Abstract
Objectives
The objective was to provide a longitudinal assessment of anxiety levels and work and home concerns of U.S. emergency physicians during the COVID‐19 pandemic.
Methods
We performed a longitudinal, cross‐sectional email survey of clinically active emergency physicians (attending, fellow, and resident) at seven academic emergency departments. Follow‐up surveys were sent 4 to 6 weeks after the initial survey and assessed the following: COVID‐19 patient exposure, availability of COVID‐19 testing, levels of home and workplace anxiety/stress, changes in behaviors, and performance on a primary care posttraumatic stress disorder screen (PC‐PTSD‐5). Logistic regression explored factors associated with a high PC‐PTSD‐5 scale score (≥3), indicating increased risk for PTSD.
Results
Of the 426 surveyed initial respondents, 262 (61.5%) completed the follow‐up survey. While 97.3% (255/262) reported treating suspected COVID‐19 patients, most physicians (162/262, 61.8%) had not received testing themselves. In follow‐up, respondents were most concerned about the relaxing of social distancing leading to a second wave (median score = 6, IQR = 4–7). Physicians reported a consistently high ability to order COVID‐19 tests for patients (median score = 6, IQR = 5–7) and access to personal protective equipment (median score = 6, IQR = 5–6). Women physicians were more likely to score ≥ 3 than men on the PC‐PTSD‐5 screener on the initial survey (43.3% vs. 22.5%; Δ 20.8%, 95% confidence interval [CI] = 9.3% to 31.5%), and despite decreases in overall proportions, this discrepancy remained in follow‐up (34.7% vs. 16.8%; Δ 17.9%, 95% CI = 7.1% to 28.1%). In examining the relationship between demographics, living situations, and institution location on having a PC‐PTSD‐5 score ≥ 3, only female sex was associated with a PC‐PTSD‐5 score ≥ 3 (adjusted odds ratio = 2.48, 95% CI = 1.28 to 4.79).
Conclusions
While exposure to suspected COVID‐19 patients was nearly universal, stress levels in emergency physicians decreased with time. At both initial and follow‐up assessments, women were more likely to test positive on the PC‐PTSD‐5 screener compared to men.
Keywords: COVID‐19, emergency medicine, physicians, psychological, stress
INTRODUCTION
High levels of psychiatric morbidity have been reported by health care workers treating coronavirus disease 2019 (COVID‐19) patients. In Asia and Europe, increased rates of anxiety, stress, insomnia, and depressive symptoms have been noted in frontline health care providers. 1 , 2 , 3 , 4 , 5 , 6 In the first and only report on U.S. emergency physicians, we similarly found negative effects of the COVID‐19 pandemic on provider mental health. 7 Given the evolving nature of the pandemic, we anticipated that stressors related to the COVID‐19 outbreak would change as health care systems and providers dealt with the initial phases of the pandemic. 8 To further examine this evolution, we undertook a longitudinal investigation of stressors, mitigating factors, and stress and anxiety levels in U.S. emergency physicians.
