Abstract
The purpose of this integrative review is to examine recent literature on the intersection of SARS‐CoV‐2 (COVID‐19 novel coronavirus) and climate change that will lead to a greater understanding of the complexities of the urgent pandemic linked with the emerging climate crisis. A literature search for peer‐reviewed, English language, literature published since the pandemic emerged was conducted using Cumulated Index to Nursing and Allied Health Literature (CINAHL), PubMed, and the Cochrane Library. The final sample yielded a total of 22 commentaries, editorials, discussion papers, and a research study that explicitly addressed the intersection of COVID‐19 and climate change. Sixty articles emerged in the initial review of the intersection of the COVID‐19 pandemic and climate change with the final yield of 22 articles deemed valid for inclusion after full text review. With the emergence of COVID‐19 and scholarly discourse that addresses the intersection of the pandemic with climate change, key issues emerged that intersect with policy /advocacy, social justice, and nursing's public health role in clinical practice, education, policy/advocacy, and research/scholarship. Five themes that emerged included the role of public health in COVID‐19 and climate change efforts; global approach addressing human‐environment issues; intersection of COVID‐19 and climate change from a community and global perspective; impacts of COVID‐19, climate change and the environment and professional associations and specialty organizations’ views and responsibilities with a lens on COVID‐19 and climate change. Despite the importance of addressing racial inequities as well as systemic and structural racism that impacts those most affected by climate change and pandemics such as COVID‐19, no literature addressed this topic. Public health nursing has a critical role in addressing climate change and the pandemic response to COVID 19 in the 21st century.
Keywords: climate change, COVID‐19, global warming, SARS‐CoV‐2
1. INTRODUCTION
As the nursing profession addresses the complexity of SARS‐CoV‐2 also known as the novel coronavirus disease 2019 (COVID‐19), public health concerns regarding the intersection of climate change and emerging pandemics are an urgent problem in the 21st century. As noted by Rosenbloom and Markard (2020), the climate crisis as well as COVID‐19 are global and unprecedented disruptors and require comprehensive and coordinated responses by policy‐makers, businesses, broader society—and to this, we urge the inclusion of public health professionals. Ivanova et al. (2012) has suggested that climate change and pandemics may individually and collectively amplify a cascade of global challenges and potential economic collapse. Further Rosenbloom and Markard (2020) suggested that the pandemic directly threatens individuals, populations, and health systems, while climate change undermines broader natural, ecological, human systems, and populations. From a global perspective, it is well established that climate change represents a looming health emergency with Lancet and Intergovernmental Panel on Climate Change reports on climate change and health contributing to our current state of the science and understanding of the deleterious health consequences associated with climate change (Intergovernmental Panel on Climate Change, 2018; Watts et al., 2019). There is a pressing need for health professionals to galvanize the response to both of these challenges for the health of the world's people. The purpose of this integrative review is to examine the intersection of climate change and COVID‐19.
While the threat of COVID‐19 is urgent for individual, community, population, and global health, climate change is more insidious in its impact and a slow march to progressively worsening human health. Nursing has a pivotal role in addressing climate change, climate justice, and health. In our institution at the MGH Institute of Health Professions School of Nursing, the first school of nursing‐led Center for Climate Change, Climate Justice, and Health was established to address the deleterious health consequences of climate change and the critical need for health professions education. Literature suggests that education of all of the health professions is integral to address the leading public health challenge of our time; in health professions education curriculum development, integration of climate change knowledge in clinical practice, policy/advocacy efforts, and research and scholarship about climate and health are key areas for the future (Maxwell & Blashki, 2016). In the midst of the COVID‐19 pandemic, it is important to leverage both climate change and associated pandemics to address the future of public health in the 21st century. From a nursing professional lens from the International Council of Nurses, Catton (2020) notes:
The next decade is likely to produce any number of global challenges that will affect health and health care, including pannational infections such as the new coronavirus, COVID‐19 and others that will be related to global warming (p. 4).
2. OVERVIEW OF THE INTERSECTION OF CLIMATE CHANGE AND COVID‐19
It is well known that animals including bats are reservoirs for several viruses and were a conduit for the Ebola epidemic as well as severe acute respiratory syndrome (SARS) Coronavirus 1, Middle Eastern Respiratory Syndrome (MERS), and the emergence of COVID‐19 (Hemida & Ba Abduallah, 2020). Habitat disruption is the main driver of loss of biodiversity, and climate change may play a role by forcing species to shift habitat and changing geographical range of species (Bale, 2020; Xiao et al., 2020). As species shift habitats, this brings animals in closer range to humans and livestock which then serve as a vehicle for launching a global pandemic. Even more extreme conditions existed in Wuhan, China, the epicenter of the COVID‐19 pandemic, where bats and pangolins—with pangolins recently emerging as vectors for transmission of viruses—are suggested as vectors for coronaviruses since they are housed in crowded, open markets with close and often squalid conditions (Bale, 2020; Xiao et al., 2020). Pangolins are similar to bat species as mammals that are known to be able to be infected with viruses such as coronaviruses (Bale, 2020; Morens et al., 2020; Xiao et al., 2020). Emerging evidence may support that in our climate‐changing world, there is encroachment on animal habitats which may impact health and risk for infectious diseases; thus there is a need for urgent efforts to limit climate change to address the emergence of new pandemics in the future (Bernstein, 2020).
As discussed by Schwartz (2020), the intersection of climate change and COVID‐19 has emerged as the most complex and threatening public health challenge ever encountered—surpassing the Influenza Pandemic that emerged in 1918 when environmental degradation had not yet accelerated. Further Schwartz suggests:
The question that haunts my mind is, how would the United States handle such a pandemic outbreak if it occurred as the coronavirus did in China, just as some kind of major climate change crisis was also stressing the American healthcare system. Are we prepared? I don't think so, do you? The reality is that not only America but the world is utterly unprepared for these outbreaks, and when one adds the migrations that climate change will compel things look very bleak indeed (p. 141).
Global Environmental Health Day was held on July 1, 2020 and Columbia University's Earth Institute released a State of the Planet report on COVID‐19’s Long‐Term Effects on Climate Change—For Better or Worse (Cho, 2020). Furthermore, because of recommendations for lockdowns, social distancing, and work from home advisories, significant decreases in transportation occurred globally and limited industrial activity resulted in a 17% decrease in daily carbon emissions in April (Cho, 2020). Cho's commentary suggested that there have been opportunities to both improve and detract from improving public health in the time of COVID‐19 with a lens on climate change. Areas of concern included plans to withdraw from the Paris Climate Accord of 2015, delays in international negotiations regarding climate change and the planned climate meeting of November 2020, deforestation in the Amazon accelerating during the pandemic, weakening of climate policies in the US and rollback of US measures. Additional areas of concern identified by Cho are disruption of science research during the pandemic, less funding for climate resilience and renewable energy, and an increase in use of plastic to prevent spread of COVID‐19. However, Cho notes that there are areas of improvement amidst COVID‐19 that may positively impact public health including a green recovery in other countries with funding for renewable energy sources, more biking and walking as a COVID/climate change co‐benefit, less international travel since transportation represents 23% off global carbon emissions and 11% reduction by aviation (Cho, 2020). It is important to note that the pandemic has led to simpler living and increased engagement of many in the important role of science in both public health and pandemic response.
