Abstract
Objective: To compare the therapeutic effects of compound betamethasone injection (CBI) combined with musculoskeletal ultrasonography (MSUS) and radial shock wave therapy (RSWT) in the treatment of tenosynovitis of the long head of the biceps brachii tendon (TLHBBT). Methods: A total of 93 patients with TLHBBT admitted to our hospital were selected and randomly divided into an observation group (n=48) and a control group (n=45). The control group received RSWT, while the observation group received CBI combined with MSUS. The therapeutic effects were compared between the two groups. Results: The visual analog scale scores for the affected sites in the observation group were lower than those in the control group immediately after treatment and at 1, 2 and 4 weeks after treatment, while the constant-Murley scale scores for the active range of motion for shoulder forward flexion and shoulder joint function in the observation group were higher than those in the control group (P < 0.05). After treatment, the positive rate in Yergason’s test in the observation group (2.08%) was lower than that in the control group (15.56%), while the negative rate in the observation group (97.92%) was higher than that in the control group (84.44%) (P < 0.05). The overall response rate (ORR) in the observation group (93.75%) was higher than that in the control group (80.00%) (P < 0.05). Conclusion: CBI combined with MSUS, is superior to RSWT in treating TLHBBT, and it can remarkably reduce pain, increase joint range of motion, and improve joint function.
Keywords: Tenosynovitis of long head of biceps brachii, musculoskeletal ultrasonography, compound betamethasone injection, radial shock wave, treatment
Introduction
The shoulder joint has the largest range of motion (ROM) out of all the joints in the human body, but its stability is low. Therefore, restricted motion and shoulder pain often occur in the shoulder joint [1]. Related statistics suggest that shoulder pain is the third largest pain condition regarding the motor system besides back pain and knee pain, with an incidence of about 20% [2]. The soft tissue injury of the shoulder is the main cause leading to shoulder motion and pain. The long head of the biceps brachii tendon (LHBBT) is the most easily damaged tissue, and is easily involved in other shoulder joint diseases, resulting in tenosynovitis of the long head of the biceps brachii tendon (TLHBBT) [3,4].
Strain, trauma, and cold primarily contribute to TLHBBT. Clinical diagnosis is conducted based on the medical history, the observation of symptoms and signs, and the related examination results [5]. In the treatment of TLHBBT, the conservative options include adequate rest, physical factors, acupuncture, or local block therapy [6,7]. However, such options have varying effects, and there is no unified conclusion on the most effective option [8,9]. However, if traditional surgical treatment is adopted, there will be marked trauma, a high risk of postoperative recurrence, and considerably increased medical cost [10]. With the advances in medical technologies, there are a growing number of options to treat such diseases. Extracorporeal shock wave therapy is a new option to treat muscular and skeletal diseases that has recently emerged in medical care. The shock-induced stress, cavitation, piezoelectric effect and metabolic activation expedite the microcirculation of the local damaged tissue, enhances the elastic formation of cells, and changes the permeability of local cell membranes. Finally, the body’s self-repair system is activated, and the improvement in inflammation is accelerated, thereby achieving good therapeutic effects [11]. However, extracorporeal shock wave therapy has to be conducted many times for the treatment of TLHBBT, increasing the medical expenses. Additionally, the therapy is no marked effect on improving the joint function of patients [12].
Ultrasound therapy is a new treatment method. Under the ultrasound guidance, drug injection, intubation and aspiration are carried out to avoid surgical operations, but the effects are similar to those with surgical treatment, remarkably reducing the pain and therapeutic costs [13]. Ultrasound therapy has been widely used in the treatment of a variety of medical and surgical diseases, but there are few studies on the differences in the therapeutic effects between ultrasound therapy and extracorporeal shock wave therapy [14,15]. In this study, a total of 93 patients were selected as the research subjects to compare ultrasound therapy and extracorporeal shock wave therapy, thereby providing a reliable reference for the selection of treatment options for patients with TLHBBT.
