Abstract
Aim
This research study focused on exploring the impact of resilience on COVID‐19 phobia (C19P) among individuals from different nations including a cluster of European countries, India, Indonesia, Pakistan and the United States of America (USA).
Method
We recruited research participants via disseminating an electronic survey on Facebook Messenger (FM) that included 812 participants. The electronic survey assessed unidentifiable demographic information, the COVID‐19 Phobia Scale (C19P‐S; Arpaci et al., 2020) and the Brief Resilience Scale (BRS; Smith et al, 2008).
Results
Based on simple linear regression, resilience had a statistically significant negative affect on all four C19P factors including psychological, psychosomatic, economic and social factors (p < .001). Resilience showed a statistically significant difference for at least two nations (p < .001) investigated in this research, as shown by using the Kruskal–Wallis test. Utilising linear regression analysis showed that age affects the resilience score positively significantly (p < .001). Based on the Kruskal–Wallis test, we found no statistically significant differences in resilience scores between genders, but found statistically significant differences in resilience scores based on marital status, educational level and professional status (p = .001).
Conclusion
We concluded that the higher the resilience level, the lower the level of C19P. The level of resilience was highest in the USA, followed by Europe, Pakistan, India and Indonesia. Age affected the resilience level positively and resilience differed based on marital status, education levels, and professional status but not between genders. Implications are offered for effective counselling interventions during this COVID‐19 pandemic and the aftermath.
Keywords: COVID‐19 phobia, resilience, nations, mental health, counseling/counselling
1. INTRODUCTION
The coronavirus (COVID‐19) pandemic has led the world to face an unprecedented health challenge as evidenced by more than 72,824,936 confirmed cases and global deaths of 1,620,490, as of 14 December 2020 (Johns Hopkins University, 2020). The COVID‐19 pandemic exerts widespread and severe effects on people's daily life and presents a combination of stressors without a certain end date and blocks access to protective factors (Gruber et al., 2020). The full impact of this health crisis on individuals and diverse populations is unknown. During this stressful time, many individuals are challenged to adapt to a new reality overshadowed by fear of contagion. The perceived lack of control and the absence of a vaccine leave many people with COVID‐19 phobia (C19P) and concerns about their future. Some individuals and communities may respond to this potential trauma with resilience (Zoellner et al., 2013), whereas others may be affected more negatively. Considering the prevalence of mental health issues, it is important to determine people's mental health during this pandemic to find potential protective measures. Gao et al. (2020) reported high prevalence of mental health problems in China in February 2020, including 21.3% of problems related to anxiety. Other studies concerning the coronavirus outbreak and related mental health problems indicate depressive symptoms, anxiety and sleep problems in diverse populations (Ahorsu et al., 2020; Chen et al., 2020; Huang & Zhao, 2020; Rajkumar, 2020). Munk et al. (2020) found a higher prevalence of mental health disorders such as anxiety, panic disorder and obsessive–compulsive disorder during this pandemic in Germany, with 50.6% reporting at least one mental disorder. The results also showed that resilience was associated with lower risks for any mental health disorder.
This worldwide pandemic has raised questions on how resilience has influenced the response to CI9P in various nations. The World Health Organization has provided general guidelines for resilience strategies after COVID‐19 was declared as a worldwide pandemic (WHO, 2020). To determine how individuals can sustain their mental health during this pandemic, resilience towards various factors of C19P should be considered. By understanding the impact of resilience on the psychological, psychosomatic, economic and social factors of C19P in different nations, counsellors can take actions to increase resilience levels by providing the most effective psychotherapy and professional counselling services for clients of diverse backgrounds. While some studies have highlighted a significant increase in mental health issues including insomnia, posttraumatic stress disorder and phobia (Kaba & Akin Sari, 2020) during this pandemic, there is a lack of studies on resilience towards C19P in different nations. To allow mental health providers to respond effectively, it is crucial for them to have detailed information on how resilience impacts the level of C19P in diverse clients.
1.1. COVID‐19 phobia
According to Abrams et al. (2020), COVID‐19 is caused by the pathogen severe acute respiratory syndrome (SARS) coronavirus 2. The response of individuals varies from denial to being frightened of becoming infected with the virus. Some of the most discussed mental health issues related to this pandemic include cognitive change, avoidance and compulsive behaviour, loss of social functioning (Qiu et al., 2020); patterns of compulsive thinking (Lee, 2020); acute stress, panic disorder, generalised anxiety disorder, specific phobia, posttraumatic stress disorder, lack of concentration, and sleeping issues (Kaba & Akin Sari, 2020); relapse of depressive disorders (Mehra et al., 2020); paranoia and nihilistic delusions (Brooks et al., 2020); and possible prevalence of schizophrenia in subsequent years (Zandifar & Badrfam, 2020). The uncertainty of when a vaccine might be available and the feeling of not being in control (Henry, 2020), loneliness due to isolation (Mehra et al., 2020), and apprehension about the future (Hiremath et al., 2020) might also be related to C19P.
Research has also found that the phobia of COVID‐19 is prevalent among children, adolescents, adults, elderly people, people with pre‐existing mental health conditions, and medical and frontline workers (Kaba & Akin Sari, 2020; Lu et al., 2020; Mehra et al., 2020). For instance, lack of information on COVID‐19 and acquiring wrong information from their peers are associated with the onset of panic and phobia among children (Kaba & Akin Sari, 2020). People with pre‐existing mental health conditions are more prone to experience re‐occurrence of their previous illness due to their heightened susceptibility to stress caused by COVID‐19 as compared to healthy individuals (Kaba & Akin Sari, 2020). Elderly patients are also susceptible to mental health issues such as relapse of depressive disorder, which was found to be particularly associated with fear of contracting COVID‐19 and fear of loneliness during the outbreak (Mehra et al., 2020). Other extremely vulnerable populations including medical staff and other frontline workers, such as nurses, showed higher scores on a fear scale as compared to non‐clinical staff (Lu et al., 2020). Frontline workers were found to be twice as likely to suffer anxiety and depression, and 1.4 times more likely to feel fear as compared to administrative or non‐clinical staff (Lu et al., 2020). Therefore, individuals from different demographic backgrounds might show varied resilience levels towards CP19.
1.2. Resilience
Resilience is the ability to maintain healthy levels of functioning despite difficult experiences or returning to normal functioning after experiences of adversity (Constanzo et al., 2009). High levels of resilience are characterised by being optimistic, acting positively, and representing self‐assurance when experiencing difficult life situations, which is linked to better physical and mental health and well‐being (Connor & Davidson, 2003). People with high resilience levels who experience serious threats and crisis have a positive mental health outcome (Rutter, 2006) and are described as being more flexible and more adaptive when responding to crisis. In the face of this pandemic, people across the world need to deal with continuing stressors to sustain their mental health.
