Abstract
Background
In the spring of 2020, New York City was an epicenter of coronavirus disease 2019 (COVID‐19). The post‐hospitalization needs of COVID‐19 patients were not understood and no outpatient rehabilitation programs had been described.
Objective
To evaluate whether a virtual rehabilitation program would lead to improvements in strength and cardiopulmonary endurance when compared with no intervention in patients discharged home with persistent COVID‐19 symptoms.
Design
Prospective cohort study.
Setting
Academic medical center.
Patients
Between April and July 2020, 106 patients discharged home with persistent COVID‐19 symptoms were treated. Forty‐four patients performed virtual physical therapy (VPT); 25 patients performed home physical therapy (HPT); 17 patients performed independent exercise program (IE); and 20 patients did not perform therapy.
Interventions
All patients were assessed by physiatry. VPT sessions were delivered via secure Health Insurance Portability and Accountability Act compliant telehealth platform 1‐2 times/week. Patients were asked to follow up 2 weeks after initial evaluation.
Main Outcome Measures
Primary study outcome measures were the change in lower body strength, measured by the 30‐second sit‐to‐stand test; and the change in cardiopulmonary endurance, measured by the 2‐minute step test.
Results
At the time of follow‐up, 65% of patients in the VPT group and 88% of patients in the HPT group met the clinically meaningful difference for improvement in sit‐to‐stand scores, compared with 50% and 17% of those in the IE group and no‐exercise group (P = .056). The clinically meaningful difference for improvement in the step test was met by 74% of patients in the VPT group and 50% of patients in the HPT, IE, and no‐exercise groups (P = .12).
Conclusions
Virtual outpatient rehabilitation for patients recovering from COVID‐19 improved lower limb strength and cardiopulmonary endurance, and an HPT program improved lower limb strength. Virtual rehabilitation seems to be an efficacious method of treatment delivery for recovering COVID‐19 patients.
INTRODUCTION
Coronavirus disease 2019 (COVID‐19), the disease caused by severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2), exists along a spectrum. In those with moderate to severe illness, pulmonary, neurologic, musculoskeletal, and psychiatric symptoms have been commonly reported. 1 , 2 During the first wave of infections in the spring of 2020, New York City was the epicenter for virus transmission in the United States. As of December 22, 2020, there have been more than 18.3 million confirmed cases of COVID‐19 in the United States 3 and more than 871,000 confirmed cases in New York State, with a rapid influx of cases occurring between March and May 2020. 4 At the New York Presbyterian Hospital system (including eight regional hospitals in the New York metropolitan area), approximately 9,500 patients in total were hospitalized with COVID‐19, 34% requiring ventilator support, and more than 6,000 were discharged between March and May 2020.
At the time of manuscript preparation, rates of hospitalization due to COVID‐19 infection across the United States and worldwide are increasing. As of December 22, 2020 more than 117,000 people are currently hospitalized with COVID‐19, an increase of over 40% during the past month. 5 Although the sequelae of patients with critical illness due to COVID‐19 have been reported, 6 , 7 the needs of patients who had been hospitalized briefly but were not critically ill with COVID‐19 were not clearly understood during the first peak of the pandemic in New York. Furthermore, given the rapid influx of patients admitted to the hospital with COVID 19 at that time, there was a need to quickly and safely discharge patients home to quarantine when they were medically stable. The literature has shown that many patients discharged after hospitalization for COVID‐19 exhibited ongoing fatigue, dyspnea, cognitive impairment, and sleep dysfunction. 1 , 2 , 7 , 8 , 9 These symptoms were found to be present in discharged patients with or without an intensive care unit stay. 2 These symptoms are often complicated by the significant stress patients experienced in the hospital: infrequent, short‐duration visits from medical providers, lack of family presence at the bedside, and a general lack of information about disease course, treatment options, and prognosis. 10 There is also an emerging body of evidence of “long hauler” patients reporting persistent symptoms weeks to months after initial COVID‐19 infection. A majority of these patients had initially mild‐moderate cases of COVID‐19 not requiring mechanical ventilation. 8 These persistent symptoms include fatigue, shortness, of breath, joint pain, chest pain, headaches, body aches, brain fog, and gastrointestinal symptoms. 1 , 11 , 12 We identified a need for close post‐discharge follow‐up to ensure recovery and better understanding of short‐, medium‐, and long‐term outcomes in these patients.