Materials and methods
Data
A total of 93 patients with TLHBBT admitted to Hainan West Central Hospital were divided into an observation group (n=48) and a control group (n=45) in accordance with a random number table. The patients were aged 34-68 years and the course of disease was 19-53 d. Inclusion criteria: patients diagnosed with TLHBBT by relevant examinations; unilateral lesion; the tendon sheath of the LHBBT was not completely torn; those not receiving any other non-surgical treatment with in the past 3 months; patients who voluntarily signed an informed consent form; this study was approval by the ethical review of the hospital. Exclusion criteria: patients complicated with severe osteoporosis; those who were allergic to steroids; those who received local shoulder injections within the past 1 month; those complicated with severe diabetes or hypertension; shoulder pain induced by other causes.
Methods
Control group: the pneumatic ballistic extracorporeal shock wave instrument of our hospital, and the standard therapeutic gun head (15 mm) were used. During the treatment, the patients were in a sitting position, and the dose was controlled at 2000 points and 1.5-2 Bar. The treatment was performed once every week, with continuous treatment of 5 applications as a course of treatment.
Observation group: injection drugs were prepared beforehand: 2 ml of water for injection + 0.5 ml of compound betamethasone injection (CBI) + 0.5 ml of 2% lignocaine injection. During the treatment, the patients were placed in a supine position. The affected shoulder joint was completely exposed and all the related muscles in the affected shoulder joint were explored using the ultrasonic probe applied with the couplant, so as to ensure there was no injury in any other parts. Then, the specific site and scope of the injuries of the LHBBT were investigated. During the treatment, the upper limb of the affected side was kept with the palm facing upwards and close to the body side, the forearm was kept bent at 90° after rotation, and the site to be operated was positioned. During positioning, the short axis was probed and the probe was kept perpendicular to the LHBBT to determine whether there was effusion near the tendon. Once the injured site was identified, the probe was rotated at a right angle, and kept parallel to the long axis of the biceps brachii. The patients were instructed to conduct active elbow flexion and extension to determine whether the tendon was partially torn or completely broken. After the accurate positioning, the drugs were injected using ultrasound intervention. Drug injection was conducted using a long-axis needle insertion technique. After complete disinfection and cleaning, the physician selected a specific puncture needle and syringe (5 ml), and inserted the needle from the positioning point into the tendon sheath. For patients with tendon sheath effusion, the effusion was drained first, and then 3 ml of the prepared medicine was accurately injected into the tendon sheath of the long head of the biceps brachii (TSLHBB) after no blood was determined. Immediately after the injection, the needle was withdrawn, and sterile dressing was applied at the injection point. The site was kept dry within 24 h after injection. Patients with discomfort after injection were treated with local cold therapy, and the dressing for patients without discomfort was removed after 24 h. Full treatment was one course of treatment.
Observational indices
General data: age, gender, body mass index (BMI), affected side and course of disease were statistically compared between the two groups.
Degree of pain: visual analog scale (VAS) [16] was selected to assess the pain degree of the affected site. A sliding scale with a length of 10 cm was prepared, with one end marked as 0 indicating painless and the other end marked as 10 indicating severe pain. The patients were instructed to select the corresponding number based on his/her feelings of pain. A greater number indicated a higher degree of pain. Two assessments were conducted within 10 min, and the average was taken as the final result, so as to ensure that the result accurately reflected the degree of pain of the patients. The assessments were performed before treatment, immediately after treatment, and at 1, 2 and 4 weeks after treatment.
The ROM for shoulder joint forward flexion: the patients were in a sitting position, and the arm on the affected side was kept in a normal anatomical position on the body side or even the elbow joint. The protractor center was opposite to the shoulder peak, the fixed arm was kept parallel to the midaxillary line, and the movable arm was kept parallel to the humerus. The patients were instructed to conduct active shoulder forward flexion, and the measured angles were recorded. In order to ensure the accuracy of the results, each patient was measured twice, and the average was taken as the final result. The measurements were conducted before treatment, immediately after treatment, and at 1, 2 and 4 weeks after treatment.
Yergason’s test: the speed test [17] was conducted. The patients were instructed to straighten their elbow joints and rotate their forearms backwards. The physician directed the patients to flex the shoulder forward with increased resistance. “Positive” was recorded for patients with pain, while “Negative” was recorded for patients without pain. The experiments were conducted at 1 and 2 weeks after treatment, respectively.
