Abstract
Purpose
This study aimed to determine the effects of progressive muscle relaxation exercises on the anxiety and sleep quality of patients with coronavirus disease 2019 (COVID‐19).
Materials and Methods
This is an experimental study. Its data were collected in the infectious diseases clinic of a research hospital from May to August, 2020. This study was carried out with 67 COVID‐19 patients (33 in the experimental group and 34 in the control group). The data were collected using a personal information form, the state‐trait anxiety inventory, and the Richards–Campbell Sleep Questionnaire. The progressive muscle relaxation exercises were performed twice a day for 5 days with the researcher's supervision. The data were analyzed using means, numbers, percentage distributions, the χ 2 test, the dependent t test, and the independent t test.
Results
Statistically significant differences were found between the experimental and control groups' mean posttest scores on the State‐Trait Anxiety Inventory and the Richards–Campbell Sleep Questionnaire (p < 0.05). The in‐group comparison of the experimental group found a statistically significant difference between their mean pretest and posttest scores on the State Anxiety Scale (p < 0.05). The in‐group comparison of the control group found no statistically significant changes in their mean pretest and posttest scores on the State Anxiety Scale (p > 0.05).
Conclusion
The progressive muscle relaxation exercises effectively reduced the anxiety and improved the sleep quality of patients with COVID‐19.
Keywords: anxiety, COVID‐19, progressive muscle relaxation exercises, sleep quality
1. INTRODUCTION
Coronavirus disease 2019 (COVID‐19), which was detected at the end of 2019 and quickly led to a pandemic, is now a global health issue. 1 More than 24 million people have been infected and 821 thousand people have died of COVID‐19. 2 There are not effective antivirals or vaccines even though studies are ongoing. 3 Therefore, it is critical to reduce the spread of the virus and to strengthen patients' immune systems.4, 5
Healthy lifestyle, regular exercise, healthy state of mind, and quality of sleep are related to strengthening the immune system. 4 Studies conducted with quarantined COVID‐19 patients have shown that a major part of the patients experience serious psychological problems.6, 7, 8, 9, 10 Corona viruses can cause psychopathological sequelae through direct viral infection of the central nervous system (CNS) or an indirect immune response. 11 Important psychological stressors include pathophobia, stigmatization, uncertainty about the future, disease‐related traumatic memories, and immunological mechanisms.7, 8, 11, 12 A number of researchers have also noted that COVID‐19 responses such as quarantines may also contribute to mental problems. 13
Studies of the psychological states of patients with COVID‐19 in hospitals have reported that they have high levels of anxiety.6, 10 Researchers have found that problems related to the anxiety and stress of patients receiving COVID‐19‐related treatment can cause serious damage as the disease progresses. 9 Chong et al. 14 found that people with pandemic‐related anxiety have high levels of posttraumatic stress disorder, health anxiety, and suicidal ideation. However, there are not enough studies of COVID‐19 patients' anxiety and related problems.6, 10 Most of the studies of anxiety concerning COVID‐19 have focused on health‐care professionals and the general public.15, 16, 17 More research is needed to mitigate or prevent the intense anxiety of COVID‐19 patients who experience the devastating effect of the virus firsthand. 6
Studies have shown that many patients experience serious sleep problems during the COVID‐19 treatment18, 19, 20, 21 Sleeping is a physiological and behavioral process required to live, and it plays an important role in strengthening the immune system.21, 22 Sleep deprivation negatively affects immune responses by disrupting the circadian rhythm. 19 A retrospective cohort study found that the poor sleep quality of COVID‐19 patients is related to slow recovery and increased need for care in intensive care units. 21 The use of sleep‐inducing drugs such as benzodiazepine with COVID‐19 patients may cause respiratory depression and delay monitoring the disease. Some researchers recommend the use of nonpharmacological methods to reduce the sleep problems of COVID‐19 patients. 23
There are numerous studies in literature on the use of progressive muscle relaxation exercises to reduce the anxiety levels and sleep problems of patients with a chronic disease.24, 25, 26, 27 Progressive muscle relaxation is a deep relaxation technique based on the principle that muscle strain is a physiological response of the human body to disturbing thoughts. This technique leads to a voluntary and regular relaxation of the major muscle groups and thus relaxes the entire body. 28 Progressive muscle relaxation exercises are easy to learn and can be done anywhere at any time. They are also economical because they do not require special technology or equipment.23, 24, 25, 26, 27, 28, 29 Studies have shown that muscle relaxation exercises help patients reduce their anxiety and improve their sleep quality because they reduce tension, stress, blood pressure, heart rate, lactic acid production, and sensitivity to pain when regularly performed with proper techniques.24, 25, 26, 27, 28, 29
This study can contribute to literature as a guide or health‐care professionals' efforts to eliminate the anxiety and sleep problems of patients with COVID‐19 that cannot be treated with pharmacological methods and can thus cause long‐term serious problems. This study aimed to determine the effects of progressive muscle relaxation exercises on the anxiety and sleep quality of patients with COVID‐19.