Our combined Department of Rehabilitation Medicine at Columbia University Irving Medical Center and Weill Cornell Medicine formed a physiatry‐led multidisciplinary team rapidly in mid‐April in order to treat those patients who had been discharged from two of the eight regional hospitals in our system who were diagnosed with COVID‐19 and who were experiencing persistent symptoms. Given the high prevalence of COVID‐19 at the time the program was developed, it was decided that all services would be offered via video visit only to limit the unintended spread of disease. We coordinated with physical therapists with a background in cardiopulmonary and musculoskeletal rehabilitation, speech language pathologists, and neuropsychologists in order to evaluate and treat the physical, cognitive, and psychological symptoms, as well as to address the functional impairments after COVID‐19 hospitalization. Our goal was to provide clinical care to patients with persistent symptoms of COVID‐19. Our pilot program evaluated and monitored the change in lower body strength, measured by the 30‐second sit‐to‐stand test; and the change in cardiopulmonary endurance, measured by the 2‐minute step test in patients who did and did not participate in our rehabilitation program.
To our knowledge this is the first report evaluating the outcomes of those patients hospitalized with COVID‐19 infection in the United States after a telemedicine virtual rehabilitation program. We compared the strength and endurance changes after participation in our program to those patients receiving home physical therapy, performing an independent exercise program, or performing no exercise intervention.
METHODS
Study design
This study was a program evaluation. The program was formed to meet the rehabilitation needs of patients diagnosed with COVID‐19 in the setting of in‐person clinic shutdowns and an immediate need to move as many services as possible to a virtual setting. This program was created for clinical purposes not research and therefore the population was not randomized. Evaluation of the outcome data was approved by the institutional review boards of Columbia University Irving Medical Center and Weill Cornell Medicine.
Eligibility
An outpatient rehabilitation program was implemented to evaluate and treat persistent symptoms as well as to address the functional impairments after COVID‐19 hospitalization. 13 Patients were referred to this program through discharging hospital teams and a remote patient monitoring program that our two affiliated hospitals used to follow patients after discharge. This is further described in our initial publication on designing our COVID‐19 rehabilitation program. 13 These medical teams identified patients with persistent symptoms and referred to our program for continued care with the following criteria: (1) discharge from the hospital with persistent symptoms of weakness, fatigue, shortness of breath that interfered with daily activities; (2) difficulty weaning from supplemental oxygenation; or (3) discharge from acute rehabilitation unit with need to continue physiatry‐led care. Exclusion criteria included patients who were unable to participate in a virtual exercise program owing to safety concerns regarding their concurrent medical conditions. Patients were not excluded if they had received mechanical ventilation; therefore, the population of patients evaluated was broad and included those recovering from mild disease as well as those who were critically ill.
Assessment
All patients were initially assessed by one of five physiatrists via telemedicine evaluation. At the start of this initiative, our outpatient rehabilitation clinics and therapy gyms were closed to prevent unintended spread of disease. Because of this limitation, our entire team relied on an Epic integrated video visit platform (Epic Haiku, Epic Canto) to deliver care. In some cases because of technical difficulties, other Health Insurance Portability and Accountability Act (HIPAA)‐compliant platforms such as Doxy.me, Doximity, or Zoom were used. A thorough virtual assessment was undertaken, including review of patient chart and hospital stay, assessment of demographics, height, weight, as well as notation of preexisting medical conditions, evaluation of persistent symptoms, identification of specific activities of daily living (ADL) impairments, and observation of vital parameters such as respiratory rate, and when pulse oximetry was available, SpO2 and heart rate. Providers followed a templated note to ensure they were able to obtain all relevant information and evaluated patients comprehensively. Screening was performed to assess any cognitive impairments using the mini‐Montreal Cognitive Assessment (MOCA) test. 14 In addition, the Patient Health Questionnaire‐4 (PHQ‐4) was used to screen for symptoms of anxiety and depression. 15 Functional impairments were evaluated virtually using the 30‐second sit‐to‐stand test, a validated tool to evaluate lower body strength, 16 , 17 which is measured by counting the number of times a patient can stand to a fully erect position from a seated position with arms folded across their chest in 30 seconds time. Additionally, we used the 2‐minute step test, which evaluates cardiopulmonary endurance and is performed by having the patient stand and step in place raising each knee to a point midway between patella and iliac crest for a total of 2 minutes, counting the number of times the right knee reaches the target. 17 We chose these functional tests because they can be easily assessed using a virtual format. After institutional review board approval was obtained, verbal consent was requested from patients to participate in our program, including permission to review data from the medical record as well as collect and analyze data during the patients' virtual visits.
The need for virtual physical therapy was ascertained based on symptoms, ADL impairments, and functional assessments. Upon evaluation, those patients who were already undergoing home physical therapy as coordinated by their discharging medical team were asked to continue their current exercise program. For those patients who were functioning at a high level, or who stated that they were unable or uninterested to participate in a virtual physical therapy program, a home exercise guide with a graded, phased exercise program was made available (see Supplementary materials). For those patients with PHQ‐4 scores >4, a neuropsychological evaluation was recommended, and for patients complaining of persistent cognitive difficulties or a score of <11 on the mini‐MOCA, a cognitive speech language pathology referral was placed. All patients were asked to follow up after 2 weeks to assess their progress.
