Abstract
Veno‐venous extracorporeal membrane oxygenation (VV ECMO) is an effective and proven adjunct support for various severe respiratory failures requiring invasive mechanical ventilation and cardiovascular support. In response to the rapidly increasing number of COVID‐19 patients in Japan, we launched an ECMO support team comprised of multidisciplinary experts including physicians, nurses, perfusionists, and bioethicists in preparation for the threat of a pandemic. From April 2 to July 15, 2020, Tokyo Medical and Dental University hospital treated 104 PCR confirmed COVID‐19 patients. Among those, 34 patients were admitted to intensive care unit (ICU) and 5 patients required VV ECMO. All management related to ECMO was decided by the ECMO support team in addition to participation of the ECMO support team in daily multidisciplinary rounds in the ICU. Median age was 54 years old. Duration from onset to mechanical ventilation (MV) and MV to ECMO were 8 and 7 days, respectively. Four patients (80%) were successfully weaned off from ECMO. One patient died after 81 days of ECMO run. Four patients were discharged and recovered to their prehospital quality of life without major disability. We achieved a high survival rate using ECMO in our low volume ECMO institution during the COVID‐19 pandemic. Multidisciplinary decision‐making and a team approach for the unclear pathology with an emerging infectious disease was effective and contributed to the survival rate.
Keywords: acute respiratory distress syndrome, coronavirus disease 2019, team approach, veno‐venous extracorporeal membrane oxygenation
High survival rate using ECMO for COVID‐19 achieved with multidisciplinary team approach.

1. INTRODUCTION
On March 11, 2020, the World Health Organization (WHO) declared the novel coronavirus (COVID‐19) outbreak a global pandemic. 1 Accordingly, Tokyo Metropolitan Government initiated systematic coordination with hospitals in the Tokyo area to secure sufficient intensive care unit (ICU) beds for critically ill COVID‐19 patients with advanced respiratory failure and to prepare for a potential shortage of medical resources under this dire situation. Prior to the pandemic, our university hospital was a tertiary referral center with a total of 753 beds to treat a wide range of complicated acute illnesses. Within these beds, there were 12 beds in general ICU and 14 beds in the Emergency Department ICU, 8 beds in High Care Units, and 16 beds in High Care Units for Emergency Department. High Care Units essentially function as a step‐down unit. In response to this political demand and societal responsibility, our hospital stopped all elective surgeries and admissions and overhauled all of the ICUs to be negatively pressurized with appropriate zoning measures to mitigate intrahospital transmission. Simultaneously, an ECMO support team was launched expediently to function as an overseeing committee to integrate decision to initiate ECMO, synthesize management, and formulate decisions whether to continue ECMO including the possibility of withdrawal of ECMO in view of optimal medical resource utilization. Members of the ECMO support team consisted of cardiovascular surgeons, pulmonologists, intensive care physicians, acute critical care physicians, ICU nurses, perfusionist, and a bioethicist.
The ECMO team constructed local regulatory guidelines and criteria for indication of initiation of ECMO according to available best evidence in conjunction with fundamental philosophy of ECMO in our hospital.
2. PATIENTS AND METHODS
From April 2 to July 15, 2020, in our hospital, 104 PCR confirmed COVID‐19 patients were treated. Among 34 critically ill patients requiring ICU management, 5 patients required ECMO.
Consent to use anonymized medical data for this retrospective case report were obtained from individual patients. Institutional Review Board (IRB) review was exempted since this case report does not meet the definition of “research” under the Ethical Guidelines for Medical and Health Research Involving Human Subjects. 2
2.1. Patient selection
Standard indications for ECMO including failure of treatment strategies (lung‐protective ventilation strategy with high positive end‐expiratory pressure (PEEP) and low tidal volume, diuretics to avoid fluid overload, muscular relaxant, and prone positioning prior to ECMO) in acute respiratory distress syndrome (ARDS) were applied for COVID‐19 patients with severe advanced respiratory failure. Worsening lung functions were regarded as ECMO indications; PaO2/FiO2 (P/F) less than 80 mm Hg for 6 hours or less than 50 for 3 hours, PaCO2 greater than 60 with pH less than 7.25 for 6 hours. Additionally, initiation of ECMO could be considered with P/F at 100 for cases with refractory hypoxia despite optimal care with prone positioning.
