Abstract
The aim of current study was to investigate risk perception of COVID‐19 pandemic, sleep quality and time change of leisure activity and their correlations with posttraumatic stress disorder (PTSD) in healthcare workers (HCWs) from four designated hospitals in China. Medical staffs (n = 317) from three designated hospitals in Guangdong Province and one designated hospital in Guangxi Province were surveyed on their demographic information, sleep quality and time change of leisure activity, risk perception of pandemic and PTSD symptoms (by using PTSD checklist for DSM‐5 (PCL‐5)). Hierarchical regression and structural equation model (SEM) were used to examine the correlated factors of PTSD. The prevalence of high level of PTSD symptoms (PCL‐5 > =33, a probable diagnosis of PTSD) was 10.7%. Regression analysis found that risk perception (dread: β = 0.142, p < 0.01; familiarity: β = 0.203, p < 0.01), sleep quality (β = 0.250, p < 0.001), time change of leisure activity (β = −0.179, p < 0.01), were independently correlated with PTSD severity, which was further confirmed by SEM. Locations of COVID‐19‐related hazards were significant different in cognitive map of risk perception between groups with high and low levels of PTSD symptoms. Risk perception of COVID‐19 pandemic influenced PTSD symptoms in HCWs. Adequate time for leisure activity and good sleep quality protected some HCWs against PTSD symptoms under the influence of pandemic. More researches were warranted to understand the path from pre‐factors of risk perception to its psychological consequences among HCWs.
Keywords: COVID‐19, healthcare workers, posttraumatic stress disorder, risk perception
Key Practitioner Message.
Risk perception of pandemic in HCWs from designated hospitals was positively correlated with PTSD symptom score after controlling other related variables.
Locations of COVID‐19‐related hazards were significant different in cognitive map of risk perception between groups with high and low levels of PTSD symptoms in HCWs from designated hospitals.
Good sleep quality and sufficient time for leisure activities were protective factors for PTSD symptoms in HCWs working at frontline hospitals.
1. INTRODUCTION
1.1. COVID‐19 pandemic
In the 21st century, the world is facing the challenge of new infectious diseases such as SARS, MERS, Ebola and avian influenza (Suwantarat & Apisarnthanarak, 2015). However, this trend has not come to end yet. A novel coronavirus, SAR‐COV‐2 as we know it, which caused pneumonia cases (on 11 February 2020), the WHO formally named the disease triggered by this virus as Corona Virus Disease 2019 (COVID‐19) has been discovered in December 2019, and rapidly emerged on lands around the globe in short time (Holshue et al., 2020; Remuzzi & Remuzzi, 2020). Fever was the most common symptom in patients with pneumonia caused by SARS‐CoV‐2, followed by cough (Lai, Shih, Ko, Tang, & Hsueh, 2020). According to the diagnosis and treatment of novel coronavirus pneumonia from National Health Committee (NHC), patients with severe symptoms and underlying disease would have life‐threatening situations (NHC, 2020). On 11 March, Tedros Adhamon Ghebreyesus, director‐general of the WHO, stated that COVID‐19 had become a global pandemic (Director‐General, 2020). This pandemic now has brought updating challenge to the whole world, reaching over 200 countries, areas or territories with 11 million confirmed cases and more than 204,967 deaths (WHO situation report updated to 9 July 2020). As of 7 July, there have been a 25% increase in cases and 18% increase in deaths reported from the African continent over the past week (WHO, 2020).
1.2. Mental health burden of frontline healthcare workers
Such widespread outbreaks are associated with adverse mental health consequences. Fear of falling sick or dying themselves, feelings of stigma and helplessness, worry about contacting the virus, closure of business were negative events that potentially put negative impact on individual mental health (Wang et al., 2020). Healthcare workers (HCWs), especially those who were working at frontline in designated hospitals for COVID‐19, have been facing kinds of enormous pressure, including a high risk of infection and inadequate protection from contamination, frustration, overwork, isolation, discrimination, negative emotions, worry about the shortage of protective equipment, feelings of incapability when facing critically ill patients, a lack of contact with their families, and exhaustion (Kang et al., 2020). It was also an alarming concern that the psychological intervention services for HCWs constantly encountered obstacles, as medical staff hesitated to participate in the group or individual psychology interventions provided to them. For example, a proportion of HCWs refused to commit they had psychological distress even they showed some signs of symptoms. And some stated that they did not want their families to worry (Chen et al., 2020). Accordingly, the mental health status of HCWs deserves more attention and investigation (McAlonan et al., 2007).
Posttraumatic stress disorder (PTSD) occurs in a subset of individuals exposed to traumatic events and consists of four clusters of symptoms: intrusive re‐experiencing of the trauma, avoidance of trauma‐related stimuli, negative alternation of cognition and mood, and excessive arousal or reactivity (Shalev, Liberzon, & Marmar, 2017). PTSD was seen as one of the major psychological impacts caused by previous massive outbreak of infectious disease in studies (Jung, Jung, Lee, & Kim, 2020; Lancee et al., 2008; Vyas, Delaney, Webb‐Murphy, & Johnston, 2016). During the ongoing COVID‐19 infections, Liu et al reported that the prevalence of posttraumatic stress symptoms in hardest‐hit area 1 month after outbreak was 7%, with women showing higher symptom severity (Liu et al., 2020). Another study investigated psychological impact of COVID‐19 pandemic (e.g., anxiety, depression and stress) during the initial stage of the COVID‐19 outbreak found that 8.1% of participants reported moderate to severe PTSD symptoms (Wang et al., 2020). Recently, published studies showed 3.8% of HCWs involved in the care for COVID‐19 patients in Singapore and India showed the prominent self‐reported PTSD symptoms (Chew et al., 2020), and general HCWs investigated online in China had prevalence rate of 2.2% (Yin et al., 2020). During the SARS outbreak, PTSD severity is significant different from those who worked at frontline and those who did not (Lin et al., 2007). The characteristics of PTSD in HCWs from designated hospital in China under influence of COVID‐19 needs further exploration.
1.3. Risk perception and PTSD
Risk perceptions reflect people's intuitive evaluations of various hazards that they are or might be exposed to, including multiple undesirable consequences that people associate with a specific cause. The elements that increase or mitigate fear and risk perceptions during pandemic included voluntariness, knowledge, visibility and trust (Cori, Bianchi, Cadum, & Anthonj, 2020). To evaluate different hazards, Slovic postulated two‐factor representations to outlines the feature of risk perception, namely ‘dread risk’ and ‘unknown risk’. The former one was defined at its high end by perceived lack of control, dread and catastrophic potential, while the latter one was defined at its high end by hazards judged to unobservable, unknown, new and delayed manifestation of harm (Slovic, 1987). It was also postulated that a combination of technical perception of hazard and outrage could provide psychometric insights of risk perception and public response (Fischhoff, 2015; Sandman, 1988). Shi et al confirmed that risk perception was a mediator between risk information and coping method and mental health of people after outbreak of an infectious disease. The cognitive map of risk perception on Slovic's two dimensions showed only one of six SAR‐related hazards was in maximum risk quadrant (Shi et al., 2003). Past experience has implicated the critical role of risk perception in unprecedented times of COVID‐19 pandemic (Cori et al., 2020).
Previous evidences supported the relation between risk perception and PTSD. Jalloh et al conducted a cross‐sectional survey to a national sample in areas of Ebola epidemic and found that perceived threat of Ebola disease was independently associated with PTSD (Jalloh et al., 2018). Another study has reported that perceptions of risks in SARS were significantly positively associated with PTSD symptom scores in HCWs after three years of outbreak (Wu et al., 2009). Studies of risk perception under COVID‐19 pandemic has explored the relationship between pandemic‐related information (e.g., risk communication and COVID‐19 related knowledge) and preventive behaviours (Abrams & Greenhawt, 2020; Taghrir, Borazjani, & Shiraly, 2020). However, there is still a lack of examination about the relation between PTSD and risk perception under the COVID‐19 pandemic within half year of outbreak by using psychometric cognitive model of risk perception. In addition, the distribution of COVID‐19‐related hazards on two‐dimension cognitive map of risk perception and its difference determined by PTSD severity were rarely explored.
1.4. Sleep quality, time for leisure activity and PTSD
Sleep and leisure activity were indispensable daily behaviours for regulating psychological stress. A systematic review and meta‐analysis has confirmed sleep quality was impaired in individuals with higher PTSD symptoms (Lewis et al., 2020). The studies conducted in COVID‐19 pandemic also have reported sleep quality was negatively correlated with PTSD symptoms in general HCWs and residents from hardest‐hit area (Liu et al., 2020; Yin et al., 2020). The significance of this correlation needs further examination in HCWs from designated hospital. The studies of leisure activity and mental health mainly focused on the domain of physical activity (White et al., 2017). However, the content of leisure activity could also include hobbies, relaxation and social intercourse with others (Hakansson, Axmon, & Eek, 2016). The 2014 Time Use Survey (2014TUS) conducted by Statistics Korea (KOSTAT) classified leisure activity into outdoor activities, indoor activities, internet use and other activities (Cha, 2018). There are individual differences on the leisure activities and the time for such activities could a reliable measure for the involvement for the leisure activities. Previous studies found more time for leisure activity was benefit for both physical and psychological health status (Cha, 2018; Hakansson, Axmon, & Eek, 2016; Holstila, Manty, Rahkonen, Lahelma, & Lahti, 2017; Mausbach et al., 2017). Under the impact of pandemic, the time for leisure activity was expected to be changed by increasing working load and frequent working shift in HCWs from designated hospitals. Whether this change is connected to PTSD was rarely explored.
