) pandemic on mental health in vulnerable groups should be an immediate research priority (Holmes et al., 2020). Corresponding to a recent review article, the extensive public health actions of “social distancing” along with the consequences of the illness itself are likely to have serious, potentially long‐lasting mental health implications for the general population (Brooks et al., 2020). To curb the spread of the virus, millions of individuals have been confined to their homes, and human contact has been fundamentally reduced.
Individuals who have been exposed to childhood traumatic experiences (CTEs) might be a particularly vulnerable group. According to the stress sensitization hypothesis (Hammen et al., 2000), exposure to CTEs, such as abuse and neglect, decreases stress tolerance, which, in turn, increases vulnerability to psychopathology in the face of subsequent stressful life events. On the biological level, potential mechanisms underlying stress sensitization effects involve dysregulation of stress response systems, metabolic dysregulation, and inflammation, which may increase both vulnerabilities to stress and the risk for psychiatric disorders (Heim et al., 2019). Within this framework, social support has been conceptualized as a potential protective factor in buffering the detrimental effects of CTEs (Heim et al., 2019). Research conducted before the COVID‐19 pandemic has provided evidence for the proposed stress sensitization effects of CTEs as well as the protective effects of social support. Research suggests that CTEs are associated with elevated levels of adult loneliness and psychopathology, including symptoms of posttraumatic stress disorder (PTSD; Evans et al., 2013; McLaughlin et al., 2010; Shevlin et al., 2015). Loneliness (i.e., perceived social isolation) and a lack of social support have been shown to mediate the effect of CTEs on adult psychopathology (Shevlin et al., 2015; Vranceanu et al., 2007) and psychological distress throughout the lifetime (Cosco et al., 2018). Moreover, CTEs have been associated with higher levels of health anxiety in clinical and general population samples (Thorgaard et al., 2018). Thus, the COVID‐19 pandemic and its associated social restrictions might place an exceptional strain on individuals, both with and without a history of mental illness, who have experienced childhood trauma.
Although research exploring the associations between previous trauma exposure and psychological distress during the COVID‐19 pandemic is still in its initial stages, a growing body of literature supports the notion that trauma‐exposed individuals could be even more liable to the implications of the COVID‐19 crisis than their unexposed peers. In several cross‐sectional studies, individuals who experienced adverse events during childhood or previous traumatic events showed elevated levels of psychopathology, including symptoms of anxiety, depression, and PTSD, during the COVID‐19 pandemic as compared to individuals who did not experience such events (Chi et al., 2020; Lahav et al., 2020; Tsur & Abu‐Raiya, 2020). Moreover, in a longitudinal study, a higher perceived risk of COVID‐19 predicted higher levels of depressive symptoms during the COVID‐19 pandemic, particularly among adults with adverse childhood experiences assessed before the COVID‐19 pandemic (Kim et al., 2020). Due to the cross‐sectional nature of mental health indicators in these previous studies, however, the question remains regarding whether CTEs are, in fact, associated with increases in psychopathology in general and PTSD symptom severity in particular during as compared to before the COVID‐19 pandemic.
Concerning potential protective factors, several cross‐sectional studies have found perceived social support to be associated with lower levels of psychopathology, including PTSD symptomatology (e.g., González‐Sanguino et al., 2020; Liu et al., 2020), whereas a lack of perceived social support has been associated with elevated levels of depressive symptomatology and psychological distress (e.g., Iob et al., 2020; Yu et al., 2020) during the COVID‐19 pandemic. Of note, in a longitudinal study of adults in the United States, perceived social support was shown to be associated with a smaller increase in depression and anxiety symptoms during as compared to before the COVID‐19 pandemic (Marroquín et al., 2020), suggesting that social support might actually mitigate the adverse mental health effects of the pandemic.
The aim of the current prospective study was to investigate general psychopathology and PTSD symptom severity during the COVID‐19 pandemic as compared to previously collected baseline data in a group of childhood trauma‐exposed individuals. The sample included participants with a broad range of CTE severity and consisted of individuals with psychiatric disorders known to be associated with high CTE prevalence rates as well as healthy volunteers (HVs). Due to the rapid spread of COVID‐19, the German government implemented unprecedented measures restricting daily life and social interactions as of March 16, 2020 (Robert Koch Institute [RKI], 2020b), with the most severe shut‐down lasting up to May 18, 2020 (Schumacher, 2020). Against this background, we expected to find increased general psychopathology and PTSD symptom severity among the whole sample during this phase of the most comprehensive social restrictions. In addition, we expected that CTEs would predict increases in both general psychopathology and PTSD symptom severity and that these effects would be mediated by a lack of perceived social support and fear of COVID‐19.
Method
Participants
For the current study, 85 individuals with varying levels of CTEs participated in an online survey. In total, 67 of these participants were women, and the mean participant age was 31.3 years (SD = 11.1, range: 18–59 years). Participants in the current study were part of a larger study on the shared effects of CTEs on social information processing across different psychiatric disorders that have demonstrated high prevalence rates of CTEs (Nelson et al., 2012; Scott et al., 2010); the larger study also included a healthy volunteer (HV) group, for a total of 140 participants. The original study is part of the German Research Foundation's Research Training Group 2350, dedicated to investigating the impact of adverse childhood experiences on psychosocial and somatic conditions across the life span.
For the original study, participants with psychiatric disorders (n = 104) were recruited through a clinical referral from inpatient and outpatient units (n = 71) as well as via advertisements (n = 33), and HVs (n = 36) were recruited through advertisements. The inclusion criterion for participants with psychiatric disorders was a current diagnosis of PTSD, major depression (MD), or somatic symptom disorder (SSD) that had been assigned as the patient's first lifetime psychiatric diagnosis. Psychiatric disorders, measured per the criteria in the Diagnostic and Statistical Manual of Mental Disorders (fifth ed.; DSM‐5), were assessed at baseline using the Structured Clinical Interview for DSM‐5 (SCID‐5; Beesdo‐Baum et al., 2019). Due to high comorbidity rates among the three included disorders, participants could be diagnosed with up to three of these disorders; diagnostic group allocation was based on the current diagnosis that had been made first during the participant's lifetime. Following a dimensional conceptualization, HVs were included to establish a sample of varying levels of CTEs and psychopathological symptoms. The inclusion criterion for HVs was the absence of current or past manifest psychiatric Axis I disorders at baseline, as assessed using the SCID‐5. The exclusion criteria for all participants (i.e., those with psychiatric disorders and HVs) were (a) age under 18 years or over 60 years; (b) neurological disorders; (c) current substance abuse at baseline, assessed via urine toxicology screening and the SCID‐5; (d) severe medical illness; (e) pregnancy; and (f) left‐handedness. Additional exclusion criteria for participants with psychiatric disorders were lifetime diagnoses of schizophrenia, schizoaffective, or bipolar disorder and self‐reported substance dependence in the last 2 years. Psychotropic medications were allowed for participants with psychiatric disorders provided this use comprised their regularly prescribed antidepressants, antipsychotics (sleep‐inducing effect only), and/or anticonvulsants (i.e., pregabalin, pain‐relieving effect only).