Several studies have reported that resilience can be a protective factor in reducing risk of suicide (Nrugham et al., 2010; Roy et al., 2011) and have shown a negative correlation between resilience and mental health problems (Peng et al., 2012). Tumlu (2013) found differences in resilience levels based on gender and concluded that women were found to be less positively resilient compared to men. He also indicated higher levels of resilience in students who were raised with a democratic maternal attitude compared to students raised with a protective maternal attitude. Spirituality and religion were also found to impact resilience positively as they helped to buffer risk for specific mental health problems and fostered psychosocial characteristics in U.S. veterans (Sharma et al., 2017). While researchers across the world are focusing on finding strategies to end the spread of the virus, we must consider the heterogeneity of this disease in different nations and understand resilience for clinically effective therapeutic applications (Sominsky et al., 2020).
1.3. Purpose of the present study
The purpose of this study was to determine the level of resilience towards C19P in various nations including the United States of America (USA), India, Indonesia, Pakistan and European countries. We focused on analysing demographic data (age, marital status, country of birth, country of residence, ethnicity, race, educational level and professional status) and the variables including factors of C19P and the construct of resilience. We aimed to determine how resilience influences the psychological, psychosomatic, economic and social factors of C19P among the populations in different nations.
1.4. Research questions
RQ1. Does resilience affect the level of C19P?
RQ2. Are there differences in resilience levels towards C19P among different nations?
RQ3. Do demographic data correlate to resilience?
2. METHOD
2.1. Ethical consideration
The proposal of the present study was submitted to the Institutional Review Board (IRB) of the University of Providence for approval. All the potential research participants were asked to read and accept the informed consent prior to their participation. The research procedures followed the ethical guidelines for research in accordance with the American Counseling Association (2014).
2.2. Sample procedures
First, we created an electronic survey on Google Forms and shared the electronic survey with our Facebook Messenger (FM) friends on our respective FMs, along with brief information about the study. As a second step, we selected 5–10 respective FM friends and requested them to forward the survey link to 5–10 individuals who were not FM friends with us. We also instructed them to request their FM friends not to forward it further to ensure stopping the chain.
Next, we followed up with our FM friends whom we requested to forward the web‐link of the survey to count the number of people who received it. We documented the total number of recipients to calculate the response rate. The rationale for using this sampling plan was to collect responses from a broad range of populations in different countries rather than from a specific population that is narrowed down based on criteria such as age, education level, profession or mental health status.
When respondents clicked the provided web‐link, they were able to access the consent form, instructions to complete the survey, a demographic questionnaire, a questionnaire on C19P, and a questionnaire on resilience. Respondents were informed that the time commitment for the survey was approximately 15–20 min. Respondents were also informed that participation was completely voluntary, and they could withdraw at any time without any penalty, and the data collected would remain anonymous.
2.3. Sample
We used FM to invite 1,267 of our respective FM friends from different countries who are fluent in English to participate in the study. Out of these 1,267 individuals, 902 decided to participate and responded to the online survey, which resulted in a calculated 71% response rate. Respondents who did not agree with the informed consent were unable to fill out the online survey and have been removed, which led to 887 participants. Missing data, incomplete answers and the elimination of a few participants who fell outside of a group of 30 individuals of a country led to the further elimination of 75 participants (N = 812). All countries under the cluster of European countries are Western European countries (Austria, Belgium, France, Germany, Ireland, Italy, the Netherlands, Spain, United Kingdom). We decided to combine them because English is not the first language in most European countries, and thus, the numbers of participants in each country were much lower than other countries in the study. Our sample consisted of 812 participants in European countries, Indonesia, India, Pakistan and USA (see Table 1). All study protocols were approved by the Institutional Review Board (IRB) at the University of Providence (002‐UPIRB‐2020).
TABLE 1.
Socio‐demographic characteristics of participants (N = 812)
| Baseline characteristics | Pakistan | Europe | India | Indonesia | USA | Full sample | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | n | % | n | % | |
| Gender | ||||||||||||
| Male | 6 | 15.79 | 22 | 25 | 168 | 42.42 | 58 | 31.52 | 38 | 35.85 | 292 | 35.96 |
| Female | 32 | 84.21 | 66 | 75 | 228 | 57.58 | 126 | 68.48 | 68 | 64.15 | 520 | 64.04 |
| Professional status | ||||||||||||
| Disabled—NOT working | 0 | 0.00 | 1 | 1.14 | 0 | 0.00 | 2 | 1.09 | 0 | 0.00 | 3 | 0.37 |
| Employed—Full time | 19 | 50.00 | 41 | 46.59 | 245 | 61.87 | 21 | 11.41 | 0 | 0.00 | 326 | 40.15 |
| Employed—Part time | 7 | 18.42 | 30 | 34.09 | 38 | 9.60 | 8 | 4.35 | 75 | 70.75 | 158 | 19.46 |
| Unemployed—Looking | 5 | 13.16 | 2 | 2.27 | 36 | 9.09 | 13 | 7.07 | 7 | 6.60 | 63 | 7.76 |
| Unemployed—Not looking | 1 | 2.63 | 3 | 3.41 | 14 | 3.54 | 16 | 8.70 | 5 | 4.72 | 39 | 4.80 |
| Retired | 0 | 0.00 | 4 | 4.55 | 16 | 4.04 | 0 | 0.00 | 1 | 0.94 | 21 | 2.59 |
| Student | 6 | 15.79 | 7 | 7.95 | 47 | 11.87 | 124 | 67.39 | 10 | 9.43 | 194 | 23.89 |
| Marital status | ||||||||||||
| Divorced | 0 | 0.00 | 5 | 5.68 | 5 | 1.26 | 1 | 0.54 | 15 | 14.15 | 26 | 3.20 |
| Married | 4 | 10.53 | 45 | 51.14 | 234 | 59.09 | 13 | 7.07 | 63 | 59.43 | 359 | 44.21 |
| Never Married | 34 | 89.47 | 33 | 37.50 | 142 | 35.86 | 166 | 90.22 | 23 | 21.70 | 398 | 49.01 |
| Separated | 0 | 0.00 | 3 | 3.41 | 7 | 1.77 | 2 | 1.09 | 0 | 0.00 | 12 | 1.48 |
| Widowed | 0 | 0.00 | 2 | 2.27 | 8 | 2.02 | 2 | 1.09 | 5 | 4.72 | 17 | 2.09 |
| Education | ||||||||||||
| Associate degree | 0 | 0.00 | 4 | 4.55 | 0 | 0.00 | 5 | 2.72 | 6 | 5.66 | 15 | 1.85 |
| Bachelor's degree | 7 | 18.42 | 23 | 26.14 | 61 | 15.40 | 69 | 37.50 | 16 | 15.09 | 176 | 21.67 |
| Incomplete high school | 1 | 2.63 | 2 | 2.27 | 0 | 0.00 | 0 | 0.00 | 0 | 0.00 | 3 | 0.37 |
| Doctoral degree | 2 | 5.26 | 8 | 9.09 | 89 | 22.47 | 6 | 3.26 | 17 | 16.04 | 122 | 15.02 |
| High School degree/GED | 0 | 0.00 | 6 | 6.82 | 3 | 0.76 | 61 | 33.15 | 4 | 3.77 | 74 | 9.11 |
| Master's degree | 13 | 34.21 | 35 | 39.77 | 117 | 29.55 | 7 | 3.80 | 50 | 47.17 | 222 | 27.34 |
| Professional degree | 15 | 39.47 | 8 | 9.09 | 124 | 31.31 | 0 | 0.00 | 5 | 4.72 | 152 | 18.72 |
| Some college—No degree | 0 | 0.00 | 2 | 2.27 | 2 | 0.51 | 36 | 19.57 | 8 | 7.55 | 48 | 5.91 |
| Age group | ||||||||||||
| 18 ≤ age < 25 | 11 | 28.95 | 6 | 6.82 | 40 | 10.10 | 166 | 90.22 | 7 | 6.60 | 230 | 28.33 |
| 25 ≤ age < 35 | 24 | 63.16 | 28 | 31.82 | 194 | 48.99 | 5 | 2.72 | 46 | 43.40 | 297 | 36.58 |
| 35 ≤ age < 45 | 3 | 7.89 | 27 | 30.68 | 100 | 25.25 | 1 | 0.54 | 21 | 19.81 | 152 | 18.72 |
| 45 ≤ age < 55 | 0 | 0.00 | 13 | 14.77 | 36 | 9.09 | 8 | 4.35 | 19 | 17.92 | 76 | 9.36 |
| 55 ≤ age < 65 | 0 | 0.00 | 12 | 13.64 | 17 | 4.29 | 2 | 1.09 | 5 | 4.72 | 36 | 4.43 |
| Age ≥ 65 | 0 | 0.00 | 2 | 2.27 | 9 | 2.27 | 2 | 1.09 | 8 | 7.55 | 21 | 2.59 |
| Total | 38 | 100 | 88 | 100 | 396 | 100 | 184 | 100 | 106 | 100 | 812 | 100 |
2.4. Instruments
2.4.1. Demographic Questionnaire
Demographic information regarding participants' age, gender identity, marital status, country of birth, country of residence, ethnicity, race, level of education and professional status was collected for descriptive and inferential statistics. To maintain participants' confidentiality, no identifiable information was collected.