1.5. The aim of the current study
On 9 July 2020, there were cumulative confirmed cases of 1647 and 254 in Guangdong province and Guangxi province in China, respectively (CDC, 2020). Based on the above literature review we conducted an investigation of risk perception, sleep quality, time change of leisure activity and PTSD in HCWs from four designated hospitals in those two provinces in China within 6 months of the pandemic. We hypothesize that (1) Risk perception of COVID‐19 is significantly correlated with PTSD symptom severity. (2) Distributions of COVID‐19‐related hazards were significantly different between groups of different PTSD symptom severity. (3) Sleep quality and time change of leisure activity are significantly correlated with PTSD symptom severity.
2. METHOD
2.1. Sample
The inclusion criteria were (a) having a medical profession and (b) working in a designated hospital during COVID‐19 outbreak. The exclusion criteria were (a) having severe disease (e.g., acute enteritis, upper respiratory tract infection with high fever and bone trauma); (b) on leave during COVID‐19 outbreak (>30d). From 4 to 18 June 2020, approximately 6 months after outbreak, questionnaires were sent to 481 qualified medical staffs in four designated hospitals by mobile phone, using online questionnaire platform Wenjuanxing (https://www.wjx.cn/). A total of 317 questionnaires were collected by the end of the survey, with the response rate of 65.9%. The process of sampling was presented in Figure 1. At recruitment demographic information was collected (including gender, age, nation, education level and working department). Oral or written informed consent was obtained from all participants prior to participation in this study. The study was approved by Ethics Committee of Southern Medical University.
FIGURE 1.
Sampling process
2.2. Data collection
The online questionnaire was designed by one of our authors (GSY) in advance, which could be accessed by a link generated by the Wenjuanxing. The link of online questionnaire was sent to the managers and administrative staffs in departments of those designated hospitals. They subsequently sent this link to the online groups of their departments so HCWs could finish the questionnaire by clicking into it by mobile phone or computer. After entering into the online survey, the questionnaire could only be submitted when all items were answered. The data were automatically stored in online system of Wenjuanxing, which could be downloaded after the survey was finished.
2.3. Measures
2.3.1. PTSD symptom severity
PTSD symptom severity was assessed by the PTSD checklist for DSM‐5 (PCL‐5). The PCL‐5 is self‐reported scale consisting of 20 items that correspond directly to the DSM‐5 (Blevins, Weathers, Davis, Witte, & Domino, 2015). Each item reflected the severity of a particular symptom, rated on a five‐point Likert scale from 0 (not at all) to 4 (extremely) during the previous month. The score of each symptom cluster was calculated as the sum of the corresponding items. The PTSD symptom severity was defined as the sum of the scores of all PCL‐5 symptom clusters. The sum of total score over cut‐point score of 33 point suggest a probable diagnosis of PTSD or significant symptom presentations. Based upon current psychometric work, the Chinese version of the original PCL‐5 has been validated and is widely used in trauma‐related research and practice (L. Wang et al., 2015). The Cronbach's alpha of PCL‐5 in the current study was 0.965, suggesting relatively high internal consistency.
2.3.2. Risk perception of COVID‐19 pandemic
According to the psychometric model of postulated by Slovic, dread and familiarity were adopted as the measurement of risk perception (Slovic, 1987). These two dimension each was rated on a five‐point Likert scale from 1 (not dreadful at all or very familiar) to 5 (extremely dreadful or not familiar at all) on a single hazard. We included following five items as hazards on the reference to previous studies: H1. Virus: SAR‐COV‐2; H2. Disease: COVID‐19; H3. COVID‐19 patient or virus carrier; H4. Treatment and prevention of COVID‐19; H5. Frontline HCWs who had contact with COVID‐19 patients. Thus there were total 10 items in section (2 dimension × 5 hazards). The reason for inclusion of H4 and H5 is that people who were exposed, infected and fall ill can be considered the potential hazard (Malecki, Keating, & Safdar, 2020). The item was rated retrospectively based on risk perception of the peak period (basically from January to March 2020) of pandemic. Factor analysis has confirmed that above items fit two‐factor model better than one factor model, which is in line with the Slovic's two‐dimension theory. Further, after exlusion of two items of H5 for having relatively low factor loading, the remaining eight items had an ideal model fit (adjusted two factor model) with good reliablity (Composite reliability were 0.927 and 0.953 for dread and familiarity, respectively) and validity (Average variance extracted were 0.763 and 0.835 dread and familiarity, respectively, with sigificant discriminant validity). Relevant analyses were presented in the appendices (See supplementary file).
2.3.3. Sleep quality
The sleep quality was assessed by one item extracted out of Pittsburg Sleep Quality Index (PSQI) as ‘How good is your sleep quality?’(Buysse, Reynolds, Monk, Berman, & Kupfer, 1989). The item is rated on a four point Likert scale ordered as ‘very good’, ‘good’, ‘bad’ and ‘very bad’. Single‐item sleep measures have been used in previous studies (Liu et al., 2020), with evidence that single‐item component of subjective sleep quality correlated highly with global sores of the full sleep questionnaire (e.g., a 11‐points single item with Medical Outcomes Study (MOS) Sleep scores and a 6‐points single time with Mary's Hospital Sleep Questionnaire) (Cappelleri et al., 2009; Pien, Sammel, Freeman, Lin, & DeBlasis, 2008).
2.3.4. Time change of leisure activity
Time change of leisure activity was measured with a study‐specific single item stated as ‘How was your time for leisure activity since the start of epidemic’. The item was rated on a five point Likert scale ordered as ‘no time’, ‘decreased’, ‘as usual’, ‘increased’ and ‘a lot’. This item was set on the reference of limited studies measuring the time for leisure activities (Hakansson et al., 2016). Specific criteria for time for leisure activity (such as >1 hr) was not used for consideration of individual difference on the demand of time for leisure activity. This item was mainly focusing on the time change caused by COVID‐19 pandemic.
2.4. Data analysis
Outliers were detected by box plot to find extreme outlying value. Spotted outliers were deleted and substituted by multiple imputation. Descriptive analyses were conducted to examine the characteristics of the sample. Bivariate analyses (t‐test and one‐way variance analysis (ANOVA)) were then carried out to analyse the PCL‐5 score among different demographic, sleep quality and time change of leisure activity, and identify the difference on risk perception among groups divided by PCL‐5 (cut‐off score of 33). Then the hierarchical regression analysis was applied to identify independent variables associated with PTSD severity. Lastly, to confirm the relations of risk perception, sleep quality, time change for leisure activity and PTSD, a structural equation model (SEM) was built. All statistical analyses were performed using the Statistical Package for Social Sciences (SPSS) version 18.0 and analysis of moment structures (AMOS) version 22.0.
3. RESULTS
3.1. The prevalence, demographic characteristics and difference of PCL‐5 score in different subgroups
A total of 317 participants recruited in this study, among which 38% (n = 121) were from emergency department, 29% (n = 91) were from respiratory department and 33% (n = 105) were from other departments (including hepatology unit (n = 54, 17%), digestive department (n = 25, 8%), department of cardiovascular medicine (n = 17, 5%), medical imaging department (n = 13, 3%)). About 70% (n = 222) of the sample were women and aged 35 or younger; 92% (n = 293) of the participants belong to the Han nationality. The proportion of doctor, nurse and other medical professions were 44% (n = 140), 45% (n = 144) and 11% (n = 33), respectively. Thirty‐six percent of participants (n = 201) had an education level of university and 37% (n = 116) had a higher degree. Using PCL‐5 cut‐off score of 33 as criterion, 34 people met the criterion of a probable PTSD diagnosis, with evaluated PTSD prevalence rate of 10.7%.
