Abstract
Study Design:
Ambispective cohort study.
Objective:
Limited data exists comparing surgeon and patient expectations of outcome following spine surgery. The objective of this study was to elicit whether any differences exist between patient and surgeon expectations for common spine surgeries.
Methods:
Ten common age-appropriate clinical scenarios were generated and sent to Canadian spine surgeons to determine surgeon expectations for standard spine surgeries. Patients in the Canadian Spine Outcomes and Research Network (CSORN) registry matching the clinical scenarios were identified. Aggregated patient expectations were compared with surgeon responses for each scenario. A χ2 analysis was then completed to determine discrepancies between surgeon and patient expectations for each scenario.
Results:
A total of 51 Canadian spine surgeons completed the survey on surgical expectations. A total of 919 patients from multiple centers were identified within the CSORN database that matched the clinical scenarios. Our results demonstrated that patients tend to be more optimistic about the expected outcomes of surgery compared with the treating surgeon. The majority of patients in all clinical scenarios anticipated improvement in back or neck pain after surgery, which differed from surgeon expectations. Results also highlighted the effect of patient age on both patient and surgeon expectations. Discrepancies between patient and surgeon expectations were higher for older patients.
Conclusion:
We present data on patient and surgeon expectations for spine surgeries and show that differences exist particularly concerning the improvement of neck or back pain. Patient age plays a role in the agreement between the treating physicians and patients in regard to surgical expectations. The reasons for the discrepancies remain unclear.
Keywords: patient expectation, spine surgery, back/neck pain, age
Introduction
Patient expectations play a major role in the decision to undergo elective surgery.1 No data exists comparing surgeon and patient expectations of outcome following common spine surgery procedures. What studies are available indicate patients’ preoperative expectations of surgical outcomes are related to satisfaction for spine procedures, but also show that these expectations are variable.2-8 Data from hip and knee arthroplasty or sports injury patients consistently indicate that surgeons estimate operative outcomes as being more favorable than their patients’ report.9-13
Martin et al14 found that there is discordance between what surgeons held to be important to patients and what patients actually ranked as significant for hip procedures. This discrepancy, in addition to the differing expectations between patients and surgeons, may contribute to a lack of patient satisfaction. Furthermore, studies from Mancuso et al have indicated that patients are obtaining their knowledge about surgery and conceivably forming their expectations from a large number of nonmedical sources.15 Realistic patient expectations are known to be correlated with increased rates of satisfaction.3,5-7
To our knowledge, there are no scientific studies that compare preoperative surgical expectations from the perspective of patients and surgeons for common cervical and lumbar spine procedures. The objective of this study was to elicit whether differences exist and identify them. The secondary objective was to see if the age of the patient affected expectations.
Materials and Methods
This was a mixed methods study in which prospectively completed patient expectation data was compared to surgeon’s expectations obtained from responses to a questionnaire describing specific clinical scenarios.
Participants
Patient expectation data collected by the Canadian Spine Outcomes and Research Network (CSORN) between 2014 and 2017 was included. CSORN is a group of over 50 neurosurgical and orthopedic spine surgeons from 18 tertiary care academic and nonacademic hospitals across Canada that prospectively collects data on patients with spinal conditions. This database serves as a national registry created to answer research questions and to facilitate the implementation of best practices. Research ethics board approval was obtained by the Conjoint Health Research Ethics Board prior to the initiation of the study.
Patients fitting 1 of the 10 vignettes (see below) within the CSORN database were identified for inclusion. Preoperative expectation of postoperative outcome was recorded within the CSORN database and included for each identified patient. The expectations were measured using the modified Musculoskeletal Outcomes Data Evaluation and Management System (MODEMS) questionnaire described by Soroceanu et al16 for lumbar and cervical spine surgery. The questionnaire sent to surgeons was composed of 7 expectation items listed in Figures 1 to 3 and captured within the CSORN database for patients. In addition, both registry patients and surgeons (survey, for each clinical scenario) were asked the following: “What would be the SINGLE most important change occurring as a result of an operation that would make you say, ‘The operation helped and was a success!’?”
