Abstract
Objectives
The current study aims to investigate the aerosol and spatter mitigation quality of 13 dry‐field isolation methods in a simulated setup that replicates real‐life work scenarios encountered in dental practices.
Methods
A crown preparation on a manikin was performed on tooth number 30 and repeated five times for each setup to simulate a patient under care. Aerosol, environmental, and operator face shield spatter, and sound intensity was measured. Generalized linear mixed models were used, and posthoc pairwise comparisons were performed to compare least‐squares means when appropriate using a Tukey adjustment.
Results
All tested setups showed some environmental spatter formation; however, these were able to control most (and in some cases all) spatter on the operator face shield. All methods resulted in excellent aerosol mitigation when a second line of high‐volume evacuation (HVE) was added to the device setup. However, in most setups, total sound levels exceeded 85 dB, posing a concern for prolonged noise exposure.
Conclusions
The Prototype device and four other tested setups with secondary HVE addition completely eliminated aerosol creation as tested. Spatter of the Face Shield was best eliminated using the Prototype device.
Clinical Significance
Within the limitations of this study, it can be concluded that the dental community has at its disposal equipment that can effectively mitigate aerosol and spatter.
Keywords: aerosol mitigation, COVID‐19, environmental spatter, face shield spatter, SARS‐CoV‐2, total sound level (TSL)
1. INTRODUCTION
The effect of SARS‐CoV‐2 in dentistry has been particularly concerning. 1 , 2 The SARS‐CoV‐2 virus appears to be unique compared to other viruses. The virus apparently can spread in the absence of clinical symptomology, or more likely, the symptoms may be so subtle that it is often unrecognized by those who are affected or their caretakers. 3 , 4
It was submitted that one of the primary mechanisms of SARS‐CoV‐2 virus transmission is via aerosols 5 , 6 known to be generated throughout dental procedures. 7 , 8 , 9 , 10 , 11 , 12 It has been shown that the SARS‐CoV‐2 virus can be detected in the saliva of affected patients. 13 , 14 The virus binds to the human angiotensin‐converting enzyme‐2 receptor, 14 , 15 that is highly concentrated in human salivary glands and ducts, leading to the postulate that the SARS‐CoV‐2 virus is transmitted via salivary droplets. 15 , 16 Furthermore, SARS‐CoV‐2 RNA has been detected in saliva for 37 days after onset. 17
Spatter (mists) consists of droplets up to 50 μm in size that sink quickly, whereas aerosols are defined as droplet particles smaller than 5 μm that can remain airborne for extended periods. These small particles can reach deep into the bronchioles and have been reported to be significant in viral infections. 18 , 19 , 20 Therefore, these drops might contain infectious particles that pose a health threat to those within the spray's pattern. 21 , 22 , 23 , 24 It is reasoned, therefore, that aerosol generation from the use of a dental handpiece or an ultrasonic scaler in a patient's mouth has, at least in theory, the potential of transmitting the virus, 7 , 8 , 9 , 10 , 11 , 25 , 26 , 27 , 28 , 29 , 30 even though to date no conclusive evidence of viral transmission occurring in a dental treatment environment has been documented. 31 The half‐life of SARS‐CoV‐2 in aerosols is reported to be approximately 1.1–1.2 h and larger droplets settled on surfaces as spatter have a median half‐life of 5.6 h. 32
Therefore, this issue has raised a concern about the potential spread of the virus in the dental setting and has contributed to the need for the development of aerosol and spatter mitigation strategies.
In response to this challenge, new devices were introduced into the dental market. In a previous paper, 33 eight dry‐field isolation methods were tested in a typodont setup in which air‐water spray was generated with a high‐speed handpiece without cutting teeth. Although standardized procedures were employed, the study was limited in that it did not reproduce real‐life work scenarios. The current study aims to investigate the mitigation quality of 13 dry‐field isolation methods in a simulated real‐life setup that more closely replicates work scenarios encountered in dental practices.
This study attempts to compare the effectiveness of the following techniques:
High‐volume evacuation—(HVE)
Rubber dam (RD) with HVE (RD and HVE)
Prototype 3D printed lip retractor with internal suction and funnel (PROTO) (Figure 1)
PROTO with additional HVE line (PROTO and HVE)
AeroSol away external vacuum device (AA)
AA with additional HVE line (AA and HVE)
IsoVac (ISO)
ISO with additional HVE line (ISO and HVE)
ReLeaf (ReLeaf)
ReLeaf with additional HVE line (ReLeaf and HVE)
Vac Station 8 cm away from mouth (VAC8)
VacStation 15 cm away from mouth (VAC15)
Vac Station 15 cm away from mouth plus HVE line (VAC15 and HVE)
FIGURE 1.

Diagram showing the 3D printed prototype retraction and funnel device (PROTO)
2. MATERIALS AND METHODS
Methods were adapted from Dahlke et al. 34 with one significant modification; in the current study, a crown preparation was performed on tooth number 30 and repeated five times for each device.
2.1. Manikin
An oral anesthesia manikin head (model 1KOATM13, Columbia Dentiform Teaching Solutions, Inc., Lancaster, PA) with a metal skull, movable tongue, and flexible silicone face and mouth lining over an anatomically correct jaw with 28 permanent typodont teeth was selected to simulate the patient. The simulator was attached to a dental chair's headrest in the usual working position where the maxillary occlusal plane was perpendicular to the floor. Tooth #30 was selected for each test for crown preparation.
2.2. Grid around manikin
A custom four by three‐foot wooden board with black plastic coating was cut to fit around the manikin head and marked with a grid to score the spatter (Figure 2). The grid was created with florescent tape fixed tightly at 5 cm intervals to create areas of 5 cm2. One clinician performed all crown preparations on tooth #30. Each preparation was completed in 2 min, with the operator sitting at the 8 o'clock position at a standard distance from the patient of 40 cm.
FIGURE 2.
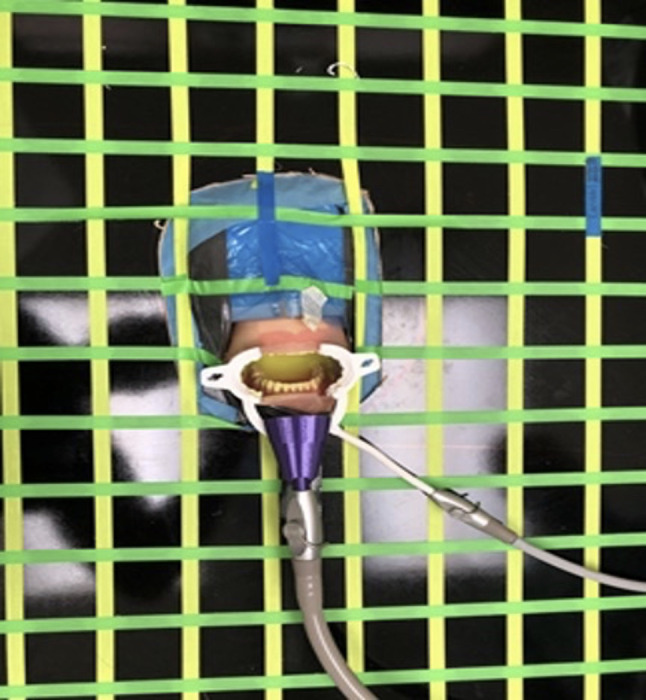
The spatter grid adapted around the manikin head. PROTO device is pictured in place in this image
2.3. Handpiece
A single high‐speed handpiece (NSK Ti‐Max X95L, Hoffman Estates, IL) was used and operated at the maximum torque and rotation speed of 200,000 revolutions per minute. The water flow through the handpiece was set at 25 ml/min, and the air pressure was selected to achieve an aerosol plume. The standard all‐ceramic crown preparation was done using a diamond bur 878K016 (Brasseler USA, Savannah, GA) placed in the dental handpiece.