The comparison between groups of demographic information, sleep quality and time change of leisure activity was shown in Table 1. Younger respondents had significantly higher PTSD symptom severity than older ones [Mean (age ≤ 35) = 17.11 (95% CI: 15.31–18.92) vs. Mean (age > 35) = 11.61 (95% CI: 9.46–13.82); t = 3.47, p = 0.001]. Female respondents had statistically significant higher PCL‐5 scores than male respondents [Mean (female) = 16.29 (95% CI: 14.95–18.44) vs. Mean (male) = 12.66 (95% CI: 10.15–15.18); t = 2.542 p = 0.011]. The PCL‐5 scores of ethnic minorities were significantly higher than those of Han nationality [Mean (Han) = 21.38 (95% CI: 15.75–27.00) vs. Mean (Minorities) = 15.00 (95% CI: 13.50–16.48); t = −2.32 p = 0.021]. People with lower education level had significantly higher PCL‐5 scores [Mean (university) = 17.59 (95% CI: 15.72–19.46) vs. Mean (postgraduate) = 11.81 (95% CI: 9.69–13.93); t = 3.875 p < 0.001]. The PTSD symptom severity among doctors (Mean = 13.02, 95% CI: 10.88–15.17), nurses (Mean = 18.19, 95% CI: 16.04–20.32) and other professions (Mean = 14.16, 95% CI: 9.68–18.44) differed significantly (F = 5.923, p = 0.003). PCL‐5 scores of emergency department (Mean = 16.83, 95% CI: 14.47–19.18) and respiratory department (Mean = 15.74, 95% CI: 12.91–18.56) were higher than other departments (Mean = 13.69, 95% CI: 11.27–16.10) but did not show significant difference (F = 1.657, p = 0.192). Participants with poorer sleep quality (Very good: Mean = 10.32, 95% CI: 8.40–12.25; Good: Mean = 17.31, 95% CI: 15.31–19.33; Bad: Mean = 19.79, 95% CI: 14.00–24.59; Very bad: Mean = 29.77, 95% CI: 18.50–41.42; F = 15.137, p < 0.001) and less time for leisure activity reported significantly higher PCL‐5 score (No time: Mean = 22.49, 95%CI: 17.35–27.62; Decreased: Mean = 15.98, 95% CI: 14.00–17.97, As usual: Mean = 12.69, 95% CI: 10.32–15.06; Increased: Mean = 11.97, 95% CI: 7.58–16.37; F = 6.753, p < 0.001).
TABLE 1.
Demographic information, sleep quality, time change of leisure activity and group differences of PCL‐5 scores in participants.
| Respondents | PCL‐5 scores | |||||
|---|---|---|---|---|---|---|
| N | % | Mean | SD | F/t | p‐value | |
| Age | ||||||
| ≤35 | 222 | 70.0 | 17.11 | 13.65 | 3.474 | 0.001 |
| >35 | 95 | 30.0 | 11.64 | 10.71 | ||
| Gender | ||||||
| Male | 96 | 30.3 | 12.66 | 12.42 | −2.542 | 0.011 |
| Female | 221 | 69.7 | 16.69 | 13.17 | ||
| Ethnic group | ||||||
| Han | 293 | 92.4 | 15.00 | 12.95 | −2.317 | 0.021 |
| Minorities | 24 | 7.6 | 21.38 | 13.33 | ||
| Education level | ||||||
| University | 201 | 63.4 | 17.59 | 13.46 | 3.875 | <0.001 |
| Postgraduate | 116 | 36.6 | 11.81 | 11.52 | ||
| Classification of medical profession | ||||||
| Doctor | 140 | 44.2 | 13.02 | 12.84 | 5.927 | 0.003 |
| Nurse | 144 | 45.4 | 18.19 | 13.01 | ||
| Others | 33 | 10.4 | 14.06 | 12.35 | ||
| Department | ||||||
| Emergency | 121 | 38.2 | 16.83 | 13.09 | 1.657 | 0.192 |
| Respiratory | 91 | 28.7 | 15.74 | 13.57 | ||
| Others | 105 | 33.1 | 13.69 | 12.50 | ||
| Subjective sleep quality in 1 month | ||||||
| Very good | 117 | 36.9 | 10.32 | 10.50 | 15.137 | <0.001 |
| Good | 158 | 49.8 | 17.31 | 12.79 | ||
| Bad | 29 | 9.1 | 19.79 | 12.61 | ||
| Very bad | 13 | 4.2 | 29.77 | 18.65 | ||
| Time change of leisure activity | ||||||
| No time | 43 | 13.6 | 22.49 | 16.69 | 6.753 | <0.001 |
| Decreased | 147 | 46.4 | 15.98 | 12.19 | ||
| As usual | 96 | 30.3 | 12.69 | 11.69 | ||
| Increased | 31 | 9.7 | 11.97 | 11.97 | ||
3.2. Related factors of the PTSD symptom severity
The results of the hierarchical regression analysis are presented in Table 2. Fear in risk perception used the mean value of fear in five hazards as continuous variable. Knowledge in risk perception used the mean value of knowledge in five hazards as continuous variable.
TABLE 2.
Regression analyses with PCL‐5 score as the dependent variable (n = 317).
| Variable | PCL‐5 score | R 2 | Adjusted R 2 | ΔR 2 | F | p value | ||
|---|---|---|---|---|---|---|---|---|
| В | β | t | ||||||
| Step 1 | 0.076 | 0.064 | 0.064 | 6.380 | <0.001 | |||
| Age | −0.144 | −0.098 | −1.777 | |||||
| Gender | 2.538 | 0.089 | 1.596 | |||||
| Ethnic group | 5.076 | 0.103 | 1.867 | |||||
| Education level | −4.751 | −0.175 | −3.141 ** | |||||
| Step 2 | 0.090 | 0.072 | 0.008 | 5.081 | <0.001 | |||
| Age | −.213 | −.146 | −2.452 * | |||||
| Gender | 2.385 | 0.084 | 1.504 | |||||
| Ethnic group | 5.822 | 0.118 | 2.114 * | |||||
| Education level | −4.287 | −0.158 | −2.636 ** | |||||
| Emergency versus other departments | 2.881 | 0.107 | 1.567 | |||||
| Respiratory versus other departments | 4.077 | 0.141 | 2.101 * | |||||
| Step 3 | 0.271 | 0.247 | 0.175 | 11.393 | <0.001 | |||
| Age | −0.115 | −0.079 | −1.372 | |||||
| Gender | 2.001 | 0.070 | 1.392 | |||||
| Ethnic group | 5.597 | 0.113 | 2.246 * | |||||
| Education level | −1.687 | −0.062 | −1.121 | |||||
| Emergency versus other departments | 2.235 | 0.083 | 1.297 | |||||
| Respiratory versus other departments | 4.432 | 0.154 | 2.487 * | |||||
| Dread in risk perception | 2.091 | 0.142 | 2.682 ** | |||||
| Familiarity in risk perception | 3.644 | 0.203 | 3.497 ** | |||||
| Time change of leisureactivity | −2.794 | −0.179 | −3.415 ** | |||||
| Sleep quality in latest 1 month | 4.236 | 0.249 | 4.758 ** , * | |||||
Note: В = unstandardized beta; β = standardized regression weight. The department was transferred into two dummy variables (emergency vs. other departments and respiratory vs. other departments). Fear in risk perception used the mean value of fear in five hazards as continuous variable. Knowledge in risk perception used the mean value of knowledge in five hazards as continuous variable.
p < 0.05.
p < 0.01.
p < 0.001.
Demographic factors in Table 1 were used as control variables. Education level (β = −0.175, p = 0.002) had significant effects on PCL‐5 scores in step 1. As shown in step 2, age (β = −0.148, p = 0.015), ethnic group (β = 0.118, p = 0.035), education level (β = −0.153, p = 0.009), working in respiratory vs. other departments (β = 0.139, p = 0.036) were significantly correlated with PCL‐5 scores.
Variables related to current study: As shown in step 3, risk perception, both on two dimension of dread (β = 0.142, p = 0.008) and familiarity (β = 0.203, p = 0.001), was positively associated with PCL‐5 scores. Time change of leisure activity (β = −0.179, p = 0.001) were negatively associated with PTSD severity. Sleep quality in latest 1 month (β = 0.250, p < 0.001) was significantly associated with PCL‐5 scores.
Other related factors: In step 3, ethnic group (β = 0.113, p = 0.025), working in respiratory vs. other departments (β = 0.152, p = 0.013), were also found positively correlated with PCL‐5 scores.
3.3. Distribution of COVID‐19‐related hazards on risk cognition map
Locations of COVID‐19‐related hazards on dread‐familiarity two‐dimension cognition map were shown in Figure 2. Overall risk perception towards pandemic was calculated by mean value of five hazards: 2.55 (95% CI: 2.45–2.64) for dread, 2.33 (95% CI: 2.25–2.41) for familiarity. The mean values of dread for SAR‐COV‐2 virus (H1), disease of COVID‐19 (H2), COVID‐19 patient or virus carrier (H3), treatment and prevention of COVID‐19 (H4), and frontline HCWs who had contact with COVID‐19 patients (H5) were 2.74 (95% CI: 14.47–19.18), 2.94 (95% CI: 2.82–3.06), 2.91 (95% CI: 2.80–3.03), 2.45 (95% CI: 2.33–3.57), 1.69 (95% CI: 1.58–1.80), respectively. There were significant differences among five hazards on dread (F = 76.690, p < 0.001). Further multiple comparison found that SAR‐COV‐2 virus (H1), treatment and prevention of COVID‐19 (H4) and frontline HCWs who had contact with COVID‐19 patients (H5) significantly differed from other hazards. The mean values of familiarity from H1 to H5 were 2.32 (95% CI: 2.23–2.41), 2.32 (95% CI: 2.23–2.41), 2.40 (95% CI: 2.31–2.49), 2.27 (95% CI: 2.19–2.36), 2.35 (95% CI: 2.26–2.45), respectively. There was no significant difference among five hazards on familiarity (F = 1.035, p = 0.388).
FIGURE 2.