Wu et al. (2020) at the Harvard School of Public Health also suggested that air quality may impact severity of illness in COVID‐19. They found that long‐term exposure to fine particulate matter has been associated with a 15% increase in the COVID‐19 death rate, even after controlling for other health conditions. Although this study did not explicitly link air quality with climate change, further research is needed on this important linkage. In the United States, we have also seen significantly higher rates of COVID rates and COVID morbidity and mortality among Blacks and Hispanics (Price‐Haywood et al., 2020). Racial and ethnic minorities are more likely to reside in communities with higher rates of pollution and particulate matter (Mikati et al., 2018). The high rate of COVID mortality in these communities has been attributed to pre‐existing conditions including respiratory illness and poor access to high quality care, but it does appear that climate change may also play a role in the etiology of poor air quality and increasing these disparities.
Manzanedo and Manning (2020) analyzed the intersection of COVID‐19 and the urgent climate crisis addressing the unique areas of overlap and differences between the two crises and the key lessons that can be learned. These lessons include “high momentum trends; irreversible changes; social and spatial inequality; weakening of international solidarity, and less costly to prevent than to cure” (p. 1). Notably, they view one critical difference: since the COVID‐19 pandemic emerged rapidly while the climate crisis has had a decades‐long emergence with a looming crisis by 2030 if urgent action is not taken. Regarding lessons of COVID‐19 and climate change, high momentum trends also identified as time lags refer to the delayed response to the pandemic and to climate change science. The authors noted that ignoring calls to action are costlier in the long run. Irreversible changes are pressing for the climate crisis since unless greenhouse gases are reduced, there will be planetary changes that are irreparable with significant damage that may negatively impact health. Social and spatial inequality refers to aspects of social determinants of health including poverty, inequity between wealthy and poor nations, lack of access to care by many of the world's people, and increased risk by race/ethnicity for black/brown populations. This is significant for both COVID‐19 whereby African‐American and Hispanic populations are disproportionately affected by the pandemic in the US and have significantly poorer outcomes (Azar et al., 2020). The weakening of international solidarity since the Paris Agreement and the US withdrawal from the treaty is another key area of international weakening in the global commitment to address climate change. The fact that both the pandemic and climate change are less costly to prevent rather than to cure is a significant outcome of both challenges that we face. As Kerry (2020) wrote “climate change and COVID‐19….[are] truly the tale of two pandemics deferred, denied, and distorted, one with catastrophic consequences [COVID‐19], the other with even greater risk if we don't reverse course [climate change]” (p. A8).
3. METHODS
A search for peer‐reviewed, English language, literature published in the scientific literature since the pandemic emerged in 2020 was developed using the following databases: Cumulative Index for Nursing and Allied Health (CINAHL), Pubmed, and the Cochrane Library. Search terms used were “climate change,” “global warming,” “pandemic,” “SARS‐CoV‐2,” and “COVID‐19.” Only articles published during 2020 were included since the COVID‐19 epidemic globally emerged in late 2019 with the eruption of the pandemic in January to February 2020. In the initial review process, article titles and abstracts were reviewed for relevance for inclusion. Subsequently full text of the initial review was conducted by two authors to determine relevance based on the inclusion criteria. Exclusion criteria were aimed at limiting any articles that did not address COVID‐19 and its intersection with climate change. The review of articles was conducted with literature published between January 2020 and June 2020. These articles represented the early emerging literature of the intersection of COVID‐19 and climate change. Two reviewers conducted independent full text article reviews and inclusion was determined based on the question: What does the literature indicate regarding the intersection of COVID‐19 and climate change? Each reviewer determined themes independently and subsequently consulted on final emergent themes. The article selection process is presented in the Preferred Reporting Items of Systematic Reviews and Meta‐Analyses (PRISMA) flow diagram (Figure 1) and the PRISMA Scoping Review Checklist for Quality Assessment (Figure 2) to support the inclusion of the 22 articles of which 21 were discussion papers or commentaries and only one was a research‐based paper.
FIGURE 1.
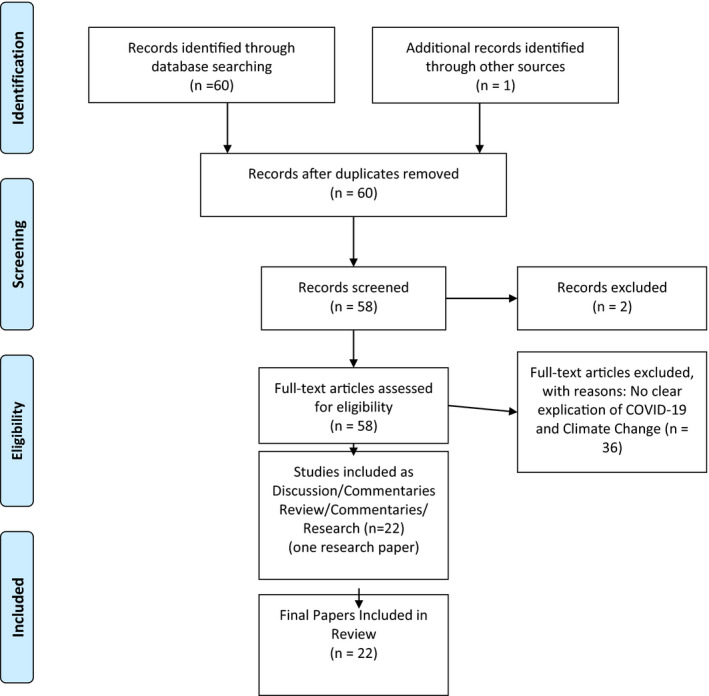
PRISMA 2009 flow diagram for review of the intersection of COVID‐19 and climate change [Color figure can be viewed at wileyonlinelibrary.com]
FIGURE 2.