In late March 2020, we initiated a three‐part longitudinal study (acceleration phase, pandemic phase, and postpandemic phase) to assess work‐ and home‐related factors affecting emergency physicians in the United States during the COVID‐19 pandemic. 7 In our first survey, we found high rates of stress, concerns about inadequate access to personal protective equipment (PPE), and changes in behaviors, of both providers and their family and friends. In this follow‐up survey, we reassessed home and workplace anxiety, work‐related stressors, changes to home life, and perceptions as to what measures might ease provider anxiety. We additionally explored stressors that we did not originally anticipate in the initial survey including loss of income, second wave/surge of COVID‐19 cases, and stress due to dependent care. Those responding to the first survey were invited to participate in the second phase follow‐up survey conducted May 7 to 14, 2020. Our goals in this follow‐up study are: (1) to assess changes in stressors and anxiety over time, (2) to determine which stress mitigators were available to respondents at follow‐up, (3) to examine how respondents’ behaviors with family and friends changed over time, and (4) to determine which variables are associated with a higher primary care posttraumatic stress disorder (PC‐PTSD‐5) screener score (≥3). 9
METHODS
Study design, setting, and selection of participants
Our follow‐up cross‐sectional survey was administered via email May 7 to 14, 2020, to all emergency physicians (attending, fellow, and resident) who responded to the first survey (March 23, 2020–April 10, 2020; N = 426) at seven emergency medicine residencies and affiliated institutions in California, New Jersey, and Louisiana. Sites were primarily recruited through their involvement in the National Emergency X‐radiography Utilization Study (NEXUS) network. To broaden the sampling to sites that were experiencing heavy surges of COVID‐19 patients during the acceleration phase (first phase of this study), we contacted two residencies in New York City and one in New Orleans. The investigators in New York declined to participate, because their staff was too overwhelmed at study initiation to meaningfully participate. We excluded nonclinically active physicians for the initial survey. Our study followed the Strengthening the Reporting of Observational Studies in Epidemiology reporting guideline and was deemed exempt by the respective institutional review boards. 10
Methods of measurement
Collaborating with the University of California Stress Network, we developed a follow‐up survey instrument to reassess perceptions and key elements about the following domains: personal experience with COVID‐19 testing, home and workplace anxiety, identification of work‐related stressors, changes in behavior at home arising from their work during the pandemic, and perceptions as to what measures might decrease provider anxiety. This is described in greater detail in our original publication. 7 On the follow‐up survey, we additionally assessed anxiety related to new stressors that physicians were facing. We generated these items based on prior literature and our teams’ own experiences. 1 , 2 , 3 , 4 , 8 These new items included potential income reductions, anxiety related to decreased staffing due to quarantines or staff furloughs, ability for respondents to adequately care for dependents, and concerns regarding patient surges and anticipated “second wave” of COVID‐19 cases. We reassessed emotional exhaustion and burnout by asking participants to rate on a 1 to 7 scale (1 = not at all, 4 = somewhat, and 7= very much) “to what extent were you experiencing severe, ongoing job stress where you felt emotionally exhausted, burned out, cynical about your work and fatigued, even when you wake up?” We also included the five items from the validated PC‐PTSD‐5 scale and used the recommended cutoff of three of five positive responses as a highly sensitive indicator of probable PTSD (Box 1). 9 After pilot testing our follow‐up instrument on five physicians to ensure understanding and a completion time of <5 minutes, our final survey consisted of 18 items. Initial respondents were contacted using the email addresses they supplied when they completed the first survey. Respondent emails were placed into a blinded listserv that was never accessed by the authors, to maintain anonymity of respondents. Only one follow‐up survey submission was allowed per each original respondent. We collected data anonymously via email (with repeat email requests sent two additional times to increase response rate) to each group of providers (Data Supplement S1, Box S1, available as supporting information in the online version of this paper, which is available at http://onlinelibrary.wiley.com/doi/10.1111/acem.14219/full).
Box 1. The Primary Care Post Traumatic Stress Disorder Screen for DSM‐5 (PC‐PTSD‐5) 9 .
In the past month, have you…
1. Had nightmares about the event(s) or thought about the event(s) when you did not want to? YES/NO.
2. Tried hard not to think about the event(s) or went out of your way to avoid situations that reminded you of the event(s)?YES/NO.
3. Been constantly on guard, watchful, or easily startled?YES/NO.
4. Felt numb or detached from people, activities, or your surroundings? YES/NO.
5. Felt guilty or unable to stop blaming yourself or others for the events(s) or any problems the event(s) may have caused? YES/NO.
Data analysis
We captured survey responses using REDCap and used IBM SPSS Statistics version 27.0 (IBM Corp., Armonk, NY) for analyses, summarizing patient characteristics and key responses as raw counts, frequency percent, medians, and interquartile ranges (IQRs). Differences in percentages are presented as Δ with 95% confidence intervals (CIs). Respondents’ ratings of ongoing concerns (initial and follow‐up survey) were compared using Wilcoxon signed‐rank tests, with p < 0.05 as significant. We a priori identified variables that we believed would be associated with a self‐reported PC‐PTSD‐5 scale score ≥ 3 at follow‐up based on our initial results as well as findings from the literature with respect to increased stress levels experienced by women. 3 , 6 A multivariable logistic regression was fitted to explore the association of a self‐reported PC‐PTSD‐5 score ≥ 3 with provider sex, increasing age, level of training (faculty vs. resident/fellow), living circumstances (roommates, partner), presence of children under 18 years in the home, and institution. For institution, individual California sites were compared with the New Jersey and Louisiana sites prior to inclusion in the model. Each California site had a higher percentage of respondents with a PC‐PTSD‐5 score ≥ 3 (all California combined, 25.7%) compared with New Jersey (21.1%) and Louisiana (24.1%). In the regression analysis, California was compared to the other two sites, (California vs. others). Inclusion of our burnout item versus our stress/anxiety item was based on which of the two had a greater association with a PC‐PTSD‐5 score ≥ 3 in univariate analysis. Due to concerns about multicollinearity affecting the preciseness of our model, we elected to only include one of these two variables. Adjusted odds ratios (aOR) are reported with 95% CI.