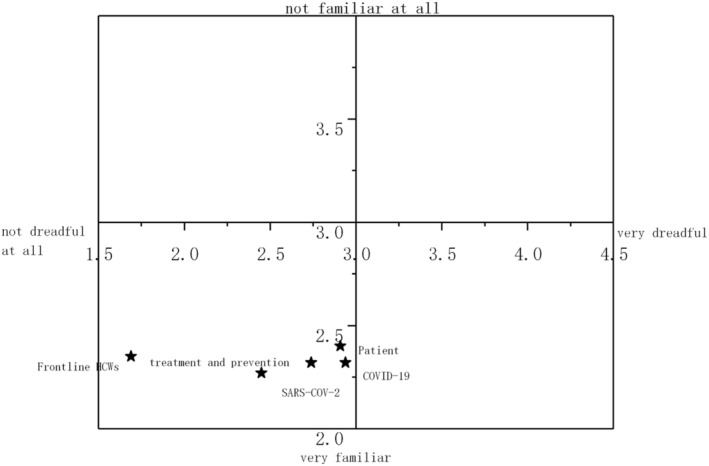
Map of risk perception in all healthcare workers (HCWs)
Locations of COVID‐19‐related hazards on dread‐familiarity two‐dimension cognition map in different subgroups divided by PCL‐5 cut‐off score (33) were shown in Figure 3. The difference of the rated scores of dread and familiarity were presented in Table 3. On the group of PCL‐5 ≥ 33 (n = 34), overall risk perceptions towards pandemic were 3.17 (mean, 95% CI: 2.89–3.45) for dread, 2.72 (mean, 95% CI: 2.53–2.91) for familiarity. The mean values of dread for SAR‐COV‐2 virus (H1), disease of COVID‐19 (H2), COVID‐19 patient or virus carrier (H3), treatment and prevention of COVID‐19 (H4), and frontline HCWs who had contact with COVID‐19 patients (H5) were 3.29 (95% CI: 2.96–3.63), 3.41 (95% CI: 3.08–3.75), 3.44 (95% CI: 3.11–3.78), 3.35 (95% CI: 3.03–3.67), 2.35 (95% CI: 1.96–2.75), respectively. There were significant differences among five hazards on dread (F = 7.381, p < 0.001). Multiple comparison found that H5 significantly differed from other hazards. The mean values of familiarity from H1 to H5 were 2.76 (95% CI: 2.49–3.04), 2.68 (95% CI: 2.45–3.90), 2.82 (95% CI: 2.62–3.02), 2.68 (95% CI: 2.47–2.88), 2.65 (95% CI: 2.42–2.87), respectively. There was no significant difference among five hazards on familiarity (F = 0.439, p = 0.781).
FIGURE 3.
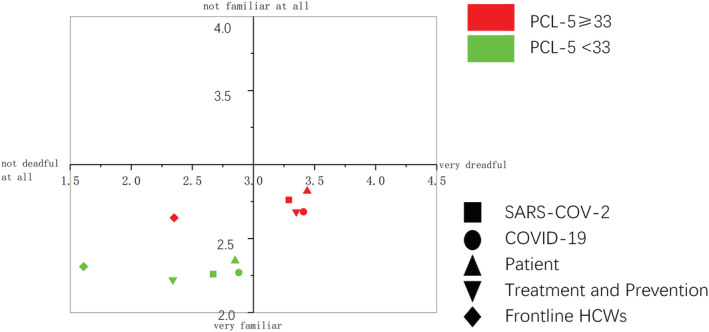
Map of risk perception in different population divided by PCL‐5 [Colour figure can be viewed at wileyonlinelibrary.com]
TABLE 3.
Feature of risk perception in different group divided by PCL‐5 score on five hazards related to COVID‐19 pandemic.
| PTSD symptom severity | Dread | t | p value | Familiarity | t | p ‐value | |||
|---|---|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | ||||||
| Virus:SAR‐COV‐2 | PCL‐5 < 33 | 2.67 | 1.05 | −3.268 | 0.001 | 2.26 | 0.81 | −3.394 | 0.001 |
| PCL‐5 ≥ 33 | 3.29 | 0.97 | 2.76 | 0.78 | |||||
| All | 2.74 | 1.06 | 2.32 | 0.82 | |||||
| Disease caused by virus: COVID‐19 | PCL‐5 < 33 | 2.88 | 1.07 | −2.748 | 0.006 | 2.27 | 0.80 | −2.801 | 0.005 |
| PCL‐5 ≥ 33 | 3.41 | 0.95 | 2.68 | 0.64 | |||||
| All | 2.94 | 1.07 | 2.32 | 0.79 | |||||
| COVID‐19 patient or virus carrier | PCL‐5 < 33 | 2.85 | 1.05 | −3.141 | 0.002 | 2.35 | 0.80 | −3.359 | 0.001 |
| PCL‐5 ≥ 33 | 3.44 | 0.96 | 2.82 | 0.58 | |||||
| All | 2.91 | 1.07 | 2.40 | 0.80 | |||||
| COVID‐19 treatment and prevention | PCL‐5 < 33 | 2.34 | 1.04 | −5.409 | <0.001 | 2.22 | 0.79 | −3.250 | 0.001 |
| PCL‐5 ≥ 33 | 3.35 | 0.92 | 2.68 | 0.59 | |||||
| All | 2.45 | 1.07 | 2.27 | 0.78 | |||||
| Frontline HCWs who had contact with COVID‐19 patients | PCL‐5 < 33 | 1.61 | 0.94 | −4.251 | <0.001 | 2.31 | 0.88 | −2.717 | 0.009 |
| PCL‐5 ≥ 33 | 2.35 | 1.12 | 2.64 | 0.65 | |||||
| All | 1.69 | 0.99 | 2.35 | 0.86 | |||||
| Overall risk perception towards pandemic | PCL‐5 < 33 | 2.47 | 0.87 | −4.474 | <0.001 | 2.29 | 0.73 | −3.330 | 0.001 |
| PCL‐5 ≥ 33 | 3.17 | 0.81 | 2.72 | 0.54 | |||||
| All | 2.55 | 0.89 | 2.33 | 0.73 | |||||
Note: Overall risk perception towards pandemic is calculated by mean value of five hazards. n (PCL‐5 < 33) = 283, n (PCL‐5 ≥ 33) = 34.
On the group of PCL‐5 < 33 (n = 283), overall risk perceptions towards pandemic were 2.47 (95% CI: 2.37–3.57) for dread, 2.29 (95% CI: 2.20–2.37) for familiarity. The mean values of dread for SAR‐COV‐2 virus (H1), disease of COVID‐19 (H2), COVID‐19 patient or virus carrier (H3), treatment and prevention of COVID‐19 (H4), and frontline HCWs who had contact with COVID‐19 patients (H5) were 2.67 (95% CI: 2.55–3.79), 2.88 (95% CI: 2.76–3.01), 2.85 (95% CI: 2.73–2.97), 2.34 (95% CI: 2.22–2.46), 1.61 (95% CI: 1.50–1.72), respectively. There were significant differences among five hazards on dread (F = 73.630, p < 0.001). H1, H4 and H5 significantly differed from other hazards. The mean values of familiarity from H1 to H5 were 2.27 (95% CI: 2.17–2.36), 2.28 (95% CI: 2.19–2.37), 2.35 (95% CI: 2.25–2.44), 2.22 (95% CI: 2.13–2.31), 2.31 (95% CI: 2.21–2.42), respectively. There was no significant difference among five hazards on familiarity (F = 0.950, p = 0.434).
There were significant differences on the rated score of risk perception for five hazards between groups divided by PCL‐5 cut‐off score [H1 (dread: t = −3.268, p = 0.001; familiarity: t = −3.394, p = 0.001); H2 (dread: t = −2.748, p = 0.006; familiarity: t = −2.801, p = 0.005); H3 (dread: t = −3.141, p = 0.002; familiarity: t = −3.359, p = 0.001); H4 (dread: t = −5.409, p < 0.001; familiarity: t = −3.250, p = 0.001); H5 (dread: t = −4.251, p < 0.001; familiarity: t = −2.717, p = 0.009); overall (dread: t = −4.474, p < 0.001; familiarity: t = −3.330, p = 0.001)].
3.4. Model for risk perception, sleep quality, time change of leisure activity and PTSD
Figure 4 shows the effect of risk perception, sleep quality and time change of leisure activity on PTSD. Regression weights were presented in Table 4. In the current model, the adjusted two‐factor model of risk perception of COVD‐19 was used. All indices suggest that the presented model reasonably fits the data (χ2 = 57.963, df = 37), (χ2/df = 1.567, p = 0.15, GFI = 0.975, AGF I = 0.969, AGFI = 0.944, CFI = 0.992, RMSEA = 0.042, SRMR = 0.032). Consistent with our hypotheses, risk perception of COVID‐19 (dread (B = 2.148, β = 0.128, p < 0.017) and familiarity (B = 4.355, β = 0.223, p < 0.001)), sleep quality (B = 4.734, β = 0.278, p < 0.001) and time change of leisure activity (B = −3.734, β = −0.195, p < 0.001) were all directly related to PTSD in HCWs from designated hospitals.
FIGURE 4.