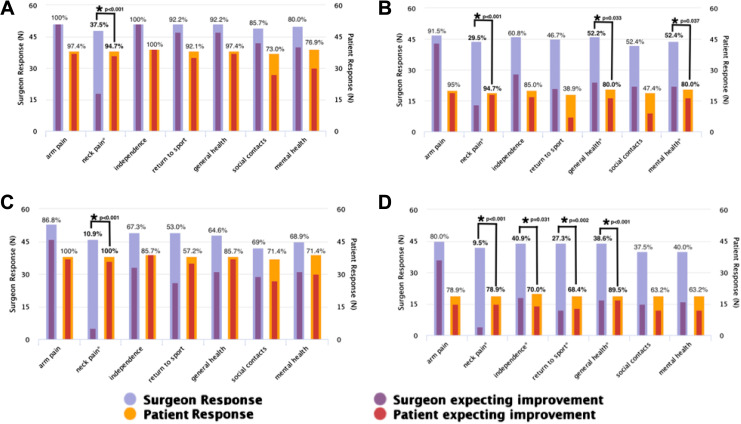
Figure 1.
Surgeon and patient expectations for specific outcomes in cervical surgery for radiculopathy. (A) Anterior surgery in young patients; (B) Anterior surgery in older patients; (C) Posterior surgery in young patients; (D) Posterior surgery in older patients (* denotes statistical significance between surgeons and patients).
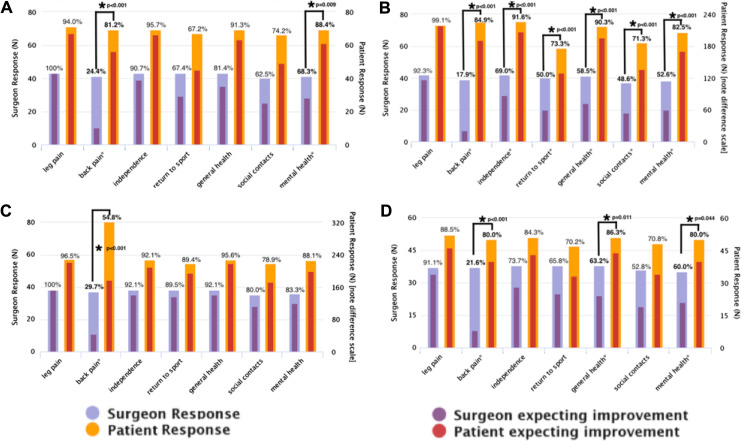
Figure 2.
Surgeon and patient expectations for specific outcomes in surgery for lumbar surgery for neurogenic claudication (A, B) and radiculopathy (C, D). (A) Neurogenic claudication in young patients; (B) Neurogenic claudication in older patients; (C) Radiculopathy in young patients; (D) Radiculopathy in older patients (*denotes statistical significance between surgeons and patients).
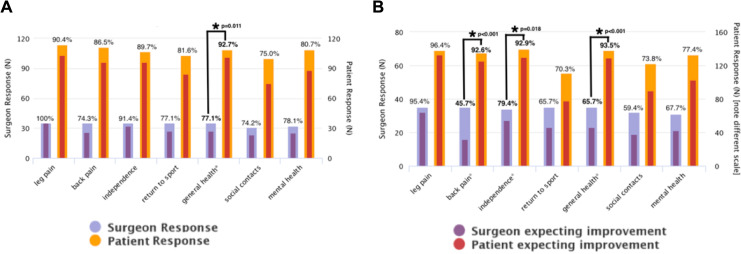
Figure 3.
Surgeon and patient expectations for specific outcomes in surgery for degenerative spondylolisthesis in young (A) and older patients (B) (*denotes statistical significance between surgeons and patients).
Patients under 65 years of age were defined as young, and those above 65 of age were defined as old as this is commonly used as an age cutoff in the literature. Inclusion criteria had to be met for each vignette, and in addition, patients had to be 18 years of age or older and able to provide consent. Exclusion criteria included the following: those unable to consent, those under 18 years of age, those having revision surgery, and those having more than one index surgery within the CSORN database.
Surgeon expectation of patient outcome data was completed for each of the 10 clinical vignettes through use of a survey. Consultant neurosurgical or orthopedic spine surgeons were recruited for participation through the Canadian Spine Society.
Clinical Vignettes Investigated, and Number of Patients Identified From CSORN Data
Cervical radiculopathy, young patient, anterior surgery
Cervical radiculopathy, young patient, posterior surgery
Cervical radiculopathy, older patient, anterior surgery
Cervical radiculopathy, older patient, posterior surgery
Neurogenic claudication, younger patient
Neurogenic claudication, older patient
Lumbar radiculopathy, younger patient
Lumbar radiculopathy, older patient
Degenerative spondylolisthesis, younger patient
Degenerative spondylolisthesis, older patient
Statistical Methods
Expectations were dichotomized as low (“no change” and “somewhat better”) versus high (“better” and “much better”) to facilitate interpretation of results across multiple clinical scenarios. Statistical analysis was performed using Stata (v14.0). Chi-square tests were used to compare surgeon versus patient expectations in regard to postoperative improvement for each of the clinical vignettes. The level of significance was set to P < .05.