Patients equal to or greater than 75 years old were excluded for ECMO because of its known poor outcomes. Once conditions met the criteria, the ECMO support team meeting was held to discuss prognosis and merits from ECMO for the patient. Final decisions were made by ECMO support team. In case of an emergency, ECMO indication could be decided by at least one pulmonologist and two other ECMO support team physicians. However, a team meeting would be subsequently held to discuss the viability of the indication by all ECMO support team members.
In terms of anticoagulation therapy, we used nafamostat mesylate along with unfractionated heparin for two reasons. First, the usage was based on the report of a possible positive effect of nafamostat directly to the COVID‐19. 3 The other reason was the excessive thrombotic features of COVID‐19 that have been widely reported as part of the disease manifestation. 4 As a matter of fact, a considerable amount of unfractionated heparin was required to maintain target range of aPTT and ACT in our case series. Some papers are also referring utility of nafamostat for extracorporeal circulation. 5 , 6
2.2. Discontinuation
When PaO2 and PaCO2 were acceptable with increased ventilator support for at least 3 hours after sweep gas was weaned off, ECMO was discontinued and vascular cannulas were removed at bedside with manual compression and single U‐shape stitches for each puncture site.
2.3. Cessation
The maximum duration of ECMO was initially set at 21 days in consideration of poor prognosis with prolonged ECMO. 7 It was also decided in the local regulatory guidelines that if a patient required ECMO exceeding 21 days, ECMO support team committee would be held twice a week to determine whether ECMO continuation would be appropriate. Additionally, younger and patients with fewer comorbid conditions were preferred for ECMO support. Due to consideration of possible shortage of ECMO capabilities in our hospital and in the greater Tokyo Metropolitan area, we included the potential for redistribution of ECMO to patients with higher likelihood of survival in our criteria which was subsequently adopted as hospital policy. Furthermore, we integrated the palliative care team from our hospital into the ECMO support team and developed a palliative care protocol to provide the best supportive care if cessation of ECMO was decided for any reason.
3. RESULTS
3.1. Indications of ECMO
During the period from April 2 ‐ July 15, three patients, one octogenarian and two late 70s, were excluded from ECMO indication and died of respiratory failure complicated by bacterial infections along with primary COVID‐19 pneumonia.
For the five patients who underwent ECMO, patient characteristics with details of treatments and outcomes are outlined in Table 1. Four (80%) of five patients were male. Median duration from mechanical ventilation (MV) initiation to ECMO initiation was 7 days (IQR 6‐9).
TABLE 1.
Patient characteristics
| Case number | #1 | #2 | #3 | #4 | #5 |
|---|---|---|---|---|---|
| Age, years | 54 | 53 | 66 | 57 | 30 |
| Sex | Male | Male | Male | Male | Female |
| BSA (m2) | 1.94 | 1.89 | 1.83 | 1.85 | 1.65 |
| BMI (kg/m2) | 26.4 | 24.7 | 24.3 | 23.9 | 21.6 |
| Onset to MV (days) | 8 | 11 | 9 | 6 | 8 |
| MV to ECMO (days) | 6 | 9 | 7 | 19 | 6 |
| Comorbidities | DLP, heavy smoker | DM | HTN, ex‐Smoker | Asthma, HTN, DLP, COPD | Postpartum |
| CRRT before ECMO | Yes | Yes | |||
| Medication for COVID‐19 | Favipiravir, HCQ, Ciclesonide, Tocilizumab | Favipiravir, HCQ, Tocilizumab | Favipiravir, HCQ, Tocilizumab, steroid pulse, and IVIG | Favipiravir, HCQ | Favipiravir, HCQ, Ciclesonide, Tocilizumab, steroid pulse, and IVIG |
| Indications (before ECMO) | |||||