2. METHODS
2.1. Study type
This is an experimental study.
2.2. Study setting
This study was conducted in the COVID‐19 clinic of a research hospital from May to August, 2020.
2.3. Study population and sample
The study population consisted of COVID‐19 patients who were receiving treatment in the clinic. Its sample consisted of 73 patients. All patients who met the inclusion criteria were included in the study. Simple randomization was used. After being informed about the study, 36 patients were assigned to the experimental group, and 37 patients were assigned to the control group. This study was completed with 67 patients with COVID‐19, 33 for experimental group and 34 for control group, because 2 patients in the experimental group and 1 patient in the control group were discharged, the clinical status of 1 patient worsened to the extent of being unable to perform progressive muscle relaxation exercises, and 2 patients in the control group were transferred to a different hospital (Figure 1). Post hoc power analysis was performed to determine the adequacy of the sample size of the study. In the power analysis performed to determine the sample's power to represent the population, it was found that the power was 0.99 at the medium effect size and significance level of .05.
Figure 1.
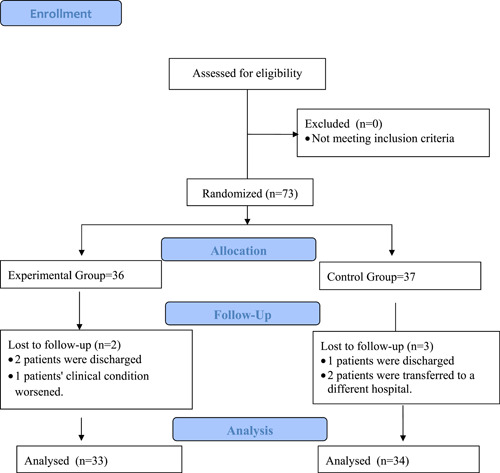
CONSORT flow diagram [Color figure can be viewed at wileyonlinelibrary.com]
The inclusion criteria were being diagnosed with COVID‐19, being at least 18 years old, having no visual or hearing impairments, being able to perform progressive muscle relation exercises, and voluntary participation.
2.4. Data collection tools
2.4.1. The Personal Information Form
A personal information form was developed by the researcher. It includes 11 questions concerning age, gender, marital status, place of residence, profession, income level, previous hospitalizations, chronic disease, smoking, alcohol consumption, and regular exercise.
2.4.2. The State‐Trait Anxiety Inventory (STAI)
This inventory was developed by Spielberger et al. 30 to assess state and trait anxiety levels. Öner & LeCompte 31 did the validity and reliability study of its Turkish version. It consists of two scales that can be administered to people who are 14 or older. The State Anxiety Scale (SAS) determines how people feel at a specific time and under specific conditions, and the Trait Anxiety Scale (TAS) determines how they feel independently of their current situation. This scale consists of 40 items. The first 20 items assess state‐dependent anxiety, and the last 20 items assess trait anxiety. This is a 4‐point Likert‐type scale. Scores on both scales range from 20 to 80, and higher scores indicate higher levels of anxiety. The Cronbach's α coefficients were .84 for the SAS and .80 for the TAS. The Cronbach's α coefficients in this study were .67 for the SAS and .63 for the TAS.
2.4.3. The Richards–Campbell Sleep Questionnaire (RCSQ)
The RCSQ was developed by Richards 32 to assess patients' perceptions of sleep. Özlü and Özer 33 did the validity and reliability study of the Turkish version of the RCSQ. The RCSQ consists of six items that assesses sleep depth, sleep latency, awakenings, returning to sleep, sleep quality, and noise. Each item is scored from 0 to 100 using the visual analogue scale. Scores from 0 to 25 indicate poor quality of sleep, and scores from 76 to 100 indicated high quality of sleep. Higher scores indicate higher levels of sleep quality. The Cronbach's α coefficient was .91 for the RCSQ. The Cronbach's α coefficient in this study was .91 for the RCSQ.