2.4.2. COVID‐19 Phobia Scale
The COVID‐19 Phobia Scale (C19P‐S) was developed by Arpaci et al. (2020), and assesses the level of phobia towards COVID‐19. This questionnaire consists of 20 items that are rated on a 5‐point Likert‐type scale ranging from 1 = strongly disagree to 5 = strongly agree.
The C19P‐S consists of four factors: psychological, psychosomatic, economic and social. Examples of items on the C19P‐S include: ‘The fear of coming down with coronavirus makes me very anxious’, ‘I experience sleep problems out of the fear of coronavirus’, ‘I stock food with the fear of coronavirus’, and ‘I am unable to curb my anxiety of catching coronavirus from others’. Participants were asked to respond with their level of agreement on the Likert scale.
Arpaci et al. (2020) found good internal consistency for the C19P‐S with a Cronbach's alpha coefficient of the 20 items of 0.925 and subscale reliabilities ranging from 0.851 to 0.903; strong levels of convergent, construct and discriminant validity were also found.
We found good internal consistency with a Cronbach's alpha coefficient of 0.93 for the overall C19P‐S (p < .001) in the current study. The four subscales showed a Cronbach's alpha coefficient of 0.87 for psychological factors (ranging from 0.83–0.89 for six items), a Cronbach's alpha coefficient of 0.86 for the psychosomatic factors (ranging from 0.81–0.86 for five items), a Cronbach's alpha coefficient of 0.82 for the economic factors (ranging from 0.75–0.82 for four items), and a Cronbach's alpha coefficient of 0.87 for the social factors (ranging from 0.82–0.84 for five items) in the present research. We conducted Spearman's rank method to analyse the item validity of the C19P‐S. The results indicated good validity, evidenced by all Spearman's correlations (0.54‐0.85, 0.68‐0.85, 0.75‐0.85, 0.78‐0.85) being p < .001.
2.4.3. Brief Resilience Scale
The Brief Resilience Scale (BRS; Smith et al., 2008) is a 6‐item self‐report questionnaire, which uses a 5‐point Likert‐type scale, ranging from 1 = strongly disagree to 5 = strongly agree. Participants were asked to choose one of these options while answering the questions. Examples of items on the BRS scale include: ‘It does not take me long to recover from a stressful event’, and ‘I tend to take a long time to get over set‐backs in my life’. The calculation was done by taking an average of scores for all 6 items, where items 2, 4 and 6 are reversed scores. For example, if a participant scored a ‘6’, he/she was given a ‘2’. Research has found strong theoretical construct validity as well as internal consistency with Cronbach's alpha coefficients ranging from 0.80 to 0.91, as well as good test–retest reliability, convergent validity and divergent validity of the BRS (Agnes, 2005; Ahern et al., 2006; Smith et al., 2008). Other studies have shown internal consistency of the BRS with Cronbach's alpha coefficients of 0.71 (Fung, 2020) and 0.78 (Soer et al., 2019). The BRS offers a summary score of characteristics that support positive adaptation, as well as increase the possibility of resilience. Moreover, the BRS supports the notion that assessing people's ability to recover is more pertinent than assessing their ability to resist illness, especially when they are already mentally or physically ill (Smith et al., 2008).
The present study found a Cronbach's alpha coefficient of 0.65 for the BRS and subscale reliabilities ranging from 0.55 to 0.68. Although a value higher than 0.70 would be ideal, a value of internal consistency close to 0.60 is satisfactory (Souza et al., 2017). The value of the Cronbach's alpha coefficient is influenced by the number of items, and thus, the fact that the BRS has only six items may have reduced the internal consistency. Furthermore, the item validity test was carried out using Spearman's rank method. The results showed that all Spearman's correlations have p‐values smaller than 2.2 × 10−16, p < .05, which confirms valid items.
2.5. Design
Our study is cross sectional and includes an electronic survey with unidentifiable demographic information, the C19P‐S (Arpaci et al., 2020) and the BRS (Smith et al., 2008). The study was designed to collect data from individuals residing in different nations to investigate the impact of resilience on C19P. First, a descriptive analysis of variables was performed. The inferential statistics are provided based on the nature of categorical and numerical variables and the research questions. The correlations between variables and predictive analysis are based on regression models and are presented as means, medians and deviations.
2.6. Statistical analysis
We used the R software (R‐4.0.3 for Windows, 2020) to analyse the data. R is widely used by statisticians and data miners for creating or developing statistical and data analysis tools and software. R was developed by Ihaka and Gentleman (1997) and is primarily used for statistical computing as well as for graphics. We reviewed the data of participants who had responded to the online survey and eliminated missing data, which led to a sample of 812 participants (see Table 1). Individuals from Europe (n = 88), India (n = 396), Indonesia (n = 184), Pakistan (n = 38) and USA (n = 106) were included. We cleaned the data set of 812 participants by recoding the Likert scale into a numbering of the responses to the C19P‐S and the BRS. We did not use the total score of the C19P‐S, which is in the range between 20 and 100, but the total scores of the four factors: psychological (range between 6 and 30), psychosomatic (range between 5 and 25), economic (range between 4 and 20) and social (range between 5 and 25). The BRS also needed the scores of items 2, 4 and 6 to be reverted.