For the online survey used in the present study, the sample included participants with a DSM‐5 diagnosis of PTSD (n = 17), MD (n = 20), and SSD (n = 26) as a first‐lifetime and current diagnosis at baseline, as well as HVs (n = 22). Participants of the original study (N = 140) and those who completed the current online survey (n = 85) did not differ significantly regarding age; gender; educational attainment; CTEs, as assessed using the Childhood Trauma Questionnaire (CTQ) total score (Klinitzke et al., 2012); general psychopathology, as assessed using the Brief Symptom Inventory Global Severity Index (BSI GSI; Franke, 2000); and PTSD symptom severity, as assessed using the PTSD Checklist for DSM‐5 (PCL‐5) total score (Krüger‐Gottschalk et al., 2017) at baseline. As expected, participants covered a broad range of CTE severity. Most participants came from Baden‐Wuerttemberg, the region with the second‐highest cumulative incidence of COVID‐19 cases in Germany at the beginning of the current online survey period (RKI, 2020a). One participant was previously infected with COVID‐19 (1.2%), and two (2.4%), 13 (15.3%), and 20 (23.5%) participants encountered cases of COVID‐19 in their family, personal, or professional environments, respectively. Demographic and clinical characteristics of the online survey sample measured before the COVID‐19 pandemic are presented in Table 1.
Table 1.
Demographic and Clinical Characteristics of the Online Survey Sample Measured Before the COVID‐19 Pandemic
| Baseline (September 2018–November 2019) | |||
|---|---|---|---|
| Characteristic | % | M | SD |
| Gender | |||
| Female | 78.8 | ||
| Male | 21.2 | ||
| Age, years | 31.31 | 11.12 | |
| Educational level, years | 12.16 | 1.49 | |
| Childhood traumatic experiences | |||
| CTQ total score | 51.58 | 21.10 | |
| CTQ Emotional Abuse | 13.08 | 6.22 | |
| CTQ Physical Abuse | 8.87 | 5.37 | |
| CTQ Sexual Abuse | 7.19 | 4.51 | |
| CTQ Emotional Neglect | 14.14 | 5.66 | |
| CTQ Physical Neglect | 8.29 | 3.79 | |
| General psychopathology (BSI GSI) | 0.96 | 0.70 | |
| PTSD symptom severity (PCL‐5 total score) | 22.28 | 20.04 | |
| Current medication | |||
| Antidepressants | 31.8 | ||
| Antipsychotics a | 5.9 | ||
| Anticonvulsants (pregabalin) | 1.2 | ||
| Current Axis I disorders | |||
| PTSD b | 23.5 | ||
| MD b | 34.1 | ||
| SSD b | 30.6 | ||
| Other anxiety disorders | 16.5 | ||
| Other affective disorders | 5.9 | ||
| Other somatization disorders | 0 | ||
| Eating disorders | 5.9 | ||
| Substance use disorders | 0 | ||
Note. BSI GSI = Brief Symptom Inventory Global Severity Index; COVID‐19 = coronavirus disease 2019; CTQ = Childhood Trauma Questionnaire; MD = major depression; PCL‐5 = Posttraumatic Stress Disorder (PTSD) Checklist for DSM‐5; SSD = somatic symptom disorder.
a Sleep‐inducing effect only. b Individuals were assigned to the group of participants with PTSD, MD, or SSD if they had a current diagnosis of at least one of these disorders at baseline and this diagnosis was their first lifetime psychiatric disorder diagnosis. Due to comorbidities among these disorders, the percentages of participants with a current diagnosis of PTSD, MD, and SSD are higher in the table than as reported in the main text.
Procedure
For the original study, interview and self‐report data on CTEs, clinical characteristics, and psychiatric disorders were collected between September 2018 and November 2019 (i.e., 2–16 months before the COVID‐19 outbreak in Germany; see Table 1). Across participants, the average time lag between the baseline assessment and those completed during the COVID‐19 outbreak in Germany was less than 1 year (M = 11.0, SD = 4.1, range: 5–19 months).
From April 16, 2020, to May 18, 2020, all participants of the original study who gave their written informed consent to be contacted again (n = 127) were invited via e‐mail or telephone to take part in the current online survey. In total, 26 participants could not be reached, and eight refused to participate. After having received comprehensive information about the current study, 93 individuals (n = 68 participants with psychiatric disorders, n = 25 HVs) were sent a designated code. Of these participants, 85 (n = 63 with psychiatric disorders, n = 22 HVs) participated in the online survey. The survey period corresponded with the stage of the most severe social restrictions during the COVID‐19 pandemic in Germany (e.g., physical distancing; contact restrictions; lockdowns of schools, cultural facilities, and leisure facilities). The study was approved by the Ethics Committee of the Medical Faculty of Heidelberg University (Heidelberg, Germany). All participants provided written informed consent and were reimbursed for their participation.
Measures
CTEs
Childhood traumatic experiences were measured at baseline using 25 of the 28 items on the German version of the CTQ (Klinitzke et al., 2012), a self‐report questionnaire used to assess emotional, physical, and sexual abuse as well as emotional and physical neglect. The five childhood trauma–related subscales consist of five items each, with items rated on a 5‐point Likert scale ranging from 1 (not at all) to 5 (very often). Scores on the total scale range from 25 to 125, and subscale scores range from 5 to 25, with higher scores indicating more severe abuse or neglect. Cutoff scores of 8 for the Physical Abuse, Sexual Abuse, and Physical Neglect subscales; 10 for the Emotional Abuse subscale; and 15 for the Emotional Neglect subscale have been recommended to indicate the presence of CTEs (Walker et al., 1999). In the present sample, the internal consistency of four of the five subscales ranged from good (i.e., Cronbach's α = .89 for Emotional Abuse and Physical Abuse) to excellent (i.e., Cronbach's α = .95 for Sexual Abuse); Cronbach's alpha for the Physical Neglect subscale was lower at .69.