Full details of the virtual physical therapy program are presented in the Supplementary materials. Briefly, virtual physical therapy sessions were held exclusively via a secure, HIPAA‐‐compliant telehealth platform. Sessions varied from 30 to 60 minutes. Patients were divided into low‐compromised patients and moderately compromised patients. Low‐compromised patients were classified as patients who did not need supplemental oxygen at home or had small variations in oxygen saturation levels (SpO2) during and after exertion (ie, SpO2 remained above 88%), and moderately compromised patients were classified as patients who needed to remain on supplemental oxygen or had large variations in oxygen saturation levels during and after exertion (ie, a reduction in SpO2 to <88%). Patients who were classified as low‐compromised patients were referred to our musculoskeletal physical therapy group through the Columbia University Programs in Physical Therapy Faculty Practice, whereas those who were considered moderately compromised were seen by cardiopulmonary physical therapists from New York Presbyterian's Outpatient Cardiopulmonary Department.
Patients were seen either once or twice per week by the physical therapist and were given guidelines of how frequently to perform their exercise program independently at home, outside of therapy sessions. At the primary physical therapy session, clinicians were able to identify exercise tolerance and obtain baseline vitals for each patient. At each subsequent physical therapy session, vitals were monitored using the pulse oximeter for heart rate and oxygen saturation levels if available, and the rate of perceived exertion 18 was also recorded and monitored throughout the session. If requiring the use of supplemental oxygen, the patient was advised to uptitrate their oxygen level to keep SpO2 > 88% while exercising. Discharge criteria included meeting therapy goals, being independent in performing their home exercise program, being independent in monitoring vitals at rest and during activity, knowing safe oxygen saturation limits, and knowing when to call their physician or emergency services.
Analysis
Analysis was performed using SPSS v.27 (IBM, Armonk, NY, USA) with significance testing set at alpha ≤ .05. Descriptive statistics were described using percentage of total population for categorical variables and medium and interquartile range for continuous variables. Categorical variables were compared between groups using a chi‐square test. Continuous variables were compared using a Kruskal‐Wallis test for the demographics. Some patients could not perform the assessments because they were performing their telemedicine visit at a location not conducive to the testing, such as work, or lost video feed so the test could not be viewed (this was approximately 10%‐15% of the total). Computational imputation was used for such missing values for the nonparametric analysis. Missing values were replaced with the series mean (N = 10 for the sit‐to‐stand: five virtual physical therapy [VPT], three home physical therapy [HPT], two independent exercise [IE], 0 none; and N = 15 for the step test: seven VPT, three HPT, two IE, three none). Computational imputation was not used for patients who were lost to follow‐up, only those who performed a follow‐up visit but exercise testing could not be assessed because of technical difficulties or location limitations, as described. Patients who were lost to follow‐up were not included in the analysis. Changes in sit‐to‐stand scores and step test scores were tested using a Wilcoxon Signed Rank Test comparing initial to follow‐up within‐group (mean, SD, test statistic, significance and effect size with Cohen's D with Hedges correction reported). The average follow‐up time was 2 weeks. We set the clinically meaningful difference (CMD) for our main functional outcomes as follows: an increase of 2 repetitions during the 30‐second sit‐to‐stand test 19 and an increase of ≥25% steps during the 2‐minute step test. 20 Differences in the number of patients who met the CMD in each of these parameters was tested using the chi‐square test linear‐by‐linear association for multiple group comparison and likelihood ratio comparing differences between VPT and none and HPT and none, with the cases that met the CMD coded accordingly.
RESULTS
We evaluated a total of 106 patients in the COVID‐19 outpatient rehabilitation program between April 24, 2020 and July 13, 2020. Two patients were excluded from the exercise assessment analysis; one was unable to perform the exercises because of a recent myocardial infarction and the other because of open wounds.
Forty‐four patients performed VPT, 25 patients performed HPT, 17 patients performed unsupervised IE, and 20 patients were referred to VPT or HPT but did not perform any therapy (none). Fifty‐three patients of the initial 106 returned for telemedicine follow‐up visits after referral to various therapy services. Of the 53 patients who returned, 31 performed VPT, eight performed HPT, eight performed IE, and six did not engage in any therapy. Thus, 70% of the VPT group, 32% of the HPT group, 47% of the IE group, and 30% of the none group returned for follow‐up visits.
Baseline characteristics for each group of patients are shown in Table 1. Groups were similar with regard to age, race/ethnicity, and medical comorbidities; the group receiving HPT had more impairments with regard to performing ADLs. More women were in the VPT and none groups. A majority of patients were Hispanic (51%), followed by White (18%), Black (17%), and Asian (12%), and hypertension and diabetes were the most common medical comorbidities (Table 1). Baseline PHQ‐4 scores were significantly higher in the VPT group than the other groups (Table 1). The mini‐MOCA scores were similar between groups; in all groups, the mean mini‐MOCA scores were within normal limits, and PHQ‐4 composite scores were in the minimal to mild range. Psychology referrals were made in 8% of visits, and speech language pathology referrals were made in 3% of visits.