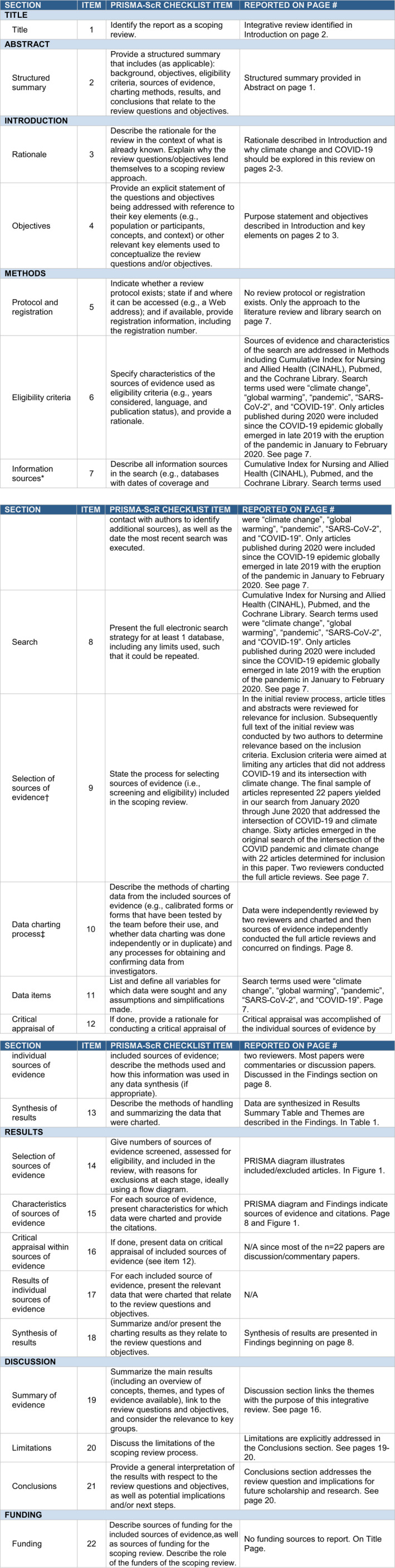
Preferred reporting items for systematic reviews and meta‐analyses extension for scoping reviews (PRISMA‐ScR) checklist: climate change in the era of COVID‐19 [Color figure can be viewed at wileyonlinelibrary.com]
4. FINDINGS
The results of this integrative review represent the key insights, findings, and themes from the selected articles, as detailed in Table 1. Five themes, based on two independent reviews, emerged from the papers that were selected for inclusion: role of public health in COVID‐19 and climate change efforts; global approach addressing human‐environmental issues; COVID‐19 and climate change from a community and global health perspective; environmental impacts of COVID‐19 and climate change and built environment; and professional associations’ and specialty organizations’ views and responsibilities with a lens on COVID‐19 and climate change.
TABLE 1.
Results summary
| Author, date, discipline | Evidence type | Theme | Findings |
|---|---|---|---|
| Amuasi, J. H., Lucas, T., Horton, R., Winkler, A. S., 2020, Public Health | Commentary/Perspective | Intersection of climate change and COVID−19 from community and global experience | The Lancet One Health Commission addressed the shared environment and the importance of the animal‐environment‐human interface in our climate‐changing world. |
| Armitage, R., Nellums, L. B., 2020, Public Health | Commentary/Correspondence | Intersection of climate change and COVID−19 from community and global experience | Access to water is critical particularly for handwashing, with special needs for water‐stressed settings. |
| Bell, D., Aronoff‐Spencer, E., 2020, Global Public Health | Commentary/Perspective | Global approach addressing human‐environment issues | There is a need to reframe global health to consider emerging infectious diseases with the understanding of the interconnectedness of the world's people. |
| Benjamin, G., 2020, Public Health | Commentary/Analysis | Role of Public Health in COVID−19 and Climate Change Efforts | The practice environment for public health is key as is addressing social determinants of health and a strong public health infrastructure. |
| Catton, H., 2020, Nursing | Commentary/Perspective | Role of Public Health in COVID−19 and Climate Change Efforts | The pandemic represents a public health emergency of international concern and the World Health Organization and the International Council of Nurses are engaged in addressing this global health challenge. |
| Coates, S., Andersen, L. K., & Boos, 2020, Professional association role in COVID−19 and climate | Commentary | Professional associations and specialty organizations addressing COVID−19 and climate change | This paper addresses the critical importance of balancing public health and lessons from climate inaction from the lens of the International Society of Dermatology Climate Change Committee. |
| Goyman, W., 2020, Biodiversity, climate, and human activity | Commentary/Editorial | COVID−19, climate change, and environment | The COVID−19 pandemic, climate change and the crisis of biodiversity offer opportunities for lessons regarding our global efforts against COVID and climate change. |
| Haines, A., Falceto de Barros, E., Berlin, A, Heymann, D. I., & Harris, M. J., 2020, Public Health/Community Health | Commentary/Perspective | Intersection of climate change and COVID−19 from community and global experience | The authors urge that a national program of community health workers be developed for a UK program of community health workers to address COVID−19 in our climate‐changing world. |
| Helm, D., 2020, Environment and Economics | Discussion paper | COVID−19, climate change, and environment | COVID−19 environmental impacts should be addressed in our climate‐changing world. These authors address five questions: short‐term impacts of emissions, natural environmental and environmental policy, longer‐term consequences from deployment of monetary and fiscal stimuli, and consequences from deployment of stimuli. In addition, there is investment in green deals, possible further deglobalization and its impact on climate change, intergenerational impacts, and behavioral changes which may be positive or negative on the environment. |
| Herrero, M., Thornton, P., 2020, Public Health | Commentary/Correspondence | Intersection of climate change and COVID−19 from community and global experience | COVID−19 presents lessons about responding to climate change and behavioral responses to global challenges are required. |
| Jin, S., 2020, COVID−19 and Environment | Commentary | Global approach addressing human | This editorial reports on the key lessons from their work including: We are all in this together; we must act now before it is too late; science and facts matter; innovation is key; international collaboration is key; and respect of our environment and planetary health is critical. |
| Jowell, A., & Barry, M., 2020, Medicine, Global Health | Commentary/Perspective | Global approach addressing human‐environment issues | Societies must adopt a “planetary health lens” to engage in pandemic response. |
| Li, Li, Huang, Wang, Zhu, Zu et al., 2020, Biodiversity, climate, and human activity | Quantitative modeling of air quality during COVID−19 lockdown in China | COVID−19, climate change, and environment | Although the COVID−19 pandemic has limited greenhouse gas emissions and air pollution, there is a need to address reductions in air pollution and industrial strategy to have a comprehensive air pollution plan. |
| Lorentzen, H. F., Benfield, T., Stisen, S., & Rahbek, C., 2020, Medicine | Commentary/Correspondence | Global approach addressing human‐environment issues | The United Nations Climate Conference (COP 25) focused on urgently needed climate adaptations. With the emergence of the COVID−19 pandemic, it is essential to address anthropogenic biodiversity. |
| Manzanedo & Manning, 2020, Climate change and environment | Discussion paper | Global approach addressing human‐environment issues | These authors examine the intersection of COVID−19 and the urgent climate crisis addressing the unique areas of overlap and differences between the two crises and the key lessons that can be learned. These lessons include “high momentum trends; irreversible changes; social and spatial inequality; weakening of international solidarity, and less costly to prevent than to cure” (p. 1). |
| Morrison, L., 2020, Lessons from former executive secretary UN Framework Convention on Climate Change | Commentary/Viewpoint | Professional associations and specialty organizations addressing COVID−19 and climate change | Morrison examines the lessons from the former executive secretary of the UN Framework Convention on Climate Change and that five major lessons are apparent. |
| O’Reilly, K. M., Auzenbergs, M., Jafari, Y., Liu, Y., Flasche, S., & Lowe, R., 2020, Public Health | Commentary | Intersection of climate change and COVID−19 from community and global experience | Effective transmission of COVID−19 may be related to climate and requires further investigation. |
| Patruno, C., Nistico, S., Fabbrocini, G., Napolitano, M., 2020, Dermatology, climate change, and COVID−19 | Commentary | Professional associations and specialty organizations addressing COVID−19 and climate change | Patruno and colleagues examine whether climate change is the next pandemic for dermatology with lessons from COVID−19. |
| Rosenbloom, D., & Markard, J., 2020, Public Health, Global Health | Commentary/Editorial | Global approach addressing human‐environment issues | COVID−19 may represent an opportunity to mitigate health and other challenges related to climate change. |
| Rutz, Loretto, Bates, Davidson, Duarte, Jetz et al., 2020, Biodiversity, climate change and human activity | Commentary | COVID−19, climate change, and environment | These authors note that the COVID−19 quarantine/lockdown offers opportunities for researchers and scholars to examine human activity and planetary health. |
