Abstract
Aim
To establish trends in Implant Dentistry in Latin America in the COVID‐19 pandemic.
Material and methods
A steering committee and an advisory group of experts in Implant Dentistry were selected among eighteen countries. An open‐ended questionnaire by Delphi methodology was validated including 64 questions, divided in 7 topics, concerning the various trends in dental implantology. The survey was conducted in two rounds, which provided the participants in the second round with the results of the first. The questionnaires were completed on August 2020, and the online meeting conference was held on September 2020. The final prediction was developed through consensus by a selected group of experts.
Results
A total of 197 experts from Latin America answered the first and second questionnaire. In the first round, the established threshold for consensus (65%) was achieved in 30 questions (46.87%). In the second round, performed on average 45 days later, this level was achieved in 47 questions (73.43%). Consensus was completely reached on the item “Diagnostic” (100%), the field with the lowest consensus was “Demand for treatment with dental implants” (37.5%).
Conclusions
The present study in Latin America has provided relevant and useful information on the predictions in the education and practice of Implant Dentistry in the COVID‐19 era. The consensus points toward a great confidence of clinicians in the biosecurity protocols used to minimize the risk of SARS‐CoV‐2 transmission. It is foreseen as an important change in education, with introduction of virtual reality and other simulation technologies in implant training.
Keywords: consensus, COVID‐19, Delphi technique, dental implant, education
1. INTRODUCTION
The growth and expansion of Dentistry in Latin America (LA), together with the increase in the educational needs of the profession, justifies conducting a comprehensive analysis on the trends in Implant Dentistry on this region (Herrera et al., 2020; López Jordi, Figueiredo, Barone, & Pereira, 2016), with distinctive political, economic, and social perspectives (Romito et al., 2020). Moreover, The COVID‐19 pandemic has become not only a major challenging public health problem for most of the countries, but it is also changing the socioeconomic balance and affecting the society at all levels, including the dental profession. This outbreak was declared a Public Health Emergency by the World Health Organization (AL‐Maweri et al., 2020; Meng et al., 2020) and since its outbreak, the COVID‐19 has infected more than 29 million people, with 950,000 deaths, by September 14rd, 2020 (Nuzzo et al., 2020). Coronavirus cases have increased considerably in Latin America. Brazil has registered more than 4.3 million confirmed cases, the third highest count in the world after the United States and India. Moreover, it is the second country, behind the United States, with the highest number of deaths. Mexico, Argentina, Colombia, and Peru have also had major outbreaks and are among the 10 countries that have confirmed more cases (Nuzzo et al., 2020).
As a health profession, Dentistry has been affected not only in terms of the prevention and spread of the infection, but also in the delivery of care, being implant dentistry one of the most affected specialties, due to its invasiveness since it combines surgical, prosthetic, and aerosol producing interventions (Boyce, 2021; Nibali et al., 2020; Rutkowski et al., 2020). Under these circumstances, it will be desirable to develop scientific information at regional level (LA) on the trends of the education and practice in implant dentistry in the COVID‐19 pandemic, since although living in a globalized world, there are regional peculiarities that need to be studied (Tiwari et al., 2018).
The Delphi method belongs to the subjective–intuitive methods of foresight, which is especially useful for forecasting, as expert opinions are the only source of information available (Dalkey & Helmer, 1963). Its main objective is to evaluate the degree of consensus among experts in a specific topic. This method is characterized by allowing a structured group of individuals to deal with complex problems through structured communication, individual feedback, group judgment, and discussion (Woudenberg, 1991). Using this methodology, the previously available information is evaluated, and suitable tendencies or evolution patterns are looked for in order to allow the most probable future environments (Dalkey & Helmer, 1963). The answers of the experts are obtained in consecutive rounds of anonymous questionnaires, aiming at looking for a consensus among experts, but keeping the maximum independency of criteria of each individual. Once the collected data from the surveys are analyzed, the final prediction is developed through consensus by a selected group of experts (Dalkey & Helmer, 1963; Woudenberg, 1991). Recently, this methodology has been successfully introduced in Dentistry to predict the development of different specialties in Europe, with the support of relevant scientific societies such as the European Federation of Periodontology (EFP) (Madianos et al., 2016) and the European Association for Osseointegration (EAO) (Sanz et al., 2019).
It was, therefore, the objective of the present study endorsed by the Ibero Panamercian Federation of Periodontology and the Peruvian Association of Oral Implantology to analyze the trends in Implant Dentistry in LA, under the perspective of the post COVID‐19 pandemic. Special attention was placed to evaluate the future perspectives in epidemiological trends, education, biosecurity, and professional practice.
2. MATERIAL AND METHODS
2.1. Study design
The Delphi methodology was used to predict the future trends in Implant Dentistry in the post COVID‐19 era based on different levels of consensus retrieved from expert opinions. An Advisory Committee (M.A., I.S., J.S., L.M., A.L.P, and M.S) was established: (a) to define the context and the timeframe in which it was desirable to forecast, (b) to design and validate the questionnaire, and (c) to select a Steering Committee with experts in oral implantology who represented each country in LA. This Steering committee was established to approve and finalized the questionnaire and to select the expert panel among each country considering the surgical and prosthetic fields of oral implantology. The study followed the COREQ (COnsolidated criteria for REporting Qualitative research) statement (Tong et al., 2007).
2.2. A Questionnaire
The structured questionnaire was designed and was expected to be completed in approximately 20 min. It contained 64 questions and was divided in the following 7 sections, specifically dealing with the following trends:
Demand for dental implant treatment (8 questions).
Diagnosis (4 questions).
Biosecurity (15 questions).
Surgical approaches (12 questions).
Prosthetic approaches (7 questions).
Peri‐implant Diseases and Maintenance (7 questions).
Education and training (11 questions).
Three well‐defined possible answers were provided to all questions, except in one where four options were provided. Furthermore, an open‐end space was always provided for each question in case the expert would like to answer differently or make any clarification to the question. These comments were analyzed in the consensus meeting to discuss and to clarify the responses.
2.3. Selection of experts and questionnaire rounds
Experts in eighteen countries were selected according to their professional profile. One‐third of the experts had a full‐time academic position at the university, one‐third worked mainly in the private clinic even though they could work part time at the university, and the remaining third worked in the public sector, including hospitals and/or state health centers. Ideally, each country contributed with a proportioned sample of surgical and prosthodontics experts. To be considered as an expert, one of the following inclusion criteria was considered: (a) specialist with a degree obtained at university; and (b) general dentist with more than 10 years of experience in dental implantology. Using these criteria, 213 experts received an invitation letter to participate in the study, as well as the online address, where the questionnaire should be answered. Each country was represented in the model by a number of experts proportional to the number of active dentists. A minimum of three experts were established for each country, as suggested by key persons assigned to each country or region by the advisory group.
The online questionnaire was sent to the selected experts (July 2020). A timeframe of 2 weeks was given to get a response. The answers were collected by the Steering Committee, and the questionnaires were sent in the second round to the experts 45 days after (August 2020), including a summary of the results for the first round. This methodology allowed the expert to “align” themselves with the thoughts of the other participants, changing their answer or remaining with his previous answer.
The responses were collected again, and a descriptive systematized data analysis was carried out to describe the different opinions and the consensus reached. Responses that achieved a minimum consensus of 65% among the expert panel were no longer discussed, while responses below this threshold were discussed in depth at the final online consensus meeting.
By convention, the following consensus levels were established: (a) no consensus when the threshold of 65% was not attained in the second round; (b) moderate consensus when achieving 65%–85%; and (c) high consensus when reaching >85%.
2.4. Consensus conference
An online meeting conference was held on September 2020. During this meeting, the results from the second round to each question were presented. However, discussion during the meeting specifically dealt with those answers not reaching the 65% level of consensus after the second round and those issues requiring further explanation. These questions were further discussed until reaching consensus from those present at the conference. During this consensus meeting, the final conclusions based on the results were discussed representing the basis for this report.
2.5. Data analysis
After the first and second round, the answers to each question were individually analyzed following descriptive statistics with data presented as absolute values and percentages, as well as means. In addition to statistical descriptors, the expert's testimonies were also taken into account in nonconsensual questions, as well as personal observations of those experts who remained opposed to the consensus achieved in certain questions.