| PEEP | 10 | 12 | 16 | 10 | 15 |
| P/F | 141 | 127.5 | 42.6 | 137 | 99.6 |
| PaCO2 | 80.6 | 125 | 38.6 | 62.1 | 47.2 |
| pH | 7.213 | 7.049 | 7.359 | 7.269 | 7.404 |
| LDH | 339 | 379 | 1205 | 389 | 574 |
| Other | Hemodynamic instability with acidosis | Acidosis | Hypoxia | Pneumothorax | Progressive worsening |
| ECMO settings | |||||
| Outflow site | Rt IJ | Rt IJ | Rt FV | Rt IJ | Rt IJ |
| Cannula size, depth | 19 Fr, 12 cm | 19 Fr, 12 cm | 19 Fr, 46 cm | 19 Fr, 13 cm | 17 Fr, 13 cm |
| Drainage site | Rt FV | Rt FV | Lt FV | Lt FV | Rt FV |
| Cannula size, depth | 24 Fr, 45 cm | 24 Fr, 43 cm | 24 Fr, 39 cm | 24 Fr, 47 cm | 24 Fr, 43 cm |
| Plateau ECMO Flow (mL/kg) | 66.7 | 68.5 | 65.6 | 70.8 | 76.6 |
| Pump exchange | 1 | – | 3 | – | – |
| Cannula exchange | – | – | Yes a | – | – |
| Anticoagulation | |||||
| Heparin b (unit/kg/hr) | 15.7 | 16.2 | 11.7 | 22.1 | 21.2 |
| Nafamostat b (mg/kg/hr) | 0.021 | 0.016 | 0.029 | 0.017 | 0.014 |
| Outcomes | |||||
| ECMO duration | 21 | 9 | 81 | 9 | 8 |
| P/F after ECMO | 229 | 356 | 333 | 210 | |
| PaCO2 after ECMO | 54.5 | 44.6 | 50.7 | 50.8 | |
| Outcome | Discharged | Discharged | Died on ECMO | Discharged | Discharged |
| Complications during ECMO | |||||
| Hemorrhagic event | Hematuria | – | Intramuscular hemorrhage | – | Intramuscular hemorrhage |
| Hemopneumothorax | |||||
| Thrombotic event | – | – | – | – | – |
Abbreviations: BMI, body mass index; BSA, body surface area; COPD, chronic obstructive pulmonary disease; CRRT, continuous renal replacement therapy; DLP, dyslipidemia; DM, diabetes mellitus; FV, femoral vein; HCQ, hydroxychloroquine; HTN, hypertension; IJ: internal jugular vein; IVIG: intravenous immunoglobulin therapy; LDH, lactate dehydrogenase; Lt, left; P/F, PaO2/FiO2; MV, invasive mechanical ventilation; Rt, right.
The initial cannulas were suspected to be infected with Staphylococcus aureus and exchanged to a new dual lumen single catheter via right internal jugular vein after 30 days of support.
Maximum dose.
Main reason for indication in cases #1 and #2 were hypercarbia and acidosis. Case #3 developed severe hypoxia. Case #4 developed extensive pneumothorax with aggressive high‐PEEP ventilation with placement of a chest tube resulting in massive air leak. To minimize airway pressure, ECMO was useful. Following ECMO initiation, 3 days of zero PEEP substantially worked to cure pneumothorax.
For case #5, relatively early indication was decided for progressive worsening in conjunction with patient’s young age and expectation as a mother of the newborn infant.
In regard to medications for COVID‐19, Favipiravir, Hydroxychloroquine, Ciclesonide as inhaled glucocorticoid, Tocilizumab, intravenous steroid pulse therapy, and intravenous immunoglobulin therapy were used prior to ECMO.
3.2. Cannulations
All cannulations except one cannula exchange to AVALON double‐lumen catheter (Maquet Cardiopulmonary GmbH, Rastatt, Germany) were done at the bedside with ultrasound guided puncture followed by portable x‐ray guided wire/cannula placement.
The direct digital radiography with a digital flat panel detector which has the ability to transmit pictures wirelessly enabled us to take x‐rays repeatedly without drawing the panel out of the patient back. Accordingly, this allowed us to take repeated x‐rays during each step of wire placement and cannula advancement which provided safe and accurate cannulation similar to guidance under fluoroscopy. In the setting of ICU where the C‐arm is not available, this technique was certainly effective and practical. Especially for COVID‐19 patients, transfer to cath lab or OR raises concerns of possible inadvertent transmission of virus to the environment and/or health care personnel.
