The coronavirus (severe acute respiratory syndrome‐coronavirus 2 [SARS‐CoV‐2], coronavirus disease 2019 [COVID‐19]) pandemic has caused over 88 million confirmed cases and nearly 2 million deaths worldwide as of December 2020. 1 Months ago, governments launched unprecedented responses in an attempt to contain the staggering health and economic threats. In most countries, emergency state declarations with strict confinement and quarantine regulations were followed by phased reopening, emphasizing adherence to public health recommendations regarding hand washing, use of masks, and social distance. However, the situation has continued to evolve, and we are witnessing an increase in the number of cases in many regions of the world. We believe addressing this increase in COVID‐19 cases and preventing further waves of the present pandemic particularly as the first vaccines begin to be offered, requires understanding and addressing optimism bias.
Optimism bias 2 , 3 refers to the mistaken belief that our chances of experiencing negative events are lower than predicted or than those faced by our peers. Such optimism can be beneficial by reducing stress, controlling anxiety, and promoting physical health. However, dealing with the pandemic requires behavioral changes, adherence to precautions, and adoption of personal hygiene practices that may be uncomfortable and cumbersome. Similarly, early acceptance of vaccine harbors some uncertainties. Individuals with excessive optimism bias are less likely to follow such recommendations if they perceive their individual risk to be low, 4 , 5 which not only puts them, but all of us in danger.
Data from the international research and analytics group YouGov (https://yougov.co.uk) reveal that all around the world, people are more worried about the potential health impact of COVID‐19 on others than on themselves. There are, however, striking differences across countries (Fig 1). On average, in the United States, people are about 15% more worried about the health impact of COVID‐19 for others than for their own health, in Europe the average difference is 22%, whereas in the Far East countries it is only 9%. Notably, the disparity in concerns for self versus others across countries is not significantly correlated with the absolute level of fear for self (ρ = −0.15; p = 0.46) or for others (ρ = 0.23; p = 0.27), and is relatively stable across time. This suggests a deeper relation of the disparity in concerns for self versus others with cultural differences. Cultures can be divided into collectivists and individualists. 6 , 7 Individualist cultures, such as those of Europe or the United States, emphasize personal achievement and individual rights even at the expense of group goals. Collectivist culture, such as those of Japan, Korea, or China, emphasize group goals above individual needs or desires. Such cultural differences influence neural activity, for example, in the medial prefrontal cortex, and can thus impact the processing of self‐related information and decision making. 8
FIGURE 1.
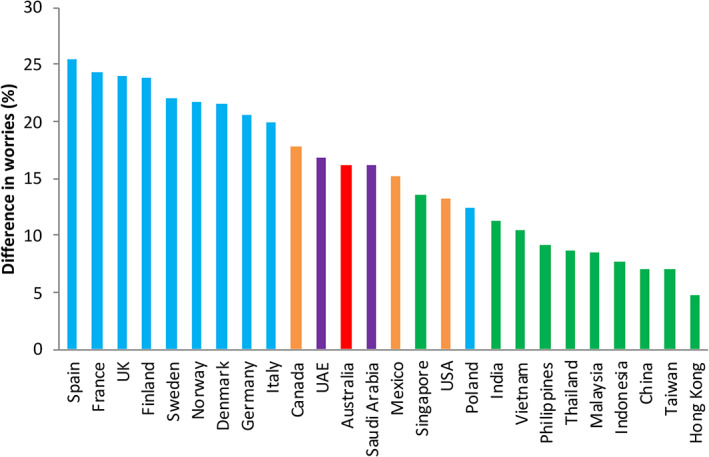
Participants were asked, between May and June, in two different questions about their worries for their own health and for that of peers, including family members and friends. The plot displays the percentage of responders who reported greater concerns for the health of others than for their own health. Colors represent different geographical areas. Blue bar represents Europe, yellow bars North America, red bar Australia, purple bars Middle East, and green bars Far East.