Shoulder joint function: the assessments were conducted using the constant-Murley scale (CMS) [18], including pain (15 points), daily living ability (20 points), ROM (40 points) and myodynamia (25 points). A higher score indicated a better shoulder joint function.
Efficacy criteria: cured: after treatment, the pain of the patient disappeared without any discomfort, and the shoulder joint activity became normal. Improved: after treatment, the patient had only slight pain and discomfort, and the shoulder joint activity recovered more than 50%. No response: after treatment, the pain and discomfort were still obvious, and the ROM for shoulder joint recovered less than 50%. Overall response rate (ORR) = Cured rate + Improved rate.
Statistical method
SPSS 23.0 was adopted for statistical analysis. The measurement data were expressed by x̅ ± sd, and detected by t test. The enumeration data were expressed by [n (%)] and detected by chi-squared. Multi-point comparison was analyzed by analysis of variance (ANVOA) and detected by F. Graphpad Prism 8 was used to illustratethe graphs. P < 0.05 indicated a statistically significant difference.
Results
General data
There was no statistical difference in the male-to-female ratio, the ratio of left to right affected side, mean age, BMI and average course of disease between the two groups (P > 0.05) (Table 1 and Figure 1).
Table 1.
Comparison of general data between the two groups (x̅ ± s)/[n (%)]
| Data | Observation group (n=48) | Control group (n=45) | t/X2 | P | |
|---|---|---|---|---|---|
| Gender | M | 28 (58.33) | 26 (57.78) | 0.003 | 0.957 |
| F | 20 (41.67) | 19 (42.22) | |||
| Age (years) | 50.13±10.62 | 51.27±11.48 | 0.497 | 0.620 | |
| BMI (kg/m2) | 22.46±1.17 | 23.31±1.24 | 3.401 | 0.001 | |
| Course of disease (d) | 34.16±5.19 | 35.51±5.46 | 1.222 | 0.225 | |
| Affected side | Left | 22 (45.83) | 24 (53.33) | 0.523 | 0.470 |
| Right | 26 (54.17) | 21 (46.67) | |||
Figure 1.
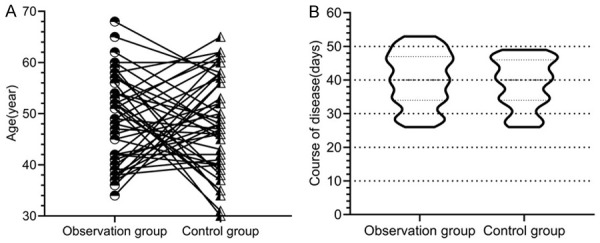
Age and course of disease. There was no significant difference in age and course of disease between the two groups (P > 0.05).
Degree of pain
There was no statistically significant difference in VAS scores between the two groups before treatment (P > 0.05). Immediately after treatment and at 1, 2 and 4 weeks after treatment, the VAS scores for affected sites decreased gradually in the two groups, there were statistically significant differences in the comparison within groups in different time periods, and the VAS scores for the affected sites in the observation group were lower than those in the control group (P < 0.05) (Figure 2).
Figure 2.
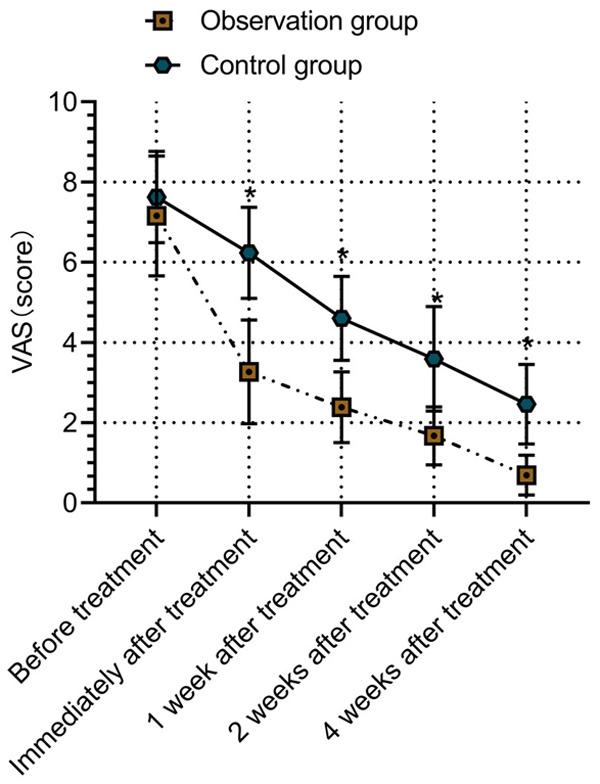
Degree of pain. There was no marked difference in the comparison of VAS scores between the two groups before treatment (P > 0.05). Immediately after treatment and at 1, 2 and 4 weeks after treatment, the degree of pain in the observation group was lower than that in the control group (P < 0.05). * indicates the comparison between the two groups (P < 0.05).