Results
All patients within the registry who satisfied criteria of a specific clinical scenario were included. In total, 919 patients were included from the CSORN registry. The number of patients included within each clinical vignette varied according to data availability. Fifty-one CSS member consultant spine surgeons (response rate of 39%) completed the online expectation survey for all clinical vignettes.
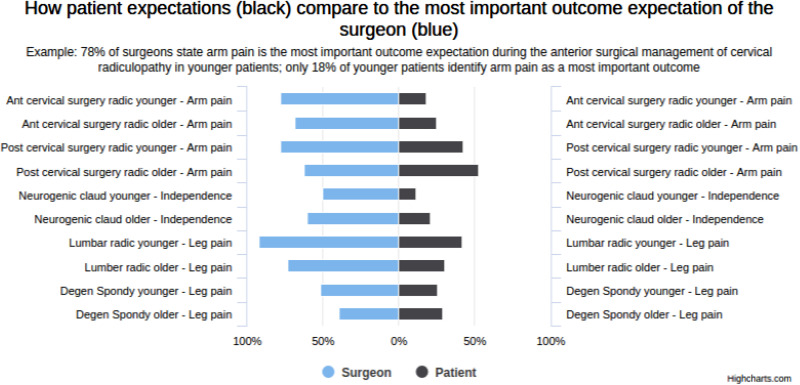
Figure 4 summarizes the most important surgeon expectation for each of the scenarios and highlights the discrepancies between the surgeons’ and patients’ most important expectation. Except for patients with claudication where improved independence was paramount, surgeons generally expected radicular symptom improvement to be the most important. In all scenarios these choices differed from the patients’ most important improvement.
Figure 4.
A comparison of how patients’ expectations differ relative to the surgeon’s most important expectation for each of the 10 clinical scenarios. This figure demonstrates that surgeons’ expectations are largely focused on alleviating radicular symptoms whereas patient expectations are more varied.
The 10 vignettes enumerated in the Methods section are presented in Figures 1 through 3. Anterior and posterior cervical surgery expectations were analyzed for both older and younger patients and are presented in Figure 1. Expectations from younger and older patients with neurogenic claudication were also analyzed and are presented in Figures 2A and 2B, while expectations of younger and older patients with lumbar radiculopathy were analyzed and are presented in Figures 2C and 2D. Expectations for younger and older patients being treated for degenerative spondylolisthesis are presented in Figure 1.
If a response was left blank by a surgeon or patient, it was removed from the analysis. Agreement or discrepancy between the surgeons’ expectations and patients’ expectations are analyzed and are presented in Figures 1 through 3, with statistical significance for all χ2 analyses being defined as a P value less than .05. Responses for both surgeons and patients were dichotomized to responses showing improvement (better or much better responses in questionnaires) and those with no improvement (no change or somewhat better in the questionnaires).
Our results demonstrated that young patients with radiculopathy expected to have improvement in neck pain with anterior or posterior cervical surgery and improvement in back pain with lumbar surgery, which differed with statistical significance compared to surgeons’ expectations (P < .001). The results also showed that young patients with neurogenic claudication expected to have improvement in back pain and mental health after surgery, which significantly differed from the expectations of the surgeons. In addition, the results demonstrated that younger patients with spondylolisthesis had comparable expectation with surgeons regarding back pain improvement but also expected to have improvement in their general health, which differed significantly compared with the surgeons’ responses.
This study demonstrates that older patients had higher expectations compared with their younger counterparts for all scenarios and these expectations differed significantly from the surgeons’ expectations. Patients with neurogenic claudication expected improvement in all categories. They only had similar expectations to that of surgeons for improved leg pain. The extent of disagreement between surgeons’ expectations and patients’ expectations differed for each scenario, but in general, surgeons had lower expectations than older patients.
Discussion
This article presents and analyzes expectations (7 items) of spine patients and surgeons with regard to 10 common clinical surgical scenarios. These 10 scenarios included radiculopathy, neurogenic claudication, and spondylolisthesis. Although some studies have shown that patient expectations are related to surgical satisfaction,3,5-7 little is known about differences between surgeon and patient expectations for different spine procedures. This study is the first to compare surgeon versus patient expectations for common clinical scenarios requiring different spine procedures.