2.5. Data Collection and Implementation
The data were collected from May to August, 2020. Pretests and posttests were conducted with patients in both the experimental and control groups. The patients in the control group did not receive any specific intervention, only routine care. The patients in both groups continued their pharmacological treatments and the routine practices of the clinic during the specified period of time. After the data were collected from the patients in the control group, they were informed that they also could receive progressive muscle relaxation exercises at any time.
The scheduling of the progressive muscle relaxation exercises was determined with the patients in the experimental group. A compact disc (CD) prepared by the Turkish Psychologists Association was used to teach the muscle relaxation exercises. The muscle relaxation exercises were shown on the TVs in the patients' rooms, and the patients exercised along with their TVs to minimize direct patient contact. The CD included instructions for muscle relaxation exercises and music to help the patients relax. Permission to use the Progressive Muscle Relaxation Exercise CD was obtained from the Turkish Psychologists Association by email. The progressive muscle relaxation exercises were done by the experimental group twice a day for 5 days in accordance with an expert's advice. It took approximately 20–30 min to perform the exercises. Posttests were conducted with the experimental group after the muscle relaxation training was completed.
2.6. Data Analysis
Data coding and analysis were performed using SPSS 21. The data were analyzed using means, numbers, percentage distributions, the χ 2 test, the dependent t test, and the independent t test.
2.7. Ethical considerations
Ethical committee approval was obtained from the Atatürk University Medical Faculty Clinical Research Ethics Committee (B.30.2.ATA.0.01.00/249). The participants were informed about the study before the data collection process and were asked to sign an informed consent form.
3. RESULTS
The results of this study, which aimed to determine the effects of progressive muscle relaxation exercises on anxiety and sleep quality of patients with COVID‐19, are shown below. Table 1 shows the sociodemographic characteristics of the participants. No significant differences were found between the groups in terms of sociodemographic characteristics (p > 0.05) (Table 1). Table 2 shows the differences between the pretest and posttest STAI scores of both groups. The mean pretest scores of the experimental group were 62.33 ± 8.33 for the SAS and 48.12 ± 5.22 for the TAS. The mean pretest scores of the control group were 60.68 ± 9.17 for the SAS and 45.35 ± 8.09 for the TAS. No significant differences were found between the state and trait anxiety levels of the groups, which were determined to be homogeneous (p > 0.05).
Table 1.
Distribution of patients according to sociodemographic features (n = 67)
| Features | Experiment group, n = 33 | % | Control group, n = 34 | % | Test value and significance |
|---|---|---|---|---|---|
| Sex | |||||
| Female | 12 | 36 | 18 | 53 | χ 2 = 1.861 |
| Male | 21 | 64 | 16 | 47 | p = 0.172 |
| Marital status | |||||
| Married | 19 | 58 | 16 | 47 | χ 2 = 0.742 |
| Single | 14 | 42 | 18 | 53 | p = 0.389 |
| Living place | |||||
| City | 25 | 76 | 28 | 82 | χ 2 = 0.441 |
| Town | 8 | 24 | 6 | 18 | p = 0.507 |
| Occupation | |||||
| Labor‐officer | 19 | 58 | 19 | 56 | |
| Housewife | 5 | 15 | 4 | 12 | χ 2 = 1.122 |
| Retired | 2 | 6 | 2 | 6 | p = 0.891 |
| Unemployed | 2 | 6 | 1 | 3 | |
| Student | 5 | 15 | 8 | 23 | |
| Income status | |||||
| Income < expenses | 13 | 39 | 12 | 35 | χ 2 = 1.853 |
| Income = expenses | 19 | 58 | 18 | 53 | p = 0.396 |
| Income > expenses | 1 | 3 | 4 | 12 | |
| Previous hospitalization | |||||
| No | 18 | 54 | 15 | 44 | χ 2 = 1.298 |
| Once | 12 | 37 | 13 | 38 | p = 0.523 |
| Twice | 3 | 9 | 6 | 18 | |
| Chronic illness | |||||
| No | 7 | 21 | 7 | 21 | χ 2 = 0.004 |
| Yes | 26 | 79 | 27 | 79 | p = 0.950 |
| Smoke | |||||
| No | 10 | 30 | 14 | 41 | χ 2 = 0.906 |
| Yes | 19 | 58 | 17 | 50 | p = 0.636 |
| Give up smoking | 4 | 12 | 3 | 9 | |
| Drinking | |||||
| No | 30 | 91 | 31 | 91 | χ2 = 0.001 |
| Yes | 3 | 9 | 3 | 9 | p = 0.969 |
| Exercise regularly | |||||
| No | 27 | 82 | 24 | 71 | χ 2 = 1.162 |
| Yes | 6 | 18 | 10 | 29 | p = 0.281 |
| Age | 36.48 ± 11.63 | 33.15 ± 11.90 | t = 1.161 | ||
| p = 0.250 | |||||
Abbreviation: t, independent groups t test.