3. RESULTS
A total of 213 experts from LA were invited to participate. In the first round, 100% answered the questionnaire and 197 participants from those participating in the first round (92.48%) finally participated in the second round. The distribution of experts for each country is depicted in Table 1.
TABLE 1.
Distribution of experts for each country
| Country | N | % | Experts |
|---|---|---|---|
| Brazil | 40 | 20.30% | Alexandre Batista Lopes Do Nascimento; Alexandre Meloti Dottore; Aline Alves Luciano; Andre Vilela; Andrea Serio Dias Britto; Aníbal; Narvaja; Celeste Hung; Daiane Fermiano; Danilo Horie Bellini; Eduardo Claudio Lopes De Chaves E Mello Dias; Fábio Eduardo Calvo Mardegan; Giuseppe A Romito; Guillermo Castro Cortellari; Ilton Mafra Mafra; Jamil Awad Shibli; Jorge Taira; Kelson Marinho De Oliveira; Luciano Oliveira; Marcelo Abla; Marcelo Augusto Ruiz Da Cunha Melo; Marlon Marx Hilariano Maximiano; Mas Uricio Aied Filho; Maurício Querido; Micheline Sandini Trentin; Paulo Roberto Ramalho; Paulo Sérgio Cruvinel; Pedro Paulo Cardoso Pita; Rafael Shinoske Siroma; Renata Boaventura Senne Paz; Renato; Gaudiosi Vianna; Roberto Ferrari; Roberto Puertas Garcia; Rodrigo Santos Da Silva; Rogerio Romeiro; Rubens Moreno De Freitas; Samy Tunchel; Stella Mendes; Tiago Marcio Costa De Oliveira; Tulio Kalife; Ulisses Dayube |
| Mexico | 15 | 7.61% | Alejandro Gonzalez Blanco B; Alejandro Treviño; Antonio Bello; Arturo M Flores Villarreal; Carlos Quiroz; Enrique Ríos Szalay; Enrique Treviño Bazan; Federico Pérez Díez; Gilberto; Tostado Escobosa; Jesus Gamez Calderon; Juan Pablo Villarreal; Luis Martín Villavicencio Fernández; Miguel Andrés Ruiz Rivera; Rodrigo Rafael Escalante Vazquez; Said Sanchez |
| Argentina | 10 | 5.08% | Alberto Daniel Loddo; Daniel Torassa; Emanuel Petronsi; Gonzalo Nicolás González; Hugo Albera; Martin Villagra Abate; Mauro Storelli; Nicolas Marsano; Pablo Gamboa; Riera Jose Miguel |
| Chile | 10 | 5.08% | Edgar Berg; José Manuel Abarca; Juan Carlos Duran Yaneth; Maria Carolina Alarcón Azócar; María Dolores De La Jara; Natacha Oyarzo; Orlando Alvarez; Sebastian Bravo; Sofia Kupfer Toro; Stuardo Valenzuela Manfredi |
| Colombia | 10 | 5.08% | Fernando Galindo G.; Guillermo Bernal; Jorge Hernan López Velasquez; Leonardo Vargas Rico; Mauricio Echeverri A; Ramón Pereira Ebratt; Roberto Mejia Molina; Tomás Villaquirán; Wilhelm Bellaiza; Yamil Augusto Lesmes Otavo |
| Venezuela | 10 | 5.08% | Ana Lorena Solórzano Peláez; Ana Luisa Bernotti Carabaño; Aulio Caires; Elizabeth Albornoz; Gredy Lugo; Ilusión Romero; Isidoro Ortiz; Roberto Fermín; Tabatha L. Rojas Marin; Xiomara Gimenez |
| Bolivia | 10 | 5.08% | Claudio Murillo Sasamoto; Darwin Sergio Justiniano Pereyra; David Muñoz Montufar; Pablo Guzmán; Jose Gonzalo Artieda Saenz; Luis Alberto Méndez Delgadillo; Luis Guillermo Peredo Paz; Marcel Quezada; Primo Herrera Subelza; Rafael Molina Vargas |
| Costa Rica | 9 | 4.57% | Allan Vargas Gonzalez; Carolina Vargas Loría; Daniel Cifuentes Jara; Francisco Jiménez Bolaños; José Solano; Lucas Gil Jimenez; Oscar Arango; Rojas Jiménez; Sergio Ortiz Pérez |
| Ecuador | 9 | 4.57% | Andrés Gustavo Vega Yépez; Cristian Abad; Fausto Mauricio Tinajero Camacho; Gustavo Andrés Molina Jaramillo; Juan Fernando Vega Rivadenira; Marco Encalada Larriva; Mario Calderon Barzallo; Veronica Tejeira; Wilson Bravo Torres |
| Guatemala | 9 | 4.57% | Alan Antillon; Alex Villela; Rodrigo Cayarga; José Molina Muñiz; Luis Fernando De León; Luis Grisolia; Luis Villacorta; Maria Del Pilar Urizar Urrutia; Otto Wug |
| Honduras | 9 | 4.57% | David Antón Hernández Rosales; Hervey Stacy Hunter Romero; Hugo Romero; Julio Cranshaw; Marcen Pinto A.; Mayra Elizabeth Pineda Salgado; Nadia Irias Funez; Sarahí Avila; Víctor Hugo David Campos |
| Paraguay | 9 | 4.57% | Hugo Enrique Aquino Gimenez; Jorge Gómez; José Manuel Lezcano Macchi; Luis Humberto Corbeta Argaña; Luis Meza; Luz González; Maria Cielo Bogarin Zalimben; Pánfilo Dominguez; Sonia María Raquel Galeano Acosta |
| Perú | 9 | 4.57% | Elmer H. Salinas Prieto; Gaby Malpartida; Jorge Noriega; Juan Francisco Berastain Arenas; Juan Francisco Ceccarelli Calle; Juan Manuel Sanchez Diaz; Lizeth Katheryn Carrion Mauricio; Patricia Horna Valle; Ruth Castillo Monzón |
| Dominican Republic | 9 | 4.57% | Ana Gonzalez Cabral; Carlos Brito; Wilson Olivo Canaan; Emilio Mateo; Luis Rafael III Serret Hernández; Miguel Iban Marrero; Rafael Llinas; Ramón Lalane; William Ariel Alvarez Cabreja |
| El Salvador | 8 | 4.06% | Adrian Avendano Valiente; Delmy M. Iglesias; Erick Naffry Saravia Lara; Erick Wahn Sosa; Gerardo Ernesto Cuenca Morales; Henry Danilo Aparicio Arce; Julio Enrique Rodríguez Castro; Rony Emerson Rivera Gomez |
| Panama | 8 | 4.06% | Gabriela Eisenmann; Gianni Calvosa; Mario Chalhoub; Mario Macrini; Marissa Cisneros; Mariulys Ramos; Marta Corro; Richard A. Ford Jimenez |
| Nicaragua | 7 | 3.55% | Gary Gutiérrez Núñez; Gerardo Avilés; Gonzalo Barquero Ortega; Gonzalo Wilfredo Navarro Murillo; Iván José Mendieta Herdocia; Julio Ochoa; Karla Margarita Sandoval Rojas |
| Uruguay | 6 | 3.05% | Daniel Rodriguez; Edgardo Andreu; Francisco Kolenc; Gerardo Gustavo Sagastume Cavelli; Magdalena Mayol; Marcos Di Pascua D'angelo |
In the first round, the established threshold for consensus (65%) was achieved in 30 questions (46.87%). In the second round, this level was achieved in 47 questions (73.43%). Consensus was completely reached on the field of “Diagnosis.” The field with the lowest level of consensus was “Demand for treatment with dental implants.” The consensus achieved for each field is depicted in Figure 1 and Table 2.
FIGURE 1.