In most cases, cannulations to femoral vein and right jugular vein for IVC drainage and blood return to right atrium were done, respectively. In a case with suspected narrowing at the junction of superior vena cava and common jugular vein, cannulations were performed via bilateral femoral approach. The tip of the venous drainage cannulas were placed at the lower end of the right atrium in all cases to achieve adequate venous drainage.
Nine ECMO systems were available in our hospital before the pandemic. Five were Capiox EBS EMERSAVE (TERUMO, Tokyo, Japan) and other four were MERA Centrifugal Blood Pump System HCS‐CFP (Senko Medical Instruments, Tokyo, Japan). One additional Capiox system was acquired to make provisions against COVID‐19 patient surge. Capiox system was used in four patients (case #1, #2, #3, and #5) and MERA was used in one (case #4). The ECMO flow and sweep gas were titrated to keep arterial oxygen saturation more than 90% and an acceptable pH. Pressure of pre‐ and post‐centrifugal pump was continuously monitored to maintain adequate blood flow. If the pre‐pump pressure was significantly depressed, fluid was intravenously given or ECMO blood flow was lowered.
3.3. Management during ECMO
During the ECMO run, multidisciplinary rounds and discussions were held twice daily in the morning and evening. To minimize ventilator‐induced lung injury, lung rest strategy with low tidal volume was employed when the inflammation in the lungs was intense. Airway occlusion pressure (P0.1) and respiratory compliance were used to estimate lung function recovery.
Anticoagulation with unfractionated heparin and nafamostat mesylate was initiated with a target activated clotting time (ACT) of 160 to 180 seconds. Activated partial thromboplastin time (aPTT), prothrombin time (PT), antithrombin III, fibrinogen, platelet count, and D‐dimer were monitored simultaneously. Thromboelastography (TEG) was also utilized to make better clinical judgment from multiple perspectives.
All patients could reach sufficient blood flow (>60 mL/kg) to support lethal respiratory failure.
Most of the cases required antimicrobials during and after ECMO for bacterial and viral infections other than the novel coronavirus.
3.4. Discontinuation
Four patients were successfully weaned from ECMO and decannulated after at least 3 hours of sweep gas discontinuation for proving lung recovery. Two patients required tracheostomy at 7 and 11 days after discontinuation of ECMO for prolonged mechanical ventilation. None of them developed serious sequela. All of the four patients were discharged to other referral hospitals for rehabilitation followed by returning to their own previous life without major disability. Transition of P/F ratio and O2 administration are shown in Figure 1. The O2 administration amount is defined by following formula:
FIGURE 1.
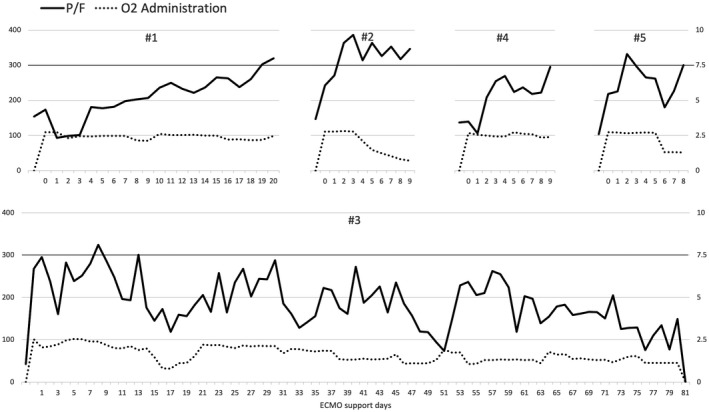
Transition of P/F ratio (black line) scaled on left side vertical axis (mm Hg) and O2 administration (dotted line) scaled on right side vertical axis (L/min ・ m2) for each patient. The O2 administration is calculated following formula: Oxygen administration = (sweep gas oxygen fraction) × (ECMO blood flow: L/min)/(BSA: body surface area: m2)
The calculation is a simplified estimation of the amount of given O2. Recirculation between inflow and outflow cannulas should be considered to utilize the formula into clinical judgment. In case #1, slow constant P/F improvement was observed followed by successful removal of ECMO after reaching P/F ratio of 300 at 21 days after ECMO initiation. Case #2 achieved P/F ratio of 300 a few days after ECMO initiation. ECMO was weaned and discontinued without a decline in P/F ratio during weaning. Case #4 spent a few days with zero PEEP to treat pneumothorax. Stepwise PEEP elevation without recurrent pneumothorax led to P/F ratio improvement and successful ECMO discontinuation. Despite reaching P/F ratio of 300 soon after the ECMO initiation, case #5 showed a decline in P/F ratio with infiltration on x‐ray after the initial improvement. Additional intravenous immunoglobulin (IVIG) therapy induced following P/F improvement resulted in successful ECMO discontinuation. 8 All patients except case #3 could maintain P/F ratio around 300 before ECMO discontinuation, whereas case #3 could not maintain the level of P/F ratio despite lung‐protective ventilation and finally expired after being placed on palliative care.