Table 2.
Comparison of the mean STAI scores of the experimental and control groups
| Experiment group (X ± SD) | Control group (X ± SD) | Test value and significance | |
|---|---|---|---|
| Pretest | |||
| State Anxiety Scale | 62.33 ± 8.33 | 60.68 ± 9.17 | t = 0.773 |
| p = 0.442 | |||
| Trait Anxiety Scale | 48.12 ± 5.22 | 45.35 ± 8.09 | t = 1.658 |
| p = 0.102 | |||
| Final test | |||
| State Anxiety Scale | 44.67 ± 5.41 | 61.29 ± 7.95 | t = −9.982 |
| p = 0.000 | |||
| Test value and significance | t = 10.618 | t = −0.453 | |
| p = 0.000 | p = 0.652 |
The experimental group's mean posttest score on the SAS was 44.67 ± 5.41, and the control group's mean posttest score on the SAS was 61.29 ± 7.95. A statistically significant difference was found between their mean posttest SAS scores. The mean posttest SAS score of the control group was higher than that of the experimental group (p < 0.05) (Figure 2).
Figure 2.
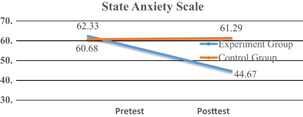
The variation of the mean State Anxiety Scale scores of the experimental and control groups by time of measurement [Color figure can be viewed at wileyonlinelibrary.com]
A statistically significant difference was found between the experimental group's mean pretest and posttest SAS scores. No significant differences were found between the mean pretest and posttest SAS scores of the control group.
The experimental group's mean posttest score on the RCSQ was 68.33 ± 14.53, and the control group's mean posttest score on the RCSQ was 46.71 ± 19.71. A statistically significant difference was found between their mean RCSQ scores. The mean posttest RCSQ score of the experimental group was higher than that of the control group (p < 0.05).
4. DISCUSSION
The psychological dimension of COVID‐19 has been ignored in the studies conducted with COVID‐19 patients.6, 8, 10 The diagnosis and treatment of COVID‐19‐related psychiatric conditions are recommended by clinical research; however, few intervention studies in the literature have attempted to eliminate the psychological problems of COVID‐19 patients. 23 Progressive muscle relaxation exercises were performed in this study to reduce or prevent the anxiety and sleep problems of patients with COVID‐19. Here, the results of this study are discussed along with the relevant literature.
The state anxiety levels of the experimental group decreased significantly compared with the control group (Table 2). The SAS determines how people feel at a specific time and under specific conditions. 31 Progressive muscle relaxation exercises may effectively reduce the anxiety of COVID‐19 patients concerning challenging situations such as hospitalization, treatment, and isolation. 23 Few studies of anxiety prevention for COVID‐19 patients have been conducted, even though the literature emphasizes that they experience high levels of anxiety. Liu et al. 23 administered progressive muscle relaxation exercises to COVID‐19 patients 30 min a day for 5 days and found that the exercises effectively reduced their anxiety levels. Manzoni et al. 34 did a 10‐year systematic review with meta‐analysis, which found that muscle relaxation training is consistently effective and should be considered to reduce anxiety. Volpato et al. 35 conducted a meta‐analysis of 25 randomized controlled studies of muscle relaxation exercises with chronic obstructive pulmonary patients (COPD) patients and found that the exercises effectively reduced anxiety. Turkish and international studies with different samples have also shown that progressive muscle relaxation exercises effectively reduce anxiety.29, 30, 31, 32, 33, 34, 35, 36, 37, 38 The results of this study are similar to those of other studies.