We screened the data for normality= in various ways to determine the statistical methods for answering our research questions, for example, analysis of variance (ANOVA; with the objective to compare if different groups of observations have the same mean). If the normality assumption is not met, or if the distribution of data is not known, non‐parametric methods can be used to analyse the data. First, we looked at intervals and frequencies, and created histograms for all five nations (see Figure A3), identifying the distribution of the data set, spread and skewness as well as whether a data set is unimodal, bimodal or multimodal and has outliers or gaps. The histograms showed that the distribution of resilience scores in Europe was bimodal and almost symmetric, India was unimodal and not symmetric, Indonesia was unimodal and almost symmetrical, and Pakistan and USA scores were not symmetric.
To confirm the correctness of normality hypothesis testing, a normality test is required. As the resilience score is a sum of item scores (range of this score is 6 to 30), it is not a continuous variable but an interval variable. Based on Conover (1999), the Shapiro–Wilk normality test was used for interval‐type data. At the conclusion of the normality test, resilience scores of Europe and Pakistan were normally distributed, while resilience scores of India, Indonesia and USA did not meet the normality assumption (p < .001). Based on the finding that not all five nations showed a normal distribution, we used the non‐parametric Kruskal–Wallis test instead of analysis of variance (ANOVA) (Walpole & Myers, 2012). We performed our statistical analysis via the Kruskal–Wallis test and linear regression. The Kruskal–Wallis test is used to compare means (or medians) of more than two populations, and linear regression is used to analyse the relationship between one dependent variable and one or more independent variable(s). Through linear regression, the relationship between an independent variable and a dependent variable can be analysed. Like most non‐parametric tests, Kruskal–Wallis is performed on the ranks of the measurement observations (Fagerland & Sandvik, 2009; Van Hecke, 2012). The linear regression analysis needs the normality assumption to be met for error, so resilience (dependent variable) should be normally distributed. However, the linear regression is robust if the normality violation is not severe, and thus, we used linear regression to answer RQ1.
3. RESULTS
3.1. Descriptive statistics
Based on the demographic questionnaire, the variables included are age, gender, marital status, country of birth, country of residence, ethnicity, race, educational level and professional status. The demographic variables of participants (N = 812) are summarised in Table 1. The ages of respondents were distributed from 18 to 71 years old (Mean = 32.75, Median = 31).
3.2. Research questions
3.2.1. RQ1: Does resilience affect the level of C19P?
This question investigated whether resilience affects the level of C19P or not. Although the dependent variable resilience did not meet the normality assumption, the violation was not severe. Therefore, we utilised linear regression to explore whether resilience affects the level of C19P significantly. Four simple linear regression models were used to determine the effect of resilience on the four C19P scales: psychological, psychosomatic, economic and social factors. The results of simple linear regression models for all four C19P factors are shown in Table 2.
TABLE 2.
Results of simple linear regression: Effects of resilience on the C19P factors (Psychological, psychosomatic, economic and social factors)
| Independent variable (X) | Dependent variable (Y) | |||
|---|---|---|---|---|
| Psychological factors | Psychosomatic factors | Economic factors | Social factors | |
| Estimate | Estimate | Estimate | Estimate | |
| Intercept | 27.7633** | 13.60539** | 14.41584** | 21.60742** |
| Resilience | −0.438** | −0.28116** | −0.27997** | −0.34926** |
p < .001.
As represented in Table 2, resilience statistically significantly affects all four C19P factors with a negative relationship. The resilience estimate coefficient (or parameter) for the psychological factors model is −0.438 with p < 2 × 10‐16, p < .001, indicating that for each increased score of resilience, there is a decreased score of the psychological factor by as much as 0.438. The resilience estimate coefficient for the psychosomatic factors model is −0.281, showing p < 2 × 10−16, p < .001, which indicates that for each increased score of resilience, there is a decreased score of the psychosomatic factor by as much as 0.281. Similar interpretations can be applied to the resilience estimate coefficient of economic and social models. In conclusion, resilience was found to affect the level of C19P negatively, which means the higher the resilience scores, the lower the level of C19P.
3.2.2. RQ2: Are there differences in resilience levels towards C19P among different nations?
We compared the resilience levels in participants (N = 812) among the five nations, including a cluster of European countries, India, Indonesia, Pakistan and USA. As the level of resilience variable has not met the normality assumption, we utilised the Kruskal–Wallis method to answer this research question. The results are presented in Table 3.
TABLE 3.
Kruskal–Wallis test of the level of resilience based on different nations
| Variable by nations | Kruskal–Wallis chi‐square |
|---|---|
| Resilience by nation | 48.552** |
p < .001.
Results show that resilience is statistically significantly different for at least two nations investigated in this research, including a cluster of European countries, India, Indonesia, Pakistan and USA; t = 48.552, p = 7.241 × 10−10, p < .001. The differences in resilience levels among the five nations are represented in Figure A1 with boxplots in the appendix. Based on our data analysis, results showed that USA has the highest level of resilience with a median of 23, followed by Europe with a median of 21, Pakistan with a median of 21, India with a median of 20 and Indonesia with a median of 19.
3.2.3. RQ3: Do demographic data correlate to resilience?
Demographic data consisted of age, gender, marital status, education level and professional status, where age is a numerical variable, and the other four variables are categorical variables. The correlation between age and resilience was measured using Pearson's correlation. Based on the data computation, the correlation coefficient is r = .2078 (95% CI [.144, 0.270]) for age and resilience. The Coefficient of x, = 0.064 is statistically significant, with p = 5.17x10(−10), p < .001. This represents that age affects the resilience score, which means that for every one‐year increase in a respondent's age, the resilience score increases by 0.064.
To identify if gender affects resilience, a Kruskal–Wallis chi‐square test was used. Results show the test statistic t = 2.626, p = .105, p > .001, indicating there is no difference in resilience scores among males and females (there were no participants who identified themselves as other). The results for the other demographic variables can be seen in Table 4, with resilience by marital status, education and professional status all having a significance of p < .001. These results indicate that there is a difference in resilience scores based on marital status, education level and professional status. Figures A2.1, A2.2, A2.3, A2.4 (see A2.1, A2.2, A2.3, A2.4) in the appendix show boxplots of resilience score by each demographic variable.
TABLE 4.
Kruskal–Wallis test of the level of resilience based on demographic groups
| Variable by group | Kruskal–Wallis chi‐square |
|---|---|
| Resilience by gender | 2.6262 |
| Resilience by marital status | 26.157** |
| Resilience by education level | 30.65** |
| Resilience by professional status | 36.724** |
p < .001.
4. DISCUSSION
We addressed the impact of resilience on C19P in different nations as the global challenge of COVID‐19 is like an interconnecting tsunami. Our data sample for this study consisted of 812 participants (Table 1). We included individuals from Europe, India, Indonesia, Pakistan and USA.