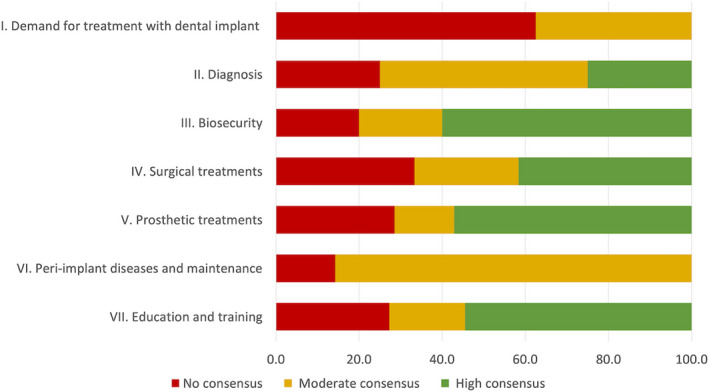
Level of consensus reached on each field (% distribution)
TABLE 2.
Open‐ended questionnaire validated by the Steering Committee
| Section | N | Question | Possible answers | Consensus achieved | ||
|---|---|---|---|---|---|---|
| I. Demand for treatment with dental implants | 1 | Demand for dental implant treatment | Will increase | Will decrease | Will remain ✓ | No Consensus 56.9% |
| 2 | Demand for dental implant treatment with a single missing tooth | Will increase | Will decrease | Will remain ✓ | No Consensus 56.9% | |
| 3 | Demand for dental implant treatment for partial edentulous patients | Will increase | Will decrease | Will remain ✓ | No Consensus 57.4% | |
| 4 | Demand for dental implant treatment for total edentulous patients | Will increase | Will decrease ✓ | Will remain | No Consensus 55.8% | |
| 5 | The profitability of implant treatments compared to general dentistry treatments will be | Higher | Less | Similar ✓ | No Consensus 57.4% | |
| 6 | The fees of dental implants and prosthetic components will be | Higher | Less | Similar ✓ | Moderate Consensus 70.6% | |
| 7 | For the professional, the laboratory cost for dental implants will be | Higher | Less | Similar ✓ | Moderate Consensus 72.1% | |
| 8 | For the patient, the fees of dental implant treatment will be | Higher | Less | Similar ✓ | Moderate Consensus 70.6% | |
| II. Diagnosis | 1 | Auxiliary diagnostic test required to discard SARS CoV‐2 | Agree ✓ | In disagreement | I'm not sure | Moderate Consensus 65% |
| 2 | Telemedicine will be a tool that must complement conventional evaluation | Agree ✓ | In disagreement | I'm not sure | Moderate consensus 75.6% | |
| 3 | Electronic dental record will replace physical dental history | Agree ✓ | In disagreement | I'm not sure | Moderate consensus 74.6% | |
| 4 | Tomographic analysis is a requirement for the preoperative diagnosis of dental implants | Agree ✓ | In disagreement | I'm not sure | High consensus 97% | |
| III. Biosecurity | 1 | In COVID‐19 pandemic, all patients should be considered as potential carriers of SARS‐CoV‐2 | Agree ✓ | In disagreement | I'm not sure | High consensus 98.5% |
| 2 | Transmission of SARS‐CoV‐2 can be 100% prevented | Agree ✓ | In disagreement | I'm not sure | High consensus 99% | |
| 3 | Each staff member should receive formal training of the use of personal protective equipment (PPE) before any contact with patients | Agree ✓ | In disagreement | I'm not sure | Moderate consensus 71.1% | |
| 4 | Each staff member should receive frequent diagnostic tests of SARS‐CoV‐2 | Agree ✓ | In disagreement | I'm not sure | Moderate consensus 65.7% | |
| 5 | Patients who will undergo surgical procedures must previously perform the diagnostic test for SARS‐CoV‐2 | Agree ✓ | In disagreement | I'm not sure | No consensus 42.6% | |
| 6 | Patients who will undergo prosthetic treatment must previously perform the diagnostic test for SARS‐CoV‐2 | Agree | In disagreement ✓ | I'm not sure | No consensus 59.4% | |
| 7 | The patient must sign an informed consent about the risk of contagion of SARS‐CoV‐2 and its possible consequences | Agree ✓ | In disagreement | I'm not sure | High consensus 88.9% | |
| 8 | The minimum standard for "full" PPE shall include surgical cap, antifluid gown with long sleeves, eye protection, N95‐99 or FFP2‐3 mask, face shield, and double layer disposable gloves | Agree ✓ | In disagreement | I'm not sure | High consensus 88.3% | |
| 9 | The dentist and team members must use a different PPE for each patient (surgical cap, antifluid gown with long sleeves, eye protection, N95‐99 or FFP2‐3 mask, face shield, and double layer of disposable gloves) | Agree ✓ | In disagreement | I'm not sure | Moderate consensus 79.2% | |
| 10 | Only essential personnel should be present in the area during patient care | Agree ✓ | In disagreement | I'm not sure | High consensus 99% | |
| 11 | Temperature recording is required for all staff members and patients before entering the dental office | Agree ✓ | In disagreement | I'm not sure | High consensus 88.3% | |
| 12 | No change of personnel or area should be made during the procedures, except in emergency situations | Agree ✓ | In disagreement | I'm not sure | High consensus 96.5% | |
| 13 | The activities with aerosol‐generating instruments must be done four‐handed | Agree ✓ | In disagreement | I'm not sure | High consensus 93.9% | |
| 14 | The activities with aerosol‐generating instruments must be carried out in wide and ventilated environments to minimize staff viral exposure | Agree ✓ | In disagreement | I'm not sure | High consensus 93.4% | |
| 15 | Photographic records are required during the intervention or procedures by a third assistant | Agree ✓ | In disagreement | I'm not sure | No consensus 61.4% | |
| IV. Surgical treatments | 1 | Dental implant placement in the future will be in the operating room | Agree | In disagreement ✓ | I'm not sure | Moderate Consensus 77.2% |
| 2 | The patient should have mouthwashes before each intervention | Agree ✓ | In disagreement | I'm not sure | High Consensus 98.5% | |
| 3 | In the future, the dental implant placement will be mainly through | Guided surgery ✓ | Surgical guide | Without Guide | Moderate Consensus 77.2% | |
| 4 | In the future, computer‐assisted surgery will be | More frequently ✓ | Less frequent | Similar | High Consensus 93.4% | |
| 5 | In the future, flapless surgery will be | More frequently ✓ | Less frequent | Similar | No Consensus 62.4% | |
| 6 | The procedures for obtaining autologous soft tissue grafts will be | More frequent ✓ | Less frequent | Similar | No Consensus 48.7% | |
| 7 | The procedures for obtaining autologous hard tissue grafts will be | More frequent | Less frequent ✓ | Similar | No Consensus 55.3% | |
| 8 | The use of aerosol‐generating instruments during surgical procedures will be | More frequently | Less frequent | Similar ✓ | Moderate Consensus 72.6% | |
| 9 | The use of absorbable suture will be | More frequently ✓ | Less frequent | Similar | No Consensus 59.4% | |
| 10 | The prescription of nonsteroidal anti‐inflammatory drugs will be | More frequently | Less frequent | Similar ✓ | High Consensus 87.8% | |
| 11 | The prescription of steroidal anti‐inflammatory drugs will be | More frequently | Less frequent | Similar ✓ | High Consensus 86.8% | |
| 12 | The prescription of systemic antibiotic therapy after surgery will be | More frequently | Less frequent | Similar ✓ | High Consensus 88.8% | |
| V. Prosthetic treatments | 1 | Immediate loading protocols will be | More frequent ✓ | Less frequent | Similar | No consensus 61.4% |
| 2 | Conventional loading protocols will be | More frequent | Less frequent | Similar ✓ | Moderate consensus 73.1% | |
