Abstract
Purpose
Non‐urgent face‐to‐face outpatient ophthalmology appointments were suspended in the United Kingdom in March 2020, due to the COVID‐19 outbreak. In common with other centres, Moorfields Eye Hospital NHS Foundation Trust (London) offered modified telephone consultations to new and follow‐up patients in the low vision clinic. Here we assess the success of this telephone service.
Methods
Data were collected for 500 consecutive telephone low vision appointments. Successful completion of the assessment and clinical outcomes (low vision aids prescribed, onward referral) were recorded.
Results
Telephone assessments were completed for 364 people (72.8%). The most common reasons for non‐completion were either no answer to the telephone call (75 people, 15%), or the patient declining assessment (20 people, 4%). There was no association between age and the likelihood of an assessment being completed. 131 new low vision aids were dispensed, 77 internal referrals were made and 15 people were referred to outside services. More than 80% of the low vision aids prescribed were useful.
Conclusions
Telephone low vision assessments were completed in about three‐quarters of cases. About one‐quarter of consultations resulted in new low vision aids being dispensed, which were generally found useful. Telephone low vision assessments can be used successfully in a large low vision clinic, but have many limitations when compared to face‐to‐face assessments.
Keywords: low vision, remote consultation, telemedicine, tele‐rehabilitation, visual acuity
Introduction
When the United Kingdom was locked down in March 2020 to combat the spread of novel coronavirus SARS‐CoV‐2, the UK’s Royal College of Ophthalmologists recommended that ‘all face‐to‐face outpatient activity should be postponed unless patients are at high risk of rapid, significant harm if their appointment is delayed’. 1 Consequently, most face‐to‐face low vision assessments at Moorfields Eye Hospital in London were converted to telephone assessments. The Moorfields low vision clinic is the largest of its type in the world, 2 and has performed more than 100 000 assessments since its formation in the 1960s. Between April and September 2020, more than 1700 telephone low vision consultations were performed.
Remote (telephone or video based) low vision assessments have previously been offered by several centres, although no large‐scale reports of the success of remote low vision assessment have yet been published. 3 One study of video based remote low vision assessment for a small group of 10 older adults with low vision showed that practitioners found little difficulty with remote assessment, and that patients were largely satisfied with their consultations. 4 In that particular study, participants were loaned equipment including a tablet computer and wireless hotspot device, which would not be practical for the size of the Moorfields clinic.
We elected to use telephone rather than video consultations as more than 1 in 8 people in the UK do not use the internet, including 48% of those over 75 years of age, 5 all of whom are classified as being of at least moderate risk of complications from COVID‐19. 6 People with lower household income are also more likely to be digitally excluded, 7 and working age people with visual impairment have higher unemployment rates than the general population. 7
Following a review of the literature, a protocol for telephone assessments was developed by experienced low vision optometrists (including authors KB, HD and MDC; Appendix S1). In line with best practice, 8 this new service was audited. Here we present results from our audit, for 500 consecutive adult patients who were offered appointments.
Method
Participants
Data were collected for 500 consecutive telephone low vision assessments (LVAs). The telephone‐based appointment was a modified and abbreviated version of a comprehensive face‐to‐face LVA.
Patients were scheduled for telephone assessment if they had new or follow‐up low vision appointments booked on the hospital clinic administration system, or if new referrals were made into the department. Participants were deemed unsuitable for telephone consultation if they required language translators, were deaf, or had learning difficulties where telephone conversations would prove too challenging. In this study we only examined those who were given appointments in the adult clinic; the children’s low vision clinic will be audited separately.
Assessments were performed by experienced low vision optometrists. Forty‐five minutes was allocated for routine assessments (follow‐up patients with no prior concerns), and 1 h was provided for new patients and complex follow‐up cases (those with ongoing difficulties, new concerns reported to the clinic or concomitant health conditions which might make the examination more difficult).