ROM for forward flexion of the shoulder joint
There was no statistically significant difference in the ROM for shoulder joint forward flexion between the two groups before treatment (P > 0.05). Immediately after treatment and at 1, 2 and 4 weeks after treatment, the ROM for active forward flexion of the shoulder joint was increased gradually in both groups, and the differences in the comparison within groups were statistically significant in different time periods, and the ROM for active forward flexion of shoulder joint in the observation group was higher than that in the control group (P < 0.05) (Figure 3).
Figure 3.
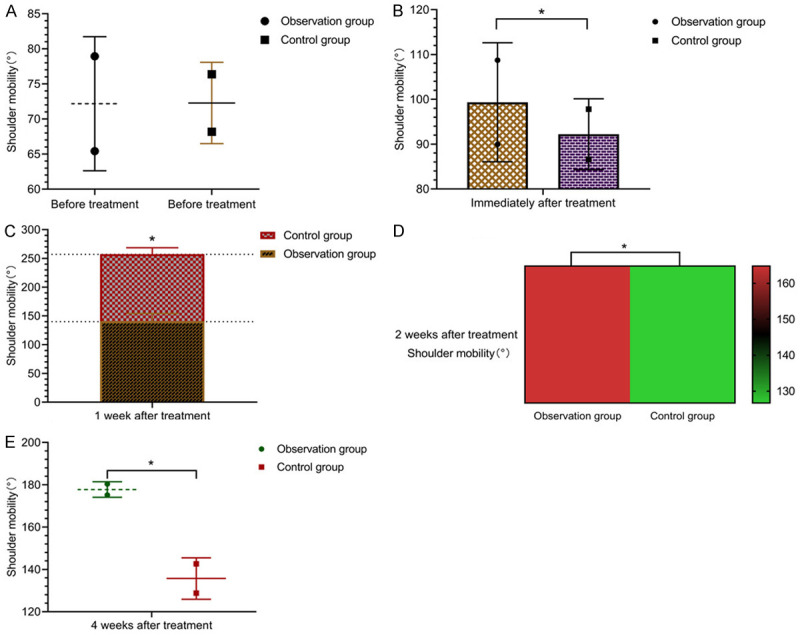
ROM of shoulder forward flexion. There was no remarkable difference in the ROM of shoulder forward flexion between the two groups (A) (P > 0.05). Immediately after treatment (B) and at 1 (C), 2 (D) and 4 (E) weeks after treatment, the ROM of shoulder forward flexion in the observation group was higher than that in the control group (P < 0.05). * indicates the comparison between the two groups (P < 0.05).
Yergason’s test
There was no statistically significant difference in the positive rate (93.75% vs. 95.56%) and negative rate (6.25% vs. 4.44%) in Yergason’s test between the observation group and the control group before treatment (P > 0.05). After treatment, the positive rates in Yergason’s test were decreased, while the negative rates were increased in both groups. After treatment, the positive rate in Yergason’s test in the observation group (2.08%) was lower than that in the control group (15.56%), while the negative rate in the observation group (97.92%) was higher than that in the control group (84.44%) (P < 0.05) (Table 2).
Table 2.