Case #3 required ECMO exceeding 21 days for insufficient lung recovery. Although 21 days was initially decided as the maximum duration of ECMO support for COVID‐19, the ECMO support team committee took place twice a week to discuss whether ECMO continuation would be appropriate in accordance with local regulatory guidelines. There were two main reasons why ECMO was continued over 21 days for the patient. First, the first pandemic wave was going to be converged and hospital and regional medical resources were not in a state of scarcity at the moment. Second, patient lung condition presumed by multiple CT scans showed possible reversibility. The patient repeatedly developed septicemia induced by immunosuppressant and hemopneumothorax that required chest tube drainage and ultimately a surgical closure of bronchopulmonary fistula. However, the patient died after 81 days of ECMO run with an agreement of withdrawal with the patient’s family for irreversible lung damage. All available best supportive care was implemented according to the palliative care protocol we had built in advance.
4. DISCUSSION
The real‐time and accurate monitoring of the number of COVID‐19 patients by Tokyo Metropolitan Government provided our group sufficient time to establish a detailed strategy of ECMO as a hospital policy. The team approach with intensive discussions made it possible to achieve our decent outcomes in the setting of a pandemic. One of the pertinent factors to achieve good outcomes requires implementing and maintaining ECMO without major complications. Appropriate treatment of pneumonia by pulmonologists, high‐quality intensive care by acute critical care physicians, intensivists, and nurses, and safe ECMO initiation and management by cardiac surgeons and perfusionists are necessary for the most critically ill patients with COVID‐19. 9 Moreover, minimizing complications during extracorporeal circulation is routine work for cardiac surgeons. We perform approximately 30 to 40 cases of veno‐arterial ECMO and 5 to 10 cases of VV ECMO per year on average in our center which is not a number associated with high‐volume ECMO centers. However, the result we report here is not inferior to other reports. 10 , 11 , 12 , 13 , 14 ECMO as a medical resource should not be limited only in a few large ECMO centers. Most cardiac centers possess enough resources including highly trained cardiac care nurses and perfusionists. In such pandemic situations, on site best practice with a multidisciplinary team approach is necessary for saving many lives.
Duration from initiation of mechanical ventilation (MV) to ECMO initiation was relatively longer than previous reports. 10 , 11 , 12 , 13 , 14 , 15 We suspect sophisticated ventilation strategies that were available may have contributed to longer time from MV initiation to ECMO initiation. Adequate medical management of COVID‐19 also decreased chances of urgent ECMO. Although our policy recommended patients with prolonged mechanical ventilation may not be a good candidate for ECMO, we ultimately proceeded with use of ECMO with cases with prolonged ventilation after careful reconsideration in conjunction with sufficient medical resources for ECMO. Despite this, we were able to observe an excellent outcome in the majority of our patients.
In a case with extensive pneumothorax (#4) with necessary high‐PEEP ventilation, drainage with a chest tube was not enough to maintain lung functions. After introduction of ECMO, PEEP was decreased to 0 cmH20 for 3 days and was gradually increased without recurrent air leak. ECMO was successfully discontinued after 9 days of ECMO run. Pneumothorax with aggressive mechanical ventilation could also be a good indication of ECMO. 16
Since there is not enough evidence, the criterion of ECMO weaning is still controversial. 17 , 18 Moreover, it is difficult to estimate patient lung recovery under low tidal volume “lung rest” ventilation. Graphical transition of P/F ratio (Figure 1) was helpful in making the decision of ECMO weaning. Maintaining P/F ratio greater than 300 during ECMO was used as a marker of sufficient lung recovery for starting ECMO weaning trial.