Our results suggest that better surgeon and patient communication is needed to ensure that patients have appropriate expectations for the given pathology and procedure. This was highlighted by the gross discrepancy in the most important expectation by surgeons versus the most important expectations of the patients. Within the 7 specific expectation items, patients tended to be more optimistic about the expected outcomes of surgery in comparison to the treating surgeons, particularly regarding the improvement of neck and back pain. This is similar to other studies, which demonstrate similar discrepancies between surgeons and patients even though credible information is often provided either verbally or in writing to patients by surgeons prior to surgery,5,8,17 patient expectations for hip disorders also differed in comparison to their treating surgeons’ expectations,14 demonstrating that this discordance is not limited to spine surgery. Patient expectations have been linked to overall satisfaction with surgery and influence health-related quality of life.18 These results highlight the need for improved preoperative communication, education, and clarification of anticipated surgical outcomes, which reconcile patient and surgeon expectations. This education could be offered in different media for emphasis and to cater to individual patient needs. Having patient-surgeon expectations well aligned may result in improved patient satisfaction postoperatively.
The majority of patients in all clinical scenarios anticipated improvement in back or neck pain after surgery. The majority of surgeons had less optimistic expectations. The lower likelihood in axial pain improvement after spine surgery is supported in the literature since its etiology is not always easy to identify.19,20 Therefore, surgeon experience may also play a role in explaining some of the discrepancies especially when it comes to axial pain. This highlights the importance of appropriate preoperative education for spine surgery patients. In contrast, young patients with degenerative spondylolisthesis and almost half of the surgeons expected improvement in axial back pain, which is in accordance with previous publications.21
Results presented in this study highlight the effect of patients’ age on both patient and surgeon expectations. Surgeon expectations tended to be more in agreement with those of younger patients, while older patients seem to overestimate the benefits of surgery. Other than disagreement over the resolution of neck pain, for anterior cervical surgery there was no statistical differences between surgeon and young patients’ expectations. By contrast, older patients had 3 categories of disagreement: pain improvement, general health improvement, and mental health improvement. This trend was seen in all clinical scenarios. This can be explained either by lower surgeon expectations of surgical benefit for their older patients or by overly optimistic older patients about the role of surgery in treating their disease. Although previous studies in patients with spinal disorders have shown that differences between surgeon and patient expectations do exist,10,14,22 this is the first study to investigate the influence of age on expectations.
The was a multicentered study, which adds to the generalizability of our results. Some scenarios had a low number of patients and may not be representative of the entire population. We were also limited to the questionnaires and data available in the CSORN database. Although this article has its limitations, the use of a large database, and the good response rate from Canadian spine surgeons, does provide an idea of the discrepancies that exist between patient and surgeon expectations for common spine procedures. Perhaps the most significant limitation was being unable to control for what influenced a patient’s expectations. It is likely multifactorial but standardized preoperative education counselling or knowing how specific surgeons educated the patient would be valuable, more specifically comparing expectations between the patient and the patient’s surgeon.
Conclusion
Differences between patient and surgeon expectations in outcome exist, even if we assume that an appropriate informed consent process has occurred. Patient age plays a significant role in whether there is agreement regarding postoperative outcomes. This article informs us that significant discrepancies may exist between patient and surgeon expectations for common spine surgical procedures. The reasons need to be clarified and may be related to ineffective communication prior to surgery. These results should encourage spine surgeons to be more explicit in the information they provide to their patients in order to ensure that their patients’ expectations are in alignment with their own.