TABLE 1.
Participant characteristics (total N = 106)
| Characteristic | VPT (n = 44) | HPT (n = 25) | IE (n = 17) | None (n = 20) | P value |
|---|---|---|---|---|---|
| COVID Admission | 93% | 96% | 94% | 95% | .97 |
| Body mass index (kg/m2) | 30.6 (8.2) (n = 27) | 28.4 (5.2) (n = 24) | 29.2 (6.7) (n = 13) | 28.7 (9.7) (n = 13) | .51 |
| Age (years) | 60 (14) | 57 (14) | 59 (20) | 58 (18) | .76 |
| Gender (% female) | 57% | 24% | 35% | 55% | .04 |
| PHQ‐4 | 1 (4) (n = 39) | 0 (1) (n = 21) | 0 (1) (n = 15) | 0 (1)(n = 17) | .02 |
| Race/Ethnicity | |||||
| White | 16% | 24% | 18% | 15% | .95 |
| Black | 18% | 16% | 12% | 20% | |
| Hispanic | 52% | 44% | 59% | 50% | |
| Asian | 9% | 16% | 12% | 15% | |
| Unknown | 5% | 0% | 0% | 0% | |
| Preexisting Medical Conditions | |||||
| Congestive heart failure | 2% | 4% | 0% | 10% | .24 |
| Coronary artery disease | 11% | 12% | 12% | 5% | .48 |
| Hypertension | 50% | 60% | 65% | 55% | .67 |
| Diabetes | 25% | 52% | 35% | 40% | .09 |
| Asthma | 9% | 12% | 6% | 0% | .46 |
| Other lung disease | 18% | 16% | 0% | 10% | .33 |
| Autoimmune disorder | 11% | 8% | 6% | 0% | .51 |
| Impaired Activities of Daily Living Post COVID | |||||
| None | 52% | 40% | 88% | 80% | .002 |
| Some (1 or 2) | 39% | 44% | 12% | 10% | |
| Most | 0% | 16% | 0% | 5% | |
| Unknown | 9% | 0% | 0% | 5% | |
Represented as percentage of total sample or median (IQR).
Abbreviations: COVID, coronavirus disease; HPT, home in‐person physical therapy; IE, independent exercise; IQR, interquartile range; None, referred to physical therapy but did not attend; PHQ‐4, Patient Health Questionnaire‐4; VPT, virtual physical therapy.
Hospitalization data are shown in Table 2. Overall, 30% of the entire cohort required mechanical ventilation and mean hospital length of stay was 21 days. The mean resting SpO2 for the population at the initial visit was 96 ± 3% (N = 80) and at the follow‐up visit was 98 ± 1% (N = 33). Resting SpO2 was not significantly different between groups at the initial visit (P = .38) or follow‐up (P = .33). Within the follow‐up population, SpO2 significant improved from 92 ± 5% to 95 ± 3% (p = .02). For patients prescribed oxygen (N = 19) the mean oxygen use was 2 ± 1 L/min, with no significant difference between groups (P = .99).
TABLE 2.
Median (IQR) for hospitalization data
| Variable | VPT (n = 44) | HPT (n = 25) | IE (n = 17) | None (n = 20) | P value |
|---|---|---|---|---|---|
| Days Hospitalized | 14 (14) | 39 (30) | 9 (17) | 13 (33) | <.001 |
| Days Intubated [n = 32] | 13 (11) (n = 6) | 20 (15) (n = 16) | 10 (15) (n = 5) | 13 (17) (n = 5) | .511 |
Abbreviations: HPT, home in‐person physical therapy; IE, independent exercise; IQR, interquartile range; None, referred to physical therapy but did not attend; VPT, virtual physical therapy.
Table 3 shows baseline and follow‐up scores for 30‐second sit‐to‐stand test and 2‐minute step test. There were no differences in baseline performance of these measures between groups. At the time of follow‐up, 65% of patients in the VPT group and 88% of patients in the HPT group met the CMD for improvement in sit‐to‐stand scores, compared with only 50% and 17% of those in the IE and no‐exercise group, respectively. Across groups these differences were not statistically significant (P = .056) but the VPT group and HPT group demonstrated a significantly higher percentage who met CMD than none (P = .03 and P < .01, respectively). The step test also demonstrated the VPT group to have a higher percentage of patients achieve the CMD. The CMD was achieved by 74% of patients in the VPT group versus 50% of the patients in the HPT group, in the IE group as well as the no‐exercise group. These differences were not statistically different across groups (P = .12) or between VPT and the none group (P = .25). The mean improvements in sit‐to‐stand and step test scores are shown in Figures 1 and 2, for all groups. Significant improvements in sit‐to‐stand scores were seen in VPT and HPT groups (Table 3 and Figure 1). Significant improvements were also seen in the step test score in VPT, HPT, and IE (Table 3 and Figure 2). Those who did not perform any type of physical therapy or IE demonstrated no significant improvement in either exercise test.