We used nafamostat as adjunctive medicine to heparin. As the mechanism of thrombosis in COVID‐19 becomes more evident, we should have a better understanding of which anticoagulation regimen would be most efficient and safe for ECMO in these patients. In the case with our longest ECMO, intramuscular hemorrhage around the shoulders subsequently required intravascular interventional coiling. We surmise the possibility of prone positioning along with muscular relaxant in addition to anticoagulation as potential contributing factors. Higher rate of hemorrhagic stroke and microbleeds are also reported in cases with COVID‐19. 19 , 20 Anticoagulation management will certainly influence patient outcomes.
ECMO remains a limited medical resource and cessation is necessary when the ECMO treatment is futile for reasons like irreversible brain damage. If the shortage became a real threat due to worst case scenario, redistribution of ECMO would have been considered for reallocation to provide effective utilization of limited medical resources. Fortunately, we have not encountered this difficult scenario. Prior to ECMO initiation, the possibility of cessation of ECMO was explained to the family and a written consent obtained for documentation.
5. CONCLUSION
We achieved satisfactory survival rate for critically ill COVID‐19 patients who required ECMO during the pandemic. Our platform of a multidisciplinary team approach which translated into detailed medical management for an emerging infectious disease was effective. Veno‐venous ECMO for acute respiratory distress syndrome is feasible in a low volume ECMO center and should not be limited to a small number of high‐volume centers during global pandemics.
CONFLICT OF INTEREST
The authors declare that they have no conflicts of interest with the contents of this article.
AUTHOR CONTRIBUTIONS
E. Nagaoka mainly wrote this article and also performed data analysis and interpretation. H. Arai organized the ECMO support team which played the most important role in this article. T. Ugawa, T. Masuda. K. Ochiai. M. Tamaoka, N. Kurashima, K. Oi, and T. Fujiwara contributed with clinical judgment for the patients in this article. M. Yoshida is the responsible person of the ethical committee of our university hospital and played an important role in making ethical decisions for the series of patients. H. Shigemitsu and Y. Otomo are chiefs of the clinical departments and had responsibilities for the series of patients.
ACKNOWLEDGMENTS
The authors are very grateful to all medical workers related to treatment of COVID‐19 patients in our university hospital ICU for their dedicated patient care regardless of their own infection risk.
Nagaoka E, Arai H, Ugawa T, et al. Efficacy of multidisciplinary team approach with extracorporeal membrane oxygenation for COVID‐19 in a low volume ECMO center. Artif Organs. 2021;45:1061–1067. 10.1111/aor.13947
For importance of multidisciplinary team, 11 authors are listed.
REFERENCES
- 1. WHO Director‐General's opening remarks at the media briefing on COVID‐19 ‐ 11 March 2020. Available from: https://www.who.int/dg/speeches/detail/who‐director‐general‐s‐opening‐remarks‐at‐the‐media‐briefing‐on‐covid‐19‐‐‐11‐march‐2020 [Accessed 15th January 2021].