| Schwartz, S. A., 2020, Environmental Health/Public Health | Discussion Paper | Intersection of climate change and COVID−19 from community and global experience | In our global world, we are poorly prepared for pandemic outbreaks and with climate change migration, there are complex challenges ahead. |
| Shankar, H. M., Ewart, G., Garcia, E., Hicks, A., & Hardie, W., 2020, American Thoracic Society, COVID−19, and climate change | Discussion paper | Professional associations and specialty organizations addressing COVID−19 and climate change | The American Thoracic Society presents a position statement on COVID−19, climate change, and shared responsibility of their professional organization related to COVID and climate change. |
5. THEME 1: ROLE OF PUBLIC HEALTH IN COVID‐19 AND CLIMATE CHANGE EFFORTS
There are important implications for addressing public health with the intersection of COVID‐19 and climate change. Since the early influence of Florence Nightingale as we celebrate the 200th year of her birth in 2020, the environment has been critically important in public health. Nightingale's nursing philosophy and pioneering efforts were steeped in environmental nursing principles which are as relevant in the 21st century as when she first launched her prescient ideas. Further the 2020 State of the Science Congress on Nursing Research meeting of the American Academy of Nursing focused on The Environment's Impact On Health, with relevance for Nightingale's environmental principles and the challenges of climate change and health. Not since the 1918–1919 influenza pandemic—widely known as the Spanish flu, has the intersection of environment and health been viewed as so profound. It is interesting to note that the COVID‐19 pandemic emerged during the Year of the Nurse 2020, a celebration of Florence Nightingale and her contributions to nursing and public health. Nightingale's contributions to addressing clean air, water, and light also offer unique contributions unlike any pandemic witnessed in over 100 years. This requires that public health professionals and climate change advocates address this complex situation with the intersection of climate change and associated deleterious health consequences.
It is clear that the threat‐amplifying effects of the intersection of COVID‐19 and climate change require a cohesive, coordinated, and comprehensive response from public health professionals and particularly public health nurses who are at the forefront of care. The response to COVID‐19 demonstrates that a comprehensive approach that is embodied in the principles of public health practice is key. This pandemic response has resulted in grave concerns about the possibilities of a pandemic response intersecting with a climate change emergency (Catton, 2020). Disasters that are occurring due to greenhouse gas emissions such as air quality issues, hurricanes, flooding, wildfires, heat stress, and heat stroke due to increasing ambient temperatures, and increased vector‐borne illnesses should be considered amidst the COVID‐19 pandemic. Although greenhouse gas emissions have decreased during the COVID‐19 pandemic, it is important to consider resurgence of these emissions post COVID‐19 that are likely to occur globally.
One article by Benjamin (2020) supported this theme and offered a recent opinion and analysis. As current president of the American Public Health Association, Benjamin noted that the recent COVID‐19 pandemic has not only stressed public health systems in countries globally, but also has further uncovered gaps in health care for those deeply affected by poorer social determinants of health. It is important to note that both COVID‐19 and climate change disproportionately affect disadvantaged populations with climate change affecting those who least contribute to greenhouse gas emissions. Benjamin noted: “tragically, underserved and vulnerable populations are being disproportionately affected, just as they are by most health threats” (p. 3). Healthy People 2020 (Centers for Disease Control & Prevention [CDC], 2020) adopted the view of the social determinants of health in five domains that include economic stability, education, health and health care, neighborhood and built environment, and social and community context. The social determinants of health have broadly included race/ethnicity; however the concepts of racism and structural/systemic racism were identified and linked due to the overwhelming deleterious impacts on health in COVID‐19 and health impacts of climate change as noted in Benjamin's (2020) commentary.
A second discussion paper by Catton (2020) identified pan‐national challenges such as COVID‐19 and potentially other emerging infectious diseases and pandemics in our warming planet. He noted the critical message of the International Council of Nurses’ position statement on Nurses, Climate Change, and Health which addressed the role of nurses globally in engaging in the critical public health issues that have emerged due to climate change. In addressing the emergent nature of the COVID‐19 pandemic and its intersection with public health and climate change, Catton (2020) suggested that the next decades of the 21st century have looming geopolitical and environmental challenges that affect public health systems, health care infrastructure, and the nursing workforce.
6. THEME 2: GLOBAL APPROACH ADDRESSING HUMAN‐ENVIRONMENTAL ISSUES
Several articles noted that there is an important role for understanding the intersection of planetary health and the human‐environment relationship. Jowel and Barry (2020) suggested that there are interconnected elements between health and environmental systems that should be viewed from a planetary health perspective. Their perspective aimed to address the encroachment of humans on natural systems and the impact of climate change on the emergence of pandemic diseases in the era of COVID‐19. Further they identified key aspects of a planetary health approach that focused not only on specific nations but addressing cross‐national borders. Further, Jowell and Barry (2020) suggested that:
COVID‐19 is not the first example of an emerging zoonotic infection that has devastating impacts on global human health. In recent decades, humans have altered surrounding habitats and increased deforestation to make room for growing populations, extract natural resources, and build farms (p. 1).
They conclude that close human‐environment habitats related to shifts in land use and forestry, increases in populations and population density are potentially lethal conduits for future pandemics.
Bell and Aronoff‐Spencer (2020) offered their commentary regarding global health in the pandemic era. They addressed the importance of nongovernmental organizations, multilateral institutions, and engaging a fully global view to engage to address the challenges of COVID‐19. Furthermore, they examined how climate change, social unrest, emerging pandemics such as COVID‐19 may impact health threats and global health funding and capacity. They suggested that:
the current novel coronavirus disease (COVID‐19) pandemic underlines the interconnectedness of health globally and the risks to all of us of maintaining inequalities in health capacity and infrastructure (p. 1,175).
Lorentzen and colleagues offered their views on COVID‐19 as a consequence of a biodiversity crisis related to climate change (Lorentzen et al., 2020). With habitat destruction and climate change, they suggested that the biodiversity crisis will accelerate as the main driver of our current and future emerging pandemics. They also noted that the emergence of COVID‐19 may be only the beginning of the emergence of novel coronaviruses and other infectious diseases that will affect humans, livestock, birds, marine life, and other organisms in the 21st century.