General Psychopathology
General psychopathology was measured before and during the COVID‐19 pandemic using the German version of the BSI (Franke, 2000), a 53‐item, self‐report questionnaire used to assess past‐week clinically relevant symptoms in nine dimensions (i.e., somatization, obsession–compulsion, interpersonal sensitivity, depression, anxiety, hostility, phobic anxiety, paranoid ideation, and psychoticism). Items are rated on a 5‐point Likert scale ranging from 0 (not at all) to 4 (extremely). The BSI GSI, defined as the mean of all items, ranges from 0 to 4, with higher scores reflecting more severe psychopathology. A BSI GSI cutoff score of 0.62 has been proposed to indicate significant psychological distress (Franke, 2000), whereas a BSI GSI cutoff score of 0.48 has been suggested to discriminate between outpatients with common psychiatric disorders (i.e., mood, anxiety, and somatoform disorders) and healthy individuals (Schulte‐van Maaren et al., 2012). In the present sample, the BSI demonstrated excellent internal consistency both at baseline, Cronbach's α = .97, and during the COVID‐19 pandemic, Cronbach's α = .97.
PTSD Symptoms
The severity of PTSD symptoms was measured before and during the COVID‐19 pandemic using the German version of the 20‐item, self‐report PCL‐5 (Krüger‐Gottschalk et al., 2017). The PCL‐5 is used to measure past‐month symptom severity, with items rated on a 5‐point Likert scale ranging from 0 (not at all) to 4 (extremely). Scores on the total scale range from 0 to 80, with higher scores indicating more severe PTSD symptomatology. When used as a screening tool, scores between 28 and 37 have been proposed to indicate probable PTSD (Ashbaugh et al., 2016; Blevins et al., 2015). In the current sample, the PCL‐5 demonstrated excellent internal consistency both at baseline, Cronbach's α = .95, and during the COVID‐19 pandemic, Cronbach's α = .97.
Social Support
Perceived social support was assessed during the COVID‐19 pandemic using the German version of the five‐item, self‐report ENRICHD Social Support Inventory (ESSI; Cordes et al., 2009). Items are rated on a 5‐point Likert scale ranging from 1 (none of the time) to 5 (all of the time). Scores on the total scale range from 5 to 25, with higher scores reflecting higher levels of perceived social support. A lack of social support is indicated by a total score of 18 or lower as well as at least two items rated with a score of 3 or lower (Cordes et al., 2009). In the present sample, the ESSI demonstrated excellent internal consistency, Cronbach's α = .94.
Fear and Personal Impact of COVID‐19
Participants’ fear of COVID‐19 was measured using the translated, but not yet validated, German version of the seven‐item, self‐report Fear of COVID‐19 Scale (FCV‐19S; Ahorsu et al., 2020), which is used to assess worries and anxiety symptoms associated with COVID‐19. Respondents score items on a 5‐point Likert scale ranging from 1 (strongly disagree) to 5 (strongly agree), with total scores ranging from 7 to 35 and higher scores indicating a higher degree of COVID‐19–related fear. Example items include “It makes me uncomfortable to think about coronavirus‐19” and “I am afraid of losing my life because of coronavirus‐19” (Ahorsu et al., 2020, p. 8). At the time of writing, no norms for interpreting FCV‐19S scores had yet been published. In the present sample, the FCV‐19S demonstrated excellent internal consistency, Cronbach's α = .93.
In addition to completing the FCV‐19S, participants were asked to indicate whether and how they had been personally impacted by COVID‐19 (i.e., if they themselves had suffered from COVID‐19 or if they encountered cases of COVID‐19 in their family or personal or professional environment).
Psychiatric Disorders
Axis I disorders were assessed at baseline by qualified diagnosticians (i.e., at least a master's degree in clinical psychology) using the German version of the SCID‐5 (Beesdo‐Baum et al., 2019). Before the study began, diagnosticians underwent standardized diagnostic training, leading to an interrater reliability of κ = 1.00, which can be qualified as “excellent" according to Cicchetti (1994).
Data Analysis
Statistical analyses were conducted using SPSS (Version 26). The online survey software used in the original and current study was implemented with a forced‐answering format, allowing participants to skip items only temporarily and requiring them to provide answers to all questions before submitting the whole survey; thus, there were no missing data in our data set. First, we used paired t tests to analyze whether general psychopathology and PTSD symptom severity increased during the COVID‐19 pandemic. In addition, we performed exploratory analyses (i.e., multivariate analyses of variance [MANOVAs], Mann Whitney U tests) to test for significant differences between participants with psychiatric disorders and HVs with regard to clinical characteristics (i.e., CTE severity, general psychopathology, PTSD symptom severity, perceived social support, and fear of COVID‐19). Effect sizes were calculated as omega squared (ω2) values. According to Kirk (1996), small, moderate, and large effects are defined as omega squared values of .01, .06, and .14, respectively. Next, we calculated Pearson product‐moment correlation coefficients to determine whether increases in general psychopathology and PTSD symptom severity were associated with self‐reported CTEs. As we hypothesized that there would be a positive association between increases in general psychopathology or PTSD symptom severity and CTE severity, we conducted one‐tailed correlation analyses. Finally, we analyzed whether the association between CTEs (i.e., independent variable) and increased PTSD symptom severity (i.e., dependent variable) was mediated by perceived social support (Mediator 1) and fear of COVID‐19 (Mediator 2), using the PROCESS macro (Hayes, 2018). Mediators were tested simultaneously. We controlled for the potential effects of mental illness history and general psychopathology before the COVID‐19 pandemic by adding a dummy‐coded group variable (i.e., participants with psychiatric disorders vs. HVs) and baseline BSI GSI score as covariates in the mediation model (i.e., Model 4 in PROCESS). Bootstrapping (20,000 resamples) was employed to estimate the 95% confidence intervals of the indirect effects. Indirect effects were considered statistically significant if the confidence interval did not include zero. All paths are reported as standardized ordinary least squares regression coefficients. According to power analyses conducted before implementing the current online survey, our sample size was sufficient to detect a small‐to‐moderate effect in paired t tests (ω2 = .02), moderate correlations (r = .27), and a moderate effect (ω2 = .13) in a mediation model with up to five predictors with a power of .80 or above (Faul et al., 2007).