RQ1. The current findings supported the hypothesis that the construct of resilience statistically significantly affects the level of C19P. The construct of resilience was measured with the BRS (Smith et al., 2008) by the summation of the six items. The results showed that resilience statistically significantly affects all four C19P factors with a negative correlation. This indicates that the higher the resilience factor, the lower the level of all four C19P factors (psychological, psychosomatic, economic and social). This finding is supported by previous research indicating that resilience can be a protective factor against mental health problems that are related to adverse experiences (Perlman et al., 2017). The conceptual study by Chen and Bonanno (2020) partially supports this hypothesis and suggests that the resilience factor of flexibility might be the most important factor in responding to the changing situational demands of COVID‐19. Table 2 provides detailed information on the negative correlations between resilience and C19P factors.
RQ2. To answer the research question ‘are there statistically significant differences in resilience levels among different nations?’, we tested whether the distribution of the construct of resilience met the normality assumption in the selected five nations (cluster of European countries, Indonesia, India, Pakistan, USA) with participants for group comparison. As the results showed that the data was not normally distributed, the Kruskal–Wallis test was applied. Our findings supported the hypothesis as they showed that resilience statistically significantly differs for each of the five nations. The highest level of resilience was found in the USA, followed by Europe, Pakistan, India and Indonesia. These results are represented in Figure A1 in the appendix. Galloway (2020) explored the economic resilience of different nations by comparing their Resilience Index data, which consisted of three core resilience factors including economic, risk quality and the supply chain. However, no study has been found to date that represents the difference in resilience levels of the general population towards C19P among different nations.
RQ3. The present study also investigated whether the demographic data correlate statistically significantly with resilience in participants among the different nations. We collected demographic data for age, gender, marital status, education level and professional status, where age was a numerical variable, and the other five variables were categorical variables. The correlation between age and resilience was tested by utilising Pearson's correlation. The results confirmed that there is a statistically significant positive correlation between age and the level of resilience, which means the higher the age of participants, the higher the level of resilience. After using a simple linear regression, the findings showed that age affects the resilience score. The data analysis with the Kruskal–Wallis test did not find a difference in resilience scores between females and males. However, there was a statistically significant difference in resilience scores based on participants' marital status, education level and professional status. The results of the Kruskal–Wallis test based on the demographic groups are represented in the results section (see Table 3). These findings are also represented in Figures A2.1, A2.2, A2.3, A2.4 (A2.1, A2.2, A2.3, A2.4) in the appendix.
5. LIMITATIONS OF THE STUDY
This study has several limitations that should be noted and addressed. One of the limitations was recruiting unequal numbers of participants from different nations, which led to an unequal distribution of the respondents (European countries = 88, India = 396, Indonesia = 184, Pakistan = 38, USA = 106). This may have limited the accuracy of determining comparisons, as well as correlations between unequal data sets among different nations. To overcome this limitation, we used a Kruskal–Wallis test instead of ANOVA for inferential statistics. Another limitation was including only English‐speaking individuals from different nations, which eliminated non‐English‐speaking people. Recruiting our friends from different nations as research participants via FM has limited the generalisation of the sample. This method might also have restricted the recruitment of a much broader range of the population and missed out the recruitment of participants from some nations completely. In addition, this recruitment method may have limited the number of responses due to their occasional or non‐usage of the FM app or non‐availability of the Internet. Moreover, the online survey relied on the participants' self‐reports, which might have elicited only a few aspects of resilience and missed other important ones.
5.1. Suggestions for future research
We offer several suggestions for future research to improve upon the methods and procedures utilised in this study, as well as to advance this research agenda. First, we encountered an issue regarding the unequal number of responses from different nations due to choosing the FM app to recruit research participants. Thus, it is recommended for future researchers to recruit research participants by other means, so that the number of responses from different nations do not differ greatly from each other. For example, inviting organisations or communities based on their number of residents in various nations may lead to more equal numbers of participants. Second, it is recommended to replicate the study with participants from non‐English‐speaking nations, to analyse if the results are consistent with the present study. Future research could also explore more details about the resilience factors in participants from various nations to promote specific strength‐based counselling methods that foster well‐being in clients.
6. IMPLICATIONS FOR PRACTICE
Surveying people from different demographic backgrounds regarding their phobia of COVID‐19 and level of resilience was a step to inquire about the possible need to foster resilience in people across the globe. Therefore, we provide implications for mental health providers dealing with C19P.
Some implications could be directed to mental health providers to help their clients and the public to increase their resilience in this pandemic. First, mental health providers are recommended to practice regular self‐care for their own resilience, so that they can help other people deal with C19P more effectively without getting burnout. In addition, mental health counsellors who work independently or with mental health agencies need to be flexible in offering online counselling services that are following the ethical codes of the American Counseling Association or other counselling organisations. Those who do not have any prior experience in offering online counselling services are recommended to receive necessary training and consult with their supervisors, mentors or colleagues regarding providing online counselling services in an ethical manner. Professional counsellors and mental health agencies should offer 24‐hr hotline services, where anyone can call in times of emotional or mental distress due to COVID‐19.
Professional counselling should focus on the strengths, self‐assurance, purpose of life, spirituality and gratitude of clients to increase resilience. Assisting clients to explore the opportunity that comes with a crisis can impact resilience positively. These counselling strategies should be applied culturally sensitively. Another recommendation for independent mental health counsellors and mental health agencies is to collaborate with primary care clinics, hospitals and other healthcare providers such as doctors, nurses, social workers, psychologists and psychiatrists to provide integrated care to the public for treating the whole person (McDaniel & deGruy, 2014).
CONFLICT OF INTEREST
We have no conflicts of interest to disclose:
Biographies
Sylvia Lindinger‐Sternart, Ph.D. is Associate Professor for the M.S. clinical mental health counseling program and has served as the program director (2016‐2019) at the University of Providence. She received her doctorate from the University of Toledo and served at Pennsylvania State University. She obtains a psychotherapy certificate from her native country Austria, is a licensed clinical mental health counselor in Montana and works with diverse populations across the globe on trauma and how to develop resiliency. She is certified in Eye Movement Desensitization and Reprocessing (EMDR) and has presented and published on mindfulness, resilience, trauma, addiction, suicide prevention, and online counseling services nationally and internationally.
Varinder Kaur, Ph.D., LPC is currently an Affiliate Professor of clinical mental health counseling at Northwestern University, IL. She holds a license of Professional Counselor (LPC) in the state of Michigan and is experienced in offering clinical counseling services to a variety of populations in different settings. She is also currently serving as a President of the Michigan Association of Counselor Education and Supervision (MACES). "Her research interests include wellness, mindfulness‐based approaches, addiction related issues, and professional identity of counselors.
Yekti Widyaningsih, Ph.D. is Associate Professor of mathematics and natural sciences at Universitas Indonesia and is a lecturer in statistics. She received her doctorate from Bogor Agricultural University, Indonesia. She received a grant for research at Pennsylvania State University in 2010 with Prof. G. P. Patil as her advisor and completed a postdoctoral fellowship at the same university in 2014. Her professional interest is statistics application including modeling, geoinformatics, and psychometrics.
Ashok Kumar Patel, M. Phil is a registered Clinical Psychologist in India. He received his Master of Philosophy in clinical psychology from Post Graduate Institute of Behavioral and Medical Sciences Raipur, India. Currently he is pursuing his Ph.D. in Clinical Psychology from Deen Dayal Upadhyay Gorakhpur University, Gorakhpur, India. His professional interests include OCD, anxiety, depression, schizophrenia, memory problems, psychosexual problems and child & adolescent mental health.