RESULTS
Of the 426 respondents to the initial survey, 262 (61.5%) completed the follow‐up survey. 7 Table 1 displays the demographics of the survey respondents and Table S1 displays the demographics and item responses to the initial survey among respondents who did and did not complete the follow‐up survey. With the exception of one item, “Personal protective equipment (PPE) is inadequate,” the median scores in the original survey items did not differ between those who participated in the follow‐up survey and those who did not (Table S1). Ninety‐eight percent (257/262) of respondents to the follow‐up survey reported patient contact from April 1, 2020, to survey time (May 7–14, 2020) and 97.3% (255/262) reported treating patients who they suspected had COVID‐19 infections during this time period. The majority reported treating between 11 and 20 patients (23% of respondents) and 21 to 50 patients (36% of respondents). Most physicians (162/262, 61.8%) had not received any testing (reverse transcription polymerase chain reaction or serologic antibody testing) for COVID‐19. Of the 209 physicians who had never received serologic testing, 167 (79.9%) were interested, with the most commonly cited reasons for desiring COVID‐19 testing being: 101 (60.5%) believed all health care workers should be tested, 90 (53.9%) wanted to tell family/friends that they had been tested, and 83 (49.7%) stated that it would help relieve personal anxiety/stress (Table 1).
TABLE 1.
Demographics and baseline characteristics for all subjects who completed the follow‐up survey (N = 262)
| Variable | All subjects |
|---|---|
| Age (y) | 35 (30–44) |
| Female, n/N (%) | 129/259 (49.8) |
| Physician training level | |
| Faculty | 149 (56.9) |
| Fellow | 9 (3.4) |
| Resident | 104 (39.7) |
| Race and ethnicity | |
| African American | 8 (3.1) |
| Asian | 42 (16.0) |
| Latinx | 19 (7.3) |
| Native American | 1 (0.4) |
| Pacific Islander | 0 |
| White | 196 (74.8) |
| Home living situation | |
| Alone | 37 (14.1) |
| With roommate(s) | 23 (8.8) |
| With partner(s) | 195 (74.4) |
| With child < 18 y | 101 (38.5) |
| With adult > 70 y | 2 (0.8) |
| COVID‐19 testing (respondent) | |
| I was tested by | |
| RT‐PCR | 41 (15.6) |
| Serologic | 6 (2.3) |
| Both | 47 (17.9) |
| None | 162 (61.8) |
| Declined to answer | 6 (2.3) |
| Interest in serologic testing (n = 209) | |
| Yes | 124 (59.3) |
| Unsure | 43 (20.6) |
| No | 42 (20.1) |
Data are reported as median (IQR), n/N (%), or n (%).
Abbreviations: COVID‐19, coronavirus disease 2019; RT‐PCR, reverse transcription polymerase chain reaction.
This article is being made freely available through PubMed Central as part of the COVID-19 public health emergency response. It can be used for unrestricted research re-use and analysis in any form or by any means with acknowledgement of the original source, for the duration of the public health emergency.
Median (IQR) work and home stress levels decreased over time from the initial survey 5 (4–6) versus 4 (4–5) at follow‐up. In fact, almost all concerns that were reassessed were less highly rated at follow‐up (Table 2). There were no differences in median stress levels between faculty versus residents/fellows, site, race, or ethnicity. When respondents were asked, “Over the past week, to what extent are you experiencing severe, ongoing job stress where you feel emotionally exhausted, burned out, cynical about your work, and fatigued even when you wake up?” the median burnout score was 4 (2–5), which did not differ from a similar item in the first assessment (Table 2). 7 We further explored potential differences in self‐reported stress levels, burnout, and PC‐PTSD‐5 scores between men and women. For the stress items, women scored higher than men in both the initial and the current surveys (Table 3).