Prior to the telephone assessment, patients were sent a large print appointment letter stating the purpose of the proposed call with a given appointment time. They were also sent a home acuity test (www.homeacuitytest.org) 9 with a 150 cm length of string to measure the chart viewing distance, Blu‐tack (www.bostik.com) to stick the charts to a wall and a near low vision test booklet.
Telephone assessment
Assessments were marked as not completed (did not attend) if patients could not be contacted within 15 min of their appointment time. In this case, patients were contacted by post to arrange a further appointment. If the patient answered their phone, identity and willingness to proceed were confirmed. A full needs assessment, similar to that done in a face‐to‐face LVA assessment, was performed. This assessment included, but was not limited to: subjective impression of vision; current use of magnifiers, spectacles and non‐optical strategies; social situation; employment and education; safety at home; daily living tasks; mobility; wellbeing; hobbies and sources of support.
Visual assessment
Distance vision was assessed using the home acuity test (www.homeacuitytest.org) 9 which consists of two A4 sheets with crowded Sloan letters sized 1.30 to 0.10 logMAR. Patients were asked to read each chart monocularly wearing their habitual distance correction.
The near low vision test booklet was used with habitual reading correction to estimate the magnification required for loaning new low vision aids. This booklet features a page of single letters decreasing in size from N72 to N6 (1.40 logMAR to 0.30 logMAR) to measure near visual acuity, followed by sentences decreasing in size from N48 to N6 (1.20 logMAR to 0.30 logMAR) to assess reading fluency.
Where patients did not receive or could not find the near low vision test booklet, they were asked whether they could read examples of different print sizes (newspaper headlines, subheadings and text and medicine labels).
Prescription of optical low vision aids
Optical low vision aids for near tasks were prescribed based on performance on the near low vision test booklet with the current spectacles or low vision aids. Device strength was calculated based on the measured and target visual acuity, including an acuity reserve where needed.
A limited range of distance devices were also available for prescription, including low power spectacle mounted Galilean telescopes (Eschenbach Max TV and Max TV clip, www.eschenbach.com), binoculars and handheld astronomical telescopes (4×, 6× and 8×), and were prescribed based on distance visual acuity and the tasks for which they were needed.
Devices were mailed to patients under the hospital permanent loan scheme. No charge was made for optical devices.
Signposting and referral
If patients reported new urgent ophthalmological symptoms (for example, new floaters or a sudden drop in vision), they were asked to attend the Moorfields Accident & Emergency service (with online assessment followed by a face‐to‐face consultation with an ophthalmologist where needed). Where patients had new but non‐urgent symptoms, such as a gradual deterioration in vision in someone with a degenerative disease, a referral was made back to the patient’s consultant ophthalmologist.
All participants were specifically asked questions about their mental health. If necessary, internal referrals could be made to a psychological counselling service, and external referrals could be made to telephone counselling services and to the general medical practitioner (GP). Internal referrals could also be made to the Certificate of Visual Impairment service, and the Eye Clinic Liaison Officer (ECLO). Signposting and referral could also be made to external services including local and national charities, local council sensory teams, mobility training services and the patient’s own medical practitioner.
Follow‐up appointments
Follow up telephone calls were offered when new devices had been issued, when referrals had been made and when the optometrist felt that the patient would benefit from further discussion. Telephone follow‐up appointments were made 4 weeks after the initial assessment.
Techniques which could only be performed in person (such as refraction, reading speed assessment and demonstration of tints or electronic devices) were discussed and appointments booked if needed. During 4‐week follow up calls, satisfaction with new magnifiers was checked. Satisfaction was defined as the patient finding the new magnifier useful for its intended task and easy to use. Where patients were not satisfied with the device, an alternative low vision aid was prescribed. Where patients had been signposted or referred, they were asked if they had heard from the appropriate service.
Communication
A summary letter was sent to each patient in appropriate font size with instructions for magnifier use and recapping important points of discussion. Relevant patient information leaflets were also sent. Examples of these included details of mobile phone applications designed to assist visually impaired people, computer advice and details of government employment support schemes.