Appendix A.
Figure A1.
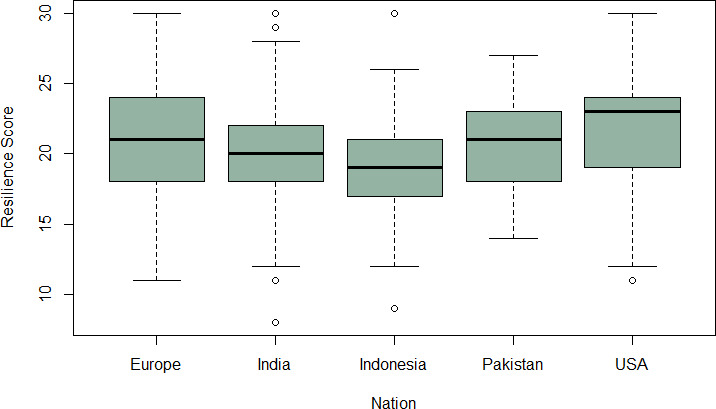
Boxplot of resilience scores of every nation (Europe Median = 21, India Median = 20, Indonesia Median = 19, Pakistan Median = 21, USA Median = 23)
Figure A2.1.
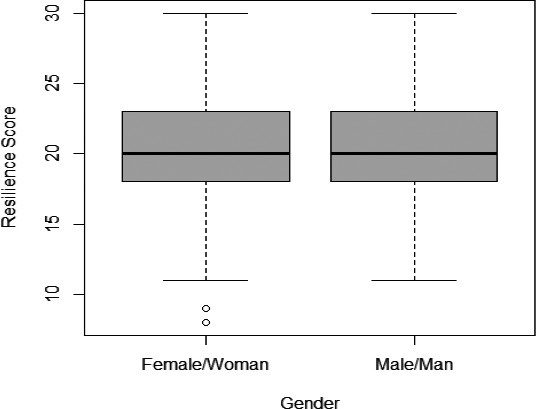
Boxplot of resilience scores based on gender (Females N = 520, Median = 20; Males N = 292, Median = 20)
Figure A2.2.
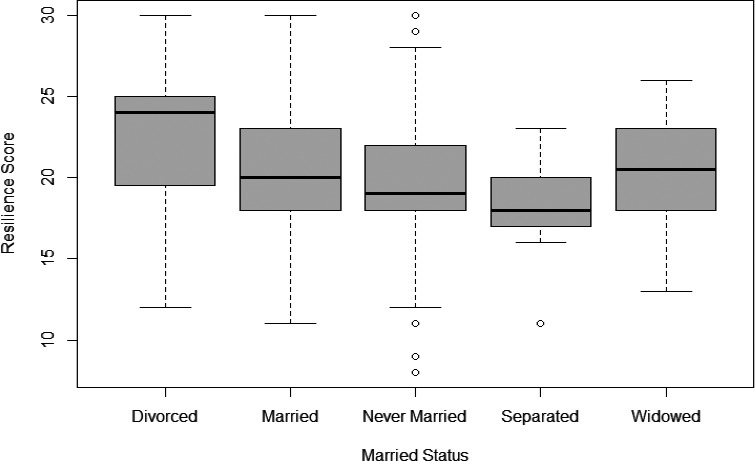
Boxplot of resilience scores based on marital status (Divorced Median = 24, Married Median = 20, Never Married Median = 20, Separated Median = 18, Widowed Median = 20)
Figure A2.3.
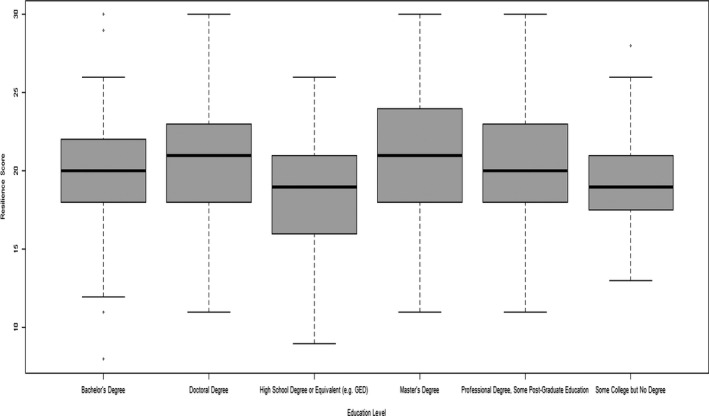
Boxplot of resilience scores based on educational level
Figure A2.4.
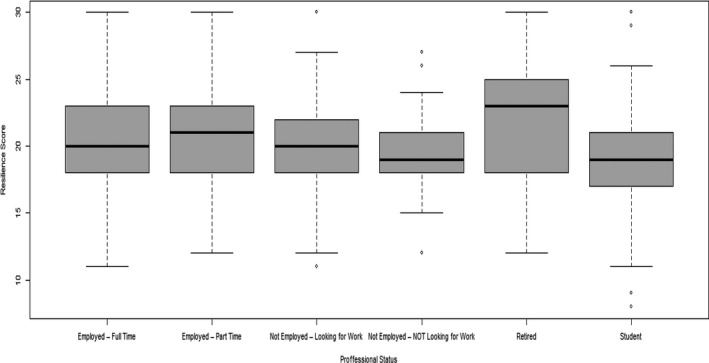
Boxplot of resilience scores based on professional status
Figure A3.
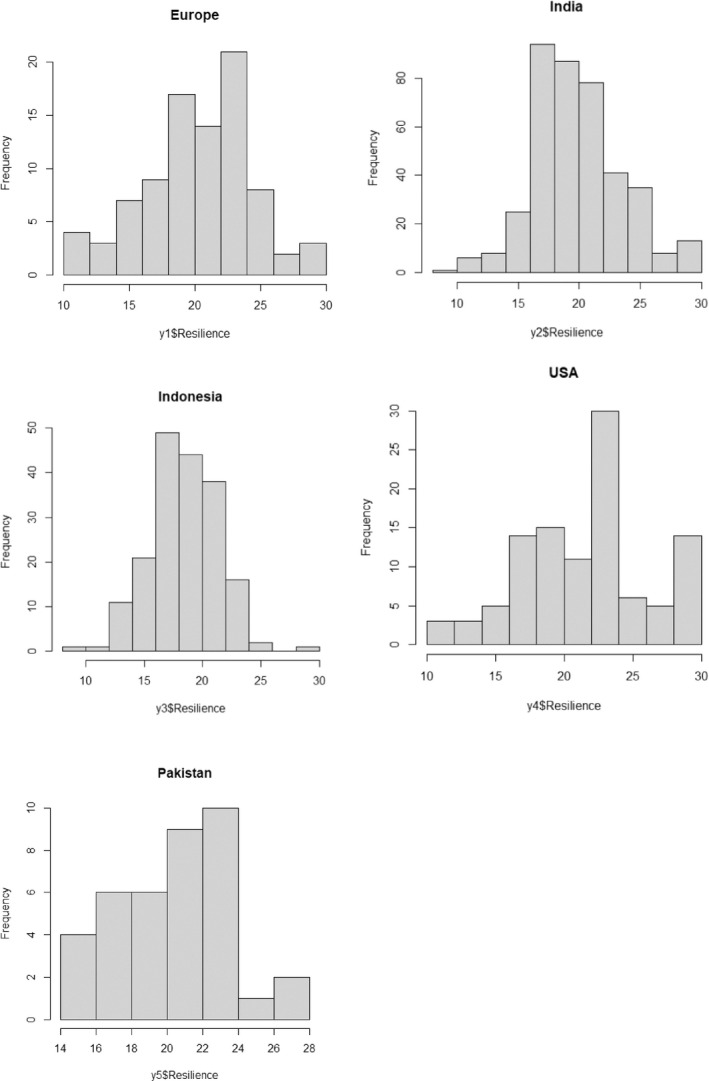
Bar charts of the distribution of resilience of every nation
Lindinger‐Sternart S, Kaur V, Widyaningsih Y, Patel AK. COVID‐19 phobia across the world: Impact of resilience on COVID‐19 phobia in different nations. Couns Psychother Res. 2021;21:290–302. 10.1002/capr.12387
Contributor Information
Sylvia Lindinger‐Sternart, Email: Sylvia.Lindingersternart@uprovidence.edu.