Results
During the COVID‐19 pandemic, general psychopathology (BSI GSI, M = 1.16, SD = 0.77) and PTSD symptom severity (PCL‐5 total score, M = 27.02, SD = 22.66) increased significantly in the whole sample, t(84) = 2.96, p = .004, ω2 = .08 for the BSI GSI and t(84) = 2.77, p = .007, ω2 = .07 for the PCL‐5 total score. Of note, 69 of 85 participants (81.2%) indicated on the PCL‐5 that their PTSD symptomatology was related to stressful life events that occurred before their 18th birthday. No participants identified exposure to COVID‐19 as their most stressful life event (i.e., index event) and the cause of their PTSD symptomatology.
As shown in Table 2, there were no significant differences between participants with psychiatric disorders and HVs with regard to increases in general psychopathology and PTSD symptom severity. The two groups also did not differ significantly in terms of CTE severity, perceived social support, or fear of COVID‐19. However, the groups differed significantly with regard to general psychopathology and PTSD symptom severity both before and during the COVID‐19 pandemic. Considering heterogeneous variances, we analyzed these data using nonparametric Mann‐Whitney U tests, with the results yielding significant group differences in general psychopathology and PTSD symptom severity both before and during the COVID‐19 pandemic (see Table 2 for mean values, standard deviations, and group comparisons).
Table 2.
Clinical Characteristics of Participants with Psychiatric Disorders and Healthy Volunteers, Measured Before and During the COVID‐19 Pandemic
| Participants with psychiatric disorders (n = 63) | Healthy volunteers (n = 22) | Group comparison | |||||
|---|---|---|---|---|---|---|---|
| Clinical characteristic | M | SD | M | SD | F(1, 83) | U | ω2 |
| Childhood traumatic experiences (CTQ total score) | 53.25 | 22.31 | 46.77 | 16.71 | 1.55 | .01 | |
| General psychopathology (BSI GSI) | |||||||
| Baseline | 1.23 | 0.61 | 0.20 | 0.11 | 10.50*** | .55 | |
| During COVID‐19 pandemic | 1.35 | 0.72 | 0.61 | 0.62 | 249.50*** | .23 | |
| Increase (baseline–pandemic) | 0.12 | 0.59 | 0.41 | 0.66 | 3.60 | .03 | |
| PTSD symptom severity (PCL‐5 total score) | |||||||
| Baseline | 28.00 | 19.93 | 5.91 | 7.37 | 200.00*** | .29 | |
| During COVID‐19 pandemic | 31.49 | 23.05 | 14.23 | 15.92 | 372.00** | .12 | |
| Increase (baseline–pandemic) | 3.49 | 16.88 | 8.32 | 11.81 | 1.53 | .01 | |
| Perceived social support (ESSI total score) | 18.75 | 5.34 | 20.77 | 4.45 | 2.55 | .02 | |
| Fear of COVID‐19 (FCV‐19S total score) | 13.97 | 6.77 | 12.05 | 7.03 | 1.29 | < .01 | |
Note. BSI GSI = Brief Symptom Inventory Global Severity Index; COVID‐19 = coronavirus disease 2019; CTQ = Childhood Trauma Questionnaire; ESSI = ENRICHD Social Support Inventory; FCV‐19S = Fear of COVID‐19 Scale; PCL‐5 = Posttraumatic Stress Disorder (PTSD) Checklist for DSM‐5.
** p < .01. *** p < .001.
In the whole sample, CTE severity was associated with increases in PTSD symptom severity, r = .19, p = .040, but not with increased general psychopathology, r < −.01, p = .489, during the COVID‐19 pandemic. In the next step, we focused our mediation model on the association between CTE severity and increases in PTSD symptom severity. As no significant group differences were found regarding CTE severity (i.e., independent variable), increases in PTSD symptom severity (i.e., dependent variable), perceived social support, and fear of COVID‐19 (i.e., mediators), we analyzed participants with psychiatric disorders and HVs together while controlling for the potential effects of baseline history of mental illness and general psychopathology. The severity of CTEs predicted increases in PTSD symptom severity during the COVID‐19 pandemic, β = .245, p = .042, (i.e., “total effect”). The severity of CTEs also predicted perceived social support, β = −.369, p = .002, but not fear of COVID‐19, β = .154, p = .199. Furthermore, a perceived lack of social support, β = −.274, p = .012, as well as fear of COVID‐19, β = .390, p < .001, predicted increases in PTSD symptom severity. Together, CTE severity, perceived lack of social support, and fear of COVID‐19 accounted for approximately 26% of the variance in increases in PTSD symptom severity, R2 = .257, F(5, 79) = 5.46, p < .001, after controlling for history of mental illness and general psychopathology at baseline. The effect of CTEs on increased PTSD symptom severity was mediated by a perceived lack of social support, indirect effect = .101 (SE = .050), 95% CI [.013, .209], but not fear of COVID‐19, indirect effect = .060 (SE = .051), 95% CI [−.035, .167] (see Figure 1 for the total, direct, and indirect effects in the mediation model).
Figure 1.
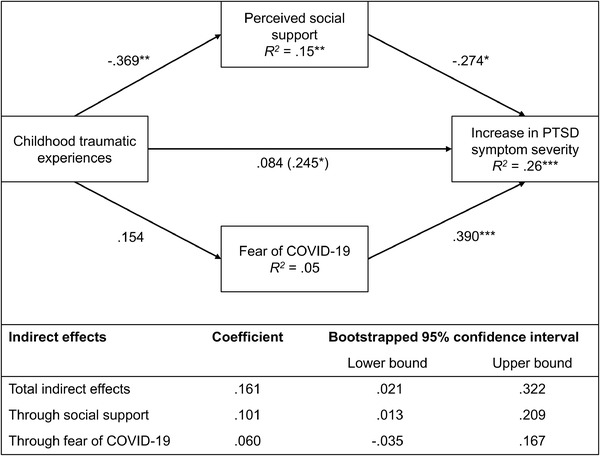
Mediation Model of Childhood Traumatic Experiences and Increase in PTSD Symptom Severity During the COVID‐19 Pandemic
Note. History of mental illness (i.e., dummy‐coded group variable, participants with psychiatric disorders vs. healthy volunteers) and general psychopathology (i.e., Brief Symptom Inventory Global Severity Index score) at baseline were used as covariates. All paths are reported as standardized ordinary least square regression coefficients, with total effects in brackets. * p < .05. ** p < .01. *** p < .001.