2.4. Suction device setups
The dental chair (ADEC, Newberg, OR) setup used in this investigation is equipped with two separate HVE lines and one saliva ejector line. The following settings were used:
In this setup, and whenever a secondary HVE was used in our testing, a conventional disposable vented tip (Henry Schein, Melville, NY) was used in one of the HVE lines and positioned 4 cm from the tooth to be prepared.
A 3D printed internally irrigated retraction device (PROTO) was created with the Prusa MK3s 3D printer using Prusament PLA (Prusa Research, Prague, Czech Republic) with a layer height of 100 mm, extruder temperature of 220°C, and a bed temperature of 68°C with an infill of 100%. The frame included suction ports attached to the saliva ejector and the HVE line (Figures 1 and 2).
Conventional dental RD trials involved using a standard 6‐in. non‐latex dental dam (Flexi Dam, Coltène/Whaledent, Inc., Cuyahoga Falls, OH) punched with five holes to isolate teeth #27–31.
For the ISO (Zyris, Santa Barbara, CA) trials, a medium‐size mouthpiece was used to obtain the best fit for the dental simulator head. The device was used alone and in conjunction with an HVE
The Aegis Aerosol VacStation (VAC) (CAO Group, Inc., West Jordan, UT) was tested at 8 (VAC8) and 15 (VAC15) cm from the manikin mouth. The VAC15 setup was tested alone and also in conjunction with a second HVE line, while the VAC8 was only tested by itself.
AA, AeroSol Away Auburn California, also was tested alone or in conjunction with HVE.
The Ivory® ReLeaf™ (Kulzer North America, South Bend, IN) is a device designed to rest in the buccal vestibule and provide additional suction. Similar to the ISO device, yet without a mouth prop, it attaches to an HVE line. The ReLeaf device was tested alone and in conjunction with an additional HVE line.
2.5. Measurements
1.Environmental Spatter: A 0.1% fluorescein dye solution (Sigma‐Aldrich, St. Louis, MO) was added to the dental unit water supply for use during the simulated tooth preparation procedure.
The resulting spatter that escaped suction during the high‐speed handpiece operation was visualized with a light‐emitting diode dental curing light (Elipar™ S10, 3 M, Inc., St. Paul, MN) emitting blue light with a spectral range of between 425 and 500 nm. The diode was held 8 cm from the paper's surface to fluoresce spatter droplets that had collected, and visualization was achieved using amber‐colored protective glasses (Figure 3).
FIGURE 3.

Fluorescence Spatter after a test run. Grid is covered with new paper prior to each test run
A calibrated operator reviewed the droplet field created during the trials. If even one spot of fluorescence was identified within a 5 cm2 square, the cell was then scored as being contaminated. The number of squares with contamination were counted to determine the amount of spatter produced in each trial. Spatter generated using the high‐speed handpiece with no suction served as the positive control value.
2.Face shield spatter: A grid was placed on a Face Shield (ZShield Health, ZVerse, Columbia, SC) worn by the operator during preparation of the typodont tooth in the manikin. The grid squares were 5 cm2 in area and were created using the same fluorescent tape. If one spatter was detected in a grid cell, it was counted as positive (Figure 4).
FIGURE 4.

The face shield contained a grid pattern. In the simulated case illustrated, the sample run would score a three because three squares contain spatter
3.Aerosol: Aerosol particles were measured using a real‐time laser particle counter device (Casella Microdust Pro Aerosol Monitoring System, CEL712 Buffalo, NY) held 4 cm away from the orifice of the mouth. The atmospheric particulate matter with a diameter of less than 2.5 μm was recorded. Results were displayed in mg/m3 units. The unit was calibrated before starting the experiments by running a 10‐min calibration cycle in open fresh air.
Particle counts were read and recorded for 2 min during the crown preparation procedure. The use of the high‐speed handpiece with no suction served as the positive control value. In contrast, negative control values were obtained by measuring the ambient air in the experimental room when no experiments were performed.
4.Sound: Soundmeter X by Faberacustical running on an iPhone X was used to measure decibels (dB) at a distance of 6 in. from the soft tissue glabella area of the mannequin head. During each experiment, a 30‐s noise measurement was made for each tested device, with the noise level recorded over a wide range of frequencies between 20 and 20,000 Hz. Between 2 and 8 kHz, sounds are perceived as 10–20 dB louder than outside this range at the same intensity 35 and in this frequency range, we also find essential parts of speech information. 36 For the analysis, we are reporting the total sound level (TSL) as computed by the application. We do not report the sound for the setup HVE and RD because we found it sufficient to report HVE alone. The same approach was implemented for the VAC setup, for which we only report sound measured when the VAC was placed 15 cm from the manikin mouth, that is, VAC15.
2.6. Statistical analysis
Based on previous publications, 34 it was determined that five trials were necessary for each setup to achieve a power of 0.80 (effect size = 0.20; p < 0.05). For each outcome (Aerosol, Environmental, and Face Shield Spatter and Sound), generalized linear mixed models were used to look at differences between groups. A random intercept was included in the model to account for replicates. Normality assumptions were checked, and a log transformation was needed for all outcomes. Post‐hoc pairwise comparisons were performed to compare least‐squares means when appropriate using a Tukey adjustment. All statistical analyses were performed using SAS v9.4 (SAS Institute, Inc.). The graphs show the median values of the five trials performed for each group, and the bars show the 25th and 75th percentiles.
3. RESULTS
Descriptive statistics of the results can be found in Table 1. The ambient room results obtained before operating the high speed are considered negative control values. In contrast, the positive control results labeled as “Control” were obtained when the high speed was used to prepare the tooth without any suction mitigation devices.
TABLE 1.