TABLE 2.
Respondents’ ratings of ongoing concerns, new concerns, and stress mitigators during the COVID‐19 pandemic on a 1 to 7 Likert scale a (N = 262)
| Concerns (initial and follow‐up), median (IQR) | Initial survey 7 | Follow‐up survey | p value |
|---|---|---|---|
| I worry that I may being secondarily exposing family members or others because of my work | 6 (4–7) | 5 (4–6) | <0.001 |
| I worry that patients with unclear diagnoses are exposing others in the community | 5 (4–6) | 5 (4–6) | <0.001 |
| I worry that we are not able to accurately diagnose COVID‐19 cases quickly | 5 (4–7) | 4 (2–5) | <0.001 |
| I worry that PPE is inadequate | 5 (4–7) | 4 (2–5) | <0.001 |
| I worry about the well‐being of coworkers who have been diagnosed with COVID‐19 | 5 (4–6) | 4 (3–5) | <0.001 |
| I worry that I might have to undergo quarantine and will not be able to work | 5 (3–6) | 4 (2–5) | <0.001 |
| I worry that we will not have enough staffing as coworkers are quarantined | 5 (3–6) | 3 (2–4) | <0.001 |
| I worry that others at home or elsewhere are afraid to come in contact with me because I’m a health care provider | 4 (3–6) | 4 (3–6) | 0.46 |
| I worry that we are having to send patients home without a clear diagnosis | 4 (3–6) | 4 (2–5) | <0.001 |
| New concerns surveyed | |||
| I worry that the relaxing of social distancing will lead to a second wave of cases | — | 6 (4–7) | |
| I worry that changes in prehospital protocols for other acute patients in the era of COVID‐19 are not best practices given efforts to mitigate exposures and risks to health care providers | — | 4 (3–6) | |
| I worry that colleagues and staff at my medical center will be furloughed or let go to mitigate medical center income loss | — | 4 (3–5) | |
| I worry that my income over the next several months will be impacted by changes in hospital or ED volumes and shortcomings in income at the medical center | — | 4 (2–6) | |
| I worry about my fulfillment with my work given the change in delivery of ED care (mask and face shields) that is less personal and with minimal patient contact | — | 4 (2–5) | |
| I worry that our ED or hospital is not prepared enough to handle a surge in cases | — | 3 (2–4) | |
| I worry that I will not be able to adequately care for my dependents (children, elderly, and others), given that my work duties require that I be outside the home | — | 2 (1–4) | |
| Follow‐up on stress mitigators Identified in first survey | |||
| I can order tests for patients suspected of having COVID‐19 at my discretion | — | 6 (5–7) | |
| I have adequate access to PPE | — | 6 (5–6) | |
| I have easily available rapid turnaround testing for COVID‐19 for my patients | — | 5 (5–6) | |
| Knowing my prior exposure and immunity to COVID‐19 by serologic (blood) testing would decrease my anxiety | — | 5 (4–6) | |
| Communication about changes in COVID‐19 protocols has been clear over the past month | — | 5 (4–6) | |
| I can easily request and obtain COVID‐19 testing for myself | — | 5 (3–6) | |
| I can easily get childcare for my children and assistance for my other dependents so that I can continue to work | — | 4 (4–5) | |
| I have an accurate estimate of my risk for getting COVID‐19 from my work as a health care provider | — | 4 (3–5) | |
| I can easily take leave from work to care for myself and my family members | — | 3 (2–5) | |
| Since the pandemic started, to what extent are you experiencing severe, ongoing job stress where you feel emotionally exhausted, burned out, cynical about your work, and fatigued even when you wake up? | 4 (3–6) | — | |
| Over the past week, to what extent are you experiencing severe, ongoing job stress where you feel emotionally exhausted, burned out, cynical about your work, and fatigued even when you wake up? | — | 4 (2–5) | |
| PTSD score b | 2 (0–3) | 1 (0–3) | 0.02 |
| PTSD score ≥ 3 c |
85/259 (32.8) |
66/255 (25.9) |
|
Data are reported as median (IQR) or n/N (%).