Varinder Kaur, Email: vkaur@family-institute.org.
Yekti Widyaningsih, Email: yekti@sci.ui.ac.id.
Ashok Kumar Patel, Email: ashok.patel95@gmail.com.
REFERENCES
- Abrams, E. M. , & Greenhawt, M. (2020). Risk communication during COVID‐19. American Academy of Allergy, Asthma & Immunology, 8(6), 1791–1794, 10.1016/j.jaip.2020.04.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Agnes, M. (Ed.) (2005). Webster's new college dictionary: Wiley. [Google Scholar]
- Ahern, N. R. , Kiehl, E. M. , Sole, M. L. , & Byers, J. (2006). A review of instruments measuring resilience. Issues in Comprehensive Pediatric Nursing, 29, 103–125. 10.1080/01460860600677643 [DOI] [PubMed] [Google Scholar]
- Ahorsu, D. K. , Imani, V. , Lin, C. Y. , Timpka, T. , Broström, A. , Updegraff, J. A. , Årestedt, K. , Griffiths, M. D. & Pakpour, A. H. (2020). Associations between fear of COVID‐19, mental health, and preventive behaviours across pregnant women and husbands: an actor‐partner interdependence modelling. International Journal of Mental Health and Addiction, 1–15. 10.1007/s11469-020-00340-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Counseling Association . (2014). ACA code of ethics, Author. https://www.counseling.org/Resources/aca‐code‐of‐ethics.pdf. [Google Scholar]
- Arpaci, I. , Karataş, K. , & Baloğlu, M. (2020). The development and initial tests for the psychometric properties of the COVID‐19 Phobia Scale (C19P‐S). Personality and Individual Differences, 164, e110108. 10.1016/j.paid.2020.110108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brooks, S. K. , Webster, R. K. , Smith, L. E. , Woodland, L. , Wessely, S. , Greenberg, N. , & Rubin, G. J. (2020). The psychological impact of quarantine and how to reduce it: rapid review of the evidence. SSRN Electronic Journal. 10.2139/ssrn.3532534 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen, I. H. , Chen, C. Y. , Pakpour, A. H. , Griffiths, M. D. , & Lin, C. Y. (2020). Internet‐related behaviors and psychological distress among schoolchildren during COVID‐19 school suspension. Journal of the American Academy of Child and Adolescent Psychiatry, 59(10), S0890–8567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen, S. , & Bonanno, G. A. (2020). Psychological adjustment during the global outbreak of COVID‐19: A resilience perspective. Psychological Trauma: Theory, Research, Practice, and Policy, 12(S1), S51–S54. 10.1037/tra0000685 [DOI] [PubMed] [Google Scholar]
- Connor, K. M. , & Davidson, J. R. T. (2003). Development of a new resilience scale: The Connor‐Davidson Resilience Scale (CD‐RISC). Depression and Anxiety, 18(2), 76–82. 10.1002/da.10113 [DOI] [PubMed] [Google Scholar]
- Conover, W. J. (1999). Practical Nonparametric Statistics, Wiley series in probability and statistics: Applied probability and statistics. [Google Scholar]
- Costanzo, E. S. , Ryff, C. D. , & Singer, B. H. (2009). Psychosocial adjustment among cancer survivors: Findings from a national survey of health and well‐being. Journal Health Psychology, 28(2), 147–156. 10.1037/a0013221 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fagerland, M. W. , & Sandvik, L. (2009). Performance of five two‐sample location tests for skewed distributions with unequal variances. Contemporary Clinical Trials, 30(5), 490–496. 10.1016/j.cct.2009.06.007 [DOI] [PubMed] [Google Scholar]
- Fung, S. F. (2020). Validity of the brief resilience scale and brief resilient coping scale in a Chinese sample. International Journal of Environmental Research and Public Health, 17(4), 1265. 10.3390/ijerph17041265 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galloway, L. (2020). Five countries with the most resilient economies: British Broadcasting Corporation. http://www.bbc.com/travel/story/20200405‐covid‐19‐how‐global‐economies‐will‐recover‐from‐coronavirus [Google Scholar]
- Gao, J. , Zheng, P. , Jia, Y. , Chen, H. , Mao, Y. , Chen, S. , Wang, Y. , Fu, H. , & Dai, J. (2020). Mental health problems and social media exposure during COVID‐19 outbreak. PLoS One, 15(4), 1–10. 10.1371/journal.pone.0231924 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gruber, J. , Prinstein, M. , Abramowitz, J. S. , Albano, A. M. , Aldao, A. , Borelli, J. , Clark, L. A. , Davila, J. , Forbes, E. , Gee, D. , Hall, G. N. , Hallion, L. S. , Hinshaw, S. P. , Hofmann, S. G. , Hollon, S. , Joormann, J. , Kazdin, A. , Klein, D. , Levenson, R. , MacDonald, A. W. … Weinstock, L. (2020). Clinical psychological science's call to action in the time of COVID‐19. PsyArXiv Preprint. 10.31234/osf.io/desg9 [DOI] [Google Scholar]
- Henry, H. (2020). AUC holds first media virtual discussion on maintaining mental wellness during COVID‐19: SyndiGate Media Inc. http://aquinas.idm.oclc.org/login?url=https://search.proquest.com/docview/2389141594?accountid=8340 [Google Scholar]
- Hiremath, P. , Kowshik, C. S. , Manjunath, M. , & Shettar, M. (2020). COVID 19: Impact of lock‐down on mental health and tips to overcome. Asian Journal of Psychiatry, 51, e102088. 10.1016/j.ajp.2020.102088 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang, Y. , & Zhao, N. (2020). Generalized anxiety disorder, depressive symptoms and sleep quality during COVID‐19 outbreak in China: A web‐based cross‐sectional survey. Psychiatry Research, 288, e112954. 10.1016/j.psychres.2020.112954 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ihaka, R. , & Gentleman, R. (1997). The R project for statistical computing: Department of Statistics, University of Auckland. [Google Scholar]
- Johns Hopkins University . (2020). COVID‐19 world map. https://coronavirus.jhu.edu/map.html [Google Scholar]
- Kaba, D. , & Akin Sari, B. (2020). Acute stress disorder with panic episodes induced by exposure to COVID‐19 outbreak news in a child. Dusunen Adam: The Journal of Psychiatry and Neurological Sciences, 33. 10.14744/DAJPNS.2020.00084 [DOI] [Google Scholar]