Acknowledgments
The authors thank all the subjects who participated in the study and the support staff, research coordinator staff, and investigators from the Canadian Spine Outcomes and Research Network (CSORN) contributing sites: Calgary Foothills Medical Centre; Canada East Spine Centre, Saint John; Vancouver General Hospital; Victoria Hospital—London Health Sciences Centre; Queen Elizabeth II—Halifax Sciences Centre; Quebec Hopital de L’enfant Jesus, Edmonton University of Alberta Hospital; St Michael’s Hospital, Toronto; the Ottawa Hospital.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Mannion AF, Junge A, Elfering A, Dvorak J, Porchet F, Grob D. Great expectations: really the novel predictor of outcome after spinal surgery? Spine (Phila Pa 1976). 2009;34:1590–1599. [DOI] [PubMed] [Google Scholar]
- 2. Gepstein R, Arinzon Z, Adunsky A, Folman Y. Decompression surgery for lumbar spinal stenosis in the elderly: preoperative expectations and postoperative satisfaction. Spinal Cord. 2006;44:427–431. [DOI] [PubMed] [Google Scholar]
- 3. Lattig F, Fekete TF, O’Riordan D, et al. A comparison of patient and surgeon preoperative expectations of spinal surgery. Spine (Phila Pa 1976). 2013;38:1040–1048. [DOI] [PubMed] [Google Scholar]
- 4. Lutz GK, Butzlaff ME, Atlas SJ, Keller RB, Singer DE, Deyo RA. The relation between expectations and outcomes in surgery for sciatica. J Gen Intern Med. 1999;14:740–744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Mannion AF, Elfering A, Staerkle R, et al. Outcome assessment in low back pain: how low can you go? Eur Spine J. 2005;14:1014–1026. [DOI] [PubMed] [Google Scholar]
- 6. McGregor AH, Hughes SP. The evaluation of the surgical management of nerve root compression in patients with low back pain: part 2: patient expectations and satisfaction. Spine (Phila Pa 1976). 2002;27:1471–1477. [DOI] [PubMed] [Google Scholar]
- 7. Ronnberg K, Lind B, Zoega B, Halldin K, Gellerstedt M, Brisby H. Patients’ satisfaction with provided care/information and expectations on clinical outcome after lumbar disc herniation surgery. Spine (Phila Pa 1976). 2007;32:256–261. [DOI] [PubMed] [Google Scholar]
- 8. Toyone T, Tanaka T, Kato D, Kaneyama R, Otsuka M. Patients’ expectations and satisfaction in lumbar spine surgery. Spine (Phila Pa 1976). 2005;30:2689–2694. [DOI] [PubMed] [Google Scholar]
- 9. Brokelman RB, van Loon CJ, Rijnberg WJ. Patient versus surgeon satisfaction after total hip arthroplasty. J Bone Joint Surg Br. 2003;85:495–498. [PubMed] [Google Scholar]
- 10. Ghomrawi HM, Ferrando NF, Mandl LA, Do H, Noor N, Valle AGD. How often are patient and surgeon recovery expectations for total joint arthroplasty aligned? Results of a pilot study. HSS J. 2011;7:229–234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Harris IA, Harris AM, Naylor JM, Adie S, Mittal R, Dao AT. Discordance between patient and surgeon satisfaction after total joint arthroplasty. J Arthroplasty. 2013;28:722–727. [DOI] [PubMed] [Google Scholar]
- 12. Moran M, Khan A, Sochart DH, Andrew G. Expect the best, prepare for the worst: surgeon and patient expectation of the outcome of primary total hip and knee replacement. Ann R Coll Surg Engl. 2003;85:204–206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Noble PC, Fuller-Lafreniere S, Meftah M, Dwyer MK. Challenges in outcome measurement: discrepancies between patient and provider definitions of success. Clin Orthop Relat Res. 2013;471:3437–3445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Martin RL, Mohtadi NG, Safran MR, et al. Differences in physician and patient ratings of items used to assess hip disorders. Am J Sports Med. 2009;37:1508–1512. [DOI] [PubMed] [Google Scholar]
- 15. Mancuso CA, Duculan R, Cammisa FP, et al. Sources of patients’ expectations of lumbar surgery. Spine (Phila Pa 1976). 2019;44:318–324. [DOI] [PubMed] [Google Scholar]
- 16. Soroceanu A, Ching A, Abdu W, McGuire K. Relationship between preoperative expectations, satisfaction, and functional outcomes in patients undergoing lumbar and cervical spine surgery: a multicenter study. Spine (Phila Pa 1976). 2012;37:E103–E108. [DOI] [PubMed] [Google Scholar]
- 17. Mancuso CA, Duculan R, Cammisa FP, et al. Proportion of expectations fulfilled: a new method to report patient-centered outcomes of spine surgery. Spine (Phila Pa 1976). 2016;41:963–970. [DOI] [PubMed] [Google Scholar]
- 18. Yee A, Adjei N, Do J, Ford M, Finkelstein J. Do patient expectations of spinal surgery relate to functional outcome? Clin Orthop Relat Res. 2008;466:1154–1161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Buchbinder R, van Tulder M, Oberg B, et al. Low back pain: a call for action. Lancet. 2018;391:2384–2388. [DOI] [PubMed] [Google Scholar]
- 20. Haldeman S, Johnson CD, Chou R, et al. The Global Spine Care Initiative: care pathway for people with spine-related concerns. Eur Spine J. 2018;27(suppl 6):901–914. [DOI] [PubMed] [Google Scholar]
- 21. Patel DR, Kinsella E. Evaluation and management of lower back pain in young athletes. Transl Pediatr. 2017;6:225–235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Graz B, Wietlisbach V, Porchet F, Vader JP. Prognosis or “curabo effect?” physician prediction and patient outcome of surgery for low back pain and sciatica. Spine (Phila Pa 1976). 2005;30:1448–1452. [DOI] [PubMed] [Google Scholar]