| 3 | The trend regarding impressions will be | Digital ✓ | Conventional or Analog | Both | No consensus 50.8% | |
| 4 | The use of CAD / CAM in implant prosthetics will be | More frequently ✓ | Less frequent | Similar | High consensus 90.4% | |
| 5 | A disinfection protocol must be followed for elastomer and hydrocolloid impressions | Agree ✓ | In disagreement | I'm not sure | High consensus 98% | |
| 6 | Prosthetic components sent to the laboratory must be previously sterilized | Agree ✓ | In disagreement | I'm not sure | High consensus 87.3% | |
| 7 | Prosthetic components from the laboratory must be sterilized | Agree ✓ | In disagreement | I'm not sure | High consensus 87.3% | |
| VI. Peri‐implant diseases and maintenance | 1 | The frequency of maintenance visits will be | Higher | Less | Similar ✓ | Moderate consensus 72.6% |
| 2 | The prevalence of mucositis will be | Higher | Less | Similar ✓ | Moderate consensus 71.6% | |
| 3 | The prevalence of peri‐implantitis will be | Higher | Less | Similar ✓ | No consensus 64% | |
| 4 | The prevalence of soft tissue deficiencies will be | Higher | Less | Similar ✓ | Moderate consensus 78.2% | |
| 5 | The prevalence of hard tissue deficiencies will be | Higher | Less | Similar ✓ | Moderate consensus 83.8% | |
| 6 | The prevalence of prosthetic complications will be | Higher | Less | Similar ✓ | Moderate consensus 71.6% | |
| 7 | As part of maintenance, telemedicine will be a useful tool for monitoring and controlling patients | Agree ✓ | In disagreement | I'm not sure | Moderate consensus 76.1% | |
| VII. Education and training | 1 | Oral implantology education will be trained primarily | Face‐to‐face | Virtual | Both of them ✓ | Moderate consensus 73.6% |
| 2 | Oral implantology education will be trained primarily by | Higher education centers ✓ | Scientific organizations | Commercial houses | No consensus 63.5% | |
| 3 | The didactic strategies for implant placement training will be | Animal model | Simulators ✓ | Models | Moderate consensus 78.7% | |
| 4 | The curriculum plan of the higher education centers must restructure the hours of clinical activity | Agree ✓ | In disagreement | I'm not sure | High consensus 91.9% | |
| 5 | The learning methodology of the higher education centers should be redesigned | Agree ✓ | In disagreement | I'm not sure | High consensus 95.4% | |
| 6 | Higher education centers will privilege the virtual modality for the theoretical activity | Agree ✓ | In disagreement | I'm not sure | High consensus 88.3% | |
| 7 | The infrastructures of higher education center shall redesign for maintaining social distancing | Agree ✓ | In disagreement | I'm not sure | High consensus 93.4% | |
| 8 | The number of patients for requirement clinical practices | Will increase | Will decrease✓ | Will remain | Moderate consensus 65% | |
| 9 | The clinical practice hours requirement with patients | Will increase | Will decrease | Will remain | No consensus 48.7% | |
| 10 | The hours of laboratory practices by simulators | Will increase✓ | Will decrease | Will remain | High consensus 86.8% | |
| 11 | It is necessary to assign a committee for prevention of COVID in educational centers | Agree ✓ | In disagreement | I'm not sure | High consensus 87.3% | |
The most frequent answer to each question is highlighted in bold.
In the field of “Demand for treatment with dental implants,” there was moderate consensus in 3 out of the 8 questions (Figure 2). The experts responded that there will be no changes in the fees of dental implants and prosthetic components (70.05%), laboratory cost (72.08%), or the costs for the patients (70.56%). However, there was no consensus in regard to the demand for dental implants irrespectively of the type of edentulism.
FIGURE 2.
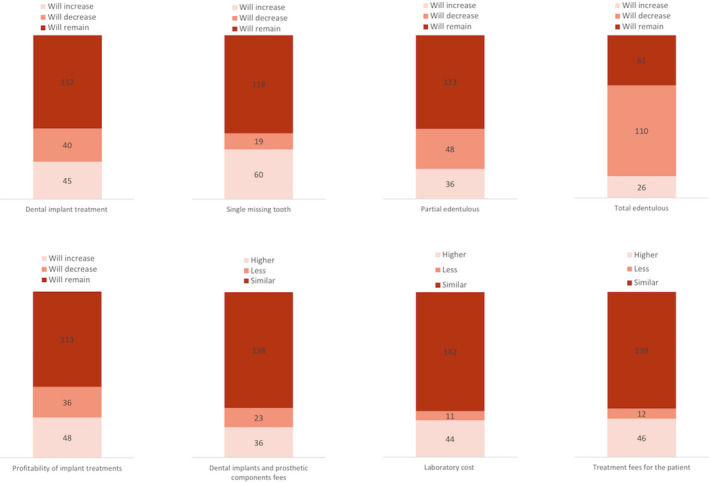
Answers from the experts for each question on the field of “Demand for dental implant treatment”
The questions related to the field “Diagnosis” provided moderate to high consensus (Figure 3). There was a clear high consensus for the use of tomography during preoperative diagnosis (96.95%). In regard to digital tools, there was moderate consensus for the use of telemedicine as an adjunctive measure to conventional evaluation (75.64%) and to the fact that electronic dental record will replace physical dental history (74.62%). The use of tests to detect the virus SARS‐CoV‐2 reached the lower borderline of consensus (65%).
FIGURE 3.
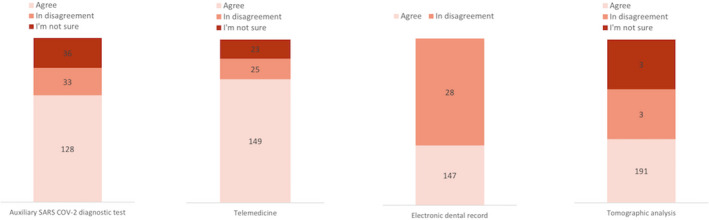
Answers from the experts for each question on the field of “Diagnosis”
The field of “Biosecurity” reached a moderate to high consensus in 12 out of the 15 questions (Figure 4). Some of the questions such as “In COVID‐19 pandemic, all patients should be considered as potential carriers of SARS‐CoV‐2” and “Transmission of SARS‐CoV‐2 can be 100% prevented,” reached a very high consensus (98.48% and 98.98%, respectively). However, there was no consensus for the use of a diagnostic test for SARS‐CoV‐2 before surgical (42.64%) or prosthetic treatment (59.39%). Moreover, the need of a third assistant to take photographs did not reach consensus (61.42%).
FIGURE 4.

Answers from the experts for each question on the field of “Biosecurity”
There was consensus in 8 out of the 12 questions related to the “Surgical treatments” (Figure 5). Most of the experts agreed that the patient should use mouthwashes before surgery (98.48%) and that the use of aerosol‐generating instruments during surgical procedures will be less frequent (93.40%). Moreover, an important number of participants also disagreed that implants will be placed in the operating room (77.16%). In regard to medication, most of the experts answered that the prescription of nonsteroidal anti‐inflammatory drugs (87.82%), steroidal anti‐inflammatory drugs (86.8%), or systemic antibiotic therapy after surgery (88.83%) will be similar to how has been used before the pandemic. No consensus was achieved for the use of flapless approaches (62.4%), for the type of suture (59.4%), or for the frequency of soft (48.7%) or hard (55.3%) autologous grafts.
FIGURE 5.
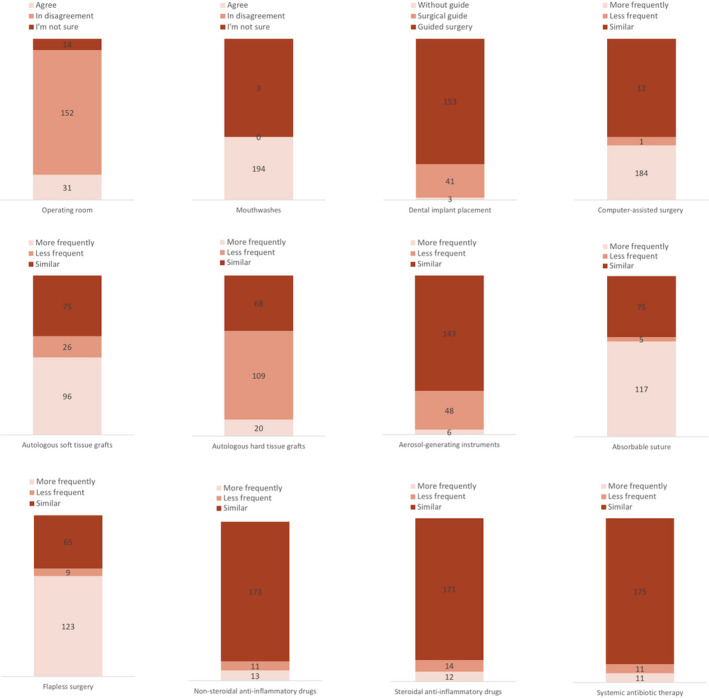
Answers from the experts for each question on the field of “Surgical approaches”
In the field “Prosthetic treatments,” there was high consensus for the fact that we must disinfect/sterilize the impression materials (97.97%), the prosthetic components sent to the laboratory” (87.31%) and the prosthetic components from the laboratory (87.31%) (Figure 6). Also, most of the experts agreed that the use of CAD/CAM technologies in the field of implantology would be more frequently” (90.36%). However, there was no consensus for the use of digital technologies to take impressions (50.76%). In regard to the time of loading, conventional protocols will be similar to before the pandemic (73.10%).