TABLE 3.
Comparison between groups in patients with follow‐up visits (N = 53)
| Variable | Group | Initial visit (mean, SD) | Follow‐up visit (mean, SD) | Wilcoxon Signed Rank Test comparing initial to follow‐up within‐group (test statistic, significance) | Effect size (Cohen's D with Hedges correction) |
|---|---|---|---|---|---|
| Sit‐to‐Stand Score | VPT | 9 ± 4 | 13 ± 3 |
Z = −4.26, P < .001 |
1.14 |
| HPT | 8 ± 3 | 12 ± 1 |
Z = −2.53, P = .01 |
1.02 | |
| IE | 10 ± 5 | 13 ± 3 |
Z = ‐1.89, P = .06 |
.61 | |
| None | 12 ± 4 | 11 ± 7 |
Z = .000, P > .99 |
.15 | |
| Step Test Score | VPT | 44 ± 23 | 73 ± 26 |
Z = ‐4.21, P < .001 |
.96 |
| HPT | 46 ± 27 | 71 ± 30 |
Z = ‐2.2, P = .02 |
1.11 | |
| IE | 54 ± 24 | 76 ± 14 |
Z = ‐2.20, P = .03 |
.85 | |
| None | 59 ± 30 | 69 ± 12 |
Z = ‐1.16, P = .25 |
.38 |
Abbreviations: HPT, home physical therapy (n = 8); IE, independent exercise (n = 8); None, referred to physical therapy but did not attend (n = 6); SD, standard deviation; VPT, virtual physical therapy (n = 31).
FIGURE 1.
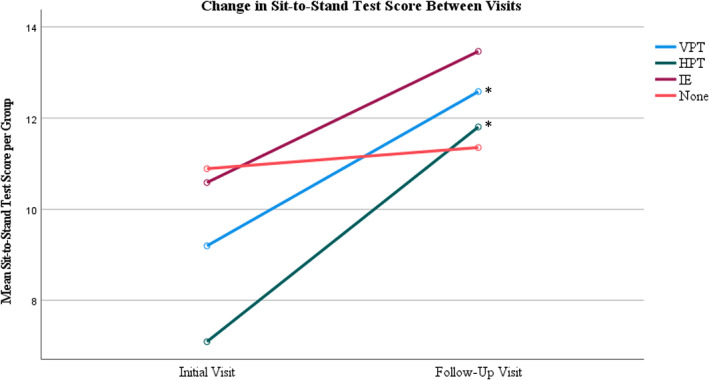
Sit‐to‐stand results for patients who returned for follow‐up. HPT, home in‐person physical therapy; IE, independent exercise; None, referred to physical therapy but did not attend; VPT, virtual physical therapy. * represents significant within group improvement. The clinically meaningful difference in sit‐to‐stand is an increase of >2 for sit‐to‐stand
FIGURE 2.
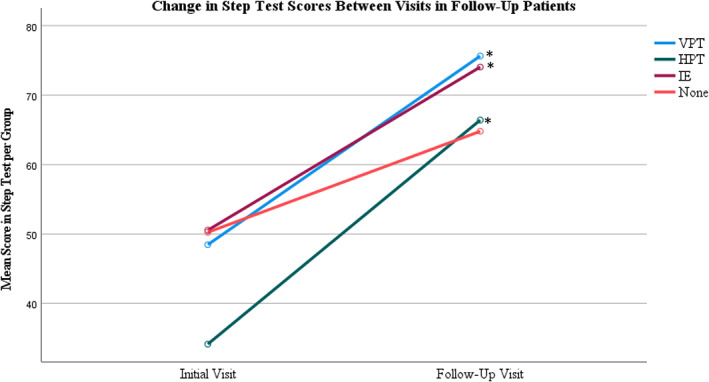
Step Test results of patients who returned for follow‐up. HPT, home in‐person physical therapy; IE, independent exercise; None, referred to physical therapy but did not attend; VPT, virtual physical therapy. * represents significant within group improvement. The clinically meaningful difference for change in step test score is an increase of ≥25%
At the time of the initial visit, 2% of the VPT group and 6% of the IE group had returned to work since their hospitalization. No one in the HPT or none group had returned to work. Of those patients who had returned for follow‐up, 14% of the VPT group and 20% of the HPT group had returned to work. Of the patients who had returned for follow‐up from the IE and no‐exercise groups, none had returned to work.