Abbreviations: COVID‐19, coronavirus disease 2019; PPE, personal protective equipment; PTSD, posttraumatic stress disorder.
Survey items are measured on a 1 to 7 Likert scale (1 = not at all, 4 = somewhat, and 7= very much)
Composite score of 5 items (score range = 0–5).
Three respondents in the initial survey and 7 in the follow‐up did not complete all items of the PTSD score.
This article is being made freely available through PubMed Central as part of the COVID-19 public health emergency response. It can be used for unrestricted research re-use and analysis in any form or by any means with acknowledgement of the original source, for the duration of the public health emergency.
TABLE 3.
Stress levels, burnout, and PTSD scale scores by sex (N = 259)
| Stress and anxiety levels |
Male (n = 130) |
Female (n = 129) |
p‐value |
|---|---|---|---|
| (Initial) How much has the COVID‐19 pandemic affected your stress or anxiety levels in the workplace? | 5 (4–6) | 6 (4.5–6) | 0.001 |
| (Initial) How much has the COVID‐19 pandemic affected your stress or anxiety levels at home (outside of work)? | 5 (4–6) | 5 (4.5–7) | 0.0001 |
| (Follow‐up) Over the past week, how much has the COVID‐19 pandemic affected your stress levels? |
4 (3–5) |
4 (4–5) | 0.008 |
| Self‐reported burnout | |||
| (Initial) Before the pandemic started, to what extent are you experiencing severe, ongoing job stress where you feel emotionally exhausted, burned out, cynical about your work, and fatigued even when you wake up? | 3 (2–3.75) | 3 (2–4) | 0.28 |
| (Initial) Since the pandemic started, to what extent are you experiencing severe, ongoing job stress where you feel emotionally exhausted, burned out, cynical about your work, and fatigued even when you wake up? | 4 (3–5.5) | 5 (3.5–6) | 0.013 |
| (Follow‐up) Over the past week, to what extent are you experiencing severe, ongoing job stress where you feel emotionally exhausted, burned out, cynical about your work, and fatigued even when you wake up? | 4 (2–5) | 4 (2–5) | 0.21 |
| PTSD scale score | |||
| Initial | 1 (0–2) | 2 (1–3) | 0.0001 |
| In follow‐up | 1 (0–2) | 2 (0–3) | 0.005 |
Data are reported as median (IQR). Initial—refers to data obtained during the initial survey conducted March, 2020. Follow‐up—refers to data obtained in this follow‐up survey conducted May 2020.
This article is being made freely available through PubMed Central as part of the COVID-19 public health emergency response. It can be used for unrestricted research re-use and analysis in any form or by any means with acknowledgement of the original source, for the duration of the public health emergency.
Differences in burnout levels over time between men and women are presented in Figure 1. For all three time periods, there were no differences in responses between male and female physicians, with the exception of the middle item, captured on the initial survey; at the beginning of the pandemic, the median stress level reported by men was 4 (3–5.5) and women was 5 (4–6; p = 0.013). Likewise, the PC‐PTSD‐5 scores also differed between men and women, both on the initial survey and in follow‐up, with women scoring higher than men in both time periods (Figure 2). On the five‐item PC‐PTSD‐5 screener, a greater proportion of women scored ≥ 3 (indicating increased risk for PTSD) on the initial survey (43.3% vs. 22.5%; Δ 20.8%, 95% CI 9.3–31.5%) and this discrepancy remained at follow up (34.7% vs. 16.8%; Δ 17.9%, 95% CI = 7.1% to 28.1%; Table S2). In follow‐up, respondents reported being most concerned about the relaxing of social distancing leading to a second wave of cases (median score = 6, IQR = 4–7), increased exposure risk to family members due to work (median score = 5, IQR = 4–6), and risk to the community by patients with unclear diagnoses (median score = 5, IQR = 4–6; Table 2). In spite of these concerns, physicians reported a high level of agreement with being able to order tests for patients suspected of having COVID‐19 at their discretion (median score = 6, IQR = 5–7) and having adequate access to PPE (median score = 6, IQR = 5–6).