Comparison of results of Yergason’s test between the two groups before and after treatment [n (%)]
| Group | Positive | Negative | ||
|---|---|---|---|---|
|
|
|
|||
| Before treatment | After treatment | Before treatment | After treatment | |
| Observation group (n=48) | 45 (93.75) | 1 (2.08) | 3 (6.25) | 47 (97.92) |
| Control group (n=45) | 43 (95.56) | 7 (15.56) | 2 (4.44) | 38 (84.44) |
| X2 | 0.149 | 5.362 | 0.149 | 5.362 |
| P | 0.700 | 0.021 | 0.700 | 0.021 |
Shoulder joint function
There was no statistically significant difference in the CMS scores for shoulder joint function between the two groups before treatment (P > 0.05). Immediately after treatment and at 1, 2 and 4 weeks after treatment, the CMS scores for shoulder joint function were increased gradually in both groups, and the differences in the comparison within groups were statistically significant in different time periods, and the CMS scores for shoulder joint function in the observation group was higher than that in the control group (P < 0.05) (Figure 4).
Figure 4.
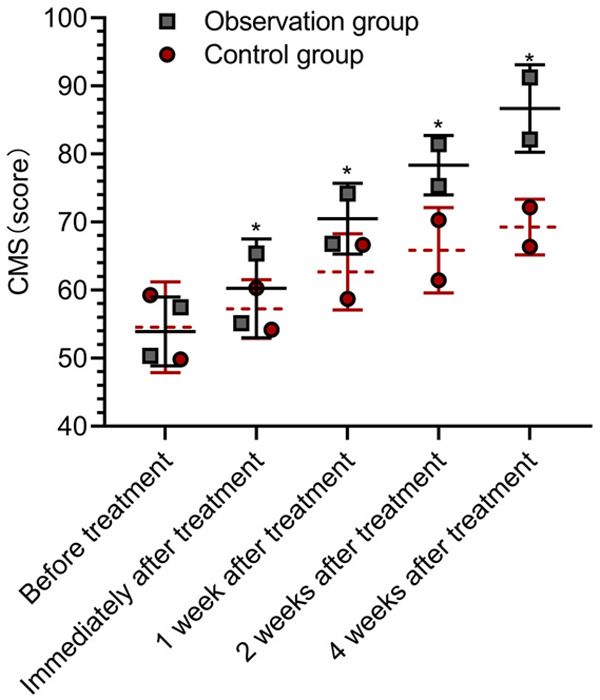
Shoulder joint function. There was no marked difference in CMS scores between the two groups before treatment (P >0.05). Immediately after treatment and at 1, 2 and 4 weeks after treatment, CMS scores in the observation group were higher than those in the control group (P < 0.05). * indicates the comparison between the two groups (P < 0.05).
Overall response rate
In the observation group, 45 patients were treated with drug injection combined with ultrasound intervention and they showed moderate response, while only 3 patients revealed no response, with the ORR of 93.75%. In the control group, 36 patients receiving radial shock wave therapy (RSWT) revealed a moderate response, while 9 patients showed no response, with the ORR of 80.00%. The differences in ORR between the two groups were statistically significant (P < 0.05) (Table 3).
Table 3.
Comparison of ORRs between the two groups [n (%)]
| Group | Cured | Improved | No response | ORR |
|---|---|---|---|---|
| Observation group (n=48) | 20 (41.67) | 25 (52.08) | 3 (6.25) | 45 (93.75) |
| Control group (n=45) | 15 (33.33) | 21 (46.67) | 9 (20.00) | 36 (80.00) |
| X2 | 3.907 | |||
| P | 0.048 |
Discussion
The improvement of living standards leads to an increased attention on chronic diseases affecting the quality of life, such as rotator cuff injury and omarthritis. However, TLHBBT is often ignored or merely seen as an accompanying symptom [19]. The LHBBT is the only tendon with a tendon sheath in the shoulder joint. There is a segment in the joint cavity, which plays a pivotal role in maintaining the function and stability of the shoulder joint [20]. TLHBBT is highly prevalent in middle-aged and young adults. A study suggested that the tear of LHBBT and supraspinatus tendon in the rotator cuff was markedly correlated, exhibiting that LHBBT is the most likely to be torn and degenerated in shoulder joint [21].
