1.
1.
Lateral femoral cutaneous neuropathy is a focal neuropathy caused by compression of the lateral femoral cutaneous nerve (LFCN) at the level of anterior‐superior iliac spine or inguinal ligament. It is commonly associated with diabetes mellitus, obesity, and wearing tight clothing. 1 It can also be iatrogenic, caused by prone positioning during spine surgery or ventilation for acute respiratory distress syndrome (ARDS).2, 3 Prone positioning is frequently used to improve oxygenation in patients with ARDS due to coronavirus disease 2019 (COVID‐19). 4 Two patients were reported with symptoms of meralgia paresthetica developed after prone positioning to treat COVID‐19‐associated ARDS. 5 Here, we report another two patients with typical sensory symptoms, in whom the diagnosis of severe lateral femoral cutaneous neuropathy was confirmed by LFCN nerve conduction study (NCS) and skin biopsy.
2. PATIENT 1
A 46‐y‐old man developed severe COVID‐19. He was intubated and spent 2 wk in the intensive care unit, during which intermittent prone positioning was done. When weaned off sedation, he noticed severe numbness in the left anterolateral thigh. He presented 4 mo later for persistent numbness. On examination, body mass index (BMI) was 33.7 kg/m2. Pinprick sensation was severely reduced over the left anterolateral thigh. There was no weakness or spine tenderness. Reflexes were normal at the knees but reduced at the ankles. HbA1C, ANA, B12, TSH, free T4, and serum immunofixation were all normal. NCS showed absent left but normal right LFCN response (Figure 1). Bilateral sural, superficial peroneal, and saphenous sensory studies, and bilateral peroneal and tibial motor studies were normal. Needle electromyography (EMG) of lower extremity and lumbosacral paraspinal muscles showed no abnormal spontaneous activity but some large‐amplitude and long‐duration motor unit potentials with mildly reduced recruitment in the bilateral L3‐S1 myotomes. Lumbosacral spine MRI showed multilevel degenerative changes with varying degrees of canal and foraminal narrowing, more pronounced at level L4‐5. Three‐mm punch skin biopsy showed absent intraepidermal nerve fibers (IENF) at the left proximal thigh, but normal IENF densities at the right proximal thigh and left distal leg (Figure 1). He was diagnosed with severe left lateral femoral cutaneous neuropathy induced by prone positioning.
FIGURE 1.
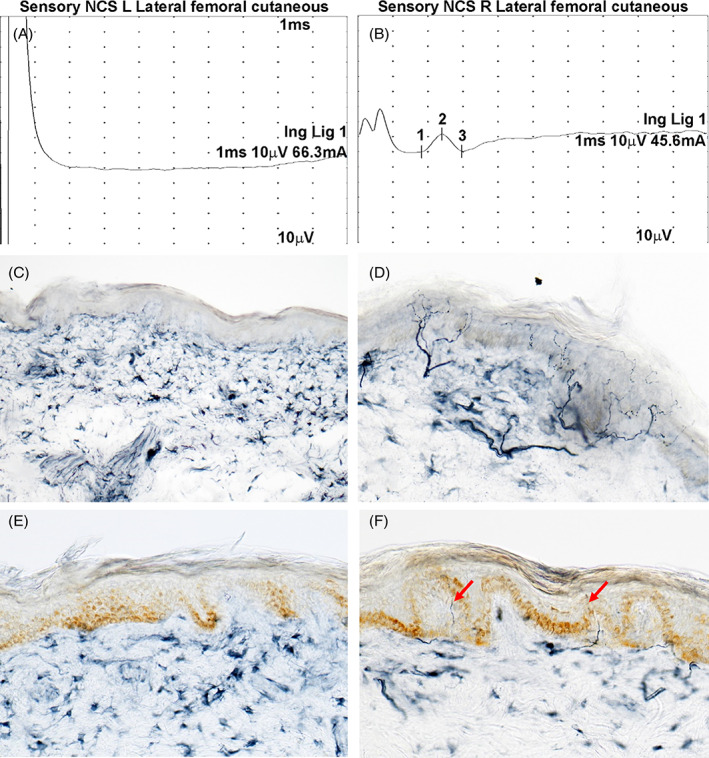
NCS and skin biopsy evaluation. NCS of Patient 1 shows that the lateral femoral cutaneous nerve response is absent on the left (A) but normal on the right with a sensory nerve action potential amplitude of 11.8 μV (B). Skin biopsy of Patient 1 shows absent intraepidermal nerve fibers at the left proximal thigh (C) but rich epidermal innervation at the right proximal thigh (14.0 fibers/mm; normal ≥ 8) (D). E, Skin biopsy of Patient 2 shows absent IENF at the left proximal thigh. F, The IENF density is severely reduced with a few fibers present at the right proximal thigh (3.3 fibers/mm; normal ≥ 8) (arrows) [Color figure can be viewed at wileyonlinelibrary.com]
3. PATIENT 2
A71‐year‐old man with a history of spine degenerative disease developed severe COVID‐19. He was intubated and in coma for 21 days, during which intermittent prone positioning was done. He noticed tingling and numbness in the anterolateral thighs bilaterally after he regained consciousness. He presented 3 mo later for bothersome paresthesias. Examination showed a mildly obese (BMI: 31.3 kg/m2) man with pinprick sensation reduced at the left > right anterolateral thighs. Strength and reflexes were normal except for the reduced ankle jerks. There was no spine tenderness. Blood tests did not reveal additional neuropathy risk factors. NCS showed absent bilateral LFCN responses but normal bilateral sural, superficial peroneal, and saphenous sensory