FIGURE 6.
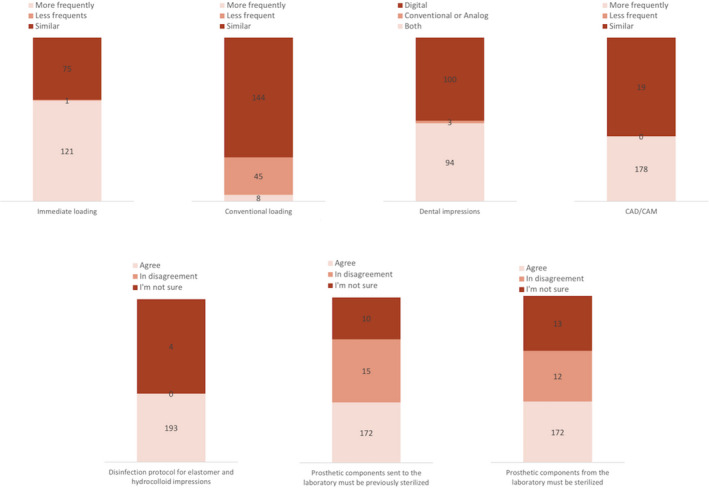
Answers from the experts for each question on the field of “Prosthetic approaches”
Most of the questions evaluated in the field “Peri‐implant diseases and maintenance” reached moderate consensus (Figure 7). The respondents estimated that 6 out of the 7 items evaluated would have a similar frequency. However, there was no consensus for the prevalence of peri‐implantitis (63.96%). Furthermore, the experts reached moderate consensus in regard to the question whether telemedicine will be a useful tool for monitoring and controlling patients (76.14%).
FIGURE 7.
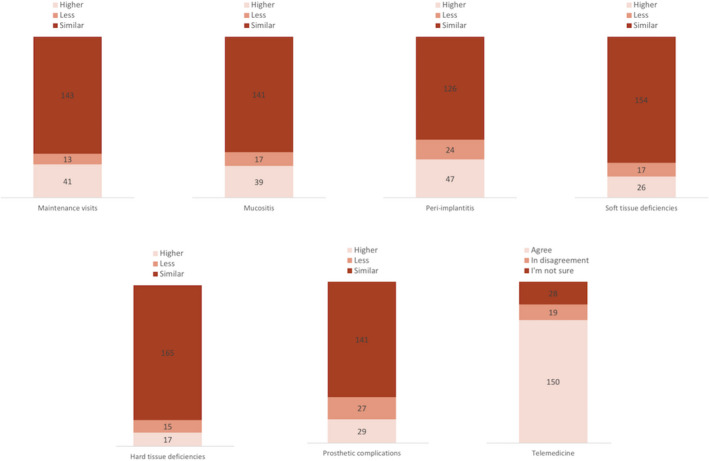
Answers from the experts for each question on the field of “Peri‐implant diseases and maintenance”
Finally, regarding the questions related to the field “Education and training in implant dentistry” the respondents achieved a high consensus for those questions highlighting that changes should be made in the basis of the hours of clinical activity within the curriculum plan (91.88%), the learning methodology (95.43%), the shift from presence to virtual attendance (88.32%), and the design of education centers to maintain social distance (94.40%). Furthermore, the experts estimated that oral implantology education will be trained face to face and by virtual education (73.60%) and that simulator will be used for implant placement training (78.68%). There was no consensus to recognize neither if higher education centers or scientific organizations will head education (63.45%) nor to an increase in the number of hours of clinical practice with patients (48.73%) (Figure 8).
FIGURE 8.
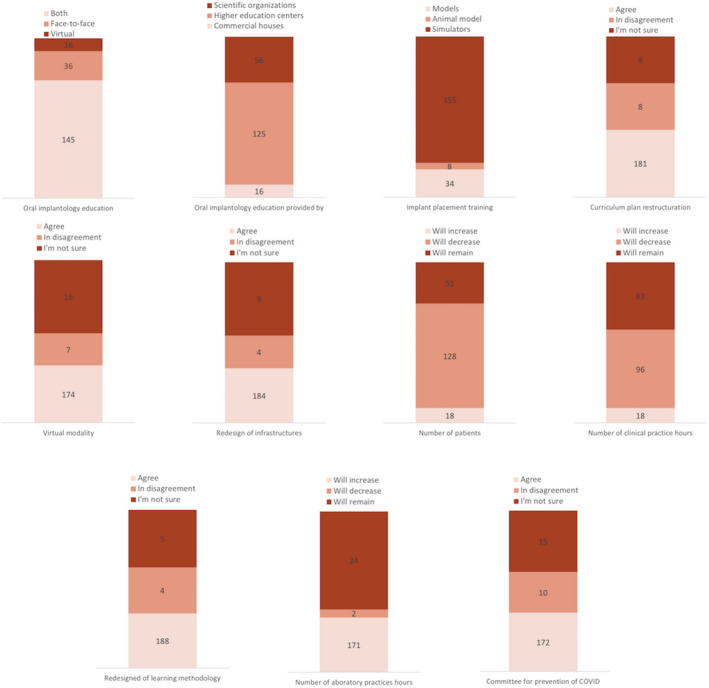
Answers from the experts for each question on the field of “Education and training”
4. DISCUSSION
The results from the present study have provided important and useful information on the trends in Implant Dentistry in the COVID‐19 era. Medical publications have recently used this methodology to generate consensus and provide recommendations for care in times of COVID‐19 (Alterio et al., 2020; Bhandari et al., 2020; Gelfand et al., 2020; Pouwels et al., 2020). The importance of these results is magnified by the fact that the study was carried out in the LA region, which presents its own cultural and economic characteristics. Furthermore, due to the representativeness within Implant Dentistry of the selected experts, the high response rate achieved and the high level of consensus in most of the items evaluated, this report will be relevant for scientific organizations, universities, and dentists that may consider these tendencies in the implementation of the needed changes for improving the practice of implant dentistry during and after the pandemic situation.
4.1. Treatment demand for dental implants
In spite of the data from the increase in life expectancy and the concern to maintain teeth in the LA population (Kassebaum et al., 2017), there was no consensus on how the demand for dental implant treatment will be in the future. It is interesting to observe the impact of the evolution of the COVID‐19 pandemic, since there was a tendency toward a more positive outlook in terms of demand, between the first and second round of questionnaires, coinciding with the return to the dental practice after the pandemic lockout. It remains unclear, however, what will be the impact of the COVID‐19 pandemic (Bolaño‐Ortiz et al., 2020) on the treatment of totally edentulous elderly subjects (Srinivasan et al., 2017). The experts concluded that more than the treatment costs, the cost‐effectiveness will be affected by this pandemic. Among other issues, the implementation of strict biosecurity protocols will affect practice times and number of patients treated, hence causing a detrimental effect on the practice economic outcome.
4.2. Diagnosis
Even though the experts agree that direct presence of the patient for a clinical examination is still a requirement of the appropriate diagnosis of a patient candidate for dental implants, the use of teledentistry will increase and thus reduce the duration of consultations and the exposure of staff and patients. Some aspects that could be remotely evaluated are the update of the medical and dental history, the radiographic examination and the assessment of patient preferences, and wishes and queries related to the prosed treatment plan (Ghai, 2020). In this sense, the use of a digital dental records could also be advised (moderate consensus), although this will depend on the legal validity of this document in each country.