There are multiple clinical options for the treatment TLHBBT. RSWT, a new option, is easy to operate and non-invasive. Therefore, RSWT has been widely recognized by patients and physicians [22]. However, there is a higher risk of recurrence after treatment with RSWT, and RSWT has no satisfactory effects on improving joint function. As a new option based on the medical technologies, ultrasound intervention has been widely used in the treatment of shoulder soft tissue injury in countries beyond China, especially in developed countries. There are numerous studies regarding ultrasound intervention in China. However, the follow-up studies need to be conducted to determine the exact efficacy [23,24]. In this study, the comparison of the therapeutic effects of musculoskeletal ultrasonography (MSUS) combined with drug injection and RSWT exhibited that the degree of pain in the observation group receiving MSUS combined with drug injection was lower than that in the control group, while the ROM for shoulder joint forward flexion was higher, and the shoulder joint function was better in the observation group immediately after treatment and at 1, 2 and 4 weeks after treatment. This suggests that MSUS combined with drug injection is superior to RSWT in reducing the pain of patients and improving the ROM for the shoulder joint and shoulder joint function. MSUS combined with drug injection exhibited a satisfactory efficacy in the treatment of omarthritis, shoulder-hand syndrome, prosopospasm, peripheral nerve injury, knee osteoarthritis, soft tissue injury around the shoulder joint, ankle joint injury and rotator cuff injury [25]. After treatment, the positive rate in Yergason’s test in the observation group was lower than that in the control group, while the ORR in the observation group was higher than that in the control group. This suggests that MSUS combined with drug injection has a more prominent effect on pain control and can achieve a higher ORR. A comparative study showed that the ultrasound group had negative Yergason’s tests at week 1 and 2 weeks after treatment, while the SWT group merely turned negative at 5 weeks after treatment. This reveals that ultrasound intervention is more effective [26]. The aforementioned results prove that drug injection combined with ultrasound intervention exhibits a more satisfactory efficacy. This may be attributed to the fact that ultrasound intervention can inhibit inflammation formation more quickly and effectively, thus reducing the risk of recurrence. CBI has the characteristics of slight solubility, and its effect can last for 2-3 weeks for each injection. MSUS can help direct injection of drugs into the TSLHBB, which can significantly relieve the shoulder pain quickly and rapidly improve the AROM of the shoulder. By comparison, SWT takes a longer time to produce effects and requires multiple sessions to achieve the same effect as that by ultrasound intervention [27]. The comparison shows that drug injection combined with ultrasound intervention through TSLHBB at the acute phase can quickly alleviate the restricted active motion of the shoulder and greatly reduce the pain of patients with shoulder pain. For the patients not suitable for ultrasound intervention, RSWT can be used to repair the damaged tendon, alleviate the symptoms, and relieve the pain [28].
In summary, CBI combined with MSUS, which is superior to RSWT in treating TLHBBT, can remarkably reduce pain, increase the joint ROM, and improve joint function. However, due to the short follow-up time in this study, only the short-term efficacy was assessed, and the long-term recurrence and efficacy have not been measured. Therefore, the longterm efficacy of drug injection combined with MSUS cannot be confirmed. In addition, the degrees of severity for patients with TLHBBT are not differentiated, and the differences in the efficacy of drug injection combined with ultrasound intervention on patients with varying degrees of severity have not been confirmed. The aforementioned shortcomings will be improved in the future studies, so as to prove the application value of drug injection combined with MSUS.
Acknowledgements
This research received no specific funding from any agency in the public, commercial, or not-for-profit sectors.
Disclosure of conflict of interest
None.