The sleep quality of the experimental group significantly increased compared with the control group (Table 3). This finding suggests that progressive muscle relaxation exercises are effective to eliminate sleep problems of COVID‐19 patients. Studies have shown that many patients experience serious sleep problems during COVID‐19 treatment.18, 19, 20, 21 However, only one study in the literature has reported that progressive muscle relaxation exercises improve the sleep quality of COVID‐19 patients. Liu et al. 23 found that progressive muscle relaxation exercises help improve the sleep quality of COVID‐19 patients. Previous studies of the respiratory system, which the virus can fatally affect, have shown that progressive muscle relaxation techniques lead to positive results. Yilmaz and Kapucu 39 ) did a systematic review of progressive muscle relaxation exercises with COPD patients and found that the exercises effectively reduce fatigue, anxiety, and depression, and improve sleep quality. Aksu et al. 24 found that progressive muscle relaxation exercises prevent the deterioration of the sleep quality of patients with pulmonary resection. Chegeni et al. 27 conducted a randomized controlled study with COPD patients and reported that progressive muscle relaxation exercises effectively reduce fatigue and improve subjective sleep quality.
Table 3.
Comparison of the mean RCSQ scores of the groups
| Experiment group (X ± SD) | Control group (X ± SD) | Test value and significance | |
|---|---|---|---|
| RCSQ | 68.33 ± 14.53 | 46.71 ± 19.71 | t = 5.100 |
| p = 0.000 |
Abbreviation: RCSQ, Richards–Campbell Sleep Questionnaire.
Studies of a variety of patient groups have shown that progressive muscle relaxation exercises effectively prevent sleep problems. Studies conducted with multiple sclerosis patients, 25 hemodialysis patients, 26 cancer patients, 40 and intensive care patients 41 have determined that progressive muscle relaxation exercises effectively improve sleep quality. The results of this study are similar to those of other studies.
Progressive muscle relaxation exercises can be considered a nonpharmacological method of reducing anxiety and improving sleep quality, and this is beneficial because the drugs used for the anxiety and sleep problems of COVID‐19 patients have a number of side effects that can prevent the monitoring of their symptoms.
5. IMPLICATIONS FOR NURSING PRACTICE
Progressive muscle relaxation exercises effectively reduced the anxiety and improved the sleep quality of patients with COVID‐19. Health‐care professionals should administer progressive muscle relaxation exercises to patients with COVID‐19.
CONFLICT OF INTERESTS
The authors declare that there are no conflict of interests.
AUTHOR CONTRIBUTIONS
Ibrahim Özlü, Zeynep Öztürk, Zeynep Karaman Özlü, Erdal Tekin and Ali Gür, were responsible for the conception and design of the study. İbrahim Özlü, Zeynep Öztürk, Zeynep Karaman Özlü, Erdal Tekin and Ali Gür were responsible for acquisition and analysis of data; furthermore, İbrahim Özlü was in charge of statistical analysis. İbrahim Özlü, Zeynep Öztürk, Zeynep Karaman Özlü, Erdal Tekin and Ali Gür, drafted the manuscript and approved the final version. All authors read and approved the final manuscript.
ACKNOWLEDGMENTS
The authors wish to thank and acknowledge the participants for sharing their experiences with us.