Further relevant insights can be obtained from the Barcelona Brain Health Initiative (BBHI), 9 a longitudinal cohort study assessing genetic, biological, and lifestyle determinants of brain health. A total of 3,326 individuals (1,955 women; mean age 54.2 ± 7.1 years) completed web‐based questionnaires in up to 4 time‐points, March 20 to 22, April 1 to 3, May 4 to 6, and June 1 to 3, 2020, approximately 1, 3, 7, and 11 weeks following the decree of a national state of emergency and a strictly enforced lock‐down mandate by the Spanish government. 10 As part of our questionnaires, participants were asked about their worries regarding their own health and that of their family and friends. Consistent with the YouGov's results, BBHI participants reported being much more worried about the health impact of COVID‐19 on others than on themselves. Figure 2 summarizes the findings across time relating them to the severity of the pandemic in Spain at the time of the various assessments.
FIGURE 2.
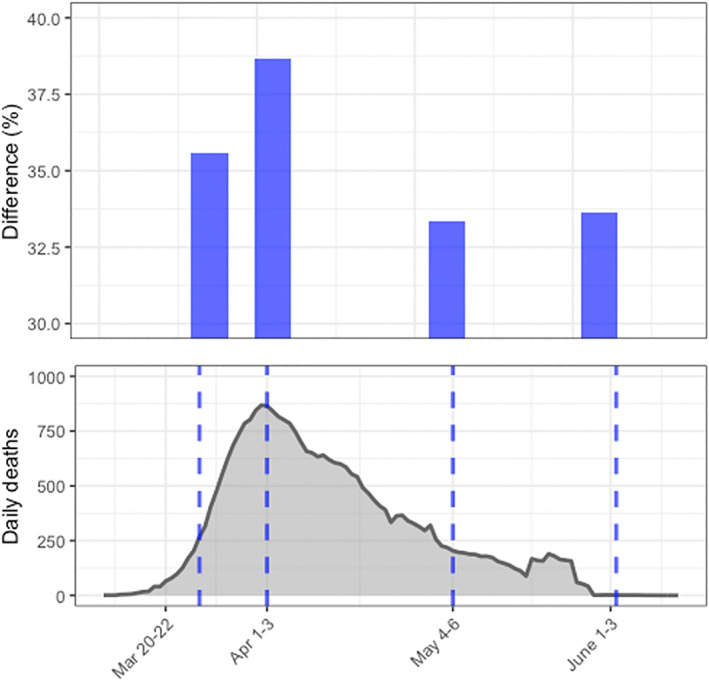
Above: Difference in percentage of Barcelona Brain Health Initiative (BBHI) participants who reported being worried or very worried for their own health versus that of others in the 4 different time points tested. Below: Daily deaths in Spain related to coronarivus disease 2019 (COVID‐19) with vertical lines indicating when the data were collected. New COVID‐19 cases increased from about 3,500 to over 7,700 per day from our first survey (March 20–22) to the second (April 1–3), decreasing afterward to 1,000 and 200 new cases per day at the third and fourth time points, respectively. Similarly, daily deaths rose from about 300 to over 900, descending then to 150 and almost 0 along with the 4 time points.
The difference of over 30% in people's concerns about the health of others than their own was present also among BBHI participants with one or more risk factors for COVID‐19 related morbidity and mortality 11 (including age older than 60 years, preexisting obesity, diabetes or cardiovascular disease, and smokers). Similarly, the discrepancy remained when we looked at the subgroup of participants who had themselves been diagnosed with COVID‐19 (n = 153), needed hospitalization for COVID‐related complications (n = 18), had a family member or close friend diagnosed with COVID (n = 1361), hospitalized for it (n = 749), or who died because of it (n = 284). The probability of stronger concerns for self than for others was, however, significantly smaller in women than men (odds ratio = 0.82, p = 0.05) and was negatively correlated with advancing age (odds ratio per 10 years older of 0.56, p < 0.0001).