Descriptive statistics
| Outcome | N | Mean | Std Dev | Median | 25th Pctl | 75th Pctl | |
|---|---|---|---|---|---|---|---|
| Ambient Room | Spatter | 0 | |||||
| Aerosol | 5 | 0 | 0 | 0 | 0 | 0 | |
| Face spatter | 0 | ||||||
| Total sound | 5 | 61.09 | 0.88 | 60.85 | 60.65 | 61.41 | |
| Control | Spatter | 5 | 54.8 | 6.06 | 54 | 49 | 60 |
| Aerosol | 5 | 72.53 | 95.69 | 26.5 | 23.02 | 61 | |
| Face spatter | 5 | 4.4 | 3.21 | 6 | 2 | 7 | |
| HVE | Spatter | 5 | 47.2 | 11.19 | 43 | 41 | 54 |
| Aerosol | 5 | 3.55 | 3.55 | 2.03 | 0.78 | 5.85 | |
| Face spatter | 5 | 1.4 | 1.14 | 1 | 1 | 2 | |
| Total sound | 5 | 84.26 | 1.48 | 83.6 | 83.43 | 85.15 | |
| RD and HVE | Spatter | 5 | 34 | 3.39 | 35 | 31 | 36 |
| Aerosol | 5 | 1.54 | 0.71 | 1.37 | 0.98 | 1.87 | |
| Face spatter | 5 | 2.4 | 0.55 | 2 | 2 | 3 | |
| PROTO | Spatter | 5 | 12.2 | 3.56 | 13 | 9 | 15 |
| Aerosol | 5 | 0 | 0 | 0 | 0 | 0 | |
| Face spatter | 5 | 0.4 | 0.55 | 0 | 0 | 1 | |
| Total sound | 5 | 98.73 | 0.48 | 98.72 | 98.45 | 98.9 | |
| PROTO and HVE | Spatter | 5 | 7.2 | 2.17 | 6 | 6 | 9 |
| Aerosol | 5 | 0 | 0 | 0 | 0 | 0 | |
| Face spatter | 5 | 0.2 | 0.45 | 0 | 0 | 0 | |
| Total sound | 5 | 97 | 0.73 | 96.82 | 96.67 | 97.14 | |
| AA | Spatter | 5 | 29 | 2.24 | 29 | 28 | 30 |
| Aerosol | 5 | 8.28 | 7.42 | 6.1 | 3.4 | 8.53 | |
| Face spatter | 5 | 2.4 | 0.55 | 2 | 2 | 3 | |
| Total sound | 5 | 88.55 | 0.12 | 88.54 | 88.51 | 88.66 | |
| AA and HVE | Spatter | 4 | 18 | 4.24 | 17.5 | 14.5 | 21.5 |
| Aerosol | 5 | 0 | 0 | 0 | 0 | 0 | |
| Face spatter | 5 | 1 | 0.71 | 1 | 1 | 1 | |
| Total sound | 5 | 88.55 | 0.39 | 88.47 | 88.38 | 88.81 | |
| ISO | Spatter | 5 | 32 | 1.58 | 32 | 31 | 33 |
| Aerosol | 5 | 0.18 | 0.11 | 0.12 | 0.1 | 0.24 | |
| Face spatter | 5 | 2 | 0.71 | 2 | 2 | 2 | |
| Total sound | 5 | 86.73 | 0.8 | 86.66 | 86.19 | 86.95 | |
| ISO and HVE | Spatter | 5 | 27.2 | 1.64 | 28 | 26 | 28 |
| Aerosol | 5 | 0 | 0 | 0 | 0 | 0 | |
| Face spatter | 5 | 1.6 | 0.55 | 2 | 1 | 2 | |
| Total sound | 5 | 87.29 | 0.48 | 87.12 | 86.97 | 87.67 | |
| ReLeaf | Spatter | 5 | 43 | 9.82 | 41 | 35 | 50 |
| Aerosol | 5 | 12.74 | 18.48 | 7.21 | 1.33 | 9.47 | |
| Face spatter | 5 | 3.4 | 2.07 | 3 | 2 | 3 | |
| Total sound | 5 | 86.69 | 1.2 | 87.19 | 86.91 | 87.34 | |
| ReLeaf and HVE | Spatter | 5 | 28.6 | 3.13 | 28 | 27 | 28 |
| Aerosol | 5 | 0 | 0 | 0 | 0 | 0 | |
| Face spatter | 5 | 1.2 | 1.3 | 1 | 0 | 2 | |
| Total sound | 5 | 86.57 | 0.37 | 86.55 | 86.34 | 86.64 | |
| VAC8 | Spatter | 5 | 11.4 | 2.3 | 11 | 10 | 12 |
| Aerosol | 5 | 0.29 | 0.4 | 0.12 | 0.03 | 0.31 | |
| Face Spatter | 5 | 0 | 0 | 0 | 0 | 0 | |
| Total sound | 5 | 79.67 | 0.77 | 79.41 | 79.31 | 80.07 | |
| VAC15 | Spatter | 5 | 31.4 | 4.39 | 30 | 29 | 31 |
| Aerosol | 5 | 7.43 | 2.5 | 8.84 | 7.24 | 8.9 | |
| Face spatter | 5 | 1.4 | 0.55 | 1 | 1 | 2 | |
| Total sound | 5 | 76.98 | 0.51 | 76.9 | 76.87 | 77.42 | |
| VAC15 and HVE | Spatter | 5 | 30.8 | 1.64 | 31 | 31 | 32 |
| Aerosol | 5 | 0 | 0 | 0 | 0 | 0 | |
| Face spatter | 5 | 1.8 | 0.84 | 2 | 1 | 2 | |
| Total sound | 5 | 86.93 | 0.38 | 87.07 | 86.58 | 87.14 |
Note: Legend: Measurement units: 1. Spatter—number of contaminated squares in the experimental grid. 2. Aerosols‐mg/m3. RD with HVE (RD and HVE), PROTO with additional HVE line (PROTO and HVE), AA with additional HVE line (AA and HVE), ISO with additional HVE line (ISO and HVE), ReLeaf with additional HVE line (ReLeaf and HVE), Vac Station 8 cm away from mouth (VAC8), VacStation 15 cm away from mouth (VAC15), Vac Station 15 cm away from mouth plus HVE line (VAC15 and HVE).
Abbreviations: HVE, high‐volume evacuation; RD, rubber dam; PROTO, Prototype 3D printed lip retractor with internal suction and funnel; AA, Aerosol Away external vacuum device; Iso, IsoVac; ReLeaf, ReLeaf.
3.1. Environmental spatter
The environmental spatter analysis (Table 2 and Figure 5) shows that a single HVE line performs similar to the ISO and ReLeaf devices. Although adding the RD to the HVE does not show a statistical improvement compared to HVE alone, the spatter results are improved, showing that the RD + HVE setup is statistically similar to the AA external vacuum device, ISO with or without HVE, ReLeaf with or without HVE, and VacStation 15 cm away from mouth (VAC15) with or without HVE. Only the prototype (PROTO) alone or with HVE and the VacStation 8 cm away from mouth (VAC8) performed better than the setup RD + HVE.
TABLE 2.