DISCUSSION
The key finding of this nonrandomized clinical program evaluation is that an outpatient pulmonary rehabilitation program, delivered virtually to patients who had been hospitalized due to COVID‐19, resulted in a clinically meaningful improvement in both lower limb strength and cardiopulmonary endurance after 2 weeks. Furthermore, those patients who underwent a home physical therapy program were found to have a clinically meaningful improvement in lower limb strength after 2 weeks.
At discharge from the hospital, the mean levels of endurance and lower body strength for all patients in this cohort were very low: the scores obtained in the 30‐second sit‐to‐stand test, which primarily measures lower body strength, were similar to those of community dwelling adults aged 80‐90 years. 17 The scores obtained in the 2‐minute step test, which primarily measures endurance, were similar to those for a group of inpatient cardiopulmonary rehabilitation patients and markedly lower than for healthy adults. 21 At 2‐week follow‐up, the patients receiving virtual pulmonary rehabilitation had 30‐second chair stand scores similar to adults aged 60‐64 years, close to the mean age of the study group.
Although not statistically significant, return to work was higher in the groups who received VPT and HPT compared to those who performed IE and no exercise. It could be inferred that patients receiving some form of physical therapy were either more motivated or benefitted specifically from either therapeutic intervention, allowing them to return to work more quickly; however, further research is needed using a randomized trial to determine whether VPT can lead to more rapid return to work. Resting SpO2 was not significantly different between groups at the initial visit or follow‐up; however, within the group who returned for follow‐up, there was a significant pre‐post improvement in SpO2. Lastly, contrary to our initial hypothesis, the baseline levels of cognition and mental health were high, and referrals to psychology or cognitive evaluation were surprisingly rare.
As of December 22, 2020 more than 117,000 people in the United States are currently hospitalized with COVID‐19, an increase of over 40% during the past month and expected to continue to rise all across the country. 5 As this large group of patients recovers from the acute phase of the illness, we expect to see significant residual deficits in strength and cardiopulmonary endurance. A virtual outpatient pulmonary rehabilitation program, which we have previously demonstrated to be feasible to develop and institute rapidly, 13 may be an intervention that is easily adoptable at other centers and would be expected to substantially decrease morbidity related to COVID‐19. If a virtual program is unavailable or too technically challenging, our study also suggests that a home physical therapy program has similar benefits and could also help patients with prolonged COVID‐19 symptoms.
Calls for broad institution of post‐COVID pulmonary rehabilitation programs have been published in Europe 22 based on the expected high burden of impairments following COVID‐19 infection. Our study is the first, to our knowledge, to directly evaluate the clinical outcomes of such a program.
Although pulmonary rehabilitation has been studied and validated mostly as an intervention for COPD, many other lung pathologies are now considered to benefit. 23 Home‐based pulmonary rehabilitation programs have been found to be equivalent to hospital‐ or clinic‐based programs 24 but historically have been deployed mostly in the United Kingdom and Canada, with institutions in the United States having little to no experience with such programs. 25 Our clinical results are broadly in line with those previously reported regarding the success of home‐based cardiopulmonary, stroke, and musculoskeletal rehabilitation programs 26 , 27 , 28 , 29 and the development of this type of program for individuals recovering from COVID‐19 is particularly critical given the current public health recommendations for quarantine and isolation to minimize additional disease transmission. The difficulty of home pulmonary rehabilitation programs in the United States generally revolves around the lack of reimbursement and coverage for such programs. Facilitating our virtual program, was the Coronavirus Preparedness and Response Supplemental Appropriations Act and 1135 waiver authority that was passed on March 6, 2020. This permitted the Centers for Medicare & Medicaid Services to expand telehealth by authorizing Medicare payments at the same rate as in‐person visits, allowing our team to see these patients virtually without concern for reimbursement. It is likely that reimbursement rates for telehealth may be affected after the public health emergency is over, which makes it of upmost importance to study and evaluate patient outcomes after virtual rehabilitation programs for those with cardiopulmonary disease.
Our study has some important limitations. The physician used their evaluation to recommend a treatment plan, and patients were collaboratively involved in this process and had to agree to a treatment plan and assignment to an intervention; thus, there were high levels of self‐selection and bias introduced into the study. Our results reflected the reality of rapidly implementing a clinical program at the height of the initial COVID‐19 surge in New York City. Our current analysis should thus be interpreted with caution as a preliminary pilot program evaluation to inform future research and clinical care. Additionally, 50% of patients were not seen in follow‐up, and loss to follow‐up was highest in the group who did not perform any supervised exercise, which adds bias to our results. One possibility affecting low retention is the natural history of milder disease and in some cases, the rapid improvement in clinical symptoms. Further, the social, environmental, and economic stressors faced by the New York region at this time may have led to a high percentage of dropout. Moreover, limitations also include the lack of randomization to the different intervention groups and the further selection bias this causes; occasional instances of inadequate space within a patient's home to complete the exercise program with an adequate vantage point of the treating therapist; lack of our ability to monitor patients' adherence to the independent exercise program; inability to modify home physical therapy prescriptions as prescribed by discharging medical teams; and possible ceiling effect for clinical improvement because of a lack of exercise equipment in the home to advance the exercise program adequately. Telemedicine also carries limitations by nature. It is reliant on good Wi‐Fi connection for video feed and for the person to be performing the visit in a private space. Intermittent technical difficulties during the video visits occasionally limited the providers' ability to do full exercise assessment and functional outcome testing, which affected our overall data collection.