References
- 1.Pfeiffer M, Eibl P, Schuh A. Clinical examination of the shoulder joint - part 2. MMW Fortschr Med. 2019;161:57–61. doi: 10.1007/s15006-019-0187-3. [DOI] [PubMed] [Google Scholar]
- 2.Wilson RD, Chae J. Hemiplegic shoulder pain. Phys Med Rehabil Clin N Am. 2015;26:641–655. doi: 10.1016/j.pmr.2015.06.007. [DOI] [PubMed] [Google Scholar]
- 3.De la Rosa-Morillo F, Galloza-Otero JC, Micheo W. Shoulder pain rehabilitation in young athletes. Rehabilitacion (Madr) 2019;53:85–92. doi: 10.1016/j.rh.2018.10.005. [DOI] [PubMed] [Google Scholar]
- 4.Saito H, Harrold ME, Cavalheri V, McKenna L. Scapular focused interventions to improve shoulder pain and function in adults with subacromial pain: a systematic review and meta-analysis. Physiother Theory Pract. 2018;34:653–670. doi: 10.1080/09593985.2018.1423656. [DOI] [PubMed] [Google Scholar]
- 5.Geannette C, Williams D, Berkowitz J, Miller TT. Ultrasound-guided biceps tendon sheath injection: spectrum of preprocedure appearances. J Ultrasound Med. 2019;38:3267–3271. doi: 10.1002/jum.15062. [DOI] [PubMed] [Google Scholar]
- 6.Wilk KE, Hooks TR. The painful long head of the Biceps Brachii: nonoperative treatment approaches. Clin Sports Med. 2016;35:75–92. doi: 10.1016/j.csm.2015.08.012. [DOI] [PubMed] [Google Scholar]
- 7.Nho SJ, Strauss EJ, Lenart BA, Provencher MT, Mazzocca AD, Verma NN, Romeo AA. Long head of the biceps tendinopathy: diagnosis and management. J Am Acad Orthop Surg. 2010;18:645–656. doi: 10.5435/00124635-201011000-00002. [DOI] [PubMed] [Google Scholar]
- 8.Xue XH, Feng ZH, Li ZX, Pan XY. Calcifying tendinitis of the long head of the biceps brachii and superior labrum: a report of one case and literature review. J Sports Med Phys Fitness. 2018;58:1090–1095. doi: 10.23736/S0022-4707.17.07080-3. [DOI] [PubMed] [Google Scholar]
- 9.Ciccotti MG. Editorial commentary: the long head of the biceps brachii tendon-the shoulder surgeon’s conundrum. Arthroscopy. 2017;33:1937–1939. doi: 10.1016/j.arthro.2017.07.009. [DOI] [PubMed] [Google Scholar]
- 10.Duff SJ, Campbell PT. Patient acceptance of long head of biceps brachii tenotomy. J Shoulder Elbow Surg. 2012;21:61–65. doi: 10.1016/j.jse.2011.01.014. [DOI] [PubMed] [Google Scholar]
- 11.Yildirim P, Gultekin A, Yildirim A, Karahan AY, Tok F. Extracorporeal shock wave therapy versus corticosteroid injection in the treatment of trigger finger: a randomized controlled study. J Hand Surg Eur Vol. 2016;41:977–983. doi: 10.1177/1753193415622733. [DOI] [PubMed] [Google Scholar]
- 12.Liu S, Zhai L, Shi Z, Jing R, Zhao B, Xing G. Radial extracorporeal pressure pulse therapy for the primary long bicipital tenosynovitis a prospective randomized controlled study. Ultrasound Med Biol. 2012;38:727–735. doi: 10.1016/j.ultrasmedbio.2012.01.024. [DOI] [PubMed] [Google Scholar]
- 13.Naredo E, D’Agostino MA, Wakefield RJ, Möller I, Balint PV, Filippucci E, Iagnocco A, Karim Z, Terslev L, Bong DA, Garrido J, Martínez-Hernández D, Bruyn GA. Reliability of a consensus-based ultrasound score for tenosynovitis in rheumatoid arthritis. Ann Rheum Dis. 2013;72:1328–1334. doi: 10.1136/annrheumdis-2012-202092. [DOI] [PubMed] [Google Scholar]
- 14.McKenna RT, Dove JC, Ratzlaff RA, Diaz-Gomez JL, Cox DJ, Simon LV. A 3-dimensional printed ultrasound probe visuospatial trainer. Ultrasound Q. 2018;34:103–105. doi: 10.1097/RUQ.0000000000000318. [DOI] [PubMed] [Google Scholar]
- 15.Tarique U, Tang B, Singh M, Kulasegaram KM, Ailon J. Ultrasound curricula in undergraduate medical education: a scoping review. J Ultrasound Med. 2018;37:69–82. doi: 10.1002/jum.14333. [DOI] [PubMed] [Google Scholar]