Environmental spatter
| Control | HVE | RD and HVE | PROTO | PROTO and HVE | AA | AA and HVE | ISO | ISO and HVE | ReLeaf | ReLeaf and HVE | VAC8 | VAC15 | VAC15 and HVE | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Control | 0.9655 | 0.0059* | <0.0001* | <0.0001* | <0.0001* | <0.0001* | 0.0011* | <0.0001* | 0.5628 | <0.0001* | <0.0001* | 0.0005* | 0.0003* | |
| HVE | 0.9655 | 0.2745 | <0.0001* | <0.0001* | 0.0076* | <0.0001* | 0.0907 | 0.0012* | 0.9999 | 0.0049* | <0.0001* | 0.0515 | 0.0375* | |
| RD and HVE | 0.0059* | 0.2745 | <0.0001* | <0.0001* | 0.9778 | <0.0001* | 1 | 0.7823 | 0.7943 | 0.9528 | <0.0001* | 1 | 0.9998 | |
| PROTO | <0.0001* | <0.0001* | <0.0001* | 0.0014* | <0.0001* | 0.0661 | <0.0001* | <0.0001* | <0.0001* | <0.0001* | 1 | <0.0001* | <0.0001* | |
| PROTO and HVE | <0.0001* | <0.0001* | <0.0001* | 0.0014* | <0.0001* | <0.0001* | <0.0001* | <0.0001* | <0.0001* | <0.0001* | 0.0054* | <0.0001* | <0.0001* | |
| AA | <0.0001* | 0.0076* | 0.9778 | <0.0001* | <0.0001* | 0.0077* | 0.9997 | 1 | 0.0762 | 1 | <0.0001* | 1 | 1 | |
| AA and HVE | <0.0001* | <0.0001* | <0.0001* | 0.0661 | <0.0001* | 0.0077* | 0.0005* | 0.0363* | <0.0001* | 0.0116* | 0.0231* | 0.001* | 0.0015* | |
| ISO | 0.0011* | 0.0907 | 1 | <0.0001* | <0.0001* | 0.9997 | 0.0005* | 0.9706 | 0.4563 | 0.9987 | <0.0001* | 1 | 1 | |
| ISO and HVE | <0.0001* | 0.0012* | 0.7823 | <0.0001* | <0.0001* | 1 | 0.0363* | 0.9706 | 0.0164* | 1 | <0.0001* | 0.993 | 0.9973 | |
| ReLeaf | 0.5628 | 0.9999 | 0.7943 | <0.0001* | <0.0001* | 0.0762 | <0.0001* | 0.4563 | 0.0164* | 0.0529 | <0.0001* | 0.3185 | 0.2562 | |
| ReLeaf and HVE | <0.0001* | 0.0049* | 0.9528 | <0.0001* | <0.0001* | 1 | 0.0116* | 0.9987 | 1 | 0.0529 | <0.0001* | 0.9999 | 1 | |
| VAC8 | <0.0001* | <0.0001* | <0.0001* | 1 | 0.0054* | <0.0001* | 0.0231* | <0.0001* | <0.0001* | <0.0001* | <0.0001* | <0.0001* | <0.0001* | |
| VAC15 | 0.0005* | 0.0515 | 1 | <0.0001* | <0.0001* | 1 | 0.001* | 1 | 0.993 | 0.3185 | 0.9999 | <0.0001* | 1 | |
| VAC15 and HVE | 0.0003* | 0.0375* | 0.9998 | <0.0001* | <0.0001* | 1 | 0.0015* | 1 | 0.9973 | 0.2562 | 1 | <0.0001* | 1 |
Note: RD with HVE (RD and HVE), PROTO with additional HVE line (PROTO and HVE), AA with additional HVE line (AA and HVE), ISO with additional HVE line (ISO and HVE), ReLeaf with additional HVE line (ReLeaf and HVE), Vac Station 8 cm away from mouth (VAC8), VacStation 15 cm away from mouth (VAC15), Vac Station 15 cm away from mouth plus HVE line (VAC15 and HVE). *Denotes statistically significant difference.
Abbreviations: HVE, high‐volume evacuation; RD, rubber dam; PROTO, Prototype 3D printed lip retractor with internal suction and funnel; AA, Aerosol Away external vacuum device; Iso, IsoVac; ReLeaf, ReLeaf.
FIGURE 5.

Environmental spatter. Legend: Measurement units: Spatter—number of contaminated squares in the experimental grid. Numbers above columns denote median values and the bars denote the 25th and 75th percentiles. Abbreviations: high‐volume evacuation—(HVE), rubber dam (RD) with HVE (RD and HVE), Prototype 3D printed lip retractor with internal suction and funnel (PROTO), PROTO with additional HVE line (PROTO and HVE), Aerosol away external Vacuum device (AA), Aerosol away with additional HVE line (AA and HVE), IsoVac (ISO), ISO with additional HVE line (ISO and HVE), ReLeaf (ReLeaf), ReLeaf with additional HVE line (ReLeaf and HVE), Vac Station 8 cm away from mouth (VAC8), VacStation 15 cm away from mouth (VAC15), Vac Station 15 cm away from mouth plus HVE line (VAC15 and HVE)
PROTO alone performed better than most setups except for AA + HVE and VAC8. PROTO, together with an additional HVE line, performs better than all other settings that were tested.
ISO or ReLeaf use provided inferior spatter mitigation compared to when an additional HVE line was added to the mix. Both devices had similar performance. Finally, VAC8 performed similarly to PROTO and significantly better than all other settings, with the exception of PROTO + HVE. Interestingly, once the VAC is distanced to 15 cm from the mouth, the spatter mitigation performance deteriorates significantly, and even adding an additional HVE line does not improve the spatter results.
3.2. Face shield spatter
The primary observation (Table 3 and Figure 6) is that HVE alone performed similarly to all other mitigation methods and was not statistically different from the control. When RD was added to the HVE setup, it decreased the HVE efficiency compared to PROTO and VAC8, probably because the RD causes spatter to bounce. Although PROTO with or without HVE and VAC8 had statistically better results than the control, overall, all mitigation devices had median Face Shield Spatter absolute results ranging between 0 and 3. When HVE was added to ISO, it was statistically inferior only to VAC8, whereas ReLeaf + HVE performed similarly to both the control and all other mitigation methods.
TABLE 3.