All data were recorded on an electronic patient record system (OpenEyes, https://openeyes.apperta.org). For the purposes of this audit, data were extracted from OpenEyes and recorded on an Excel spreadsheet. Statistical analyses were performed in Excel (www.microsoft.com) and SPSS (https://www.ibm.com/uk‐en/analytics/spss‐statistics‐software).
Approval
The study was approved by the Clinical Audit Committee of Moorfields Eye Hospital (approval number 640).
Results
Five hundred people were offered a telephone low vision assessment. Their mean age was 60.7 years (S.D.: 22.3, range 15–103 years; Figure 1 ). 262 (52%) were female. More than half had retinal disease (Table 1 ), and 143 people (28.6%) had multiple ophthalmic diagnoses. One hundred and thirty‐eight were new appointments and 362 were follow‐up appointments.
Figure 1.
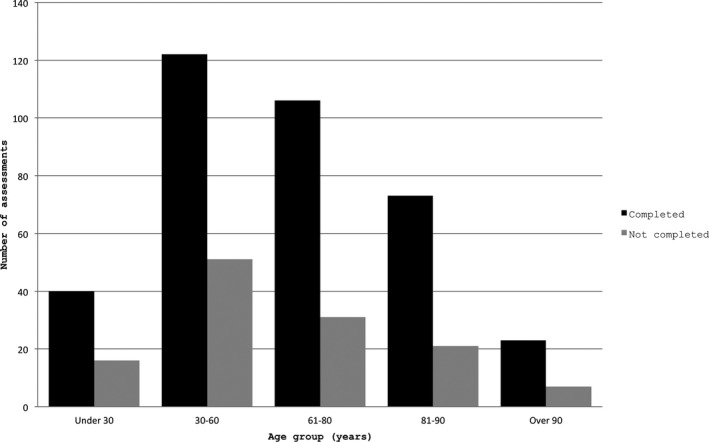
Number of assessments completed (black bars) and not completed (grey bars) by age group.
Table 1.
Diagnosis of participants
| Diagnosis | Examples | Number (%) of participants |
|---|---|---|
| Retinal disease | ||
| Age‐related macular disease | 76 (15%) | |
| Inherited macular disease | Stargardt Disease, Best Disease | 61 (12%) |
| Inherited peripheral retina disease | Retinitis pigmentosa, achromatopsia | 95 (19%) |
| Diabetic retinopathy | 37 (7.4%) | |
| Retinal detachment/vitreoretinal disease | 4 (0.8%) | |
| Optic nerve disease | ||
| Optic atrophy | 16 (3.2%) | |
| Glaucoma | 10 (2%) | |
| Other diseases | ||
| Uveitis | 6 (1.2%) | |
| Corneal disease | Keratoconus, Fuch’s dystrophy | 4 (0.8%) |
| Other diseases | 47 (9.4%) | |
| Multiple diseases | 143 (29%) | |
This article is being made freely available through PubMed Central as part of the COVID-19 public health emergency response. It can be used for unrestricted research re-use and analysis in any form or by any means with acknowledgement of the original source, for the duration of the public health emergency.
Mean distance visual acuity in the better eye was 0.78 logMAR (6/38 + 1; standard deviation 0.34 logMAR). Near visual acuity was measured uncorrected (N = 29), with the current magnifier (N = 118), spectacles (N = 77) or contact lenses (N = 1). Mean near visual acuity was N13 (approximately 0.65 logMAR or 1.6M).
Telephone assessments were completed in 364 people (72.8%). The most common reason for the assessment not being completed was no answer (75 people, 15%) followed by the patient declining the service (20 people, 4%), Table 2 . Data were missing for 10 patients.
Table 2.
Reasons for telephone assessment not being completed
| Assessment completed? | Count | Percentage of total |
|---|---|---|
| Yes | 364 | 72.80% |
| No ‐ no answer | 75 | 15.00% |
| No ‐ patient declined | 20 | 4.00% |
| No ‐ patient has poor hearing | 1 | 0.20% |
| No ‐ patient has poor English | 3 | 0.60% |
| No ‐ patient confused | 1 | 0.20% |
| No ‐ patient in hospital | 1 | 0.20% |
| No ‐ patient rescheduled for another day | 7 | 1.40% |
| No ‐ other | 18 | 3.60% |
| Not recorded | 10 | 2.00% |
This article is being made freely available through PubMed Central as part of the COVID-19 public health emergency response. It can be used for unrestricted research re-use and analysis in any form or by any means with acknowledgement of the original source, for the duration of the public health emergency.