4.3. Biosecurity
The dental team has been regularly using infection control measures before the COVID‐19 pandemic; however, most of the experts responded that these measurements should be enhanced in light of the SARS‐CoV‐2 infectivity, mainly in cases of procedures generating aerosols (Herrera et al., 2020; Li et al., 2020; Umer et al., 2020). However, the experts did not agree on whether full personal protective equipment should be worn for each patient. Moreover, there was no consensus on the need of diagnostic for SARS‐CoV‐2 virus to every patient in the dental clinic (Gurzawska‐Comis et al., 2020), since some experts found it unattainable. Instead, experts suggested the filling by every patient of a self‐reported medical questionnaire and telephone triage prior to each appointment, as well as the strict abidement to all the infection control measures during the patient visits to the dental office. Experts found this protocol sufficient to reduce the risk of infection in the dental office, in line with international recommendations (Centers for Disease Control & Prevention, 2020; Gurzawska‐Comis et al., 2020; Ren et al., 2020).
It is interesting to discuss that experts agreed that the transmission SARS‐CoV‐2 can be 100% prevented despite the complete prevention of SARS‐CoV‐2 is yet almost unheard. This could be explained by their clinical experience during these pandemic months, employing suitable biosecurity measures that protected them from infection. Moreover, emerging evidence is showing that by applying proper biosecurity protocols, the risk of infection in the dental setting is very low (Froum & Froum, 2020; Kumbargere Nagraj et al., 2020). Also, one could debate why the transmission of SARS‐CoV‐2 should be addressed in the future when the vaccine may end up with the pandemic. However, since we still do not know how effective it will be and how long it will stand, we might need to live together with the virus even after a vaccine is available, being the transmission methods against SARS‐CoV‐2 probably necessary.
With vaccination starting now all over the world, one could think that the outcomes of this project would be different, which could be right in the best possible scenario where once the patients receive the vaccine they are immunized forever. However, as it occurs with influenza virus, we might need to live together with the virus having yearly vaccines, which are not 100% effective (Demicheli et al., 2018). Moreover, the risk of future zoonotic diseases due to climate change and human expansion (Hashimoto et al., 2020) justifies evaluating how a future pandemic situation could affect the trends in Implant Dentistry.
4.4. Surgical treatment
The surgical phase of dental implants may become a challenge with the newly established protocols for COVID‐19. It is interesting to note that experts believed that a special operating room would not be a requirement to perform surgery as long as the dental office complies with the established protocols.
There was a very high consensus toward the use of mouthwashes before each intervention and the reduction of aerosol‐generating instruments during surgical procedures, which should be taken with caution since there is not sufficient clinical evidence to support the antiviral activity of reagents in mouth rinses against SARS‐CoV‐2 (Carrouel et al., 2020). Emerging data clearly shows extremely short‐lasting action of mouthwash in reducing SARS‐CoV‐2 virus in saliva/oral cavity, and therefore, its use may give a totally false sense of security (Yoon et al., 2020). Moreover, despite it is known that the virus content is reduced immediately after rinsing, implant procedures generally last longer than seconds or a minute, and tissue manipulation in the mouth may further increase the flow of contaminated saliva with newly produced virus.
In addition, before a vaccine against COVID‐19 is available, experts recommend the implementation of different strategies and measures, such as the personal protective equipment, barrier devices to minimize aerosol contamination, air purification systems, antiviral chemicals to clean surfaces, chairside screening for SARS‐CoV‐2, or other future innovations (Ali & Raja, 2020). In regard to medications, most of the experts agreed that there would not be major variations to the prescription of nonsteroidal or steroidal anti‐inflammatory drugs and systemic antibiotic therapy after surgery, although practitioners should be knowledgeable on the health risks of these medications, mainly in patients with systemic conditions (Crighton et al., 2020).
4.5. Prosthetic treatment
Experts agreed that the current situation will accelerate the shift from conventional prosthetic methods to a full digital workflow in implant dentistry. There was a very high consensus toward the increased use of CAD/CAM technologies, which is in agreement with a similar Delphi study on implant dentistry from Europe (Sanz et al., 2019). Experts also agreed that it is currently necessary to apply strict methods of infection control during the restorative procedures, by disinfecting all prosthetic components and impression materials. In fact, there is scientific evidence of the importance of sterilizing prosthetic devices for biosecurity and prevention of biological complications (Bidra et al., 2020; Canullo et al., 2015).
4.6. Peri‐implant diseases and maintenance
Due to the pandemic, the fear of infection in the population will indeed refrain many patients from attending preventive and supportive therapy appointments. In spite of this, experts estimated that the incidence of peri‐implant diseases and prosthetic complications will be similar to what is today. This problem could be counteracted by the use of telemedicine, providing a quicker access to the dentist without attending the dental office (Maret et al., 2020). Nevertheless, clinical and radiographic evaluation are still necessary for the proper diagnosis of peri‐implant health or disease, and therefore, it is important that the professional can discern when the patient must come in person. Implementing this tool proactively is likely to generate greater benefits in the long term and help with the everyday (and emergency) challenges of general health care (Smith et al., 2020).
4.7. Education and training
One of the aspects that the COVID‐19 has impacted more strongly is education, with clear shift to change presence to remote education. There was a high consensus that there is a need to change the educational plans and learning methods in higher education institutions (Spanemberg et al., 2020). New educational models should be developed with an increasing use of virtual simulation technologies that will replace, at least in part, traditional preclinical education (Galibourg et al., 2020). However, its use in LA may be limited, at least in the immediate future, due to their high cost, and therefore, universities should develop policies to adapt their infrastructures for maintain the recommended social distancing and for assuring the protection of students, staff, and patients during the practical education in implant dentistry (Iyer, Aziz, & Ojcius, 2020).
One important limitation of this study that could have influenced the results is the potential conflict of interest, as all experts could have an inherent conflict of interest related to their jobs, their business, or their research. The management of conflict of interests was discussed with the Steering Committee and the Advisory group following the principles provided by the Guidelines International Network (Schünemann et al., 2015). According to these principles, experts with relevant potential conflict of interests abstained from commenting or recommending during the consensus conference. It should be noted that each country was asked to select experts with no direct conflicts of interest to the study.
In conclusion, the present study using the Delphi methodology in LA has provided insightful and useful information in regard to the practice of Implant Dentistry during and after the COVID‐19 era. Scientific organizations, universities, and dentists should consider these tendencies in the implementation of the needed changes for improving the practice of implant dentistry during and after the pandemic situation.
CONFLICTS OF INTEREST
The authors report no conflicts of interest related to this study.
AUTHOR CONTRIBUTIONS
M.A. and I.S. conceived the ideas drafted in the manuscript. J.A., A.T., A.L.P., L.M., and M.S. designed the questionnaire. S.C., A.L., P.J., R.D., R.T., J.A., A.A., R.G., V.U., M.S., C.I., C.Y., J.C., L.C., and L.B. validated the questionnaire and supervised the application of the questionnaire in each country. J.A., A.L.P., L.M., and M.S. drafted the manuscript. M.A., I.S., L.M., A.L.P., and R.L. analyzed the data. M.A., A.L.P., M.S., and I.S. critically reviewed the manuscript. All the authors participated in the consensus meeting.
Supporting information
Supplementary Material
ACKNOWLEDGMENTS
The authors would like to acknowledge the support from the Ibero Panamerican Federation of Periodontology (FIPP) and the Peruvian Association of Oral Implantology (ASPIOI). This study could not have been possible without the efforts from the 197 experts participating in the project.