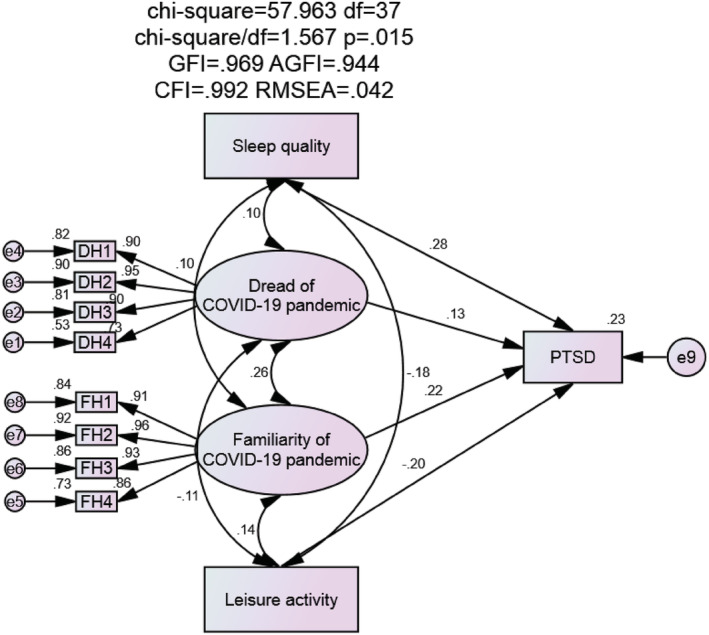
Structural equation model of the effect of risk perception, sleep quality and time change of leisure activity on posttraumatic stress disorder (PTSD) in healthcare workers (HCWs). DH1: Dread of H1 (virus: SAR‐COV‐2); DH2: Dread of H2 (disease: COVID‐19); DH3: Dread of H3 (COVID‐19 patient or virus carrier); DH4: Dread of H4 (treatment and prevention of COVID‐19). FH1: Familiarity of H1 (virus: SAR‐COV‐2); FH2: Familiarity of H2 (disease: COVID‐19); FH3: Familiarity of H3 (COVID‐19 patient or virus carrier); FH4: Familiarity of H4 (treatment and prevention of COVID‐19) [Colour figure can be viewed at wileyonlinelibrary.com]
TABLE 4.
Regression weights in structural model of impact of risk perception, sleep quality and time change of leisure activity on PTSD in HCWs
| Path | Unstd. | S.E. | t value | p | Std | ||
|---|---|---|---|---|---|---|---|
| Dread of COVID‐19 pandemic | —> | PTSD | 2.148 | 0.903 | 2.379 | 0.017 | 0.128 |
| Familiarity of COVID‐19 pandemic | —> | PTSD | 4.355 | 1.061 | 4.106 | <0.001 | 0.223 |
| Sleep quality | —> | PTSD | 4.734 | 0.866 | 5.466 | <0.001 | 0.278 |
| Leisure activity | —> | PTSD | −3.052 | 0.807 | −3.783 | <0.001 | −0.195 |
Note: PTSD is measured by PCL‐5.
4. DISCUSSION AND CONCLUSION
4.1. Summary of the main findings
This study mainly investigated the PTSD symptom and risk perception of COVID‐19 pandemic in HCWs from four designated hospitals for COVID‐19 in Guangdong Province and Guangxi Province 6 months after the outbreak. We found the prevalence of PTSD was 10.7%. Consistent with our hypotheses, our results showed that risk perception of COVID‐19 pandemic was associated with PTSD symptom severity, with those who reporting severer PTSD symptoms having significant different distributions of COVID‐19‐related hazards in cognition map of risk perception from those who did not. As far as we know, this is the first study describing the cognition map based on subgroups of different PTSD severity. In addition, sleep quality in last 1 month and time change of leisure activity were both significantly correlated with PTSD. Other potential related factors of PTSD were also identified (ethnic group and working department).
4.2. Prevalence of PTSD
The prevalence of PTSD in current sample was relatively high compared with recent‐published studies concerning PTSD in HCWs (Chew et al., 2020; Yin et al., 2020) and was close to the prevalence rate from another study conducted in stratified sample of HCWs from Beijing 3 years after outbreak of SARS (Wu et al., 2009). Different from above studies, the current study mainly focused on the population of HCWs in designated hospitals. Over two thirds of our respondents were frontline department staff who continued suffering long hours of work and confronted with high risk of infection. And those who worked in non‐frontline department in a designated hospital also, when consultation of COVID‐19 was needed, were required to have face‐to‐face contact with patients, exposed to deleterious environment. Relatively high working pressure and risk potentially raised the possibility of enhanced PTSD prevalence rate in those population group. Furthermore, the onset of psychiatric symptom could be delayed by the cumulative effect of time. For instance, PTSD symptoms of HCWs would become severer after long time of chronic stress (overloading of work, lack of sleep, worry and fear) and experiencing multiple traumatic event (such as witnessing patient suffering or dying) (Kilpatrick et al., 2013; Schmeltzer et al., 2015). Therefore, the prevalence of PTSD in HCWs might tend to be higher at half year after outbreak than other time points close to the onset of epidemic. However, this finding should be taken cautiously for the current investigation did not directly study the higher prevalence of PTSD by comparing controlled and matched groups of HCWs from designated and non‐designated hospitals with appropriate sampling method. More qualified studies are needed to clarify this issue.
4.3. Risk perception and PTSD
Consistent with our hypothesis, results from regression analysis and SEM supported the significant correlation between the risk perception of COVID‐19 pandemic and PTSD. This finding is similar to the points from previous studies concerning risk perception of infectious disease and PTSD (Jalloh et al., 2018; Lau et al., 2005; Wu et al., 2009). Our results also demonstrated that those HCWs who had significant PTSD symptoms perceived higher pandemic risk. Nevertheless, the causality between risk perception and PTSD remains unclear. Based on psychopathology characteristics of PTSD, it could be inferred that HCWs with significant PTSD symptoms were prone to formulate negative cognition (e.g., ‘Now the world is even more dangerous’) towards COVID‐19 pandemic and elevated their risk perceptions (Brown et al., 2018). On the other hand, high level of risk perception could worsen HCWs' vulnerability towards traumatic experience or chronic stress. The interaction might also exist between those two pathways. Further understanding of this subtle relation demands follow‐up study in large sample at multiple time points.
To add more bricks on previous evidence, we further described two‐dimension (dread‐familiarity) cognition map based on Slovic's paradigm to give more intuitive presentations. In line with our hypothesis, a noteworthy separation of five hazards was observed between two group divided by PTSD severity (four of five hazards from severer PTSD group were separately in another quadrant), which further explained the covered details in the correlation between risk perception and PTSD. In both groups, H5 (frontline HCWs who had contact with COVID‐19 patients) distinctly deviates from the other four hazards, confirming the results of factor analysis of structure of COVID‐19 perception. This result implicated that frontline HCWs, even they were fully exposed to COVID‐19‐related risk, could not appropriately represented perceived risk of COVID‐19 pandemic in the population group of HCWs in designated hospitals, which might be owe to the recognition, acceptance, and knowledge of their own carrier. The locations of risk perception of five hazards among all participants were in the quadrant representing the lower level of dread and unfamiliarity and. Those hazards which drove higher perceived risk were mainly H2 (Disease: COVID‐19) and (H3. COVID‐19 patient or virus carrier). The relatively low perception of the risk of COVID‐19 pandemic in HCWs might partly rely on their professional convenience of learning about the virus and disease, which consequently impeded the generalization of fear. Meanwhile, effective measures of the government, such as increasing physical distance, wearing mask, self‐quarantine at home, closed schools, discouraged mass gatherings, and cancelled or postponed large public events, along with the powerful compliance of general public, hampered the further spread of the epidemic and reduced fear in general public (Chen, Yang, Yang, Wang, & Bärnighausen, 2020; MacIntyre & Wang, 2020; Prem et al., 2020). On the last day of current research, there were only 17 COVID‐19 patients being treated in Guangdong Province, with no increased cases from native population (CDCGD, 2020). Shi et al. (2003) investigated SARS‐related hazards public in 2003 among the public, using a different method to describe of SAR‐related hazards and controllability as the representation of dread risk, also showed similar pattern that majority of the hazards were mainly concentrating around the ‘Minimum risk’ quadrant, except that the aetiology of SARS was in the ‘Maximum risk’ quadrant (Shi et al., 2003), which implicated general population had higher risk perception of source of the wide‐spread infectious disease than HCWs.
4.4. Sleep quality, time change of leisure activity and PTSD
Similarly, our results also supported the that sleep quality and time change of leisure activity were significantly correlated with PTSD, respectively. Sleep quality was consistently found positively correlated with PTSD symptom. One main reason could be that sleep disturbance was one of the self‐reported items in PTSD scales (Foa et al., 2016a; Foa et al., 2016b; Weathers et al., 2013). Ered, Cooper, and Ellman (2018) suggested that depression and PTSD mediated the relationship between psychotic‐like experiences and sleep quality. Treating symptoms of depression and PTSD might improve several domains of psychotic illness (Ered et al., 2018). Majority of the recruited HCWs reported that they had less or none time for leisure activity. Those who had more time for leisure activity, which might reflect less hours of work, lower level of COVID‐19 risk exposure and more time for self‐adjustment, had less self‐reported PTSD symptoms. Results from sleep quality and time for leisure activity indicated that sufficient rest and rational working shift were protective factors for psychological impact of pandemic.