There was no relationship between age and the likelihood of a telephone assessment being completed (mean age, assessment completed: 61.3 years; assessment not completed: 59.4 years; p = 0.4; Figure 1 ). New appointments were no more likely to be completed than follow‐ups (new: 97/138 completed; follow‐up: 267/362 completed; Chi‐square statistic 0.35, p = 0.56).
Vision was subjectively deemed stable in nearly two‐thirds of the patients (225 people, 62%). None reported a sudden decline in their vision. Ten people (3%) thought their vision had improved and 90 (25%) reported a gradual decline. Vision data were not recorded in 39 cases.
Home Acuity Test
The Home Acuity Test was used to measure vision in 257 people (70.6%). The most common reasons for non‐completion were charts not being received in the post (N = 35, 9.6%), and unable to see the top of the chart (N = 21, 5.8%). Data were not recorded for 28 people (7.7%).
Follow‐up appointments
A follow‐up appointment was offered in 111 cases. Of these, 93 (84%) completed the follow up. The overwhelming majority of appointments (106/111, 95%) were offered to those who had been prescribed new low vision aids.
Low Vision Aids (LVAs)
131 LVAs were prescribed from 88 patient encounters for which follow–up data were available. Patients reported being happy with 108 of these devices. Patients were unhappy with 23 of the LVAs, 8 of which were exchanged for an alternate LVA.
Onward referral and signposting
Internal referrals were made for 77 patients either to the ECLO (N = 34, 9.3%), the nurse counselling service (N = 20, 5.5%) or to medical services, such as the medical retina clinic, optometry‐led glaucoma and uveitis service (N = 10). Ten were referred to multiple internal services. 8.8% (32/364) of assessments led to a referral back to the consultant led ophthalmology clinic. In 81% of these cases this was for reduced vision.
External referrals were made in 15 cases, most commonly to the GP (N = 5) and charity services (N = 4).
Discussion
The majority of patients could be assessed using our telephone low vision service, including those up to 101 years old. From 364 completed assessments, 131 new low vision aids were dispensed, 77 internal referrals were made and 15 people were referred to outside services. Only 32 patients needed to be reassessed in an ophthalmologist led service.
Common reasons for not being able to complete a telephone LVA included not answering the phone and patient choice. There were several limitations of our telephone assessment when compared to a full face‐to‐face LVA. At ‘in person’ LVAs we have access to far more measures of visual function, including reading speed, contrast sensitivity, colour vision, visual fields and sensitivity to glare, which provides a more holistic view of visual impairment. Working distances can be measured accurately, as can the power of existing spectacles. Our usual LVA includes refraction and the prescription of suitable spectacles, which we were not able to perform remotely. At face‐to‐face clinics we also have access to a wider range of optical devices and tints, and we can demonstrate apps, electronic magnifiers and the effect of task lighting. Observing people walking from the waiting area to the clinic room can highlight mobility problems, and it can be easier to identify low mood or mental health difficulties in person.
A further obvious limitation of a telephone‐based service is difficulty assessing people with poor hearing. Notes were reviewed to determine whether people had poor hearing before a telephone assessment was offered. Once this screening was completed, only one assessment was not completed due to poor hearing. We suggest that video based calling is used for patients who use sign language: applications such as Attend Anywhere (www.attendanywhere.com) allow a sign language interpreter to be present in a video consultation.