Alarcón MA, Sanz‐Sánchez I, Shibli JA, et al. Delphi Project on the trends in Implant Dentistry in the COVID‐19 era: Perspectives from Latin America. Clin Oral Impl Res. 2021;32:521–537. 10.1111/clr.13723
REFERENCES
- Ali, K. , & Raja, M. (2020). Coronavirus disease 2019 (COVID‐19): Challenges and management of aerosol‐generating procedures in dentistry. Evidence‐Based Dentistry, 21(2), 44–45. 10.1038/s41432-020-0088-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- AL‐Maweri, S. A. , Halboub, E. , & Warnakulasuriya, S. (2020). Impact of COVID‐19 on the early detection of oral cancer: A special emphasis on high risk populations. Oral Oncology, 106, 104760. 10.1016/j.oraloncology.2020.104760 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alterio, D. , Volpe, S. , Bacigalupo, A. , Bonomo, P. , De Felice, F. , Dionisi, F. , D'Onofrio, I. , D'Angelo, E. , Di Rito, A. , Fanetti, G. , Franco, P. , Maddalo, M. , Merlotti, A. , Micciché, F. , Orlandi, E. , Paiar, F. , Ursino, S. , Pepa, M. , Corvò, R. , … Musio, D. (2020). Head and neck radiotherapy amid the COVID‐19 pandemic: Practice recommendations of the Italian Association of Radiotherapy and Clinical Oncology (AIRO). Medical Oncology, 37(10), 85. 10.1007/s12032-020-01409-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bhandari, P. , Subramaniam, S. , Bourke, M. J. , Alkandari, A. , Chiu, P. W. Y. , Brown, J. F. , Keswani, R. N. , Bisschops, R. , Hassan, C. , Raju, G. S. , Muthusamy, V. R. , Sethi, A. , May, G. R. , Albéniz, E. , Bruno, M. , Kaminski, M. F. , Alkhatry, M. , Almadi, M. , Ibrahim, M. , … Repici, A. (2020). Recovery of endoscopy services in the era of COVID‐19: Recommendations from an international Delphi consensus. Gut, 69(11), 1915–1924, 10.1136/gutjnl-2020-322329 [DOI] [PubMed] [Google Scholar]
- Bidra, A. S. , Kejriwal, S. , & Bhuse, K. (2020). Should healing abutments and cover screws for dental implants be reused? A systematic review. Journal of Prosthodontics, 29(1), 42–48. 10.1111/jopr.13106 [DOI] [PubMed] [Google Scholar]
- Bolaño‐Ortiz, T. R. , Camargo‐Caicedo, Y. , Puliafito, S. E. , Ruggeri, M. F. , Bolaño‐Diaz, S. , Pascual‐Flores, R. , Saturno, J. , Ibarra‐Espinosa, S. , Mayol‐Bracero, O. L. , Torres‐Delgado, E. , & Cereceda‐Balic, F. (2020). Spread of SARS‐CoV‐2 through Latin America and the Caribbean region: A look from its economic conditions, climate and air pollution indicators. Environmental Research, 191, 109938. 10.1016/j.envres.2020.109938 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boyce, R. A. (2021). Prosthodontic principles in dental implantology: Adjustments in a coronavirus disease‐19 pandemic‐battered economy. Dental Clinics of North America, 65(1), 135–165. 10.1016/j.cden.2020.09.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Canullo, L. , Peñarrocha, D. , Clementini, M. , Iannello, G. , & Micarelli, C. (2015). Impact of plasma of argon cleaning treatment on implant abutments in patients with a history of periodontal disease and thin biotype: Radiographic results at 24‐month follow‐up of a RCT. Clinical Oral Implants Research, 26(1), 8–14. 10.1111/clr.12290 [DOI] [PubMed] [Google Scholar]
- Carrouel, F. , Gonçalves, L. S. , Conte, M. P. , Campus, G. , Fisher, J. , Fraticelli, L. , Gadea‐Deschamps, E. , Ottolenghi, L. , & Bourgeois, D. (2020). Antiviral activity of reagents in mouth rinses against SARS‐CoV‐2. Journal of Dental Research, 100(2), 124–132. 10.1177/0022034520967933 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention . (2020). Guidance for dental settings. Interim infection prevention and control guidance for dental settings during the COVID‐19 response. Retrieved from https://www.cdc.gov/coronavirus/2019‐ncov/hcp/dental‐settings.html
- Crighton, A. J. , McCann, C. T. , Todd, E. J. , & Brown, A. J. (2020). Safe use of paracetamol and high‐dose NSAID analgesia in dentistry during the COVID‐19 pandemic. British Dental Journal, 229(1), 15–18. 10.1038/s41415-020-1784-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dalkey, N. , & Helmer, O. (1963). An experimental application of the DELPHI method to the use of experts. Management Science, 9(3), 458–467. 10.1287/mnsc.9.3.458 [DOI] [Google Scholar]
- Demicheli, V. , Jefferson, T. , Ferroni, E. , Rivetti, A. , & Di Pietrantonj, C. (2018). Vaccines for preventing influenza in healthy adults. Cochrane Database of Systematic Reviews, 2(2), CD001269. 10.1002/14651858.CD001269 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Froum, S. H. , & Froum, S. J. (2020). Incidence of COVID‐19 virus transmission in three dental offices: A 6‐month retrospective study. International Journal of Periodontics & Restorative Dentistry, 40(6), 853–859. 10.11607/prd.5455 [DOI] [PubMed] [Google Scholar]
- Galibourg, A. , Maret, D. , Monsarrat, P. , & Nasr, K. (2020). Impact of COVID‐19 on dental education: How could pre‐clinical training be done at home? Journal of Dental Education, 84(9), 949. 10.1002/jdd.12360 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gelfand, J. M. , Armstrong, A. W. , Bell, S. , Anesi, G. L. , Blauvelt, A. , Calabrese, C. , Dommasch, E. D. , Feldman, S. R. , Gladman, D. , Kircik, L. , Lebwohl, M. , Lo Re, V. , Martin, G. , Merola, J. F. , Scher, J. U. , Schwartzman, S. , Treat, J. R. , Van Voorhees, A. S. , Ellebrecht, C. T. , … Ritchlin, C. T. (2020). National psoriasis foundation COVID‐19 task force guidance for management of psoriatic disease during the pandemic: Version 1. Journal of the American Academy of Dermatology, 83(6), 1704–1716. 10.1016/j.jaad.2020.09.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ghai, S. (2020). Teledentistry during COVID‐19 pandemic. Diabetes & Metabolic Syndrome: Clinical Research & Reviews, 14(5), 933–935. 10.1016/j.dsx.2020.06.029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gurzawska‐Comis, K. , Becker, K. , Brunello, G. , Gurzawska, A. , & Schwarz, F. (2020). Recommendations for dental care during COVID‐19 pandemic. Journal of Clinical Medicine, 9(6), 1833. 10.3390/jcm9061833 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hashimoto, S. , Hikichi, M. , Maruoka, S. , & Gon, Y. (2020). Our future: Experiencing the coronavirus disease 2019 (COVID‐19) outbreak and pandemic. Respiratory Investigation, 5345(20), 30181–30187. 10.1016/j.resinv.2020.11.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herrera, D. , Serrano, J. , Roldán, S. , & Sanz, M. (2020). Is the oral cavity relevant in SARS‐CoV‐2 pandemic? Clinical Oral Investigations, 24(8), 2925–2930. 10.1007/s00784-020-03413-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iyer, P. , Aziz, k. , & Ojcius, D.M. (2020). Impact of COVID‐19 on dental education in the United States. Journal of Dental Education, 84(6), 718–722. 10.1002/jdd.12163 [DOI] [PubMed] [Google Scholar]