Discussion
In the current study, we aimed to investigate the mental health impact of the COVID‐19 pandemic among individuals with varying levels of CTEs compared to previously collected baseline data. Participants both with and without psychiatric disorders experienced increases in general psychopathology and PTSD symptom severity during the COVID‐19 pandemic compared to baseline data collected 2–16 months before the COVID‐19 outbreak in Germany. These results are in line with two recent meta‐analyses that reported heightened psychological distress with increased levels of depression and anxiety in general population samples during the COVID‐19 pandemic (Salari et al., 2020), particularly a heightened prevalence of posttraumatic stress symptoms (Cooke et al., 2020). However, thus far, most studies have relied on cross‐sectional data, and pre–post analyses with prepandemic data have been scarce. Our longitudinal results suggest that the COVID‐19 pandemic and its associated public health actions might lead to a rise in psychopathological symptoms in general and trauma‐related symptomatology in particular, particularly among susceptible individuals with preexisting mental health conditions and/or a history of CTEs.
Consistent with our findings, PTSD has recently been characterized as “the second tsunami” (Dutheil et al., 2020, p. 1) of the COVID‐19 pandemic, considering that elevated levels of PTSD symptomatology among both the general and high‐risk populations constitute a common consequence of major disasters (Dutheil et al., 2020). Prior research suggests that the COVID‐19 pandemic, including the strict measures enacted to counteract the spread of the virus and the fear of contracting a potentially fatal virus, might be perceived as a traumatic event (Forte et al., 2020; Hawryluck et al., 2004). On the PCL‐5, however, no participants in the current sample identified the COVID‐19 pandemic as their most stressful life event and the cause of their PTSD symptomatology. Thus, in the current sample of participants with varying levels of CTEs, it seems that being exposed to the COVID‐19 pandemic and its associated countermeasures led to an aggravation of already existing trauma‐related symptoms. Corroborating a stress sensitization hypothesis (Hammen et al., 2000), the current pandemic is likely to pose an additional major strain on individuals with an already heightened liability to psychopathology that stems from existing psychiatric disorders and/or CTEs. Stressors associated with the pandemic, such as anticipatory fear of contagion, loneliness, and threats to individual freedom, as well as feelings of helplessness and frustration (Forte et al., 2020) in the face of increasing unemployment rates and economic losses, might therefore exacerbate symptoms related to prior, entirely unrelated traumatic events.
Higher levels of CTEs were associated with a higher degree of increased PTSD symptom severity during the COVID‐19 pandemic compared to baseline, but they were unrelated to increased general psychopathology. In line with recent cross‐sectional findings (Chi et al., 2020; Lahav, 2020; Tsur & Abu‐Raiya, 2020), the current prospective results suggest that previous trauma exposure is associated with elevated levels of psychopathology during the COVID‐19 pandemic. Contrary to previous cross‐sectional findings, however, the present longitudinal findings indicate that CTE severity is associated particularly with a rise in trauma‐related symptomatology rather than general psychopathology during the current public health emergency.
Low levels of perceived social support—but not the fear of COVID‐19—mediated this association. Following a recent transdiagnostic model of mechanisms linking CTEs to psychopathology (McLaughlin et al., 2020), perceived social support might be conceptualized as a key protective factor that buffers the detrimental effects of CTEs on multiple forms of psychopathology. Building on and extending upon this evidence‐based framework, the present results suggest that in individuals with CTEs, perceived social support might mitigate the psychological consequences of the social lockdown implemented to stem the spread of the COVID‐19 pandemic. In line with recent studies (e.g., González‐Sanguino et al., 2020; Liu et al., 2020; Marroquín et al., 2020), our findings emphasize once more the importance of maintaining social contact (e.g., via social media, virtual workspaces, tele–mental health services) to reduce the detrimental effects of perceived social isolation (Cao et al., 2020; Galea et al., 2020). Although the fear of COVID‐19 did not mediate the effect of CTEs in our sample, it was still significantly associated with increases in PTSD symptom severity. Thus, alleviating worries about COVID‐19 by providing accurate, up‐to‐date information (Druss, 2020) while raising awareness about the adverse effects associated with frequent media consumption concerning COVID‐19 (Bendau et al., 2020; Gao et al., 2020) may be another useful strategy to reduce distress and improve mental health, particularly in vulnerable groups.
Several limitations of the present study should be acknowledged. First, mental health assessment during the COVID‐19 pandemic was solely based on online, self‐report questionnaires, including a nonvalidated German version of the Fear of COVID‐19 Scale. Thus, interview data on psychiatric diagnoses could not be ascertained for the pandemic phase of the study. Second, a disproportionate number of female participants completed the online survey, which corresponds with the uneven distribution of sexes in the original study. Female sex has been identified as a risk factor for higher levels of anxiety and depression during the COVID‐19 pandemic in both the general and high‐risk populations (Vindegaard & Benros, 2020). Hence, our results might overestimate increases in psychopathology in individuals who report male or nonbinary gender, with or without a history of mental illness, who have been exposed to childhood trauma. Third, despite our prospective study design, both mediators (i.e., perceived social support, fear of COVID‐19) were measured only during the COVID‐19 outbreak in Germany and, thus, at the same time point as the outcome variable. Although the ability to analyze changes in general psychopathology and PTSD symptom severity during as compared to before the pandemic represents a major strength of our study, it would have also been desirable to look at changes in perceived social support between these two assessment points. To the best of our knowledge, no longitudinal study has been published yet that analyzes the effects of the COVID‐19 pandemic on perceived social support as assessed before and during the pandemic. Future research is therefore needed to uncover the impact of the pandemic on social resources, which appear to play a crucial role in limiting the negative effects of social distancing measures. Finally, as our rather small sample size did not allow for detecting small effects in the mediation model or conducting subgroup analyses, future studies with larger samples of childhood trauma–exposed individuals, both with and without a history of mental illness, are needed to gain a more comprehensive understanding of the association between CTEs and the mental health impact of the COVID‐19 pandemic. In addition, these larger replication studies would provide researchers with the opportunity to examine potential moderation effects to understand whether increases in trauma‐related psychopathology vary by individual characteristics, such as sex, or differential experiences, such as CTE type.