Face shield spatter
| Control | HVE | RD and HVE | PROTO | PROTO and HVE | AA | AA and HVE | ISO | ISO and HVE | ReLeaf | ReLeaf and HVE | VAC8 | VAC15 | VAC15 and HVE | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Control | 0.3786 | 0.9998 | 0.0026* | 0.0004* | 0.9998 | 0.1321 | 0.9763 | 0.7908 | 1 | 0.1321 | <0.0001* | 0.5879 | 0.8974 | |
| HVE | 0.3786 | 0.9078 | 0.8065 | 0.455 | 0.9078 | 1 | 0.9958 | 1 | 0.455 | 1 | 0.1719 | 1 | 0.9998 | |
| RD and HVE | 0.9998 | 0.9078 | 0.0367* | 0.0076* | 1 | 0.6074 | 1 | 0.9981 | 1 | 0.6074 | 0.0013* | 0.9799 | 0.9998 | |
| PROTO | 0.0026* | 0.8065 | 0.0367* | 1 | 0.0367* | 0.9799 | 0.1407 | 0.396 | 0.0038* | 0.9799 | 0.9981 | 0.6074 | 0.2692 | |
| PROTO and HVE | 0.0004* | 0.455 | 0.0076* | 1 | 0.0076* | 0.8065 | 0.0367* | 0.1407 | 0.0006* | 0.8065 | 1 | 0.2692 | 0.0832 | |
| AA | 0.9998 | 0.9078 | 1 | 0.0367* | 0.0076* | 0.6074 | 1 | 0.9981 | 1 | 0.6074 | 0.0013* | 0.9799 | 0.9998 | |
| AA and HVE | 0.1321 | 1 | 0.6074 | 0.9799 | 0.8065 | 0.6074 | 0.9078 | 0.9958 | 0.1719 | 1 | 0.455 | 0.9998 | 0.9799 | |
| ISO | 0.9763 | 0.9958 | 1 | 0.1407 | 0.0367* | 1 | 0.9078 | 1 | 0.9888 | 0.9078 | 0.0076* | 0.9998 | 1 | |
| ISO and HVE | 0.7908 | 1 | 0.9981 | 0.396 | 0.1407 | 0.9981 | 0.9958 | 1 | 0.8531 | 0.9958 | 0.0367* | 1 | 1 | |
| ReLeaf | 1 | 0.455 | 1 | 0.0038* | 0.0006* | 1 | 0.1719 | 0.9888 | 0.8531 | 0.1719 | <0.0001* | 0.6694 | 0.9368 | |
| ReLeaf and HVE | 0.1321 | 1 | 0.6074 | 0.9799 | 0.8065 | 0.6074 | 1 | 0.9078 | 0.9958 | 0.1719 | 0.455 | 0.9998 | 0.9799 | |
| VAC8 | <0.0001* | 0.1719 | 0.0013* | 0.9981 | 1 | 0.0013* | 0.455 | 0.0076* | 0.0367 | <0.0001* | 0.455 | 0.0832 | 0.0196* | |
| VAC15 | 0.5879 | 1 | 0.9799 | 0.6074 | 0.2692 | 0.9799 | 0.9998 | 0.9998 | 1 | 0.6694 | 0.9998 | 0.0832 | 1 | |
| VAC15 and HVE | 0.8974 | 0.9998 | 0.9998 | 0.2692 | 0.0832 | 0.9998 | 0.9799 | 1 | 1 | 0.9368 | 0.9799 | 0.0196 | 1 |
Note: RD with HVE (RD and HVE), PROTO with additional HVE line (PROTO and HVE), AA with additional HVE line (AA and HVE), ISO with additional HVE line (ISO and HVE), ReLeaf with additional HVE line (ReLeaf and HVE), Vac Station 8 cm away from mouth (VAC8), VacStation 15 cm away from mouth (VAC15), Vac Station 15 cm away from mouth plus HVE line (VAC15 and HVE). *Denotes statistically significant difference.
Abbreviations: HVE, high‐volume evacuation; RD, rubber dam; PROTO, Prototype 3D printed lip retractor with internal suction and funnel; AA, Aerosol Away external vacuum device; Iso, IsoVac; ReLeaf, ReLeaf.
FIGURE 6.
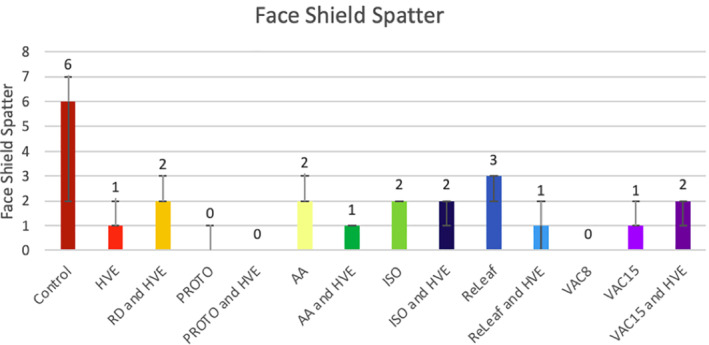
Face shield spatter. Legend: Measurement units: Spatter—number of contaminated squares on the experimental grid. Numbers above columns denote median values and the bars denote the 25th and 75th percentiles. Abbreviations: high‐volume evacuation—(HVE), rubber dam (RD) with HVE (RD and HVE), Prototype 3D printed lip retractor with internal suction and funnel (PROTO), PROTO with additional HVE line (PROTO and HVE), Aerosol away external Vacuum device (AA), Aerosol away with additional HVE line (AA and HVE), IsoVac (ISO), ISO with additional HVE line (ISO and HVE), ReLeaf (ReLeaf), ReLeaf with additional HVE line (ReLeaf and HVE), Vac Station 8 cm away from mouth (VAC8), VacStation 15 cm away from mouth (VAC15), Vac Station 15 cm away from mouth plus HVE line (VAC15 and HVE)
3.3. Aerosol
It is worth noticing (Table 4 and Figure 7) that the setting RD + HVE performed similarly to all other mitigation techniques. HVE alone was inferior to ambient negative control values and to PROTO. However, when HVE was used in conjunction with any other device tested, it brought the aerosols to negative control levels (ambient room) values. PROTO alone was able to mitigate aerosol to negative control (ambient) values. When used alone, AA, ReLeaf, and VAC15 were significantly inferior to all other aerosol mitigation setups.
TABLE 4.
Aerosol creation
| Ambient Room | Control | HVE | RD and HVE | PROTO | PROTO and HVE | AA | AA and HVE | ISO | ISO and HVE | ReLeaf | ReLeaf and HVE | VAC8 | VAC15 | VAC15 and HVE | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Ambient Room | <0.0001* | 0.0435* | 0.4029 | 1 | 1 | <0.0001* | 1 | 1 | 1 | <0.0001* | 1 | 1 | <0.0001* | 1 | |
| Control | <0.0001* | <0.0001* | <0.0001* | <0.0001* | <0.0001* | 0.0006* | <0.0001* | <0.0001* | <0.0001* | 0.0002* | <0.0001* | <0.0001* | 0.0013* | <0.0001* | |
| HVE | 0.0435* | <0.0001* | 0.9994 | 0.0435* | 0.0435* | 0.69 | 0.0435* | 0.1373 | 0.0435* | 0.8411 | 0.0435* | 0.2075 | 0.538 | 0.0435* | |
| RD and HVE | 0.4029 | <0.0001* | 0.9994 | 0.4029 | 0.4029 | 0.1263 | 0.4029 | 0.7138 | 0.4029 | 0.2206 | 0.4029 | 0.8259 | 0.0738 | 0.4029 | |
| PROTO | 1 | <0.0001* | 0.0435* | 0.4029 | 1 | <0.0001* | 1 | 1 | 1 | <0.0001* | 1 | 1 | <0.0001* | 1 | |
| PROTO and HVE | 1 | <0.0001* | 0.0435* | 0.4029 | 1 | <0.0001* | 1 | 1 | 1 | <0.0001* | 1 | 1 | <0.0001* | 1 | |
| AA | <0.0001* | 0.0006* | 0.69 | 0.1263 | <0.0001* | <0.0001* | <0.0001* | 0.0002* | <0.0001* | 1 | <0.0001* | 0.0003* | 1 | <0.0001* | |
| AA and HVE | 1 | <0.0001* | 0.0435* | 0.4029 | 1 | 1 | <0.0001* | 1 | 1 | <0.0001* | 1 | 1 | <0.0001* | 1 | |
| ISO | 1 | <0.0001* | 0.1373 | 0.7138 | 1 | 1 | 0.0002 | 1 | 1 | 0.0004 | 1 | 1 | <0.0001* | 1 | |
| ISO and HVE | 1 | <0.0001* | 0.0435 | 0.4029 | 1 | 1 | <0.0001* | 1 | 1 | <0.0001* | 1 | 1 | <0.0001* | 1 | |
| ReLeaf | <0.0001* | 0.0002* | 0.8411 | 0.2206 | <0.0001* | <0.0001* | 1 | <0.0001* | 0.0004* | <0.0001* | <0.0001* | 0.0008* | 1 | <0.0001* | |
| ReLeaf and HVE | 1 | <0.0001* | 0.0435* | 0.4029 | 1 | 1 | <0.0001* | 1 | 1 | 1 | <0.0001* | 1 | <0.0001* | 1 | |
| VAC8 | 1 | <0.0001* | 0.2075 | 0.8259 | 1 | 1 | 0.0003* | 1 | 1 | 1 | 0.0008* | 1 | 0.0002* | 1 | |
| VAC15 | <0.0001* | 0.0013* | 0.538 | 0.0738 | <0.0001* | <0.0001* | 1 | <0.0001* | <0.0001* | <0.0001* | 1 | <0.0001* | 0.0002* | <0.0001* | |
| VAC15 and HVE | 1 | <0.0001* | 0.0435* | 0.4029 | 1 | 1 | <0.0001* | 1 | 1 | 1 | <0.0001* | 1 | 1 | <0.0001* |
Note: RD with HVE (RD and HVE), PROTO with additional HVE line (PROTO and HVE), AA with additional HVE line (AA and HVE), ISO with additional HVE line (ISO and HVE), ReLeaf with additional HVE line (ReLeaf and HVE), Vac Station 8 cm away from mouth (VAC8), VacStation 15 cm away from mouth (VAC15), Vac Station 15 cm away from mouth plus HVE line (VAC15 and HVE). *Denotes statistically significant difference.