Furthermore, as Rosenbloom and Markard (2020) suggested regarding the intersection of climate change and COVID‐19 from a planetary health perspective:
we are witnessing how worldwide lockdowns have decreased air pollution and greenhouse gas emissions because of reduced transportation, electricity generation, and industrial production. This shows how intertwined modern economic life and fossil fuels have become, and suggests consideration of climate implications in economic recovery plans (p. 447).
7. THEME 3: COVID‐19 AND CLIMATE CHANGE FROM A COMMUNITY AND GLOBAL HEALTH PERSPECTIVE
Theme 3 offers a unique lens on COVID‐19 and climate change from a community and global health perspective that differs from other themes in that the discussion papers focus on global responses including from the World Health Organization and offering unique global perspectives. This theme also focuses on suggested interventions to address community and global emergencies and emergency workforce approaches through community health approaches. Haines, Falceto de Barros, Berlin, Heymann, and Harris (2020) discussed the importance of community health workers in COVID‐19 response. Their commentary proposed a large scale emergency program to engage community health workers for care of vulnerable populations in the UK based on the World Health Organization response and suggested that “young people in the range of 18–30 years deemed at lower risk of acquiring serious consequences from the pandemic exposure should offer a coordinated community workforce in the pandemic” (p. 1,174). Armitage and Nellums (2020) focused on the importance of water in the era of climate change and COVID‐19 and examined the importance of access to fresh water for regular handwashing during the pandemic. They further urged that fresh water be provided free of cost to engage populations in hygiene recommendations and to limit spread of COVID‐19. As they suggested, access to water is inextricably linked with climate change and integrally related to limiting the spread of the current pandemic.
A commentary by Herrero and Thornton (2020) inquired: “What can COVID‐19 teach us about responding to climate change?” (p. e174). Their most important lesson is that investment in behavioral responses such as social distancing and engagement of governments, businesses, and resource mobilization can be achieved and may limit the spread of the pandemic. They noted that “governments have found $8 trillion to help combat the spread and effects of COVID‐19 in just 10 weeks” (p. e174) and that these same aggressive measures should be applied with the same urgency to climate change. O’Reilly et al. (2020) examined the transmission across the globe and the role of climate in mitigation of the current pandemic. They discussed the importance of future studies on climate variability, air pollution, heat and humidity in the incidence, susceptibility, and surveillance of COVID‐19 related disease. Further Amuasi and colleagues (2020) examined the interconnection of The Lancet One Health Commission with climate change and COVID‐19. They also suggested a linkage with the United Nations Sustainable Development Goals and the approach of the One Lancet Health Commission which includes the animal—environment—human interface. Their goal is to enhance health within an environment shared by humans and animals in our climate‐changing world. Schwartz (2020) urged greater preparedness and consciousness about climate change and COVID‐19 and the need for understanding of what climate change migration will bring to the landscape of current and future pandemics. Rosenbloom and Markard (2020) offered a lens on COVID‐19 recovery for our struggling climate and planet. One outcome may be that there are opportunities to catalyze change on climate change for communities, nations, and globally as we address the COVID‐19 pandemic.
8. THEME 4: COVID‐19 AND CLIMATE CHANGE AND THE ENVIRONMENT
Environmental impacts of COVID‐19 and climate change are another theme that emerged in this review. Helm (2020) addressed the impacts of the pandemic virus and suggested an agenda for research. The agenda included five sets of questions: examining the short‐term impacts on emissions, the natural environment, and the need to address environmental policies; the importance of the 26th UN Climate Change Conference of the Parties (COP 26); long term consequences of the financial impact of climate change and COVID‐19; investment in green opportunities and legislation; deglobalization related to climate change and pandemics; debt and burden of pollution on future generations; and positive and negative behavioral changes related to the pandemic and climate change (Helm, 2020).
Keenan (2020) focused on resilience and the built environment in the era of COVID‐19 and our climate‐changing world. The physical and social environment in which individuals, communities, and populations reside in the 21st century in the midst of the current pandemic and climate change are important to examine. Their recommendations are that current COVID‐19 responses yield important efforts for future resilience designs in the built environment as well as frameworks and practices to address community health amidst climate change with lessons learned. Jin (2020) described the importance of renewable energy research to address the intersection of climate change and COVID‐19. The focus was on a message of we are all in this together and the time to act is now. Jin noted that “a pandemic and climate change are both existential challenges facing the whole human race who share this planet together. Neither Coronavirus nor climate see country borders” (p. 1709). Other key messages offered by Jin are that it is essential to act now before it is too late; that science and facts matter; that international collaboration is critical; and we must respect mother nature.
Goymann (2020) discussed the COVID‐19 pandemic and its intersection with climate change and the biodiversity crisis, thus fitting with Theme 3 on climate change and the environment; however Goymann's commentary also overlaps with Theme 2—Global Approach Addressing Human‐Environmental Issues. The commentaries by Helm (2020) and Goymann (2020) are two examples that offer key themes that also overlap with other themes.
Goymann (2020) suggested that the pandemic offers opportunities for governments across the globe to address the urgent challenges and to listen to scientists to address carbon emissions to eliminate biodiversity loss. Similarly, Rutz and colleagues describe the opportunities for researchers to examine the impacts of COVID‐19, climate change, and the effects of human activity. They described the great pause during the COVID‐19 pandemic and critical importance of engaging in climate change action. In the sole research article found in this integrative review of the intersection of climate change and COVID‐19, Li and colleagues (2020) studied air quality changes during the COVID‐19 lockdown in the Yangtze River Delta Region of China. They offered insight into the impact of human activity and air pollution and suggested that national lockdown policies in China resulted in significantly reduced air pollutant emissions with improved air quality. Furthermore, they found that human activities—which contribute to greenhouse gas emissions and air pollution—were limited with a resulting improvement in climate change related impacts such as air quality.
9. THEME 5: PROFESSIONAL ASSOCIATIONS’ AND SPECIALTY ORGANIZATIONS’ VIEWS AND RESPONSIBILITIES WITH A LENS ON COVID‐19 AND CLIMATE CHANGE
Although relatively few professional associations and specialty organizations have addressed the intersection of climate change and COVID‐19, Coates and colleagues (2020) examined the critical role of advancing public health and climate action from the perspective of the International Society of Dermatology's Climate Action Committee. They urged a wake‐up call for the convergence of climate change and COVID‐19 and meaningful action for both of these global health crises. The American Thoracic Society (ATS) discussed the importance of shared responsibility in engaging in action to confront COVID‐19 and climate change (Shankar et al., 2020). The primary focus was on air travel and its impact on the environment and as a reservoir of COVID‐19 infection. Their position statement was aimed at urging individuals to fly less, fly more efficiently, purchase carbon offsets, and address other sources of waste at conference attendance. As a society aimed at addressing lung health, the ATS’s commentary was a critical viewpoint on opportunities to address our current pandemic and an urgent climate change agenda. Furthermore, Morrison (2020) also urged that general practitioners examine the importance of COVID‐19 in our climate‐changing world. Morrison's lens was based on an understanding of health and social inequalities during the current pandemic; the author also suggested that there is a need for progressive and comprehensive actions to assure health equity in pandemics and amidst climate change. The findings of Morrison (2020) fit within this theme of the role of professional organizations, but also overlap with Theme 2 Global Approach Addressing Human‐Environmental Issues. Finally, Patruno and colleagues (2020) offered a commentary regarding the intersection of climate change, COVID‐19 and dermatology. They suggested that telehealth has emerged as a key way to provided health care to reduce contacts and discussed the influence climate change has on dermatological conditions such as cancer in our climate‐changing world.
