Dear Editor,
The pandemic of coronavirus disease 19 (COVID‐19) is ongoing. After a reduction of the spread during summer in Western Countries, a rise of incidence has been registered in the last few months. During the first pandemic wave we described an outbreak of chilblain‐like lesions (CLL), affecting in particular children and young adults. 1 , 2 Similar lesions were also observed in many other dermatologic centres. 3 , 4 While in summer no more patients with CLL have been reported, during the second wave of infection we faced again new cases of CLL (n = 10, F/M = 9/1, average age 16.6 years). In addition, interestingly, we could document a relapse of CLL in seven young patients previously observed in spring (F/M = 3/4, average age 15.3 years). These latter were otherwise healthy subjects and had no relevant medical history. Screening for autoimmune diseases was negative. Clinical manifestations were perfectly comparable to their first episode (Fig. 1). In these patients, nasopharyngeal swabs and serology for SARS‐CoV‐2 were performed in spring and showed negative results. Serology was repeated during the relapse, yielding again negative results. In one case we performed a biopsy consistent with histological pictures previously described (Fig. 2). 5 Therefore, both clinical and histological findings were similar to the first episode of CLL. Patients were treated with topical antibiotic and steroid cream with improvement, and follow‐up is currently ongoing.
Figure 1.

Clinical presentation of chilblain‐like lesions on a feet of a 14‐year‐old male. (a) First presentation on April 2020. (b) Relapsing lesions on December 2020. Arrow indicates site of biopsy.
Figure 2.
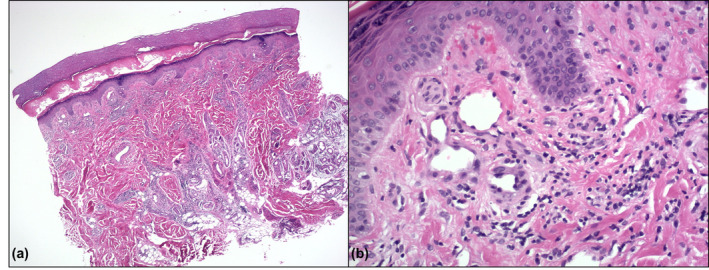
Histologic findings of patient of Fig. 1. (a) Diffuse perivascular and periadnexal involvement of the dermis and hypodermis by a dense lymphoid infiltrate (H&E, 2,5×). (b) Thickening of the vessel wall and activation of the endothelium with nuclear enlargement (H&E, 20×).
How can we explain this relapse? Common characteristics of CLL patients reported so far are the appearance of the lesions during active pandemic in otherwise healthy young subjects, the frequent history of contact with symptomatic affected patients and the lack, in the majority of patients, of laboratory evidence of SARS‐CoV‐2 infection. Even if most of the reports correlate CLL to COVID‐19, the pathogenetic mechanisms which lead to CLL are, so far, speculative. Several reports link the appearance of CLL to the activation of a type I interferon (IFN) response in infected patients. 6 , 7 , 8 , 9 , 10 IFN is crucial in the early response to viral infections and its production is higher in infancy and young adulthood and then decreases with age. 6 Achoff et al. provided evidence for a role of type I IFN in the pathogenesis of CLL by using immunohistochemistry. They speculated that the direct infection of endothelial cells may be sufficient to induce local type I IFN induction and CLL. 7 This finding has been recently supported by Hubiche et al. 6 , who demonstrated an increased IFN‐alfa response in CLL patients as compared to non‐CLL patients with acute COVID‐19 infection. The hypothesis of a pathogenetic role of IFNs in the development of CLL is further supported by the observation that patients with chronic type I IFN activation due to rare genetic type I interferonopathies frequently develop chilblain lesions. 8 According to this hypothesis, a strong early type I IFN response would lead to a fast and efficient control of the viral infection by the innate immune system, thus protecting from progression to severe respiratory disease. 9 , 10 This might be the reason for the low positive rate of nasopharyngeal swabs and the lack of an antibody response in these young patients, who possibly cleared the infection before an antibody response occurs. 4 On this basis, the relapse of CLL would follow a new contact with SARS‐CoV‐2: the lack of anti‐SARS‐CoV‐2 antibodies made these patients liable to reinfection and to a new IFN response. This new viral contact can be related to the resurgence of the pandemic we are now facing, especially if we consider that most of these patients are children of health workers.
Funding sources
None to declare.
Conflict of interest
The authors have no conflicts of interest to declare.
Acknowledgement
The patients in this manuscript have given written informed consent to publication of their case details.
References
- 1. Recalcati S, Barbagallo T, Frasin LA et al. Acral cutaneous lesions in the time of COVID‐19. J Eur Acad Dermatol Venereol 2020; 34: e346–e347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Recalcati S, Fantini F. Chilblain‐like lesions during the COVID‐19 pandemic: early or late sign? Int J Dermatol 2020; 59: e268–e269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. El Hachem M, Diociaiuti A, Concato C et al. A clinical, histopathological and laboratory study of 19 consecutive Italian paediatric patients with chilblain‐like lesions: lights and shadows on the relationship with COVID‐19 infection. J Eur Acad Dermatol Venereol 2020; 34: 2620–2629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Roca‐Ginés J, Torres‐Navarro I, Sánchez‐Arráez J et al. Assessment of acute acral lesions in a case series of children and adolescents during the COVID‐19 pandemic. JAMA Dermatol 2020; 156: 992–997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Gianotti R, Recalcati S, Fantini F et al. Histopathological study of a broad spectrum of skin dermatoses in patients affected or highly suspected of infection by COVID‐19 in the Northern Part of Italy: analysis of the many faces of the viral‐induced skin diseases in previous and new reported cases. Am J Dermatopathol 2020; 42: 564–570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Hubiche T, Cardot‐Leccia N, Le Duff F et al. Clinical, laboratory, and interferon‐alpha response characteristics of patients with chilblain‐like lesions during the COVID‐19 pandemic. JAMA Dermatol 2021; 157: 202–206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Aschoff R, Zimmermann N, Beissert S, Günther C. Type I interferon signature in chilblain‐like lesions associated with the COVID‐19 pandemic. Dermatopathology (Basel) 2020; 7: 57–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Lee‐Kirsch MA. The type I interferonopathies. Annu Rev Med 2017; 68: 297–315. [DOI] [PubMed] [Google Scholar]
- 9. Damsky W, Peterson D, King B. When interferon tiptoes through COVID‐19: pernio‐like lesions and their prognostic implications during SARS‐CoV‐2 infection. J Am Acad Dermatol. 2020; 83: e269–e270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Hadjadj J, Yatim N, Barnabei L et al. Impaired type I interferon activity and inflammatory responses in severe COVID‐19 patients. Science 2020; 369: 718–724. [DOI] [PMC free article] [PubMed] [Google Scholar]