Özlü İ, Öztürk Z, Karaman Özlü Z, Tekin E, Gür A. The effects of progressive muscle relaxation exercises on the anxiety and sleep quality of patients with COVID‐19: a randomized controlled study. Perspect Psychiatr Care. 2021;57:1791–1797. 10.1111/ppc.12750
REFERENCES
- 1. World Health Organisation (WHO). Coronavirus disease (COVID‐19) Dashboard; 2020. https://covid19.who.int/
- 2. World Health Organisation (WHO). Coronavirus disease (COVID‐19) technical guidance; 2020. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/technical-guidance
- 3. Dhama K, Sharun K, Tiwari R, et al. COVID‐19, an emerging coronavirus infection: advances and prospects in designing and developing vaccines, immunotherapeutics, and therapeutics. Hum Vaccines Immunother. 2020;16(6):1‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Kim SW, Su KP. Using psychoneuroimmunity against COVID‐19. Brain Behav Immun. 2020;87:4‐5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Calder PC. Nutrition, immunity and Covid‐19. BMJ Nutr Prev Health. 2020;2020:1‐19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Kong X, Zheng K, Tang M, et al. Prevalence and factors associated with depression and anxiety of hospitalized patients with COVID‐19. MedRxiv. 2020. 10.1101/2020.03.24.20043075 [DOI] [Google Scholar]
- 7. Brooks SK, Webster RK, Smith LE, et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020;395(10227):14‐20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Mazza MG, De Lorenzo R, Conte C, et al. Anxiety and depression in COVID‐19 survivors: role of inflammatory and clinical predictors. Brain Behav Immun. 2020;89:594‐600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Speth MM, Singer‐Cornelius T, Oberle M, Gengler I, Brockmeier SJ, Sedaghat AR. Mood, anxiety and olfactory dysfunction in COVID‐19: evidence of central nervous system involvement? Laryngoscope. 2020;130(11):2520‐2525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Yang L, Wu D, Hou Y, et al. Analysis of psychological state and clinical psychological intervention model of patients with COVID‐19. medRxiv. 2020. 10.1101/2020.03.22.20040899 [DOI] [Google Scholar]
- 11. Wu Y, Xu X, Chen Z, et al. Nervous system involvement after infection with COVID‐19 and other coronaviruses. Brain Behav Immun. 2020;87:18‐22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Carvalho PM. The psychiatric impact of the novel coronavirus outbreak. Psychiatr Res. 2020;286(112902):10‐1016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Xiao H, Zhang Y, Kong D, Li S, Yang N. Social capital and sleep quality in individuals who self‐isolated for 14 days during the coronavirus disease 2019 (COVID‐19) outbreak in January 2020 in China. Med Sci Monitor Int Med J Exp Clin Res. 2020;26:e923921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Chong PY, Chui P, Ling AE, et al. Analysis of deaths during the severe acute respiratory syndrome (SARS) epidemic in Singapore: challenges in determining a SARS diagnosis. Arch Pathol Lab Med. 2004;128(2):195‐204. [DOI] [PubMed] [Google Scholar]
- 15. Huang Y, Zhao N. Generalized anxiety disorder, depressive symptoms and sleep quality during COVID‐19 outbreak in China: a web‐based cross‐sectional survey. Psychiatry Res. 2020;288:112954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Roy D, Tripathy S, Kar SK, Sharma N, Verma SK, Kaushal V. Study of knowledge, attitude, anxiety & perceived mental healthcare need in Indian population during COVID‐19 pandemic. Asian J Psychiatry. 2020;51:102083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Shanafelt T, Ripp J, Trockel M. Understanding and addressing sources of anxiety among health care professionals during the COVID‐19 pandemic. JAMA. 2020;323(21):2133‐2134. [DOI] [PubMed] [Google Scholar]
- 18. Vitale JA, Perazzo P, Silingardi M, Biffi M, Banfi G, Negrini F. Is disruption of sleep quality a consequence of severe Covid‐19 infection? A case‐series examination. Chronobiol Int. 2020;37(7):1110‐1114. [DOI] [PubMed] [Google Scholar]