CONCLUSIONS
A novel, home‐based virtual pulmonary rehabilitation program was developed for adults recovering from COVID‐19 infection and resulted in clinically meaningful improvements in lower body strength and endurance compared with both no exercise and a nonsupervised home exercise program. Additionally, a home physical therapy program was found to have a clinically meaningful improvement in lower limb strength after 2 weeks. Such programs should be feasible to develop and rapidly implement and may serve as a model of care delivery for the large burden of impairment due to COVID‐19 following acute infection. Further study in randomized clinical trials is warranted.
DISCLOSURES
The authors declare no potential conflict of interest.
Supporting information
Supporting information
ACKNOWLEDGMENTS
We thank Samuel Rosenberg, DO, Clark Smith, MD, Rebekah Wallach, PT, DPT, Suzanne Semanson, PT, DPT, Kimberly Stavrolakes MS, PT, Marykathryn Pavol, PhD, Dora Kanellopoulos, PhD, Ian Kronish, MD and Andrea Duran, PhD and all other clinical and departmental staff that worked with us to create and facilitate this program.
Hameed F, Palatulan E, Jaywant A, et al. Outcomes of a COVID‐19 recovery program for patients hospitalized with SARS‐CoV‐2 infection in New York City: A prospective cohort study. PM&R. 2021;13:609–617. 10.1002/pmrj.12578
Dr. Aimee Layton and Dr. Alfred Gellhorn are the senior Co‐authors
REFERENCES
- 1. Carfì A, Bernabei R, Landi F. Persistent symptoms in patients after acute COVID‐19. JAMA. 2020;324(6):603‐605. 10.1001/jama.2020.12603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Garrigues E, Janvier P, Kherabi Y, et al. Post‐discharge persistent symptoms and health‐related quality of life after hospitalization for COVID‐19. J Infect. 2020;81:e4‐e6. 10.1016/j.jinf.2020.08.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Dong E, Du H, Gardner L. An interactive web‐based dashboard to track COVID‐19 in real time. Lancet Infect Dis. 2020;20(5):533‐534. 10.1016/S1473-3099(20)30120-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. NYSDOH. NYSDOH Covid 19 Tracker . https://covid19tracker.health.ny.gov/views/NYS‐COVID19‐Tracker/NYSDOHCOVID‐19Tracker‐Map?%3Aembed=yes&%3Atoolbar=no&%3Atabs=n.
- 5. The COVID‐19 Tracking Project. The Atlantic .
- 6. Kiekens C, Boldrini P, Andreoli A, et al. Rehabilitation and respiratory management in the acute and early post‐acute phase “instant paper from the field” on rehabilitation answers to the COVID‐19 emergency. Eur J Phys Rehabil Med. 2020;56(3):323‐326. 10.23736/S1973-9087.20.06305-4. [DOI] [PubMed] [Google Scholar]
- 7. Simpson R, Robinson L. Rehabilitation after critical illness in people with COVID‐19 infection. Am J Phys Med Rehabil. 2020;99(6):470‐474. 10.1097/PHM.0000000000001443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Rubin R. As their numbers grow, COVID‐19 “long haulers” stump experts. J Am Med Assoc. 2020;324(14):1381‐1383. 10.1001/jama.2020.17709. [DOI] [PubMed] [Google Scholar]
- 9. Li Z, Zheng C, Duan C, et al. Rehabilitation needs of the first cohort of post‐acute COVID‐19 patients in Hubei, China. Eur J Phys Rehabil Med. 2020;56(3):339‐344. 10.23736/S1973-9087.20.06298-X. [DOI] [PubMed] [Google Scholar]
- 10. Bo HX, Li W, Yang Y, et al. Posttraumatic stress symptoms and attitude toward crisis mental health services among clinically stable patients with COVID‐19 in China. Psychol Med. 2020;1‐2. 10.1017/S0033291720000999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Banda JM, Singh GV, Alser O et al. Long‐term patient‐reported symptoms of COVID‐19: an analysis of social media data 2020. doi: 10.1101/2020.07.29.20164418 [DOI]
- 12. Assaf G, Davis H, McCorkell L et al. What does COVID‐19 recovery actually look like? An analysis of the prolonged COVID‐19 symptoms survey by patient‐led research team 2020. https://patientresearchcovid19.com.