Abbreviations: HVE, high‐volume evacuation; RD, rubber dam; PROTO, Prototype 3D printed lip retractor with internal suction and funnel; AA, Aerosol Away external vacuum device; Iso, IsoVac; ReLeaf, ReLeaf.
FIGURE 7.

Aerosol creation. Legend: Measurement units: Aerosols‐mg/m3. Numbers above columns denote median values and the bars denote the 25th and 75th percentiles. Abbreviations: high‐volume evacuation—(HVE), rubber dam (RD) with HVE (RD and HVE), Prototype 3D printed lip retractor with internal suction and funnel (PROTO), PROTO with additional HVE line (PROTO and HVE), Aerosol away external vacuum device (AA), Aerosol away with additional HVE line (AA and HVE), IsoVac (ISO), ISO with additional high‐volume evacuation (HVE) line (ISO and HVE), ReLeaf (ReLeaf), ReLeaf with additional HVE line (ReLeaf and HVE), Vac Station 8 cm away from mouth (VAC8), VacStation 15 cm away from mouth (VAC15), Vac Station 15 cm away from mouth plus HVE line (VAC15 and HVE)
3.4. Total sound level
Although the VAC had the lowest noise level (less than 80 dB), it loses this advantage when an HVE line is added to the mix (Table 5 and Figure 8). Next is a single HVE line with a median TSL of 83.6 dB. Most setups (AA, AA+HVE, ISO, ISO + HVE, ReLeaf, ReLeaf+HVE, VAC15 + HVE) have TSL levels between 86.55 and 88.54 dB; although the statistical analysis shows some statistical differences among these setups, it is probable that the range of less than 2 dB is not practically very significant. The setup PROTO with or without HVE has significantly higher TSL at 96.82 and 98.72 dB, respectively.
TABLE 5.
Total sound level
| Ambient Room | HVE | PROTO | PROTO and HVE | AA | AA and HVE | ISO | ISO and HVE | ReLeaf | ReLeaf and HVE | VAC8 | VAC15 | VAC15 and HVE | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Ambient Room | <0.0001* | <0.0001* | <0.0001* | <0.0001* | <0.0001* | <0.0001* | <0.0001* | <0.0001* | <0.0001* | <0.0001* | <0.0001* | <0.0001* | |
| HVE | <0.0001* | <0.0001* | <0.0001* | <0.0001* | <0.0001* | 0.0005* | <0.0001* | 0.0007* | 0.0014* | <0.0001* | <0.0001* | 0.0001* | |
| PROTO | <0.0001* | <0.0001* | 0.1433 | <0.0001* | <0.0001* | <0.0001* | <0.0001* | <0.0001* | <0.0001* | <0.0001* | <0.0001* | <0.0001* | |
| PROTO and HVE | <0.0001* | <0.0001* | 0.1433 | <0.0001* | <0.0001* | <0.0001* | <0.0001* | <0.0001* | <0.0001* | <0.0001* | <0.0001* | <0.0001* | |
| AA | <0.0001* | <0.0001* | <0.0001* | <0.0001* | 1 | 0.0378* | 0.4166 | 0.0299* | 0.0156* | <0.0001* | <0.0001* | 0.102 | |
| AA and HVE | <0.0001* | <0.0001* | <0.0001* | <0.0001* | 1 | 0.0383* | 0.4199 | 0.0303* | 0.0158* | <0.0001* | <0.0001* | 0.1032 | |
| ISO | <0.0001* | 0.0005* | <0.0001* | <0.0001* | 0.0378* | 0.0383* | 0.9956 | 1 | 1 | <0.0001* | <0.0001* | 1 | |
| ISO and HVE | <0.0001* | <0.0001* | <0.0001* | <0.0001* | 0.4166 | 0.4199 | 0.9956 | 0.9915 | 0.9652 | <0.0001* | <0.0001* | 0.9999 | |
| ReLeaf | <0.0001* | 0.0007* | <0.0001* | <0.0001* | 0.0299* | 0.0303* | 1 | 0.9915 | 1 | <0.0001* | <0.0001* | 1 | |
| ReLeaf and HVE | <0.0001* | 0.0014* | <0.0001* | <0.0001* | 0.0156* | 0.0158* | 1 | 0.9652 | 1 | <0.0001* | <0.0001* | 0.9999 | |
| VAC8 | <0.0001* | <0.0001* | <0.0001* | <0.0001* | <0.0001* | <0.0001* | <0.0001* | <0.0001* | <0.0001* | <0.0001* | <0.0001* | <0.0001* | |
| VAC15 | <0.0001* | <0.0001* | <0.0001* | <0.0001* | <0.0001* | <0.0001* | <0.0001* | <0.0001* | <0.0001* | <0.0001* | <0.0001* | <0.0001* | |
| VAC15 and HVE | <0.0001* | 0.0001* | <0.0001* | <0.0001* | 0.102 | 0.1032 | 1 | 0.9999 | 1 | 0.9999 | <0.0001* | <0.0001* |
Note: RD with HVE (RD and HVE), PROTO with additional HVE line (PROTO and HVE), AA with additional HVE line (AA and HVE), ISO with additional HVE line (ISO and HVE), ReLeaf with additional HVE line (ReLeaf and HVE), Vac Station 8 cm away from mouth (VAC8), VacStation 15 cm away from mouth (VAC15), Vac Station 15 cm away from mouth plus HVE line (VAC15 and HVE). *Denotes statistically significant difference.
Abbreviations: HVE, high‐volume evacuation; RD, rubber dam; PROTO, Prototype 3D printed lip retractor with internal suction and funnel; AA, Aerosol Away external vacuum device; Iso, IsoVac; ReLeaf, ReLeaf.