- 19. Chen Y, Zhao A, Xia Y, et al. In the big picture of COVID‐19 pandemic: what can sleep do. Sleep Med. 2020;72:109‐110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Mao L, Jin H, Wang M, et al. Neurologic manifestations of hospitalized patients with coronavirus disease 2019 in Wuhan China. JAMA Neurol. 2020;77(6):683‐690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Zhang J, Xu D, Xie B, et al. Poor‐sleep is associated with slow recovery from lymphopenia and an increased need for ICU care in hospitalized patients with COVID‐19: a retrospective cohort study. Brain Behav Immun. 2020;88:50‐58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Mônico‐Neto M, dos Santos RVT, Antunes HKM. The world war against the COVID‐19 outbreak: don't forget to sleep!. J Clin Sleep Med. 2020;16:1215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Liu K, Chen Y, Wu D, Lin R, Wang Z, Pan L. Effects of progressive muscle relaxation on anxiety and sleep quality in patients with COVID‐19. Complement Ther Clin Pract. 2020;39:101132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Aksu NT, Erdogan A, Ozgur N. Effects of progressive muscle relaxation training on sleep and quality of life in patients with pulmonary resection. Sleep Breath. 2018;22(3):695‐702. [DOI] [PubMed] [Google Scholar]
- 25. Jalalmanesh SH, Zargarani F. Effects of progressive muscle relaxation technique on fatigue and sleep quality in patients with multiple sclerosis. Sci J Hamadan Nurs Midwifery Faculty. 2015;23(3):5‐14. [Google Scholar]
- 26. Saeedi M, Ashktorab T, Saatchi K, Zayeri F, Amir Ali Akbari S. The effect of progressive muscle relaxation on sleep quality of patients undergoing hemodialysis. Iran J Crit Care Nurs. 2012;5(1):23‐28. [Google Scholar]
- 27. Chegeni PS, Gholami M, Azargoon A, Pour AHH, Birjandi M, Norollahi H. The effect of progressive muscle relaxation on the management of fatigue and quality of sleep in patients with chronic obstructive pulmonary disease: a randomized controlled clinical trial. Complement Ther Clin Pract. 2018;31:64‐70. [DOI] [PubMed] [Google Scholar]
- 28. Kapucu S, Kütmeç YC. Kronik hastalıklarda progresif gevşeme egzersizlerinin yararı. FÜ Sağ Bil Tıp Derg. 2018;32(2):111‐114. [Google Scholar]
- 29. Yildirim YK, Fadiloglu C. The effect of progressive muscle relaxation training on anxiety levels and quality of life in dialysis patients. Edtna‐Erca J. 2006;32(2):86‐88. [DOI] [PubMed] [Google Scholar]
- 30. Spielberger CD, Gorsuch RL, ve Lushene RE. Manual for State‐Trait Anxiety Inventory. Palo Alto, CA: Consulting Psychologists Press; 1970. [Google Scholar]
- 31. Öner N, LeCompte A. Durumluk Sürekli Kaygı Envanteri El Kitabı (The Manual of State‐Trait Anxiety). Istanbul, Boǧaziçi Üniversitesi Yayınları. 1982. [Google Scholar]
- 32. Richards K. Techniques for measurement of sleep in critical care. Focus Crit Care. 1987;14(4):34. [PubMed] [Google Scholar]
- 33. Özlü ZK, Özer N. Richard‐Campbell Uyku Ölçeği Geçerlilik ve Güvenilirlik Çalışması. J Turkish Sleep Med. 2015;2:29‐32. [Google Scholar]
- 34. Manzoni GM, Pagnini F, Castelnuovo G, Molinari E. Relaxation training for anxiety: a ten‐years systematic review with meta‐analysis. BMC Psychiatry. 2008;8(1):41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Volpato E, Banfi P, Rogers SM, Pagnini F. Relaxation techniques for people with chronic obstructive pulmonary disease: a systematic review and a meta‐analysis. Evidence‐Based Complem Altern Med. 2015;2015:2015‐2022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Yilmaz SG, Arslan S, Arslan S. Effects of progressive relaxation exercises on anxiety and comfort of Turkish breast cancer patients receiving chemotherapy. Asian Pac J Cancer Prev. 2015;16(1):217‐220. [DOI] [PubMed] [Google Scholar]
- 37. Cheung YL, Molassiotis A, Chang AM. The effect of progressive muscle relaxation training on anxiety and quality of life after stoma surgery in colorectal cancer patients. Psycho‐Oncol J Psychol Soc Behav Dimens Cancer. 2003;12(3):254‐266. [DOI] [PubMed] [Google Scholar]
- 38. Dehdari T, Heidarnia A, Ramezankhani A, Sadeghian S, Ghofranipour F. Effects of progressive muscular relaxation training on quality of life in anxious patients after coronary artery bypass graft surgery. Indian J Med Res. 2009;129(5):603. [PubMed] [Google Scholar]
- 39. Yilmaz KC, Kapucu S. Use of progressive relaxation exercises in chronic obstructive pulmonary patients: a systematic review. Hacettepe Faculty Nurs J. 2019;6(2):65‐74. [Google Scholar]
- 40. Demiralp M, Oflaz F, Komurcu S. Effects of relaxation training on sleep quality and fatigue in patients with breast cancer undergoing adjuvant chemotherapy. J Clin Nurs. 2010;19(7‐8):1073‐1083. [DOI] [PubMed] [Google Scholar]
- 41. Richards K, Nagel C, Markie M, Elwell J, Barone C. Use of complementary and alternative therapies to promote sleep in critically ill patients. Crit Care Nurs Clin North Am. 2003;15(3):329‐340. [DOI] [PubMed] [Google Scholar]