- 16.Faiz KW. [VAS--visual analog scale] . Tidsskr Nor Laegeforen. 2014;134:323. doi: 10.4045/tidsskr.13.1145. [DOI] [PubMed] [Google Scholar]
- 17.Arrigoni P, Ragone V, D’Ambrosi R, Denard P, Randelli F, Banfi G, Cabitza P, Randelli P. Improving the accuracy of the preoperative diagnosis of long head of the biceps pathology: the biceps resisted flexion test. Joints. 2014;2:54–58. doi: 10.11138/jts/2014.2.2.054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Vrotsou K, Ávila M, Machón M, Mateo-Abad M, Pardo Y, Garin O, Zaror C, González N, Escobar A, Cuéllar R. Constant-Murley Score: systematic review and standardized evaluation in different shoulder pathologies. Qual Life Res. 2018;27:2217–2226. doi: 10.1007/s11136-018-1875-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gurnani N, van Deurzen DF, Janmaat VT, van den Bekerom MP. Tenotomy or tenodesis for pathology of the long head of the biceps brachii: a systematic review and meta-analysis. Knee Surg Sports Traumatol Arthrosc. 2016;24:3765–3771. doi: 10.1007/s00167-015-3640-6. [DOI] [PubMed] [Google Scholar]
- 20.Angelo RL. Surgical management of proximal long head biceps tendon disorders. Sports Med Arthrosc Rev. 2018;26:176–180. doi: 10.1097/JSA.0000000000000197. [DOI] [PubMed] [Google Scholar]
- 21.Longo UG, Loppini M, Marineo G, Khan WS, Maffulli N, Denaro V. Tendinopathy of the tendon of the long head of the biceps. Sports Med Arthrosc Rev. 2011;19:321–332. doi: 10.1097/JSA.0b013e3182393e23. [DOI] [PubMed] [Google Scholar]
- 22.Schnurrer-Luke-Vrbanić T, Avancini-Dobrović V, Sosa I, Cvijanovic O, Bobinac D. Effect of radial shock wave therapy on long bone fracture repair. J Biol Regul Homeost Agents. 2018;32:875–879. [PubMed] [Google Scholar]
- 23.Olszynski P, Anderson J, Trinder K, Domes T. Point-of-care ultrasound in undergraduate urology education: a prospective control-Intervention study. J Ultrasound Med. 2018;37:2209–2213. doi: 10.1002/jum.14571. [DOI] [PubMed] [Google Scholar]
- 24.Kumbhare D, Singh D, Rathbone HA, Gunn M, Grosman-Rimon L, Vadasz B, Clarke H, Peng PWH. Ultrasound-guided interventional procedures: myofascial trigger points with structured literature review. Reg Anesth Pain Med. 2017;42:407–412. doi: 10.1097/AAP.0000000000000572. [DOI] [PubMed] [Google Scholar]
- 25.Korbe S, Udoji EN, Ness TJ, Udoji MA. Ultrasound-guided interventional procedures for chronic pain management. Pain Manag. 2015;5:465–482. doi: 10.2217/pmt.15.46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wildeboer RR, Panfilova AP, Mischi M, Wijkstra H. Imaging modalities in Focal Therapy: Multiparametric Ultrasound. Arch Esp Urol. 2016;69:281–290. [PubMed] [Google Scholar]
- 27.Arirachakaran A, Boonard M, Yamaphai S, Prommahachai A, Kesprayura S, Kongtharvonskul J. Extracorporeal shock wave therapy, ultrasound-guided percutaneous lavage, corticosteroid injection and combined treatment for the treatment of rotator cuff calcific tendinopathy: a network meta-analysis of RCTs. Eur J Orthop Surg Traumatol. 2017;27:381–390. doi: 10.1007/s00590-016-1839-y. [DOI] [PubMed] [Google Scholar]
- 28.Njawaya MM, Moses B, Martens D, Orchard JJ, Driscoll T, Negrine J, Orchard JW. Ultrasound guidance does not improve the results of shock wave for plantar fasciitis or calcific achilles tendinopathy: a randomized control trial. Clin J Sport Med. 2018;28:21–27. doi: 10.1097/JSM.0000000000000430. [DOI] [PubMed] [Google Scholar]