responses as well as bilateral peroneal and tibial motor responses. Needle EMG showed a few fibrillation potentials in the right rectus femoris muscle, and some large‐amplitude and long‐duration motor unit potentials with mildly reduced recruitment in the L2‐S1 myotomes bilaterally. To date, the patient has declined a lumbosacral spine MRI. Skin biopsy showed absent IENFs at the left proximal thigh, reduced IENF density at the right proximal thigh, but normal IEFN density at the left distal leg (Figure 1). He was diagnosed with severe, left > right, lateral femoral cutaneous neuropathy induced by prone positioning.
As COVID‐19 cases continue to increase, we may see an increasing number of patients with lateral femoral cutaneous neuropathy caused by prone positioning to treat ARDS. However, the neuropathy may be preventable by using egg‐crate style foam padding between hip and bed to achieve more evenly distributed pressure over the hip to avoid LFCN compression. 5 It is important to take preventive measures, as the neuropathy can be severe, disturbing, and protracted as seen in our patients. Skin biopsy is useful to confirm lateral femoral cutaneous neuropathy, 1 as LFCN conduction response can be difficult to obtain in obese or older patients. 6 The mild chronic polyradiculopathy in our patients was most likely caused by spine degenerative disease, given the history and lumbosacral spine MRI findings. There was no history to suggest inflammatory polyradiculoneuropathy, which can be a neurological complication of COVID‐19. 7
CONFLICT OF INTEREST
None of the authors has any conflict of interest to disclose.
ETHICAL PUBLICATION STATEMENT
We confirm that we have read the Journal's position on issues involved in ethical publication and affirm that this report is consistent with those guidelines.
Zhou L, Siao P. Lateral femoral cutaneous neuropathy caused by prone positioning to treat COVID‐19‐associated acute respiratory distress syndrome. Muscle & Nerve. 2021;63:E50–E52. 10.1002/mus.27202
Abbreviations: ARDS, acute respiratory distress syndrome; BMI, body mass index; COVID‐19, coronavirus disease 2019; EMG, electromyography; IENF, intraepidermal nerve fiber; LFCN, lateral femoral cutaneous nerve; NCS, nerve conduction study.
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.
REFERENCES
- 1. Wongmek A, Shin S, Zhou L. Skin biopsy in assessing meralgia paresthetica. Muscle Nerve. 2016;53:641‐643. [DOI] [PubMed] [Google Scholar]
- 2. Cho KT, Lee HJ. Prone position‐related meralgia paresthetica after lumbar spinal surgery: a case report and review of the literature. J Korean Neurosurg Soc. 2008;44:392‐395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Juhl CS, Ballegaard M, Bestle MH, Tfelt‐Hansen P. Meralgia Paresthetica after prone positioning ventilation in the intensive care unit. Case Rep Crit Care. 2016;2016:7263201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Mittermaier M, Pickerodt P, Kurth F, et al. Evaluation of PEEP and prone positioning in early COVID‐19 ARDS. EClinicalMedicine. 2020;28:100579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Bellinghausen AL, LaBuzetta JN, Chu F, Novelli F, Rodelo AR, Owens RL. Lessons from an ICU recovery clinic: two cases of meralgia paresthetica after prone positioning to treat COVID‐19‐associated ARDS and modification of unit practices. Crit Care. 2020;24:580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Boon AJ, Bailey PW, Smith J, Sorenson EJ, Harper CM, Hurdle MF. Utility of ultrasound‐guided surface electrode placement in lateral femoral cutaneous nerve conduction studies. Muscle Nerve. 2011;44:525‐530. [DOI] [PubMed] [Google Scholar]
- 7. Caress JB, Castoro RJ, Simmons Z, et al. COVID‐19‐associated Guillain‐Barre syndrome: the early pandemic experience. Muscle Nerve. 2020;62:485‐491. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.