4.5. Other related factors of PTSD
The current study also found that related factors of PTSD symptom score included ethnic group, and working department (respiratory vs. other departments). HCWs of minorities had relatively high PTSD severity. This finding needs further confirmation for number of minorities was quite small. However, there have been studies reporting the reporting the relation between the identity of minorities and PTSD (Koo, Hebenstreit, Madden, & Maguen, 2016; Spoont, Sayer, Kehle‐Forbes, Meis, & Nelson, 2017; Wei, Wang, Heppner, & Du, 2012). In terms of the difference between the working department, HCWs in respiratory department directly handled the affairs of treatment and diagnosis for COVID‐19 patients, with increased risk and workload. An acute overwhelming stress might induce rapid changes in psychological status among those frontline HCWs and effect could last for a long time (Su et al., 2007).
4.6. Limitations
Although current study demonstrated some meaningful outcomes, several limitations need to be considered in this study. First, we intended to focus on the groups of HCWs with relative high risk of COVID‐19 epidemic—those who were in designated hospitals. However, instead of using probability sampling method, convenience sampling is adopted to extract samples, making it difficult to generalize our results to HCWs in designated hospitals. To balance the sample at best of our ability, we both investigated frontline and non‐frontline departments. Second, in order to control the length of online questionnaire, only one factor (dread and familiarity) was used in each dimension of the Slovic's risk perception cognitive model (dread risk and unknown risk). Whether two factor in our analysis could fully represent the Slovic's model still awaits further confirmation. More factorial questions were required to comprehensively evaluate the risk perception in the future. Third, there was only one single item to investigated sleep quality and time change of leisure activity which limited the reliability and validity of those investigations. Fourth, in the difference analysis, the difference between the number of participants in each subgroup is large, which could result in potential bias. Last, the causal relation and psychological mechanism and mediators between risk perception and PTSD were not explored in this article.
4.7. Implications
Based on the significant associations between risk perceptions and PTSD in the current study, it implicated the management or intervention of risk cognition, such as health education or propaganda for strengthening the knowledge of the risk and effective prevention of COVID‐19 pandemic, could help to regulate stress for HCWs who work in frontline, which further contributes to reducing psychological distress, including PTSD symptoms. Since sleep quality and time change of leisure activity both had significant relation to PTSD severity, importance should be attached to having HCWs realize the necessity to arrange enough time for daily adjustment to restore health status against adverse effect triggered by negative events.
5. CONCLUSIONS
In HCWs from designated hospitals, risk perception independently and positively correlated with PTSD symptom. The locations of COVID‐19 hazards were significantly different between groups of high and low level PTSD symptom. Other PTSD‐related factors included sleep quality, time change of leisure activities, ethnic group, and working department (respiratory vs. other departments). This study provides latent target points for the management and control of the PTSD symptoms under pandemic in frontline HCWs. More large‐sample researches with long‐term follow‐up are warranted on the formulation and predictors of pandemic risk perception, and causal relationship between risk perception and psychological impact of pandemic.
CONFLICT OF INTEREST
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
AUTHOR CONTRIBUTIONS
GSY carried out statistical analyses and wrote the protocol and manuscript draft. ZYG and ZWY individually searched for relevant studies, eligibility assessments for inclusion criteria, and quality checks for the obtained studies. ZYG also participated in specific parts of data analysis and preparation of manuscript. LAN, CYH, XJY and SJ assisted with the preparation and proof‐reading of the manuscript, LX designed the study, and supervised the data analysis and the writing of the paper. LWZ and ZWM provided the advices on statistical analysis.
Supporting information
Figures S1. One factor model of risk perception of COVID‐19 pandemic DH1: Dread of H1 (virus: SAR‐COV‐2); DH2: Dread of H2 (disease: COVID‐19); DH3: Dread of H3 (COVID‐19 patient or virus carrier); DH4: Dread of H4 (treatment and prevention of COVID‐19); DH5: Dread of H5 (frontline HCWs who had contact with COVID‐19 patients). FH1: Familiarity of H1 (virus: SAR‐COV‐2); FH2: Familiarity of H2 (disease: COVID‐19); FH3: Familiarity of H3 (COVID‐19 patient or virus carrier); FH4: Familiarity of H4 (treatment and prevention of COVID‐19); FH5: Familiarity of H5 (frontline HCWs who had contact with COVID‐19 patients).
Figures S2. Two model factor of risk perception of COVID‐19 pandemic DH1: Dread of H1 (virus: SAR‐COV‐2); DH2: Dread of H2 (disease: COVID‐19); DH3: Dread of H3 (COVID‐19 patient or virus carrier); DH4: Dread of H4 (treatment and prevention of COVID‐19); DH5: Dread of H5 (frontline HCWs who had contact with COVID‐19 patients). FH1: Familiarity of H1 (virus: SAR‐COV‐2); FH2: Familiarity of H2 (disease: COVID‐19); FH3: Familiarity of H3 (COVID‐19 patient or virus carrier); FH4: Familiarity of H4 (treatment and prevention of COVID‐19); FH5: Familiarity of H5 (frontline HCWs who had contact with COVID‐19 patients).
Figures S3. Adjusted Two model factor of risk perception of COVID‐19 pandemic. The dread and familiarity of frontline HCWs who had contact with COVID‐19 patients were deleted. DH1: Dread of H1 (virus: SAR‐COV‐2); DH2: Dread of H2 (disease: COVID‐19); DH3: Dread of H3 (COVID‐19 patient or virus carrier); DH4: Dread of H4 (treatment and prevention of COVID‐19). FH1: Familiarity of H1 (virus: SAR‐COV‐2); FH2: Familiarity of H2 (disease: COVID‐19); FH3: Familiarity of H3 (COVID‐19 patient or virus carrier); FH4: Familiarity of H4 (treatment and prevention of COVID‐19)
Table S1. Summary of the model fit of risk perception of COVID‐19 pandemic
AGFI: Standardized Root Mean Square Residual; CFI: Comparative Fit Index; GFI: Goodness‐of‐fit index; RMSEA: Comparative Fit Index; SRMR: Standardized Root Mean Square Residual
Table S2. Reliability and convergent validity of adjusted two factor model of risk perception of COVID‐19 pandemic
AVE: Average variance extracted; CR: Composite reliability; SMC: Square multiple correlations.
Table S3. Analysis of discriminant validity of adjusted two factor model of risk perception of COVID‐19 pandemic
AVE: Average variance extracted
ACKNOWLEDGEMENTS
The authors would like to acknowledge the volunteers who participated in the study.
Geng, S. , Zhou, Y. , Zhang, W. , Lou, A. , Cai, Y. , Xie, J. , Sun, J. , Zhou, W. , Liu, W. , & Li, X. (2021). The influence of risk perception for COVID‐19 pandemic on posttraumatic stress disorder in healthcare workers: A survey from four designated hospitals. Clinical Psychology & Psychotherapy, 28(5), 1146–1159. 10.1002/cpp.2564
Shiyu Geng, Yaoguang Zhou and Wenyong Zhang are contributed equally to this work.
Contributor Information
Wangmei Zhou, Email: zhouwangmei01@163.com.
Weizhi Liu, Email: 13024141970@163.com.
Xu Li, Email: mylx99@163.com.
DATA AVAILABILITY STATEMENT
Data in this study will not be shared, for data protection reasons and participants were informed that the data would only be used in the form of publication and would not be shared.
REFERENCES
- Abrams, E. M. , & Greenhawt, M. (2020). Risk communication during COVID‐19. The Journal of Allergy and Clinical Immunology. In Practice, 8(6), 1791–1794. 10.1016/j.jaip.2020.04.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blevins, C. A. , Weathers, F. W. , Davis, M. T. , Witte, T. K. , & Domino, J. L. (2015). The posttraumatic stress disorder checklist for DSM‐5 (PCL‐5): Development and initial psychometric evaluation. Journal of Traumatic Stress, 28(6), 489–498. 10.1002/jts.22059 [DOI] [PubMed] [Google Scholar]
- Brown, W. J. , Dewey, D. , Bunnell, B. E. , Boyd, S. J. , Wilkerson, A. K. , Mitchell, M. A. , & Bruce, S. E. (2018). A critical review of negative affect and the application of CBT for PTSD. Trauma Violence Abuse, 19(2), 176–194. 10.1177/1524838016650188 [DOI] [PubMed] [Google Scholar]
- Buysse, D. J. , Reynolds, C. F. 3rd , Monk, T. H. , Berman, S. R. , & Kupfer, D. J. (1989). The Pittsburgh sleep quality index: A new instrument for psychiatric practice and research. Psychiatry Research, 28(2), 193–213. 10.1016/0165-1781(89)90047-4 [DOI] [PubMed] [Google Scholar]
- Cappelleri, J. C. , Bushmakin, A. G. , McDermott, A. M. , Sadosky, A. B. , Petrie, C. D. , & Martin, S. (2009). Psychometric properties of a single‐item scale to assess sleep quality among individuals with fibromyalgia. Health and Quality of Life Outcomes, 7, 54. 10.1186/1477-7525-7-54 [DOI] [PMC free article] [PubMed] [Google Scholar]
- CDC . (2020). Real time data of distribution of COVID‐19 epidemic. Official web of Chinese Center for Disease Control and Prevention.