- 13. Steere HK, Polich G, Silver JK, et al. Ambulatory rehabilitation of patients hospitalized with <scp>SARS CoV</scp> −2 infections: early pandemic experience in New York City and Boston. PM R. 2020;13:81–86. 10.1002/pmrj.12506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Nasreddine Z.. A short, 5‐minute version of MoCA test. https://www.mocatest.org/the-moca-test/
- 15. Kroenke K, Spitzer RL, Williams JBW, Löwe B. An ultra‐brief screening scale for anxiety and depression: the PHQ‐4. Psychosomatics. 2009;50(6):613‐621. 10.1176/appi.psy.50.6.613. [DOI] [PubMed] [Google Scholar]
- 16. Bisca GW, Morita AA, Hernandes NA, Probst VS, Pitta F. Simple lower limb functional tests in patients with chronic obstructive pulmonary disease: a systematic review. Arch Phys Med Rehabil. 2015;96(12):2221‐2230. 10.1016/j.apmr.2015.07.017. [DOI] [PubMed] [Google Scholar]
- 17. Rikli RE, Jones CJ. Functional fitness normative scores for community‐residing older adults, ages 60‐94. J Aging Phys Act. 1999;7(2):162‐181. 10.1123/japa.7.2.162. [DOI] [Google Scholar]
- 18. Borg GAV. Psychophysical bases of perceived exertion. Med Sci Sports Exerc. 1982;14(5):377‐381. https://pubmed.ncbi.nlm.nih.gov/7154893/. Accessed October 21, 2020. [PubMed] [Google Scholar]
- 19. Zanini A, Crisafulli E, D'Andria M, et al. Minimal clinically important difference in 30 second sit‐to‐stand test after pulmonary rehabilitation in patients with COPD. Eur Respir J. 2018;52:OA5199. 10.1183/13993003.congress-2018.oa5199. [DOI] [PubMed] [Google Scholar]
- 20. Wise RA, Brown CD. Minimal clinically important differences in the six‐minute walk test and the incremental shuttle walking test. J Chron Obstruct Pulmon Dis. 2005;2:125‐129. 10.1081/COPD-200050527. [DOI] [PubMed] [Google Scholar]
- 21. Bohannon RW, Crouch RH. Two‐minute step test of exercise capacity: systematic review of procedures, performance, and Clinimetric properties. J Geriatr Phys Ther. 2019;42(2):105‐112. 10.1519/JPT.0000000000000164. [DOI] [PubMed] [Google Scholar]
- 22. Polastri M, Nava S, Clini E, Vitacca M, Gosselink R. COVID‐19 and pulmonary rehabilitation: preparing for phase three. Eur Respir J. 2020;55(6):2001822. 10.1183/13993003.01822-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Spruit MA, Singh SJ, Garvey C, et al. An official American thoracic society/European respiratory society statement: key concepts and advances in pulmonary rehabilitation. Am J Respir Crit Care Med. 2013;188(8):e13‐e64. 10.1164/rccm.201309-1634ST. [DOI] [PubMed] [Google Scholar]
- 24. Maltais F, Bourbeau J, Shapiro S, et al. Effects of home‐based pulmonary rehabilitation in patients with chronic obstructive pulmonary disease: a randomized trial. Ann Intern Med. 2008;149(12):869‐878. 10.7326/0003-4819-149-12-200812160-00006. [DOI] [PubMed] [Google Scholar]
- 25. Thomas RJ, Beatty AL, Beckie TM, et al. Home‐based cardiac rehabilitation. J Am Coll Cardiol. 2019;74(1):133‐153. 10.1016/j.jacc.2019.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Cramer SC, Dodakian L, Le V, et al. Efficacy of home‐based Telerehabilitation vs in‐clinic therapy for adults after stroke: a randomized clinical trial. JAMA Neurol. 2019;76(9):1079‐1087. 10.1001/jamaneurol.2019.1604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Prvu Bettger J, Green CL, Holmes DJN, et al. Effects of virtual exercise rehabilitation in‐home therapy compared with traditional care after Total knee Arthroplasty: VERITAS, a randomized controlled trial. J Bone Joint Surg Am. 2020;102(2):101‐109. 10.2106/JBJS.19.00695. [DOI] [PubMed] [Google Scholar]
- 28. Paneroni M, Colombo F, Papalia A, et al. Is telerehabilitation a safe and viable option for patients with COPD? A feasibility study. J Chronic Obstr Pulm Dis. 2015;12(2):217‐225. 10.3109/15412555.2014.933794. [DOI] [PubMed] [Google Scholar]
- 29. Chan C, Yamabayashi C, Syed N, Kirkham A, Camp PG. Exercise telemonitoring and telerehabilitation compared with traditional cardiac and pulmonary rehabilitation: a systematic review and meta‐analysis. Physiother Can. 2016;68(3):242‐251. 10.3138/ptc.2015-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supporting information