10. DISCUSSION
The themes that emerged from this integrative review of the intersection of COVID‐19 and climate change suggested that public health professionals—including public health nurses have important roles in addressing the current pandemic and the climate change‐related health consequences that are already occurring. Further the second theme and the literature that supported this theme indicated that there is a global role for addressing human‐environment challenges. The third theme offered a lens on both a community and a global perspective on COVID‐19 and climate change. Theme four supported the environmental impacts that uniquely occur due to both COVID‐19 and climate change health consequences, which included a focus on the built environment. Finally, the fifth theme addressed the roles of professional associations’ and specialty associations’ views and responsibilities with a lens on COVID‐19 and climate change.
11. PUBLIC HEALTH NURSING IN THE ERA OF COVID‐19 AND CLIMATE CHANGE
Public health nurses have unique and essential roles in addressing COVID‐19 and the urgent challenge of climate changes. There are important nursing roles in clinical practice integrating climate change knowledge in the assessment and care of individuals, families, communities, and populations. It is critical to educate all those whom for whom public health nurses provide care, however there are key distinctions in that vulnerable and marginalized populations are disproportionately affected by morbidity and mortality in the COVID‐19 pandemic. Thus it is essential for public health nurses to educate those whom they serve regarding the acute and chronic impacts of climate change amidst the COVID‐19 pandemic; this is critical due to the complex intersection of overlapping health challenges that may occur in our current crisis. Furthermore, vulnerable and marginalized populations are also disproportionately affected by the deleterious consequences of climate change. Exposure to poor air with associated respiratory challenges such as asthma leads to higher morbidity and mortality, particularly in pediatric populations and those with co‐morbid chronic illnesses. Sharing public health knowledge with individuals, families, communities, and populations about the emergence of pandemics, the intersection with climate change, and that infectious diseases are more likely to emerge in our climate‐changing world are key roles for public health nurses.
Education of public health nurses to address pandemic care and response in the era of climate change is essential in the pre‐licensure, graduate, and doctoral levels of education. Health professionals also require ongoing continuing education about the emergence of pandemics, the care of patients, and the education of individuals, families, communities, and populations. There are enormous challenges that we face in addressing health of the world's people as natural habitats are destroyed and wildlife encroaches on areas where populations reside. Education is key in addressing the health challenges confronted related to pandemics such as COVID‐19 in our climate‐changing world.
Policy and advocacy efforts are among the most essential areas where public health nurses can engage in addressing pandemics and climate change in the 21st century. Working with local, state, and national legislatures and governing bodies are important venues to bring concerns about climate change and its intersection with pandemic emergence and response. It is important to be aware key initiatives of global organizations such as the United Nations (UN) since they have also promulgated the UN Sustainable Development Goals (UN SDGs) which include Goal 13 aimed at Climate Action.
Furthermore, public health nurses’ efforts should also address social justice and climate justice, as well as key issues related to pandemic preparedness and response. Where do social justice and climate justice intersect in the age of COVID‐19? The mission of social justice is integrally tied to the mission of public health (Gostin & Powers, 2006). Widely viewed as embedded in public health practice, social justice—the idea that benefits and burdens should be equally distributed within a society—is embedded in the efforts that were espoused by Beauchamp (1999) and Powers and Faden (2006). The intersection of public health as well as social justice and climate justice are key principles for advancing the health of the world's people. The World Health Organization's Commission on Social Determinants of Health (2008) stated that: “social justice is a matter of life and death. It affects the way people live, their consequent chance of illness, and their risk of premature death” (p. 3).
Many of the groups that have been identified as most vulnerable to the health impacts of climate change have emerged as being equally vulnerable to the most deleterious effects of COVID‐19. This overlap occurs with certain communities of color, indigenous populations, the very young, and older adults as well as people with chronic medical and psychiatric illness and those with disabilities (CDC, 2020). The same long‐standing health inequities and structural inequalities that have led vulnerable groups to experience climate injustice are contributing to higher rates of COVID‐19, hospitalization rates, and death particularly among racial and ethnic minorities (CDC, 2020). For instance, as of June 2020, the CDC (2020) reported that age‐adjusted hospitalization rates were highest among non‐Hispanic American Indian or Alaska native and non‐Hispanic Black persons.
It is important to note that those who are vulnerable, marginalized, from communities of color and those living with chronic illnesses are among those individuals, families, communities, and populations who are most susceptible to infectious diseases such as COVID‐19 and climate health consequences. Our integrative review on COVID‐19 and climate change yielded no specific literature to date that explicitly focused on the issues of the most vulnerable. This finding is complex and unanticipated since recent literature suggests that systemic and structural racism are embedded in the health consequences of COVID‐19 and climate change. Azar and colleagues found that “compared with non‐Hispanic white patients, African Americans had 2.7 times the odds of hospitalization, after adjusting for age, sex, comorbidities, and income” (Azar et al., 2020, p. 1,253). In April 2020, the CDC explicitly linked risk factors for COVID‐19 to include race/ethnicity, age, gender, certain medical conditions, medication use, poverty/crowding, certain occupations, and pregnancy (CDC, April 4, 2020). While in July 2020, the journal Health Affairs published a paper calling for racism and racial health inequities to be explicitly identified in matters of public health (Boyd et al., 2020), which certainly includes the public health problems of COVID‐19 and climate‐related health consequences. Further they noted that: “In short, racism kills. Whether through force, deprivation, or discrimination, it is a fundamental cause of disease and the strange and familiar root of racial health inequities.” Waite et al. (2020) discussed structural racism and its disenfranchisement of black/brown race groups, suggesting that key steps to address racism for health equity are critical for health and public health. They offered a call to action for governing bodies of the nursing profession and key leadership organizations in public health and global organizations to engage in policy and advocacy efforts to address social justice in public health practice. Waite et al. (2020) further suggested that “social justice accounts for human dignity, respect, and recognition of longstanding oppressions such as racism that have impacted current health systems and outcomes” (p. 127). Lemery, Williams, and Farmer (2014) noted that there are complex disparities and social inequalities related to health challenges for those who least contribute to greenhouse gas emissions, yet are disproportionately affected by the negative health outcomes in our climate‐changing world.