- Lee, S. A. (2020). How much “Thinking” about COVID‐19 is clinically dysfunctional? Brain, Behavior, and Immunity, 87, 97–98. 10.1016/j.bbi.2020.04.067 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lu, W. , Wang, H. , Lin, Y. , & Li, L. (2020). Psychological status of medical workforce during the COVID‐19 pandemic: A cross‐sectional study. Psychiatry Research, 288, e112936. 10.1016/j.psychres.2020.112936 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McDaniel, S. H. , & de Gruy, F. V. (2014). An introduction to primary care and psychology. American Psychologist, 69, 325–331. 10.1037/a0036222 [DOI] [PubMed] [Google Scholar]
- Mehra, A. , Rani, S. , Sahoo, S. , Parveen, S. , Singh, A. P. , Chakrabarti, S. , & Grover, S. (2020). A crisis for elderly with mental disorders: Relapse of symptoms due to heightened anxiety due to COVID‐19. Asian Journal of Psychiatry, 51, e102114. 10.1016/j.ajp.2020.102114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization [WHO] . (2020). Mental health and psychosocial considerations during the COVID‐19 outbreak: Author. https://apps.who.int/iris/bitstream/handle/10665/331490/WHO‐2019‐nCoV‐MentalHealth‐2020.1‐eng.pdf [Google Scholar]
- Munk, A. J. L. , Schmidt, N. M. , Alexander, N. , Henkel, K. , & Hennig, J. (2020). Covid‐19—Beyond virology: Potentials for maintaining mental health during lockdown. PLoS One, 15(8), e0236688. 10.1371/journal.pone.0236688 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nrugham, L. , Holen, A. , & Sund, A. M. (2010). Associations between attempted suicide, violent life events, depressive symptoms, and resilience in adolescents and young adults. The Journal of Nervous and Mental Disease, 198(2), 131–136. 10.1097/NMD.0b013e3181cc43a2 [DOI] [PubMed] [Google Scholar]
- Peng, L. , Zhang, J. , Li, M. , Li, P. , Zhang, Y. , Zuo, X. , Miao, Y. , & Xu, Y. (2012). Negative life events and mental health of Chinese medical students: The effect of resilience, personality and social support. Psychiatry Research, 196(1), 138–141. 10.1016/j.psychres.2011.12.006 [DOI] [PubMed] [Google Scholar]
- Perlman, D. , Patterson, C. , Moxham, L. , Taylor, E. K. , Brighton, R. , Sumskis, S. , & Heffernan, T. (2017). Understanding the influence of resilience for people with a lived experience of mental illness: A self‐determination theory perspective. Journal of Community Psychology, 45(8), 1026–1032. 10.1002/jcop.21908 [DOI] [Google Scholar]
- Qiu, J. , Zhou, D. , Liu, J. , & Yuan, T. (2020). Mental wellness system for COVID‐19. Brain, Behavior, and Immunity., 10.1016/j.bbi.2020.04.032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- R‐4.0.3 for Windows . (2020). R Software. https://cran.r‐project.org/bin/windows/base/ [Google Scholar]
- Rajkumar, R. P. (2020). COVID‐19 and mental health: A review of the existing literature. Asian Journal of Psychiatry, 52, e102066. 10.1016/j.ajp.2020.102066 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roy, A. , Carli, V. , & Sarchiapone, M. (2011). Resilience mitigates the suicide risk associated with childhood trauma. Journal of Affective Disorders, 133(3), 591–594. 10.1016/j.jad.2011.05.006 [DOI] [PubMed] [Google Scholar]
- Rutter, M. (2006). Implications of resilience concepts for scientific understanding. Annuals of New York Academy of Sciences, 1094(1), 1–12. 10.1196/annals.1376.002 [DOI] [PubMed] [Google Scholar]
- Sharma, V. , Marin, D. B. , Koenig, H. K. , Feder, A. , Iacoviello, B. M. , Southwick, S. M. , & Pietrzak, R. H. (2017). Religion, spirituality, and mental health of US military veterans: Results from the National Health and Resilience in Veterans Study. Journal of Affective Disorders, 217, 197–204. 10.1016/j.jad.2017.03.071 [DOI] [PubMed] [Google Scholar]
- Smith, B. W. , Dalen, J. , Wiggins, K. , Tooley, E. , Christopher, P. , & Bernard, J. (2008). The brief resilience scale: Assessing the ability to bounce back. International Journal of Behavioral Medicine, 15, 194–200. 10.1080/10705500802222972 [DOI] [PubMed] [Google Scholar]
- Soer, R. , Six Dijkstra, M. W. M. C. , Bieleman, H. J. , Stwart, R. E. , Reneman, M. F. , & Oosterveld, F. G. J. (2019). Measurement properties and implications of the Brief Resilience Scale in healthy workers. Journal of Occupational Health, 61(3), 242–250. 10.1002/1348-9585.12041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sominsky, L. , Walker, D. W. , & Spencer, S. J. (2020). One size does not fit all ‐ Patterns of vulnerability and resilience in the COVID‐19 pandemic and why heterogeneity of disease matters. Brain, Behavior, and Immunity, 87, 1–3. 10.1016/j.bbi.2020.03.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Souza, A. C. D. , Alexandre, N. M. C. , & Guirardello, E. D. B. (2017). Psychometric properties in instruments evaluation of reliability and validity. Epidemiologia e Serviços de Saúde, 26, 649–659. [DOI] [PubMed] [Google Scholar]
- Tumlu, G. U. (2013). The investigation of Turkish pre‐service teacher's resilience levels in terms of certain variables. Procedia‐Social and Behavioral Sciences, 93, 2053–2057. 10.1016/j.sbspro.2013.10.164 [DOI] [Google Scholar]
- Van Hecke, T. (2012). Power study of anova versus Kruskal‐Wallis test. Journal of Statistics and Management Systems, 15(2–3), 241–247. 10.1080/09720510.2012.10701623 [DOI] [Google Scholar]
- Walpole, R. E. , & Myers, R. H. (2012). Probability & statistics for engineers & scientists: Pearson Education Limited. [Google Scholar]
- Zandifar, A. , & Badrfam, R. (2020). COVID‐19: Considering the prevalence of schizophrenia in the coming decades. Psychiatry Research, 288, e112982. 10.1016/j.psychres.2020.112982 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zoellner, L. A. , & Feeny, N. C. (Eds.) (2013). Facilitating resilience and recovery following trauma: Guilford Press. https://www.statisticssolutions.com/kruskal‐wallis‐test/ [Google Scholar]