It is tempting to want to interpret the difference in health concerns for self versus others as a sign of empathy. Rather than hypothesizing optimism bias leading to a relative lack of concern for oneself, one could consider a stronger “theory of mind” resulting in greater worries for loved ones and friends. 12 However, the cross‐cultural differences, the gender difference, the age‐relation, and the persistence of the findings in the face of changing objective markers of disease severity, are most consistent with optimism bias. 2 , 3 Optimism bias is a pervasive human trait related to prefrontal activity and cognitive control. 3 , 13 An excessive feeling of personal safety harbors the serious threat of disregarding public health recommendations and failing to adopt personal hygiene practices and precautions that may be uncomfortable and cumbersome but are critical to protect us all. Fortunately, optimism bias can be modulated and collectivist values can be promoted. 2 , 14 Therefore, consideration of psychology and cognitive neuroscience is critical to optimize the educational campaigns to ensure the efficacy of public health policies and the early acceptance of vaccination campaigns in limiting pandemic consequences.
Potential Conflicts of Interest
The authors declared no conflict of interest.
Acknowledgments
The research leading to the reported results is funded by grants from “la Caixa” Foundation (grant agreement no. LCF/PR/PR16/11110004), Institut Guttmann and Fundació Abertis. David Bartrés‐Faz was funded by the Spanish Ministry of Science, Innovation, Universities (RTI2018‐095181‐B‐C21), and an ICREA Academia 2019 award research grants. Josep M. Tormos‐Muñoz was partly supported by INNOBRAIN (COMRDI15‐1‐0017).
A special thanks is extended to all participants and other partners (Ad‐Salutem Institute, Sodexo, I.C.A. Informática y Comunicaciones Avanzadas, Neuroelectrics, Corporació Catalana de Mitjans Audiovisuals, Club Metropolitan, Casa Ametller, and Agència de Qualitat i Avaluació Sanitàries de Catalunya‐AQuAS) for their invaluable collaboration.
References
- 1. Worldometer ‐ COVID‐19 . Coronavirus Pandemic. Available at: https://www.worldometers.info/coronavirus/. Last accessed January 8, 2021.
- 2. Sharot T. The optimism bias. Curr Biol 2011;21:R941–R945. [DOI] [PubMed] [Google Scholar]
- 3. Sharot T, Riccardi AM, Raio CM, Phelps EA. Neural mechanisms mediating optimism bias. Nature 2007;450:102–105. [DOI] [PubMed] [Google Scholar]
- 4. Maddux JE, Rogers RW. Protection motivation and self‐efficacy: a revised theory of fear appeals and attitude change. J Exp Soc Psychol 1983;19:469–479. [Google Scholar]
- 5. Floyd DL, Prentice‐Dunn S, Rogers RW. A meta‐analysis of research on protection motivation theory. J Appl Soc Psychol 2000;30:407–429. [Google Scholar]
- 6. Markus HR, Kitayama S. Culture and the self: implications for cognition, emotion, and motivation. Psychol Rev 1991;98:224–253. [Google Scholar]
- 7. Oyserman D, Coon HM, Kemmelmeier M. Rethinking individualism and collectivism: evaluation of theoretical assumptions and meta‐analyses. Psychol Bull 2002;128:3–72. [PubMed] [Google Scholar]
- 8. Chiao JY, Harada T, Komeda H, et al. Neural basis of individualistic and collectivistic views of self. Hum Brain Mapp 2009;30:2813–2820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Cattaneo G, Bartrés‐Faz D, Morris TP, et al. The Barcelona brain health initiative: a cohort study to define and promote determinants of brain health. Front Aging Neurosci 2018;10:321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Del Estado, J . Disposición 3824 del BOE núm. 73 de 2020. (2020).
- 11. Wang L, He W, Yu X, et al. Coronavirus disease 2019 in elderly patients: characteristics and prognostic factors based on 4‐week follow‐up. J Infect 2020;80:639–645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Schaafsma SM, Pfaff DW, Spunt RP, Adolphs R. Deconstructing and reconstructing theory of mind. Trends Cogn Sci 2015;19:65–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Kress L, Aue T. The link between optimism bias and attention bias: a neurocognitive perspective. Neurosci Biobehav Rev 2017;80:688–702. [DOI] [PubMed] [Google Scholar]
- 14. Jolls C, Sunstein CR. Debiasing through law. J Legal Stud 2006;35:199–241. [Google Scholar]