Finally, Edmonds, Kneipp, and Campbell (2020) offered key considerations for public health nurses to address the pressing issues of the COVID‐19 era. They argued that there are urgent acute and chronic health issues that are paramount during this unprecedented pandemic. Edmonds et al. described the key roles of public health nurses in investigating case contact searches, education about social distancing and face covers as key opportunities for minimizing COVID spread, and educating the public about guidelines from the CDC. Further they noted that public health nurses are experts in responding to infectious and chronic disease challenges, and offering safe, nondiscriminatory care that can successfully address systemic and structural racism and challenges that disproportionately affect black/brown people in our COVID‐19 situation. These same populations are also disproportionately affecting these populations in our climate‐changing world. In this review, we supported these views and further advocated that public health nursing has an important role in linking COVID‐19 and the complex health challenges posed by the pandemic with the dire health consequences that are inextricably linked with climate change.
12. CONCLUSIONS
As evidenced by the themes yielded from this review, nursing has a global role which requires an urgent response in public health challenges locally, regionally, nationally, and internationally. Further nursing workforce development globally is poised to expand the role of nurses in addressing the current pandemic and future potential pandemics. Further education of nurses about these public health challenges must be incorporated in formal nursing education programs as well as continuing education programs. The themes that emerged in our review offer opportunities for the future of public health nursing; these themes may also further support a framework of public health and necessary tenets that are critical in addressing the intersection of COVID‐19 and climate change. Understanding human‐environmental impacts are important in the current pandemic and offering insight for the emergence of future pandemics and the climate crisis. A community and a global perspective are integral to engaging in a public health approach to this dual crisis. Environmental impacts, including the built environment are important for policy and advocacy efforts by public health professionals. Professional associations and specialty organizations should fully engage in advancing knowledge about the current and possibly future pandemics and the emerging current climate crisis and associated health consequences. Recommendations for future scholarship and research should focus on the critical role of public health nursing in addressing emerging infectious diseases and potential pandemics and further study of health consequences of climate change within the lens of public health nursing.
Limitations of this integrative review include the nascent body of knowledge of COVID‐19 which only recently emerged in 2019 with viral spread intensifying globally throughout 2020. The recommendations for prevention of spread of disease and treatment were ambiguous and at times—conflicting—early in the pandemic. Emerging knowledge and development of an effective vaccine will galvanize our future public health response and amplify current public health recommendations aimed at limiting the spread of COVID‐19. Similarly, fostering a unified message and a comprehensive public health approach to address the crisis of climate change and associated health consequences also requires persistence by public health nurses in addressing the needs of individuals, families, communities, and populations in the face of this complex intersection of COVID‐19 and climate change.
CONFLICT OF INTERESTS
The authors report no conflicts of interest.
Zang SM, Benjenk I, Breakey S, Pusey‐Reid E, Nicholas PK. The intersection of climate change with the era of COVID‐19. Public Health Nurs. 2021;38:321–335. 10.1111/phn.12866
DATA AVAILABILITY STATEMENT
All data that emerged from this study are available from the corresponding author, Dr. Patrice Nicholas.
REFERENCES
- Azar, K. M. J. , Shen, Z. , Romanelli, R. J. , Lockhart, S. H. , Smits, K. , Robinson, S. , Brown, S. , & Pressman, A. R. (2020). Disparities in outcomes among COVID‐19 patients in a large health care system in California. Health Affairs, 39(7), 1–10. [DOI] [PubMed] [Google Scholar]
- Bale, R. (2020). Trafficked pangolins can carry coronaviruses closely related to pandemic strain. Scientific American, 322. Retrieved from https://www.nationalgeographic.com/animals/2020/03/pangolins‐coronavirus‐covid‐possibility/ [Google Scholar]
- Beauchamp, D. E. (1999). Public health as social justice. In Beauchamp D. E. & Steinbock B. (Eds.), New Ethics for the Public’s Health (pp. 105–114). Oxford University Press. [Google Scholar]
- Benjamin, G. C. (2020). Ensuring health equity during the COVID‐19 pandemic: The role of public health infrastructure. Pan American Journal of Public Health, 44, e70. 10.26633/RPSP.2020.70 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bernstein, A. (2020). An interview with Dr. Aaron Bernstein at the Harvard School of Public Health: Coronavirus and climate change. Retrieved from https://www.hsph.harvard.edu/c‐change/subtopics/coronavirus‐and‐climate‐change/
- Boyd, R. W. , Lindo, E. G. , Weeks, L. D. , & McLemore, M. R. (2020). On racism: A new standard for publishing on racial health inequities. Health Affairs, Published online July 2, 2020.
- Catton, H. (2020). Global challenges in health and health care for nurses and midwives everywhere. International Nursing Review, 67(1), 4–6. 10.1111/inr.12578 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention . (2020). COVID‐19 in racial and ethnic minority groups. Retrieved from https://www.cdc.gov/coronavirus/2019‐ncov/need‐extra‐precautions/racial‐ethnic‐minorities.html
- Cho, R. (2020). COVID‐19 impacts climate change. Retrieved from https://blogs.ei.columbia.edu/2020/06/25/covid‐19‐impacts‐climate‐change/
- Coates, S. J. , Andersen, L. K. , & Boos, M. D. (2020). Balancing public health and private wealth: Lessons on climate inaction from the COVID‐19 pandemic ‐ a report from the International Society of Dermatology Climate Change Committee. International Journal of Dermatology, 59(7), 869–871. 10.1111/ijd.14917 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gostin, L. O. , & Powers, M. (2006). What does social justice require for the public’s health? Public health ethics and policy imperatives. Health Affairs, 25(4), 1053–1060. 10.1377/hlthaff.25.4.1053 [DOI] [PubMed] [Google Scholar]