- Kassebaum, N. J. , Smith, A. , Bernabé, E. , Fleming, T. D. , Reynolds, A. E. , Vos, T. , Murray, C. , Marcenes, W. , Abyu, G. Y. , Alsharif, U. , Asayesh, H. , Benzian, H. , Dandona, L. , Dandona, R. , Kasaeian, A. , Khader, Y. S. , Khang, Y. H. , Kokubo, Y. , Kotsakis, G. A. , … Yonemoto, N. (2017). Global, regional, and national prevalence, incidence, and disability‐adjusted life years for oral conditions for 195 countries, 1990–2015: A systematic analysis for the global burden of diseases, injuries, and risk factors. Journal of Dental Research, 96(4), 380–387. 10.1177/0022034517693566 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kumbargere Nagraj, S. , Eachempati, P. , Paisi, M. , Nasser, M. , Sivaramakrishnan, G. , & Verbeek, J. H. (2020). Interventions to reduce contaminated aerosols produced during dental procedures for preventing infectious diseases. Cochrane Database of Systematic Reviews, 10, CD013686. 10.1002/14651858.CD013686.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li, D. T. S. , Samaranayake, L. P. , Leung, Y. Y. , & Neelakantan, P. (2020). Facial protection in the era of COVID‐19: A narrative review. Oral Diseases, 13460. Epub ahed of print. 10.1111/odi.13460 [DOI] [PMC free article] [PubMed] [Google Scholar]
- López Jordi, M.D. , Figueiredo, M.C. , Barone, D. , & Pereira, C. (2016). Study and analysis of information technology in dentistry in Latin American countries. Acta Odontologica Latinoamericana, 29(1), 14–22. [PubMed] [Google Scholar]
- Madianos, P. , Papaioannou, W. , Herrera, D. , Sanz, M. , Baeumer, A. , Bogren, A. , Bouchard, P. , Chomyszyn‐Gajewska, M. , Demirel, K. , Gaspersic, R. , Giurgiu, M. , Graziani, F. , Jepsen, K. , Jepsen, S. , O′Brien, T. , Polyzois, I. , Preshaw, P. M. , Rakic, M. , Reners, M. , … Llodra, J. C. (2016). EFP Delphi study on the trends in Periodontology and Periodontics in Europe for the year 2025. Journal of Clinical Periodontology, 43(6), 472–481. 10.1111/jcpe.12551 [DOI] [PubMed] [Google Scholar]
- Maret, D. , Peters, O. A. , Vaysse, F. , & Vigarios, E. (2020). Integration of telemedicine into the public health response to COVID‐19 must include dentists. International Endodontic Journal, 53(6), 880–881. 10.1111/iej.13312 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meng, L. , Hua, F. , & Bian, Z. (2020). Coronavirus disease 2019 (COVID‐19): Emerging and future challenges for dental and oral medicine. Journal of Dental Research, 99(5), 481–487. 10.1177/0022034520914246 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nibali, L. , Ide, M. , Ng, D. , Buontempo, Z. , Clayton, Y. , & Asimakopoulou, K. (2020). The perceived impact of Covid‐19 on periodontal practice in the United Kingdom: A questionnaire study. Journal of Dentistry, 102, 103481. 10.1016/j.jdent.2020.103481 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nuzzo, J. , Moss, B. , Kahn, J. , & Rutkow, L. ; Applied Physics Laboratory . (2020). The Johns Hopkins Coronavirus Resource Center. Retrieved from https://coronavirus.jhu.edu/map.html
- Pouwels, S. , Omar, I. , Aggarwal, S. , Aminian, A. , Angrisani, L. , Balibrea, J. M. , Bhandari, M. , Biter, L. U. , Blackstone, R. P. , Carbajo, M. A. , Copaescu, C. A. , Dargent, J. , Elfawal, M. H. , Fobi, M. A. , Greve, J.‐W. , Hazebroek, E. J. , Herrera, M. F. , Himpens, J. M. , Hussain, F. A. , … Mahawar, K. (2020). The first modified Delphi consensus statement for resuming bariatric and metabolic surgery in the COVID‐19 times. Obesity Surgery, 31(1), 451–456. 10.1007/s11695-020-04883-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ren, Y. , Feng, C. , Rasubala, L. , Malmstrom, H. , & Eliav, E. (2020). Risk for dental healthcare professionals during the COVID‐19 global pandemic: An evidence‐based assessment. Journal of Dentistry, 101, 103434. 10.1016/j.jdent.2020.103434 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Romito, G. A. , Feres, M. , Gamonal, J. , Gomez, M. , Carvajal, P. , Pannuti, C. , Duque Duque, A. , Romanelli, H. , Rösing, C. K. , Aranguiz Freyhofer, V. , Cavagni, J. , Fischer, R. G. , Figueiredo, L. , Carrer, F. C. D. A. , Malheiros, Z. , Stewart, B. , Sanz, M. , & Ryan, M. (2020). Periodontal disease and its impact on general health in Latin America: LAOHA consensus meeting report. Brazilian Oral Research, 34(suppl 1), e027. 10.1590/1807-3107bor-2020.vol34.0027 [DOI] [PubMed] [Google Scholar]
- Rutkowski, J. L. , Camm, D. P. , & el Chaar, E. (2020). AAID white paper: Management of the dental implant patient during the COVID‐19 pandemic and beyond. Journal of Oral Implantology, 46(5), 454–466. 10.1563/aaid-joi-d-20-00316 [DOI] [PubMed] [Google Scholar]
- Sanz, M. , Noguerol, B. , Sanz‐Sanchez, I. , Hammerle, C. H. F. , Schliephake, H. , Renouard, F. , Sicilia, A. , Cordaro, L. , Jung, R. , Klinge, B. , Valentini, P. , Alcoforado, G. , Ornekol, T. , Pjetursson, B. , Sailer, I. , Rochietta, I. , Manuel Navarro, J. , Heitz‐Mayfield, L. , & Francisco, H. (2019). European Association for Osseointegration Delphi study on the trends in Implant Dentistry in Europe for the year 2030. Clinical Oral Implants Research, 30(5), 476–486. 10.1111/clr.13431 [DOI] [PubMed] [Google Scholar]
- Schünemann, H. J. , Al‐Ansary, L. A. , Forland, F. , Kersten, S. , Komulainen, J. , Kopp, I. B. , Macbeth, F. , Phillips, S. M. , Robbins, C. , van der Wees, P. , & Qaseem, A. (2015). Guidelines international network: Principles for disclosure of interests and management of conflicts in guidelines. Annals of Internal Medicine, 163(7), 548. 10.7326/M14-1885 [DOI] [PubMed] [Google Scholar]
- Smith, A. C. , Thomas, E. , Snoswell, C. L. , Haydon, H. , Mehrotra, A. , Clemensen, J. , & Caffery, L. J. (2020). Telehealth for global emergencies: Implications for coronavirus disease 2019 (COVID‐19). Journal of Telemedicine and Telecare, 26(5), 309–313. 10.1177/1357633X20916567 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spanemberg, J. C. , Simões, C. C. , & Cardoso, J. A. (2020). The impacts of the COVID‐19 pandemic on the teaching of dentistry in Brazil. Journal of Dental Education, 84(11), 1185–1187. 10.1002/jdd.12364 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Srinivasan, M. , Meyer, S. , Mombelli, A. , & Müller, F. (2017). Dental implants in the elderly population: A systematic review and meta‐analysis. Clinical Oral Implants Research, 28(8), 920–930. 10.1111/clr.12898 [DOI] [PubMed] [Google Scholar]
- Tiwari, T. , Jamieson, L. , Broughton, J. , Lawrence, H. P. , Batliner, T. S. , Arantes, R. , & Albino, J. (2018). Reducing indigenous oral health inequalities: A review from 5 nations. Journal of Dental Research, 97(8), 869–877. 10.1177/0022034518763605 [DOI] [PubMed] [Google Scholar]
- Tong, A. , Sainsbury, P. , & Craig, J. (2007). Consolidated criteria for reporting qualitative research (COREQ): A 32‐item checklist for interviews and focus groups. International Journal for Quality in Health Care, 19(6), 349–357. 10.1093/intqhc/mzm042 [DOI] [PubMed] [Google Scholar]
- Umer, F. , Haji, Z. , & Zafar, K. (2020). Role of respirators in controlling the spread of novel coronavirus (COVID‐19) amongst dental healthcare providers: A review. International Endodontic Journal, 53(8), 1062–1067. 10.1111/iej.13313 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woudenberg, F. (1991). An evaluation of Delphi. Technological Forecasting and Social Change, 40(2), 131–150. 10.1016/0040-1625(91)90002-W [DOI] [Google Scholar]
- Yoon, J. G. , Yoon, J. , Song, J. Y. , Yoon, S.‐Y. , Lim, C. S. , Seong, H. , Noh, J. Y. , Cheong, H. J. , & Kim, W. J. (2020). Clinical significance of a high SARS‐CoV‐2 viral load in the Saliva. Journal of Korean Medical Science, 35(20), e195. 10.3346/JKMS.2020.35.E195 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Material