- CDCGD . (2020). Daily report of situation of COVID‐19 in Guandong Province.
- Cha, Y. J. (2018). Correlation between leisure activity time and life satisfaction: Based on KOSTAT time use survey data. Occupational Therapy International, 2018, 5154819–9. 10.1155/2018/5154819 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen, Q. , Liang, M. , Li, Y. , Guo, J. , Fei, D. , Wang, L. , … Zhang, Z. (2020). Mental health care for medical staff in China during the COVID‐19 outbreak. Lancet Psychiatry, 7, e15–e16. 10.1016/s2215-0366(20)30078-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen, S. , Yang, J. , Yang, W. , Wang, C. , & Bärnighausen, T. (2020). COVID‐19 control in China during mass population movements at new year. Lancet, 395(10226), 764–766. 10.1016/s0140-6736(20)30421-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chew, N. W. S. , Lee, G. K. H. , Tan, B. Y. Q. , Jing, M. , Goh, Y. , Ngiam, N. J. H. , … Sharma, V. K. (2020). A multinational, multicentre study on the psychological outcomes and associated physical symptoms amongst healthcare workers during COVID‐19 outbreak. Brain, Behavior, and Immunity, 88, 559–565. 10.1016/j.bbi.2020.04.049 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cori, L. , Bianchi, F. , Cadum, E. , & Anthonj, C. (2020). Risk perception and COVID‐19. International Journal of Environmental Research and Public Health, 17(9). 10.3390/ijerph17093114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Director‐General, W. (2020). WHO Director‐General's opening remarks at the Mission briefing on COVID‐19‐2 April 2020. WHO Director‐General Speech.
- Ered, A. , Cooper, S. , & Ellman, L. M. (2018). Sleep quality, psychological symptoms, and psychotic‐like experiences. Journal of Psychiatric Research, 98, 95–98. 10.1016/j.jpsychires.2017.12.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fischhoff, B. (2015). The realities of risk‐cost‐benefit analysis. Science (New York, N.Y.), 350(6260), aaa6516. 10.1126/science.aaa6516 [DOI] [PubMed]
- Foa, E. B. , McLean, C. P. , Zang, Y. , Zhong, J. , Powers, M. B. , Kauffman, B. Y. , … Knowles, K. (2016a). Psychometric properties of the posttraumatic diagnostic scale for DSM‐5 (PDS‐5). Psychological Assessment, 28(10), 1166–1171. 10.1037/pas0000258 [DOI] [PubMed] [Google Scholar]
- Foa, E. B. , McLean, C. P. , Zang, Y. , Zhong, J. , Rauch, S. , Porter, K. , … Kauffman, B. Y. (2016b). Psychometric properties of the posttraumatic stress disorder symptom scale interview for DSM‐5 (PSSI‐5). Psychological Assessment, 28(10), 1159–1165. 10.1037/pas0000259 [DOI] [PubMed] [Google Scholar]
- Hakansson, C. , Axmon, A. , & Eek, F. (2016). Insufficient time for leisure and perceived health and stress in working parents with small children. Work, 55(2), 453–461. 10.3233/WOR-162404 [DOI] [PubMed] [Google Scholar]
- Holshue, M. L. , DeBolt, C. , Lindquist, S. , Lofy, K. H. , Wiesman, J. , Bruce, H. , … Pillai, S. K. (2020). First case of 2019 novel coronavirus in the United States. The New England Journal of Medicine, 382(10), 929–936. 10.1056/NEJMoa2001191 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holstila, A. , Manty, M. , Rahkonen, O. , Lahelma, E. , & Lahti, J. (2017). Changes in leisure‐time physical activity and physical and mental health functioning: A follow‐up study. Scandinavian Journal of Medicine & Science in Sports, 27(12), 1785–1792. 10.1111/sms.12758 [DOI] [PubMed] [Google Scholar]
- Jalloh, M. F. , Li, W. , Bunnell, R. E. , Ethier, K. A. , O'Leary, A. , Hageman, K. M. , … Redd, J. T. (2018). Impact of Ebola experiences and risk perceptions on mental health in Sierra Leone, July 2015. BMJ Global Health, 3(2). 10.1136/bmjgh-2017-000471 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jung, H. , Jung, S. Y. , Lee, M. H. , & Kim, M. S. (2020). Assessing the presence of post‐traumatic stress and turnover intention among nurses post‐Middle East respiratory syndrome outbreak: The importance of supervisor support. Workplace Health & Safety, 68, 345. 10.1177/2165079919897693 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kang, L. , Li, Y. , Hu, S. , Chen, M. , Yang, C. , Yang, B. X. , … Liu, Z. (2020). The mental health of medical workers in Wuhan, China dealing with the 2019 novel coronavirus. Lancet Psychiatry, 7(3), e14. 10.1016/s2215-0366(20)30047-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kilpatrick, D. G. , Resnick, H. S. , Milanak, M. E. , Miller, M. W. , Keyes, K. M. , & Friedman, M. J. (2013). National estimates of exposure to traumatic events and PTSD prevalence using DSM‐IV and DSM‐5 criteria. Journal of Traumatic Stress, 26(5), 537–547. 10.1002/jts.21848 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koo, K. H. , Hebenstreit, C. L. , Madden, E. , & Maguen, S. (2016). PTSD detection and symptom presentation: Racial/ethnic differences by gender among veterans with PTSD returning from Iraq and Afghanistan. Journal of Affective Disorders, 189, 10–16. 10.1016/j.jad.2015.08.038 [DOI] [PubMed] [Google Scholar]
- Lai, C. C. , Shih, T. P. , Ko, W. C. , Tang, H. J. , & Hsueh, P. R. (2020). Severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2) and coronavirus disease‐2019 (COVID‐19): The epidemic and the challenges. International Journal of Antimicrobial Agents, 55(3), 105924. 10.1016/j.ijantimicag.2020.105924 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lancee, W. J. , Maunder, R. G. , Goldbloom, D. S. , & Coauthors for the Impact of, S. S . (2008). Prevalence of psychiatric disorders among Toronto hospital workers one to two years after the SARS outbreak. Psychiatric Services, 59(1), 91–95. 10.1176/ps.2008.59.1.91 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lau, J. T. F. , Yang, X. , Pang, E. , Tsui, H. Y. , Wong, E. , & Wing, Y. K. (2005). SARS‐related perceptions in Hong Kong. Emerging Infectious Diseases, 11(3), 417–424. 10.3201/eid1103.040675 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewis, C. , Lewis, K. , Kitchiner, N. , Isaac, S. , Jones, I. , & Bisson, J. I. (2020). Sleep disturbance in post‐traumatic stress disorder (PTSD): A systematic review and meta‐analysis of actigraphy studies. European Journal of Psychotraumatology, 11(1), 1767349. 10.1080/20008198.2020.1767349 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin, C. Y. , Peng, Y. C. , Wu, Y. H. , Chang, J. , Chan, C. H. , & Yang, D. Y. (2007). The psychological effect of severe acute respiratory syndrome on emergency department staff. Emergency Medicine Journal, 24(1), 12–17. 10.1136/emj.2006.035089 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu, N. , Zhang, F. , Wei, C. , Jia, Y. , Shang, Z. , Sun, L. , … Liu, W. (2020). Prevalence and predictors of PTSS during COVID‐19 outbreak in China hardest‐hit areas: Gender differences matter. Psychiatry Research, 287, 112921. 10.1016/j.psychres.2020.112921 [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacIntyre, C. R. , & Wang, Q. (2020). Physical distancing, face masks, and eye protection for prevention of COVID‐19. Lancet, 395(10242), 1950–1951. 10.1016/s0140-6736(20)31183-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Malecki, K. , Keating, J. A. , & Safdar, N. (2020). Crisis communication and public perception of COVID‐19 risk in the era of social media. Clinical Infectious Diseases: An Official Publication of the Infectious Diseases Society of America.. 10.1093/cid/ciaa758 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mausbach, B. T. , Romero‐Moreno, R. , Bos, T. , von Kanel, R. , Ziegler, M. G. , Allison, M. A. , … Grant, I. (2017). Engagement in pleasant leisure activities and blood pressure: A 5‐year longitudinal study in Alzheimer caregivers. Psychosomatic Medicine, 79(7), 735–741. 10.1097/PSY.0000000000000497 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McAlonan, G. M. , Lee, A. M. , Cheung, V. , Cheung, C. , Tsang, K. W. , Sham, P. C. , … Wong, J. G. (2007). Immediate and sustained psychological impact of an emerging infectious disease outbreak on health care workers. Canadian Journal of Psychiatry, 52(4), 241–247. 10.1177/070674370705200406 [DOI] [PubMed] [Google Scholar]