FIGURE 8.

Total sound level. Legend: Measurement units: Sound‐dB. Numbers above columns denote median values and the bars denote the 25th and 75th percentiles. Abbreviations: high‐volume evacuation—(HVE), rubber dam (RD) with HVE (RD and HVE), Prototype 3D printed lip retractor with internal suction and funnel (PROTO), PROTO with additional HVE line (PROTO and HVE), Aerosol away external vacuum device (AA), Aerosol away with additional HVE line (AA and HVE), IsoVac (ISO), ISO with additional HVE line (ISO and HVE), ReLeaf (ReLeaf), ReLeaf with additional HVE line (ReLeaf and HVE), Vac Station 8 cm away from mouth (VAC8), VacStation 15 cm away from mouth (VAC15), Vac Station 15 cm away from mouth plus HVE line (VAC15 and HVE)
4. DISCUSSION
The American Dental Association, 37 emphasized the importance of oral health care and that millions of patients have been safely treated during the last few months of the pandemic. They emphasize that appropriate personal protective equipment in concert with aerosol‐generating procedure (AGP) mitigation efforts are responsible for this success. This study brings to light the most successful techniques that can be incorporated into the dental practice to mitigate spatter and aerosols from AGP.
The creation of aerosol and spatter during dental procedures has been a keen focus of concern during the COVID‐19 pandemic. Many different mitigation strategies and devices have been created and advertised to address these concerns. However, there has not been, any clear understanding if these devices are effective. Ravenel et al. 33 demonstrated that several of the conventional evacuation apparatuses found in the dental practice could effectively reduce and eliminate aerosol and spatter when used in combination, typically with both and intra and extraoral high volume evacuation. However, it did not replicate aerosol and spatter creation that occurs when actually working with a handpiece intraorally since the preparation of teeth was not part of that study. This paper attempts to demonstrate potential effective mitigation strategies that can be employed while the dentist actually works in the oral cavity.
Environmental spatter on the patient, the test site area, and the operator face shield was measured during this study. All tested devices and configurations tested showed some spatter formation on the test area, although the results show that some setups performed better. To that end, we observed that the PROTO and VAC8 setups performed better than other setups, without the need to add a second HVE line to mitigate spatter. The same trend was observed for the Face Shield spatter, where these two devices had a median value of zero. However, some spatter was found on the operator face shield with the VAC at 15 cm, either with or without secondary HVE. The suction limitations of the VAC over a larger distances from the operating area may have contributed to this higher face shield spatter.
The PROTO device that uses both the HVE line and the saliva ejector line was able to mitigate aerosols to a satisfactory level. This also was observed for ISO and VAC8. The dome‐like clear shield of the VAC enables the clinician to view the operating area; however, the close proximity to the oral cavity for effective use may hinder effective clinician performance. At 15 cm (approximately 6 in.), the VAC aerosol mitigation ability dropped significantly. However, in contrast with the Face Shield spatter, when this greater distance was used in conjunction with a secondary HVE, the aerosol was entirely contained. The ReLeaf and AA devices used alone were less effective in aerosol mitigation in our testing. For both these devices, good aerosol mitigation was obtained by incorporating a secondary HVE placed correctly in the treated area. All other setups also resulted in considerable aerosol mitigation when a second line of HVE was added to the mix.
Regarding RD use with HVE, our results show that it is an efficient aerosol mitigation strategy. These results are consistent with previously reported data. 33 This is surprising because our study showed that HVE alone provided only partial aerosol mitigation. We can postulate that the use of RD limits the dispersion of aerosols in the patient's mouth and the resulting turbulence that may cause the aerosols to escape from the HVE suction.
Sound also comes into play when attempting to mitigate aerosol and spatter in the dental workplace. As previously discussed in Ravenel et al. 33 the sound output of these various mitigation devices can be problematic, especially in light of the Occupational Safety and Health Administration (OSHA) 38 and National Institute for Occupational Safety and Health (NIOSH) maximum noise standards 39 of 90 and 85 dB respectively. In this study, the TSL of the setups tested ranged from a low of 76.9 dB for VAC 15 to a high of 98.72 dB for PROTO. Most setups TSL measured between the OSHA and the NIOSH standards, that is, between 85 and 90 dB. One reason the PROTO device might be loud is that it was a 3D printed prototype with an irregular surface.
5. CONCLUSION
Within the limitations of this study, it can be concluded that the dental community has at its disposal equipment and instrumentation that can significantly mitigate the creation of aerosol when performing AGPs. The simplest and most widely used solution setup HVE + RD (HVE with RD) allows satisfactory mitigation of spatter and most aerosols when the clinical situation allows. However, this study demonstrates that there are other mitigation strategies that are more effective, particularly when used in conjunction with a secondary HVE apparatus. These simple setups can be quickly incorporated into every practice, often without requiring a significant capital investment.
DISCLOSURE
This research is the subject of currently pending U.S. Non‐Provisional Patent Application Serial Number 16/895,915 entitled “Lip Retractor with Integrated Suction” filed on June 8, 2020. This research was funded by South Carolina Clinical and Translational Research Grant SCTR 2106. This project was supported, in part, by the National Center for Advancing Translational Sciences of the National Institutes of Health under Grant Number UL1 TR001450. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Comisi JC, Ravenel TD, Kelly A, Teich ST, Renne W. Aerosol and spatter mitigation in dentistry: Analysis of the effectiveness of 13 setups. J Esthet Restor Dent. 2021;33:466–479. 10.1111/jerd.12717
Funding information National Center for Advancing Translational Sciences of the National Institutes of Health, Grant/Award Number: UL1 TR001450; South Carolina Clinical and Translational Research, Grant/Award Number: SCTR 2106.
Contributor Information
John C. Comisi, Email: comisi@musc.edu.
Abigail Kelly, Email: lauera@musc.edu.