- Goymann, W. (2020). What the Corona (SARS‐CoV 2) pandemic, climate change, and the biodiversity crisis teach us about human nature. Ethology, 126(6), 593–594. 10.1111/eth.13031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Helm, D. (2020). The environmental impacts of the coronavirus. Environmental and Resource Economics, 76, 21–38. 10.1007/s10640-020-00426-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hemida, M. G. , & Ba Abduallah, F. (2020). The SARS‐CoV‐2 outbreak from a one health perspective. One Health, 10, 10.1016/j.onehlt.2020.100127 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herrero, M. , & Thornton, P. (2020). What can COVID‐19 teach us about responding to climate change. The Lancet Planetary Health, 4(5), e174. 10.1016/S2542-5196(20)30085-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Intergovernmental Panel on Climate Change . (2018). Global warming of 1.5 degree C. An IPCC special report on the impacts of global warming of 1.5degree C. above preindustrial levels and related greenhouse gas emission pathways, in the strengthening of the global response to the context of climate change. World Meterological Society. Retrieved from https://www.ipcc.ch/sr15/ [Google Scholar]
- Ivanova, M. , Baste, I. , Lee, B. , Belliethathan, S. , Gelil, I. A. , Gupta, J. , Haas, P. , Habtezion, Z. , Halpaap, A. , Mohamed‐Katerere, J. , King, P. , Kok, M. , Lee, M. , Patterson, T. , Campal, V. , Chambers, B. , Goodall, M. , Milutinovic, S. , & Preston, F. (2012). GEO5 – Global environmental outlook – Environment for the future we want. Retrieved from https://www.researchgate.net/publication/258838485_GEO5_‐_Global_Environmental_Outlook_‐_Environment_for_the_Future_We_Want/stats
- Jin, S. (2020). COVID‐19, climate change, and renewable energy research: We are all in this together, and the time to act is now. ACS Energy Letters, 5(5), 1709–1711. 10.1021/acsenergylett.0c00910 [DOI] [PubMed] [Google Scholar]
- Jowell, A. , & Barry, M. (2020). COVID‐19: A matter of planetary, not only national health. American Journal of Tropical Medicine and Hygiene, 103(1), 31–32. 10.4269/ajtmh.20-0419 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keenan, J. M. (2020). COVID, resilience, and the built environment. Environment Systems and Decisions, 40, 216–221. 10.1007/s10669-020-09773-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kerry, J. F. (2020). The parallels between the coronoavirus and the climate. The Boston Globe, p. A8. [Google Scholar]
- Li, L. , Li, Q. , Huang, L. , Wang, Q. , Zhu, A. , Xu, J. , Liu, Z. , Li, H. , Shi, L. , Li, R. , Azari, M. , Wang, Y. , Zhang, Z. , Liu, Z. , Zhu, Y. , Zhang, K. , Zue, S. , Ooi, M. C. G. , Zhang, D. , & Chan, A. (2020). Air quality changes during the COVID‐19 lockdown over the Yangtze River Delta Region: An insight into the impact of human activity pattern changes on air pollution variation. Science of the Total Environment, 732, 139282. 10.1016/j.scitotenv.2020.139282 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lorentzen, H. F. , Benfield, T. , Stisen, S. , & Rahbek, C. (2020). COVID‐19 is possibly a consequence of the anthropogenic biodiversity crisis and climate changes. Danish Medical Journal, 67(5), A205025. [PubMed] [Google Scholar]
- Manzanedo, R. D. , & Manning, P. (2020). COVID‐19: Lessons for the climate change emergency. The Science of the Total Environment, 742, 140563. 10.1016/j.scitotenv.2020.140563 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maxwell, J. , & Blashki, G. (2016). Teaching about climate change in medical education. Journal of Public Health Research, 5, 673. 10.4081/jphr.2016.673 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mikati, I. , Benson, A. F. , Luben, T. J. , Sacks, J. D. , & Richmond‐Bryant, J. (2018). Disparities in distribution of particulate matter emission sources by race and poverty status. American Journal of Public Health, 108, 480–485. 10.2105/AJPH.2017.304297 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morens, D. M. , Breman, J. G. , Calisher, C. H. , Doherty, P. C. , Hahn, B. H. , Keusch, G. T. , Karamer, L. D. , LeDuc, J. W. , Monath, T. P. , & Taubenbergger, J. K. (2020). The origins of COVID‐19 and why it matters. American Journal of Tropical Medicine and Hygiene, 10.4269/ajtmh.20-0849 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morrison, L. (2020). Viewpoint: The COVID‐19 and climate crises. British Journal of General Practice, 70(694), 241. 10.3399/bjgp20X709637 [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Reilly, K. M. , Auzenbergs, M. , Jafari, Y. , Liu, Y. , Flasche, S. , & Lowe, R. (2020). Effective transmission across the globe: The role of climate in COVID‐19 mitigation strategies. The Lancet Planetary Health, 4(5), e172. 10.1016/S2542-5196(20)30106-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patruno, C. , Nistico, S. P. , Fabbrocini, G. , & Napolitano, M. (2020). Is climate change the next pandemic for dermatology? Lessons from COVID‐19. Dermatologic Therapy, 33(4), e13682. 10.1111/dth.13682 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Powers, M. , & Faden, R. (2006). Social justice: The moral foundations of public health and health policy. Oxford University Press. [DOI] [PubMed] [Google Scholar]
- Price‐Haywood, E. G. , Burton, J. , Fort, D. , & Seoane, L. (2020). Hospitalization and mortality among Black patients and White patients with Covid‐19. New England Journal of Medicine, 382(26), 2534–2543. 10.1056/NEJMsa2011686 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenbloom, D. , & Markard, J. (2020). A covid‐19 recovery for climate. Science, 268(6490), 447. 10.1126/science.abc4887 [DOI] [PubMed] [Google Scholar]
- Schwartz, S. A. (2020). Climate change, Covid‐19, preparedness, and consciousness. Explore, 16(3), 141–144. 10.1016/j.explore.2020.02.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shankar, H. M. , Ewart, G. , Garcia, E. , Hicks, A. , & Hardie, W. (2020). COVID‐19, climate change, and the American Thoracic Society. A shared responsibility. Annals of the American Thoracic Society, 17(9), 1052–1055. 10.1513/AnnalsATS.202002-180VP [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waite, B. , Sayer, L. , & Waite, D. (2020). A call to action for community/public health nurses: Treat structural racism as the critical social determinant of health it is. Public Health Nursing, 37, 147–148. 10.1111/phn.12717 [DOI] [PubMed] [Google Scholar]
- Watts, N. , Amann, M. , Arnell, N. , Ayeb‐Karlsson, S. , Belesova, K. , Boykoff, M. , Byass, P. , Cai, W. , Campbell‐Lendrum, D. , Capstick, S. , Chambers, J. , Dalin, C. , Daly, M. , Dasandi, N. , Davies, M. , Drummond, P. , Dubrow, R. , Ebi, K. L. , Eckelman, M. , … Montgomery, H. (2019). The 2019 report of The Lancet Countdown on health and climate change: Ensuring that the health of a child born today is not defined by a changing climate. The Lancet, 394, 1836–1878. 10.1016/S0140-6736(19)32596-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu, X. , Nethery, R. C. , Sabat, B. M. , Braun, D. , & Dominici, F. (2020). Exposure to air pollution and COVID 19 mortality in the United States: A nationwide cross‐sectional study. 10.1101/2020.04.05.20054502 [DOI] [PMC free article] [PubMed]
- Xiao, K. , Zhai, J. , Feng, Y. , Zhou, N. , Zhang, X. U. , Zou, J.‐J. , Li, N. A. , Guo, Y. , Li, X. , Shen, X. , Zhang, Z. , Shu, F. , Huang, W. , Li, Y. U. , Zhang, Z. , Chen, R.‐A. , Wu, Y.‐J. , Peng, S.‐M. , Huang, M. , … Shen, Y. (2020). Isolation of SARS‐CoV‐2‐related coronavirus from Malayan pangolins. Nature, 583(7815), 286–289. 10.1038/s41586-020-2313-x [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data that emerged from this study are available from the corresponding author, Dr. Patrice Nicholas.