- NHC . (2020). Diagnosis and treatment of novel coronavirus pneumonia. www.gov.cn
- Pien, G. W. , Sammel, M. D. , Freeman, E. W. , Lin, H. , & DeBlasis, T. L. (2008). Predictors of sleep quality in women in the menopausal transition. Sleep, 31(7), 991–999. [PMC free article] [PubMed] [Google Scholar]
- Prem, K. , Liu, Y. , Russell, T. W. , Kucharski, A. J. , Eggo, R. M. , Davies, N. , … Hellewell, J. (2020). The effect of control strategies to reduce social mixing on outcomes of the COVID‐19 epidemic in Wuhan, China: A modelling study. The Lancet Public Health, 5(5), e261–e270. 10.1016/s2468-2667(20)30073-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Remuzzi, A. , & Remuzzi, G. (2020). COVID‐19 and Italy: What next? Lancet, 395(10231), 1225–1228. 10.1016/s0140-6736(20)30627-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sandman, P. M. (1988). Risk communication: Facing public outrage. Management Communication Quarterly, 2(2), 235–238. 10.1177/0893318988002002006 [DOI] [Google Scholar]
- Schmeltzer, S. N. , Vollmer, L. L. , Rush, J. E. , Weinert, M. , Dolgas, C. M. , & Sah, R. (2015). History of chronic stress modifies acute stress‐evoked fear memory and acoustic startle in male rats. Stress, 18(2), 244–253. 10.3109/10253890.2015.1016495 [DOI] [PubMed] [Google Scholar]
- Shalev, A. , Liberzon, I. , & Marmar, C. (2017). Post‐traumatic stress disorder. The New England Journal of Medicine, 376(25), 2459–2469. 10.1056/NEJMra1612499 [DOI] [PubMed] [Google Scholar]
- Shi, K. , Fan, H. , Jia, J. , Li, W. , Song, Z. , Gao, J. , … Hu, W. (2003). The risk perceptions of SARS and Scio‐psychologcal behaviors of urban people in China. Acta Psychologica Sinica, 35(4), 546–554. [Google Scholar]
- Slovic, P. (1987). Perception of risk. Science (New York, N.Y.), 236(4799), 280‐285. 10.1126/science.3563507 [DOI] [PubMed]
- Spoont, M. R. , Sayer, N. A. , Kehle‐Forbes, S. M. , Meis, L. A. , & Nelson, D. B. (2017). A prospective study of racial and ethnic variation in VA psychotherapy services for PTSD. Psychiatric Services, 68(3), 231–237. 10.1176/appi.ps.201600086 [DOI] [PubMed] [Google Scholar]
- Su, T.‐P. , Lien, T.‐C. , Yang, C.‐Y. , Su, Y. L. , Wang, J.‐H. , Tsai, S.‐L. , & Yin, J.‐C. (2007). Prevalence of psychiatric morbidity and psychological adaptation of the nurses in a structured SARS caring unit during outbreak: A prospective and periodic assessment study in Taiwan. Journal of Psychiatric Research, 41(1–2), 119–130. 10.1016/j.jpsychires.2005.12.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suwantarat, N. , & Apisarnthanarak, A. (2015). Risks to healthcare workers with emerging diseases: Lessons from MERS‐CoV, Ebola, SARS, and avian flu. Current Opinion in Infectious Diseases, 28(4), 349–361. 10.1097/QCO.0000000000000183 [DOI] [PubMed] [Google Scholar]
- Taghrir, M. H. , Borazjani, R. , & Shiraly, R. (2020). COVID‐19 and Iranian medical students: A survey on their related‐knowledge, preventive behaviors and risk perception. Arch Iran Med, 23(4), 249–254. 10.34172/aim.2020.06 [DOI] [PubMed] [Google Scholar]
- Vyas, K. J. , Delaney, E. M. , Webb‐Murphy, J. A. , & Johnston, S. L. (2016). Psychological impact of deploying in support of the U.S. response to Ebola: A systematic review and meta‐analysis of past outbreaks. Military Medicine, 181(11), e1515–e1531. 10.7205/MILMED-D-15-00473 [DOI] [PubMed] [Google Scholar]
- Wang, C. , Pan, R. , Wan, X. , Tan, Y. , Xu, L. , Ho, C. S. , & Ho, R. C. (2020). Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID‐19) epidemic among the General population in China. International Journal of Environmental Research and Public Health, 17(5). 10.3390/ijerph17051729 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang, L. , Zhang, L. , Armour, C. , Cao, C. , Qing, Y. , Zhang, J. , … Fan, G. (2015). Assessing the underlying dimensionality of DSM‐5 PTSD symptoms in Chinese adolescents surviving the 2008 Wenchuan earthquake. Journal of Anxiety Disorders, 31, 90–97. 10.1016/j.janxdis.2015.02.006 [DOI] [PubMed] [Google Scholar]
- Weathers, F. W. , Litz, B. T. , Keane, T. M. , Palmieri, P. A. , Marx, B. P. , & Schnurr, P. P. (2013). The PTSD checklist for DSM‐5 (PCL‐5). National Center for PTSD.
- Wei, M. , Wang, K. T. , Heppner, P. P. , & Du, Y. (2012). Ethnic and mainstream social connectedness, perceived racial discrimination, and posttraumatic stress symptoms. Journal of Counseling Psychology, 59(3), 486–493. 10.1037/a0028000 [DOI] [PubMed] [Google Scholar]
- White, R. L. , Babic, M. J. , Parker, P. D. , Lubans, D. R. , Astell‐Burt, T. , & Lonsdale, C. (2017). Domain‐specific physical activity and mental health: A meta‐analysis. American Journal of Preventive Medicine, 52(5), 653–666. 10.1016/j.amepre.2016.12.008 [DOI] [PubMed] [Google Scholar]
- WHO (2020). Coronavirus disease (COVID‐19) Situation Report—171.
- Wu, P. , Fang, Y. , Guan, Z. , Fan, B. , Kong, J. , Yao, Z. , … Hoven, C. W. (2009). The psychological impact of the SARS epidemic on hospital employees in China: Exposure, risk perception, and altruistic acceptance of risk. Canadian Journal of Psychiatry, 54(5), 302–311. 10.1177/070674370905400504 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yin, Q. , Sun, Z. , Liu, T. , Ni, X. , Deng, X. , Jia, Y. , … Liu, W. (2020). Posttraumatic stress symptoms of health care workers during the corona virus disease 2019. Clinical Psychology & Psychotherapy, 27(3), 384–395. 10.1002/cpp.2477 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Figures S1. One factor model of risk perception of COVID‐19 pandemic DH1: Dread of H1 (virus: SAR‐COV‐2); DH2: Dread of H2 (disease: COVID‐19); DH3: Dread of H3 (COVID‐19 patient or virus carrier); DH4: Dread of H4 (treatment and prevention of COVID‐19); DH5: Dread of H5 (frontline HCWs who had contact with COVID‐19 patients). FH1: Familiarity of H1 (virus: SAR‐COV‐2); FH2: Familiarity of H2 (disease: COVID‐19); FH3: Familiarity of H3 (COVID‐19 patient or virus carrier); FH4: Familiarity of H4 (treatment and prevention of COVID‐19); FH5: Familiarity of H5 (frontline HCWs who had contact with COVID‐19 patients).
Figures S2. Two model factor of risk perception of COVID‐19 pandemic DH1: Dread of H1 (virus: SAR‐COV‐2); DH2: Dread of H2 (disease: COVID‐19); DH3: Dread of H3 (COVID‐19 patient or virus carrier); DH4: Dread of H4 (treatment and prevention of COVID‐19); DH5: Dread of H5 (frontline HCWs who had contact with COVID‐19 patients). FH1: Familiarity of H1 (virus: SAR‐COV‐2); FH2: Familiarity of H2 (disease: COVID‐19); FH3: Familiarity of H3 (COVID‐19 patient or virus carrier); FH4: Familiarity of H4 (treatment and prevention of COVID‐19); FH5: Familiarity of H5 (frontline HCWs who had contact with COVID‐19 patients).
Figures S3. Adjusted Two model factor of risk perception of COVID‐19 pandemic. The dread and familiarity of frontline HCWs who had contact with COVID‐19 patients were deleted. DH1: Dread of H1 (virus: SAR‐COV‐2); DH2: Dread of H2 (disease: COVID‐19); DH3: Dread of H3 (COVID‐19 patient or virus carrier); DH4: Dread of H4 (treatment and prevention of COVID‐19). FH1: Familiarity of H1 (virus: SAR‐COV‐2); FH2: Familiarity of H2 (disease: COVID‐19); FH3: Familiarity of H3 (COVID‐19 patient or virus carrier); FH4: Familiarity of H4 (treatment and prevention of COVID‐19)
Table S1. Summary of the model fit of risk perception of COVID‐19 pandemic
AGFI: Standardized Root Mean Square Residual; CFI: Comparative Fit Index; GFI: Goodness‐of‐fit index; RMSEA: Comparative Fit Index; SRMR: Standardized Root Mean Square Residual
Table S2. Reliability and convergent validity of adjusted two factor model of risk perception of COVID‐19 pandemic
AVE: Average variance extracted; CR: Composite reliability; SMC: Square multiple correlations.
Table S3. Analysis of discriminant validity of adjusted two factor model of risk perception of COVID‐19 pandemic
AVE: Average variance extracted
Data Availability Statement
Data in this study will not be shared, for data protection reasons and participants were informed that the data would only be used in the form of publication and would not be shared.