Despite these limitations, the current prospective study improves our understanding of how individuals with CTEs are affected by the COVID‐19 pandemic. Based on our findings, individuals with CTEs might develop elevated levels of PTSD symptomatology during the current health crisis. Moreover, our study revealed the mediating role of perceived social support in the association between CTEs and increased PTSD symptom severity during the COVID‐19 pandemic. Our results shed light on how interventions that foster social inclusion may reduce the pervasive psychological consequences associated with social lockdowns in individuals with CTEs. Thus, researchers and clinicians should be advised to consider indicators of previous trauma exposure in general and CTEs in particular when evaluating or treating the impact of the COVID‐19 pandemic and its associated social restrictions on public mental health. By doing so, particularly vulnerable individuals could be identified and provided with targeted treatment or, preferably, prevention strategies that promote a sense of social inclusion and resilience in these challenging times.
Open Practices Statement
The current study reported in this article was not formally preregistered. Neither the data nor the materials have been made available on a permanent third‐party archive; requests for the data or materials should be sent via email to the lead author at katja.seitz@med.uni-heidelberg.de .
Acknowledgments
Open access funding enabled and organized by Projekt DEAL.
The authors have no conflicts of interest to disclose. This work was funded by a grant from the German Research Foundation (Deutsche Forschungsgemeinschaft [DFG]), awarded to Sabine C. Herpertz and Katja Bertsch within the GRK2350/1–324164820 (speaker: Christian Schmahl). The funding source was not involved in the collection, analysis, and interpretation of data; in the writing of the manuscript; or in the decision to submit the article for publication. The authors would like to thank E. Blume, N. Ehler, and the team of the GRK2350/1 for participant recruitment, data collection, and organization.
References
- Ahorsu, D. K. , Lin, C. ‐Y. , Imani, V. , Saffari, M. , Griffiths, M. D. , & Pakpour, A. H. (2020). The Fear of COVID‐19 Scale: Development and initial validation. International Journal of Mental Health And Addiction. Advance online publication. 10.1007/s11469-020-00270-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ashbaugh, A. R. , Houle‐Johnson, S. , Herbert, C. , El‐Hage, W. , & Brunet, A. (2016). Psychometric validation of the English and French versions of the Posttraumatic Stress Disorder Checklist for DSM‐5 (PCL‐5). PLOS ONE, 11(10), e0161645. 10.1371/journal.pone.0161645 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beesdo‐Baum, K. , Zaudig, M. , & Wittchen, H.‐U. (2019). SCID‐5‐CV. Strukturiertes Klinisches Interview für DSM‐5®‐Störungen – Klinische Version. Deutsche Bearbeitung des Structured Clinical Interview for DSM‐5® Disorders – Clinician Version von Michael B. First, Janet B. W. Williams, Rhonda S. Karg, Robert L. Spitzer. [SCID‐5‐CV. Structured Clinical Interview for DSM‐5® disorders – Clinical Version. German adaptation of the Structured Clinical Interview for DSM‐5 disorders – Clinician Version by Michael B. First, Janet B. W. Williams, Rhonda S. Karg, Robert L. Spitzer]. Hogrefe.
- Bendau, A. , Petzold, M. B. , Pyrkosch, L. , Mascarell Maricic, L. , Betzler, F. , Rogoll, J. , Große, J. , Ströhle, A. , & Plag, J. (2020). Associations between COVID‐19–related media consumption and symptoms of anxiety, depression, and COVID‐19–related fear in the general population in Germany. European Archives of Psychiatry and Clinical Neuroscience. Advance online publication. 10.1007/s00406-020-01171-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blevins, C. A. , Weathers, F. W. , Davis, M. T. , Witte, T. K. , & Domino, J. L. (2015). The Posttraumatic Stress Disorder Checklist for DSM‐5 (PCL‐5): Development and initial psychometric evaluation. Journal of Traumatic Stress, 28(6), 489–498. 10.1002/jts.22059 [DOI] [PubMed] [Google Scholar]
- Brooks, S. K. , Webster, R. K. , Smith, L. E. , Woodland, L. , Wessely, S. , Greenberg, N. , & Rubin, G. J. (2020). The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. The Lancet, 395(10227), 912–920. 10.1016/S0140-6736(20)30460-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cao, W. , Fang, Z. , Hou, G. , Han, M. , Xu, X. , Dong, J. , & Zheng, J. (2020). The psychological impact of the COVID‐19 epidemic on college students in China. Psychiatry Research, 287, 112934. 10.1016/j.psychres.2020.112934 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chi, X. , Becker, B. , Yu, Q. , Willeit, P. , Jiao, C. , Huang, L. , Hossain, M. M. , Grabovac, I. , Yeung, A. , Lin, J. , Veronese, N. , Wang, J. , Zhou, X. , Doig, S. R. , Liu, X. , Carvalho, A. F. , Yang, L. , Xiao, T. , Zou, L. , … Solmi, M. (2020). Prevalence and psychosocial correlates of mental health outcomes among Chinese college students during the coronavirus disease (COVID‐19) pandemic. Frontiers in Psychiatry, 11, 803. 10.3389/fpsyt.2020.00803 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cicchetti, D. V. (1994). Guidelines, criteria, and rules of thumb for evaluating normed and standardized assessment instruments in psychology. Psychological Assessment, 6(4), 284–290. 10.1037/1040-3590.6.4.284 [DOI] [Google Scholar]
- Cooke, J. E. , Eirich, R. , Racine, N. , & Madigan, S. (2020). Prevalence of posttraumatic and general psychological stress during COVID‐19: A rapid review and meta‐analysis. Psychiatry Research, 292, 113347. 10.1016/j.psychres.2020.113347 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cordes, A. , Herrmann‐Lingen, C. , Büchner, B. , & Hessel, A. (2009). Psychometric properties of the ENRICHD Social Support Instrument (ESSI, German version) in a representative German population sample. Klinische Diagnostik und Evaluation, 2, 16–32. [Google Scholar]