We have not attempted to evaluate how useful patients found our telephone service as we felt that the unusual situation around lockdown meant that this would not be comparable to previously collected data on clinic satisfaction. For example, increased loneliness and social isolation during lockdown might have inflated satisfaction ratings for the service. We attempted to measure satisfaction with any new low vision aids prescribed by asking whether they performed the task they were prescribed for. This is a weak measure of satisfaction: it is well known that people will often say that they are happy with any intervention provided. We did not measure visual acuity with the new device, although we will do this in any follow‐up studies. Future research could also consider relative satisfaction with telephone or face‐to‐face low vision assessments, and more sophisticated measures of satisfaction should be used. A recent systematic review did not find any completed randomised controlled trials or controlled clinical trials of telemedicine rehabilitation for low vision. 3
It is concerning that no data were recorded for 10 participants. Moorfields Eye Hospital is in a period of transition to electronic records only, and it is possible that entries were made on paper records. Clinical staff have been reminded of the importance of adequate record keeping.
At the time of writing (September 2020), lockdown measures in the UK are being eased and we are once again able to offer face to face assessments. However, some of our patients remain reluctant to attend hospital appointments. For the week beginning 3 August, 2020, when the clinic was gradually reopening, 29 patients attended face‐to‐face appointments and 6 failed to attend. This gives an attendance rate of 82.9%, broadly similar to the 72.8% in the audit. The hospital is in central London with very limited car parking, so most patients need to use hospital patient transport services or public transport, a known cause of anxiety. 10 It has been established that travelling safely to an appointment and manoeuvring around a hospital can be a barrier for access to care for patients with vision impairment. 11 In a study of blind rehabilitation in the USA, individuals receiving tele‐rehabilitation services saved an average of 122 travel miles, more than 2 h of time and $65.29 per person. 12
The ageing population means that a larger number of people need access to ophthalmic care. As a result, virtual consultations are becoming increasingly necessary across all ophthalmic subspecialties in order to maximise capacity and cater to this growing demand. Accordingly, the future of low vision services is likely to be heavily impacted by the increasing number of people with visual impairment, even when accounting for improved treatments and public health education. This will create a strong need for improved availability of cost effective services. 13
We see telephone‐based low vision assessment as being used alongside other methods of low vision rehabilitation, such as hospital low vision clinics, mobile clinics in hard‐to‐reach areas 14 and providing additional training in low vision for community optometrists. 15 In pre‐COVID times, i.e., prior to mandated social distancing, increasing capacity was difficult where clinical space is a premium. Therefore, in the future a need for telephone consultations may not arise solely from pandemics but also from patient preference and pressure on clinical space within the hospital.
In ‘our modern epidemic era’ 16 globalization is leading to more regular pandemics 17 and therefore an adequate, robust and safe service is essential to be prepared for future occurrences. Unlike some low vision tele‐rehabilitation services, which stopped at the end of a study period due to funding being withdrawn (e.g., a project at the University of Houston 18 ), it is important that telephone consultations continue to be offered. We believe that our telephone low vision service is safe and easy to access for many of our patients with visual impairment, but it is not yet able to provide the holistic, multidisciplinary, low vision assessment which can be provided in person.
Disclosure
The authors report no conflicts of interest and have no proprietary interest in any of the materials mentioned in this article. This research received no specific grant from any funding agency in the public, commercial, or not‐for‐profit sectors.
Author contributions
Ankit Patel: Data curation (lead); Formal analysis (lead); Investigation (equal); Writing‐original draft (supporting); Writing‐review & editing (supporting). Alicia S Fothergill: Data curation (supporting); Formal analysis (supporting); Investigation (equal); Writing‐original draft (supporting); Writing‐review & editing (supporting). Katy E C Barnard: Conceptualization (equal); Methodology (equal); Project administration (lead); Supervision (equal); Writing‐review & editing (supporting). Hannah Dunbar: Conceptualization (equal); Supervision (equal); Writing‐review & editing (equal). Michael D Crossland: Conceptualization (equal); Methodology (equal); Supervision (equal); Writing‐original draft (lead).