- 2. Ethical guidelines for medical and health research involving human subjects. Available from: https://www.mhlw.go.jp/file/06‐Seisakujouhou‐10600000‐Daijinkanboukouseikagakuka/0000080278.pdf [Accessed 15th January 2021]. [Google Scholar]
- 3. Hoffmann M, Schroeder S, Kleine‐Weber H, Müller MA, Drosten C, Pöhlmann S. Nafamostat mesylate blocks activation of SARS‐CoV‐2: new treatment option for COVID‐19. Antimicrob Agents Chemother. 2020;64:e00754‐20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Paranjpe I, Fuster V, Lala A, Russak A, Glicksberg BS, Levin MA, et al. Association of treatment dose anticoagulation with in‐hospital survival among hospitalized patients with COVID‐19. J Am Coll Cardiol. 2020;76:122–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Nagaya M, Futamura M, Kato J, Niimi N, Fukuta S. Application of a new anticoagulant (nafamostat mesilate) to control hemorrhagic complications during extracorporeal membrane oxygenation—a preliminary report. J Pediatr Surg. 1997;32:531–5. [DOI] [PubMed] [Google Scholar]
- 6. Lim JY, Kim JB, Choo SJ, Chung CH, Lee JW, Jung SH. Anticoagulation during extracorporeal membrane oxygenation; nafamostat mesilate versus heparin. Ann Thorac Surg. 2016;102:534–9. [DOI] [PubMed] [Google Scholar]
- 7. Bartlett RH, Ogino MT, Brodie D, McMullan DM, Lorusso R, MacLaren G, et al. Initial ELSO guidance document: ECMO for COVID‐19 patients with severe cardiopulmonary failure. ASAIO J. 2020;66:472–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Takayama W, Endo A, Yoshii J, Arai H, Oi K, Nagaoka E, et al. Severe COVID‐19 pneumonia in a 30‐year‐old woman in the 36th week of pregnancy treated with postpartum extracorporeal membrane oxygenation. Am J Case Rep. 2020;28:e927521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Rafiq MU, Valchanov K, Vuylsteke A, Taghavi FJ, Iyer SB, Sudarshan CD, et al. Regional extracorporeal membrane oxygenation retrieval service during the severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2) pandemic: an interdisciplinary team approach to maintain service provision despite increased demand. Eur J Cardiothorac Surg. 2020;58:875–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Zeng Y, Cai Z, Xianyu Y, Yang BX, Song T, Yan Q. Prognosis when using extracorporeal membrane oxygenation (ECMO) for critically ill COVID‐19 patients in China: a retrospective case series. Version 2. Crit Care. 2020;24:148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Li X, Guo Z, Li B, Zhang X, Tian R, Wu W, et al. Extracorporeal membrane oxygenation for coronavirus disease 2019 in Shanghai, China. ASAIO J. 2020;66:475–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Osho AA, Moonsamy P, Hibbert KA, Shelton KT, Trahanas JM, Attia RQ, et al. Veno‐venous extracorporeal membrane oxygenation for respiratory failure in COVID‐19 patients: early experience from a major Academic Medical Center in North America. Ann Surg. 2020;272:e75–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Barbaro RP, MacLaren G, Boonstra PS, Iwashyna TJ, Slutsky AS, Fan E, et al. Extracorporeal membrane oxygenation support in COVID‐19: an international cohort study of the Extracorporeal Life Support Organization registry. Lancet. 2020;396:1071–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Zayat R, Kalverkamp S, Grottke O, Durak K, Dreher M, Autschbach R, et al. Role of extracorporeal membrane oxygenation in critically Ill COVID‐19 patients and predictors of mortality. Artif Organs. 2020. Nov 24. 10.1111/aor.13873. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Jäckel M, Rilinger J, Lang CN, Zotzmann V, Kaier K, Stachon P, et al. Outcome of acute respiratory distress syndrome requiring extracorporeal membrane oxygenation in Covid‐19 or influenza: a single‐center registry study. Artif Organs. 2020. Nov 14. 10.1111/aor.13865. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Nakatsutsumi K, Sekiya K, Urushibata N, Hosoi M, Arai H, Nagaoka E, et al. A successful case of extracorporeal membrane oxygenation treatment for intractable pneumothorax in a patient with COVID‐19. Acute Med Surg. 2020;7:e612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Broman LM, Malfertheiner MV, Montisci A, Pappalardo F. Weaning from veno‐venous extracorporeal membrane oxygenation: how I do it. J Thorac Dis. 2018;10 Suppl 5:S692–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Swol J, Shekar K, Protti A, Tukacs M, Broman LM, Barrett NA, et al. Extubate before VV ECMO decannulation or decannulate while remaining on the ventilator? The EuroELSO 2019 Weaning Survey. ASAIO J. 2020. Jul 17. 10.1097/MAT.0000000000001237. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 19. Schmidt M, Hajage D, Lebreton G, Monsel A, Voiriot G, Levy D, et al. Extracorporeal membrane oxygenation for severe acute respiratory distress syndrome associated with COVID‐19: a retrospective cohort study. Lancet. Respir Med. 2020;8:1121–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Koralnik IJ, Tyler KL. COVID‐19: a global threat to the nervous system. Ann Neurol. 2020;88:1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]