- Cosco, T. D. , Hardy, R. , Howe, L. D. , & Richards, M. (2018). Early‐life adversity, later‐life mental health, and resilience resources: A longitudinal population‐based birth cohort analysis. International Psychogeriatrics, 31(9), 1249–1250. 10.1017/s1041610218001795 [DOI] [PubMed] [Google Scholar]
- Druss, B. G. (2020). Addressing the COVID‐19 pandemic in populations with serious mental illness. JAMA Psychiatry, 77(9), 891–892. 10.1001/jamapsychiatry.2020.0894 [DOI] [PubMed] [Google Scholar]
- Dutheil, F. , Mondillon, L. , & Navel, V. (2020). PTSD as the second tsunami of the SARS‐Cov‐2 pandemic. Psychological Medicine. Advance online publication. 10.1017/s0033291720001336 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans, S. E. , Steel, A. L. , & DiLillo, D. (2013). Child maltreatment severity and adult trauma symptoms: Does perceived social support play a buffering role? Child Abuse & Neglect, 37(11), 934–943. 10.1016/j.chiabu.2013.03.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Faul, F. , Erdfelder, E. , Lang, A.‐G. , & Buchner, A. (2007). G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behavior Research Methods, 39(2), 175–191. 10.3758/BF03193146 [DOI] [PubMed] [Google Scholar]
- Forte, G. , Favieri, F. , Tambelli, R. , & Casagrande, M. (2020). COVID‐19 pandemic in the Italian population: Validation of a post‐traumatic stress disorder questionnaire and prevalence of PTSD symptomatology. International Journal of Environmental Research and Public Health, 17(11), 4151. 10.3390/ijerph17114151 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Franke, G. H. (2000). Brief Symptom Inventory von L. R. Derogatis (Kurzform der SCL‐90‐R) ‐ Deutsche Version. Manual [Brief Symptom Inventory by L. R. Derogatis (Short form of the SCL‐90‐R) – German version. Manual]. Beltz Test.
- Galea, S. , Merchant, R. M. , & Lurie, N. (2020). The mental health consequences of COVID‐19 and physical distancing: The need for prevention and early intervention. JAMA Internal Medicine, 180(6), 817–818. 10.1001/jamainternmed.2020.1562 [DOI] [PubMed] [Google Scholar]
- Gao, J. , Zheng, P. , Jia, Y. , Chen, H. , Mao, Y. , Chen, S. , Wang, Y. , Fu, H. , & Dai, J. (2020). Mental health problems and social media exposure during COVID‐19 outbreak. PLOS ONE, 15(4), e0231924. 10.1371/journal.pone.0231924 [DOI] [PMC free article] [PubMed] [Google Scholar]
- González‐Sanguino, C. , Ausín, B. , Castellanos, M. , Saiz, J. , López‐Gómez, A. , Ugidos, C. , & Muñoz, M. (2020). Mental health consequences during the initial stage of the 2020 coronavirus pandemic (COVID‐19) in Spain. Brain, Behavior, and Immunity, 87, 172–176. 10.1016/j.bbi.2020.05.040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hammen, C. , Henry, R. , & Daley, S. E. (2000). Depression and sensitization to stressors among young women as a function of childhood adversity. Journal of Consulting and Clinical Psychology, 68(5), 782–787. 10.1037//0022-006X.68.5.782 [DOI] [PubMed] [Google Scholar]
- Hawryluck, L. , Gold, W. L. , Robinson, S. , Pogorski, S. , Galea, S. , & Styra, R. (2004). SARS control and psychological effects of quarantine, Toronto, Canada. Emerging Infectious Diseases, 10(7), 1206–1212. 10.3201/eid1007.030703 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes, A. F. (2018). Introduction to mediation, moderation, and conditional process analysis: A regression‐based approach. (2nd ed.). Guilford Press. [Google Scholar]
- Heim, C. M. , Entringer, S. , & Buss, C. (2019). Translating basic research knowledge on the biological embedding of early‐life stress into novel approaches for the developmental programming of lifelong health. Psychoneuroendocrinology, 105, 123–137. 10.1016/j.psyneuen.2018.12.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holmes, E. A. , O'Connor, R. C. , Perry, V. H. , Tracey, I. , Wessely, S. , Arseneault, L. , Ballard, C. , Christensen, H. , Cohen Silver, R. , Everall, I. , Ford, T. , John, A. , Kabir, T. , King, K. , Madan, I. , Michie, S. , Przybylski, A. K. , Shafran, R. , Sweeney, A. , … Bullmore, E. (2020). Multidisciplinary research priorities for the COVID‐19 pandemic: A call for action for mental health science. The Lancet Psychiatry, 7(6), 547–560. 10.1016/S2215-0366(20)30168-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iob, E. , Frank, P. , Steptoe, A. , & Fancourt, D. (2020). Levels of severity of depressive symptoms among at‐risk groups in the UK during the COVID‐19 pandemic. JAMA Network Open, 3(10), e2026064. 10.1001/jamanetworkopen.2020.26064 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim, A. W. , Nyengerai, T. , & Mendenhall, E. (2020). Evaluating the mental health impacts of the COVID‐19 pandemic: Perceived risk of COVID‐19 infection and childhood trauma predict adult depressive symptoms in urban South Africa. Psychological Medicine. Advance online publication. 10.1017/s0033291720003414 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirk, R. E. (1996). Practical significance: A concept whose time has come. Educational and Psychological Measurement, 56(5), 746–759. 10.1177/0013164496056005002 [DOI] [Google Scholar]
- Klinitzke, G. , Romppel, M. , Häuser, W. , Brähler, E. , & Glaesmer, H. (2012). The German version of the Childhood Trauma Questionnaire (CTQ): Psychometric characteristics in a representative sample of the general population. Psychotherapie, Psychosomatik, Medizinische Psychologie, 62(2), 47–51. 10.1055/s-0031-1295495 [DOI] [PubMed] [Google Scholar]