Supporting information
Appendix S1. Protocol for Moorfields telephone based low vision assessment
Patel A, Fothergill AS, Barnard KEC, Dunbar H, & Crossland MD. Lockdown low vision assessment: an audit of 500 telephone‐based modified low vision consultations. Ophthalmic Physiol Opt. 2021; 41: 295–300. 10.1111/opo.12789
References
- 1. Royal College of Ophthalmologists . Management of Ophthalmology Services during the Covid pandemic. http://www.rcophth.ac.uk/wp‐content/uploads/2020/03/RCOphth‐Management‐of‐Ophthalmology‐Services‐during‐the‐Covid‐pandemic‐280320.pdf (Accessed 10 September 2020).
- 2. Crossland MD & Silver JH. Thirty years in an urban low vision clinic: changes in prescribing habits of low vision practitioners. Optom Vis Sci 2005; 82: 617–622. [DOI] [PubMed] [Google Scholar]
- 3. Bittner AK, Yoshinaga PD, Wykstra SL & Li T. Telerehabilitation for people with low vision. Cochrane Database Syst Rev 2020; 2: CD011019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Bittner AK, Yoshinaga P, Bowers A, Shepherd JD, Succar T & Ross NC. Feasibility of telerehabilitation for low vision: satisfaction ratings by providers and patients. Optom Vis Sci 2018; 95: 865–872. [DOI] [PubMed] [Google Scholar]
- 5. Ofcom . Adults’ media use and attitudes report. Ofcom. 2019. https://www.Ofcom.org.uk/research‐and‐data/media‐literacy‐research/adults/adults‐media‐use‐and‐attitudes (Accessed 1 June 2020).
- 6. NHS . Coronavirus (COVID‐19): Shielded patients list. https://digital.nhs.uk/coronavirus/shielded‐patient‐list (Accessed 1 June 2020).
- 7. Kelly SM. Labor force participation rates among working‐age individuals with visual impairments. J Vis Impair Blind 2013; 107: 509–513. [Google Scholar]
- 8. Wolffsohn JS & Karas M. Clinical audit cycle of low vision rehabilitation services. Optom Pract 2004; 5: 115–126. [Google Scholar]
- 9. Crossland MD, Dekker TM, Hancox J, Lisi M, Wemyss TA & Thomas PBM. Evaluation of a home‐printable vision screening test for telemedicine. JAMA Ophthalmol 2021. 10.1001/jamaophthalmol.2020.597 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Pollard TL, Simpson JA, Lamoureux EL & Keeffe JE. Barriers to accessing low vision services. Ophthalmic Physiol Opt 2003; 23: 321–327. [DOI] [PubMed] [Google Scholar]
- 11. Ryan B & McCloughan L. Our Better Vision What People Need from Low Vision Services in the UK. Royal National Institute for the Blind: London; 1999. [Google Scholar]
- 12. Ihrig C. Travel cost savings and practicality for low‐vision telerehabilitation. Telemed J E Health 2019; 25: 649–654. [DOI] [PubMed] [Google Scholar]
- 13. Ryan B. Models of low vision care: past, present and future. Clin Exp Optom 2014; 97: 209–213. [DOI] [PubMed] [Google Scholar]
- 14. Gobeille MR, Malkin AG, Jamara R & Ross NC. Utilization and abandonment of low vision devices prescribed on a mobile clinic. Optom Vis Sci 2018; 95: 859–864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Ryan B, Khadka J, Bunce C & Court H. Effectiveness of the community‐based Low Vision Service Wales: a long‐term outcome study. Br J Ophthalmol 2013; 97: 487–491. [DOI] [PubMed] [Google Scholar]
- 16. Morens DM, Daszak P & Taubenberger JK. Escaping Pandora’s box ‐ another novel coronavirus. N Engl J Med 2020; 382: 1293–1295. [DOI] [PubMed] [Google Scholar]
- 17. Akin L & Gözel MG. Understanding dynamics of pandemics. Turk J Med Sci 2020; 50: 515–519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Tang RA, Morales M, Ricur G & Schiffman JS. Telemedicine for eye care. J Telemed Telecare 2005; 11: 391–396. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix S1. Protocol for Moorfields telephone based low vision assessment