REFERENCES
- 1. Lu R, Zhao X, Li J, et al. Genomic characterisation and epidemiology of 2019 novel coronavirus: implications for virus origins and receptor binding. Lancet. 2020;395(10224):565‐574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Mahase E. China coronavirus: WHO declares international emergency as death toll exceeds 200. BMJ: British Med J. 2020;368. 10.1136/bmj.m408 [DOI] [PubMed] [Google Scholar]
- 3. Backer JA, Klinkenberg D, Wallinga J. Incubation period of 2019 novel coronavirus (2019‐nCoV) infections among travellers from Wuhan, China, 20–28 January 2020. Eurosurveillance. 2020;25(5):2000062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Chan JF‐W, Yuan S, Kok K‐H, et al. A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person‐to‐person transmission: a study of a family cluster. Lancet. 2020;395(10223):514‐523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Gamio L. The workers who face the greatest coronavirus risk. New York Times. 2020. https://www.nytimes.com/interactive/2020/03/15/business/economy/coronavirus-worker-risk.html [Google Scholar]
- 6. Jayaweera M, Perera H, Gunawardana B, Manatunge J. Transmission of COVID‐19 virus by droplets and aerosols: a critical review on the unresolved dichotomy. Environ Res. 2020;188:109819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Gross K, Overman P, Cobb C, Brockmann S. Aerosol generation by two ultrasonic scalers and one sonic scaler. A comparative study. J Dent Hyg: JDH. 1992;66(7):314‐318. [PubMed] [Google Scholar]
- 8. Holbrook W, Muir K, Macphee I, Ross P. Bacteriological investigation of the aerosol from ultrasonic sealers. Brit Dent J. 1978;144(8):245‐247. [DOI] [PubMed] [Google Scholar]
- 9. Larato DC, Ruskin PF, Martin A, Delanko R. Effect of a dental air turbine drill on the bacterial counts in air. J Prosthet Dent. 1966;16(4):758‐765. [Google Scholar]
- 10. Micik RE, Miller RL, Mazzarella MA, Ryge G. Studies on dental aerobiology: I. bacterial aerosols generated during dental procedures. J Dent Res. 1969;48(1):49‐56. [DOI] [PubMed] [Google Scholar]
- 11. Miller R. Generation of airborne infection… By high speed dental equipment. J Am Soc Prev Dent. 1976;6(3):14‐17. [PubMed] [Google Scholar]
- 12. Miller RL, Micik RE, Abel C, Ryge G. Studies on dental aerobiology: II. Microbial splatter discharged from the oral cavity of dental patients. J Dent Res. 1971;50(3):621‐625. [DOI] [PubMed] [Google Scholar]
- 13. Del Rio C, Malani PN. 2019 novel coronavirus—important information for clinicians. JAMA. 2020;323(11):1039‐1040. [DOI] [PubMed] [Google Scholar]
- 14. W‐j G, Ni Z‐Y, Hu Y, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382(18):1708‐1720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223):497‐506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Control CfD . Transmission of coronavirus disease 2019 (COVID‐19); 2020.
- 17. Tajima Y, Suda Y, Yano K. A case report of SARS‐CoV‐2 confirmed in saliva specimens up to 37 days after onset: proposal of saliva specimens for COVID‐19 diagnosis and virus monitoring. J Infect Chemother. 2020;26:1086‐1089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Bentley CD, Burkhart NW, Crawford JJ. Evaluating spatter and aerosol contamination during dental procedures. J Am Dent Assoc (1939). 1994;125(5):579‐584. [DOI] [PubMed] [Google Scholar]
- 19. Harrel SK, Barnes JB, Rivera‐Hidalgo F. Aerosol and splatter contamination from the operative site during ultrasonic scaling. J Am Dent Assoc. 1998;129(9):1241‐1249. [DOI] [PubMed] [Google Scholar]
- 20. King TB, Muzzin KB, Berry CW, Anders LM. The effectiveness of an aerosol reduction device for ultrasonic sealers. J Periodontol. 1997;68(1):45‐49. [DOI] [PubMed] [Google Scholar]
- 21. Harrel SK, Molinari J. Aerosols and splatter in dentistry: a brief review of the literature and infection control implications. J Am Dent Assoc. 2004;135(4):429‐437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. O'Donnell MJ, Boyle MA, Russell RJ, Coleman DC. Management of dental unit waterline biofilms in the 21st century. Future Microbiol. 2011;6(10):1209‐1226. [DOI] [PubMed] [Google Scholar]
- 23. Szymanska J, Sitkowska J, Dutkiewicz J. Microbial contamination of dental unit waterlines. Ann Agric Environ Med. 2008;15(2):173‐179. [PubMed] [Google Scholar]
- 24. Yamada H, Ishihama K, Yasuda K, et al. Aerial dispersal of blood‐contaminated aerosols during dental procedures. Quintessence Int. 2011;42(5):399‐405. [PubMed] [Google Scholar]
- 25. Ali K, Raja M. Coronavirus disease 2019 (COVID‐19): challenges and management of aerosol‐generating procedures in dentistry. Evid Based Dent. 2020;21(2):44‐45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Data on COVID‐19 Discussed by Researchers at University of Health Sciences Coronavirus disease 2019 (COVID‐19): challenges and management of aerosol‐generating procedures in dentistry. Medical Letter on the CDC & FDA NewsRX LLC.; 2020. p. 360.
- 27. Ge ZY, Yang LM, Xia JJ, Fu XH, Zhang YZ. Possible aerosol transmission of COVID‐19 and special precautions in dentistry. J Zhejiang Univ Sci B. 2020;21(5):361‐368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Teichert‐Filho R, Baldasso CN, Campos MM, Gomes MS. Protective device to reduce aerosol dispersion in dental care in times of COVID‐19 pandemic. Int Endod J. 2020;53:1588‐1597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Li Y, Ren B, Peng X, et al. Saliva is a non‐negligible factor in the spread of COVID‐19. Mol Oral Microbiol. 2020;35:141‐145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Singh A, Shiva Manjunath RG, Singla D, Bhattacharya HS, Sarkar A, Chandra N. Aerosol, a health hazard during ultrasonic scaling: a clinico‐microbiological study. Indian J Dent Res. 2016;27(2):160‐162. [DOI] [PubMed] [Google Scholar]
- 31. Control CfD, Prevention. Interim Infection Prevention and Control Guidance for Dental Settings during the COVID‐19 Response: Centers for Disease Control and Prevention, Atlanta, GA, USA; 2019.
- 32. Van Doremalen N, Bushmaker T, Morris DH, et al. Aerosol and surface stability of SARS‐CoV‐2 as compared with SARS‐CoV‐1. N Engl J Med. 2020;382(16):1564‐1567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Ravenel TD, Kessler R, Comisi JC, et al. Evaluation of the spatter‐reduction effectiveness and aerosol containment of eight dry‐field isolation techniques. Quintessence Int. 1985;2020:2‐12. [DOI] [PubMed] [Google Scholar]
- 34. Dahlke WO, Cottam MR, Herring MC, Leavitt JM, Ditmyer MM, Walker RS. Evaluation of the spatter‐reduction effectiveness of two dry‐field isolation techniques. J Am Dent Assoc. 2012;143(11):1199‐1204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Kam P, Kam A, Thompson J. Noise pollution in the anaesthetic and intensive care environment. Anaesthesia. 1994;49(11):982‐986. [DOI] [PubMed] [Google Scholar]
- 36. Friedrich M, Tirilomis T, Kollmeier J, Wang Y, Hanekop G. Modifications of surgical suction tip geometry for flow optimisation: influence on suction‐induced noise pollution. Surg Res Pract. 2018;2018:1‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. ADA 'respectfully yet strongly disagrees' with WHO guidance recommending delay of dental care. https://www.ada.org/en/publications/ada‐news/2020‐archive/august/ada‐respectfully‐yet‐strongly‐disagrees‐with‐who‐guidance‐recommending‐delay‐of‐dental‐care. Accessed 17 August 2020.
- 38. United States Department of Labor, Occupational Safety and Health Administration . Occupational noise exposure. https://www.osha.gov/pls/oshaweb/owadisp.show_document?p_id=9735&p_table=STANDARDS. Accessed August 17, 2020.
- 39. The National Institute for Occupational Safety and Health (NIOSH) . Occupational Noise Exposure, DHHS (NIOSH) Publication Number 98–126. https://www.cdc.gov/niosh/docs/98-126/. Accessed August 17, 2020.