- Krüger‐Gottschalk, A. , Knaevelsrud, C. , Rau, H. , Dyer, A. , Schäfer, I. , Schellong, J. , & Ehring, T. (2017). The German version of the Posttraumatic Stress Disorder Checklist for DSM‐5 (PCL‐5): Psychometric properties and diagnostic utility. BMC Psychiatry, 17(1), 379. 10.1186/s12888-017-1541-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lahav, Y. (2020). Psychological distress related to COVID‐19—The contribution of continuous traumatic stress. Journal of Affective Disorders, 277, 129–137. 10.1016/j.jad.2020.07.141 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu, C. H. , Zhang, E. , Wong, G. T. F. , Hyun, S. , & Hahm, H. C. (2020). Factors associated with depression, anxiety, and PTSD symptomatology during the COVID‐19 pandemic: Clinical implications for U.S. young adult mental health. Psychiatry Research, 290, 113172. 10.1016/j.psychres.2020.113172 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marroquín, B. , Vine, V. , & Morgan, R. (2020). Mental health during the COVID‐19 pandemic: Effects of stay‐at‐home policies, social distancing behavior, and social resources. Psychiatry Research, 293, 113419. 10.1016/j.psychres.2020.113419 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLaughlin, K. A. , Colich, N. L. , Rodman, A. M. , & Weissman, D. G. (2020). Mechanisms linking childhood trauma exposure and psychopathology: A transdiagnostic model of risk and resilience. BMC Medicine, 18(1), 96. 10.1186/s12916-020-01561-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLaughlin, K. A. , Conron, K. J. , Koenen, K. C. , & Gilman, S. E. (2010). Childhood adversity, adult stressful life events, and risk of past‐year psychiatric disorder: A test of the stress sensitization hypothesis in a population‐based sample of adults. Psychological Medicine, 40(10), 1647–1658. 10.1017/s0033291709992121 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nelson, S. , Baldwin, N. , & Taylor, J. (2012). Mental health problems and medically unexplained physical symptoms in adult survivors of childhood sexual abuse: An integrative literature review. Journal of Psychiatric and Mental Health Nursing, 19(3), 211–220. 10.1111/j.1365-2850.2011.01772.x [DOI] [PubMed] [Google Scholar]
- Robert Koch Institute . (2020a). Coronavirus disease 2019 (COVID‐19). Daily situation report of the Robert Koch Institute, 16/04/2020 . https://www.rki.de/DE/Content/InfAZ/N/Neuartiges_Coronavirus/Situationsberichte/2020-04-16-en.pdf?__blob=publicationFile
- Robert Koch Institute . (2020b). Coronavirus disease 2019 (COVID‐19). Daily situation report of the Robert Koch Institute, 17/03/2020 . https://www.rki.de/DE/Content/InfAZ/N/Neuartiges_Coronavirus/Situationsberichte/2020-03-17-en.pdf?__blob=publicationFile
- Salari, N. , Hosseinian‐Far, A. , Jalali, R. , Vaisi‐Raygani, A. , Rasoulpoor, S. , Mohammadi, M. , Rasoulpoor, S. , & Khaledi‐Paveh, B. (2020). Prevalence of stress, anxiety, depression among the general population during the COVID‐19 pandemic: A systematic review and meta‐analysis. Globalization and Health, 16(1), 57. 10.1186/s12992-020-00589-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schulte‐van Maaren, Y. W. , Carlier, I. V. , Zitman, F. G. , van Hemert, A. M. , de Waal, M. W. , van Noorden, M. S. , & Giltay, E. J. (2012). Reference values for generic instruments used in routine outcome monitoring: The Leiden Routine Outcome Monitoring Study. BMC Psychiatry, 12, 203. 10.1186/1471-244x-12-203 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schumacher, E. (2020). Merkel cautiously optimistic as she announces lockdown rollback. Deutsche Welle. https://www.dw.com/en/merkel-cautiously-optimistic-as-she-announces-lockdown-rollback/a-53346427 [Google Scholar]
- Scott, K. M. , Smith, D. R. , & Ellis, P. M. (2010). Prospectively ascertained child maltreatment and its association with DSM‐IV mental disorders in young adults. Archives of General Psychiatry, 67(7), 712–719. 10.1001/archgenpsychiatry.2010.71 [DOI] [PubMed] [Google Scholar]
- Shevlin, M. , McElroy, E. , & Murphy, J. (2015). Loneliness mediates the relationship between childhood trauma and adult psychopathology: Evidence from the Adult Psychiatric Morbidity Survey. Social Psychiatry and Psychiatric Epidemiology, 50(4), 591–601. 10.1007/s00127-014-0951-8 [DOI] [PubMed] [Google Scholar]
- Thorgaard, M. V. , Frostholm, L. , & Rask, C. U. (2018). Childhood and family factors in the development of health anxiety: A systematic review. Children's Health Care , 47(2), 198–238. 10.1080/02739615.2017.1318390 [DOI] [Google Scholar]
- Tsur, N. , & Abu‐Raiya, H. (2020). COVID‐19‐related fear and stress among individuals who experienced child abuse: The mediating effect of complex posttraumatic stress disorder. Child Abuse & Neglect. Advance online publication. 10.1016/j.chiabu.2020.104694 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vindegaard, N. , & Benros, M. E. (2020). COVID‐19 pandemic and mental health consequences: Systematic review of the current evidence. Brain, Behavior, and Immunity. Advance online publication. 10.1016/j.bbi.2020.05.048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vranceanu, A. M. , Hobfoll, S. E. , & Johnson, R. J. (2007). Child multi‐type maltreatment and associated depression and PTSD symptoms: The role of social support and stress. Child Abuse & Neglect, 31(1), 71–84. 10.1016/j.chiabu.2006.04.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walker, E. A. , Gelfand, A. , Katon, W. J. , Koss, M. P. , Von Korff, M. , Bernstein, D. , & Russo, J. (1999). Adult health status of women with histories of childhood abuse and neglect. The American Journal of Medicine, 107(4), 332–339. 10.1016/S0002-9343(99)00235-1 [DOI] [PubMed] [Google Scholar]
- Yu, H. , Li, M. , Li, Z. , Xiang, W. , Yuan, Y. , Liu, Y. , Li, Z. , & Xiong, Z. (2020). Coping style, social support, and psychological distress in the general Chinese population in the early stages of the COVID‐19 epidemic. BMC Psychiatry, 20(1), 426. 10.1186/s12888-020-02826-3 [DOI] [PMC free article] [PubMed] [Google Scholar]