FIGURE 1.
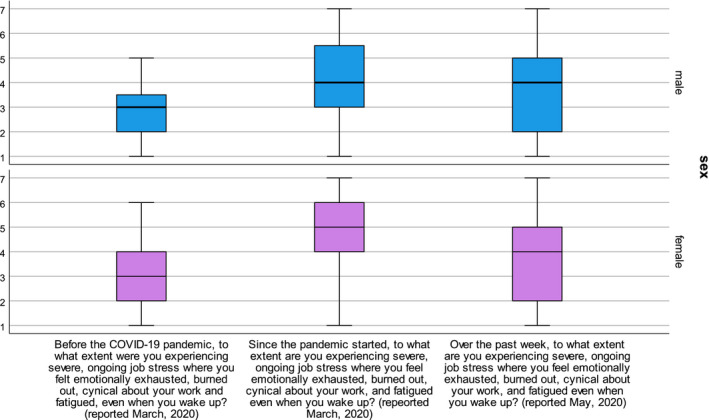
Self‐reported stress and burnout scores (range = 1–7) by men and women. Median value represented by horizontal line, box represents IQR, and whiskers represent range of responses
FIGURE 2.
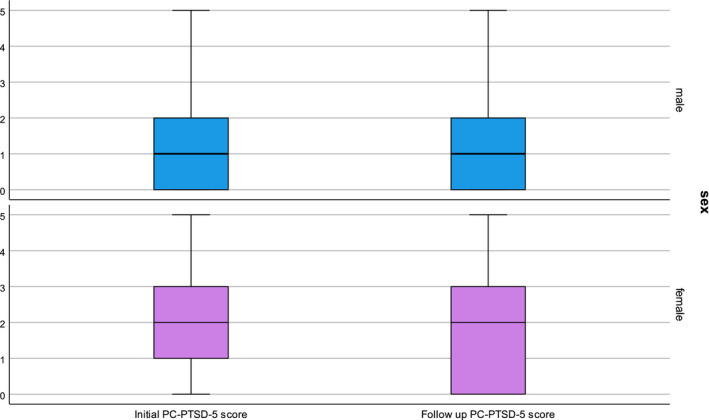
PTSD scale score (range = 0–5) by men and women. Median value represented by horizontal line, box represents IQR, and whiskers represent range of responses
Several questions added to the follow‐up survey to further explore personal stressors had median scores suggesting that they played a contributing role to stress levels. Physicians were “somewhat” worried about colleagues and staff being furloughed or let go to mitigate medical center income loss (median score = 4, IQR = 3–5). Similarly, emergency physicians worried that their own income would be cut due to changes in hospital or emergency department (ED) volumes and shortcomings in income at the medical center (median score = 4, IQR = 2–6). Physicians neither agreed nor disagreed with the statement “I can easily get childcare for my children and assistance for my other dependents so that I can continue to work” (median score = 4, IQR = 4–5) and providers were less likely to agree with the statement “I can easily take leave from work to care for myself and my family members” (median score = 3, IQR = 2–5; Table 2).
More respondents reported changing their behaviors with friends and family as a result of ongoing risk of exposure as a health care worker 88.9% (initial) versus 92.4% (follow‐up; Δ 3.4%, 95% CI = 1.6% to 8.5%). At follow‐up, a reduction in signs of affection with family and friends was the most common behavior change (204/262, 77.9%). However, fewer endorsed a reduction in signs of affection with romantic partners at follow‐up 47.0% (initial) versus 37.4% (follow‐up; Δ 9.6%, 95% CI = 1.1% to 17.8%). When asked to what degree friends and family were treating them differently on a 1 to 7 scale, the response was “somewhat” (median score = 4, IQR = 3–5). The most common changes in the behavior of family and friends included reluctance for close contact (155/262, 59.2%) and expression of concerns about potential exposure (115/262, 44.0%). Two‐thirds of respondents reported that family and friends expressed concerns for their health (Table 4).
TABLE 4.
Responses (N = 262) to survey items inquiring about changes in behavior of respondents and family and friends
| Survey item | Initial survey 7 |
Follow‐up survey |
Percent change Δ % (95% CI) |
|---|---|---|---|
| I have changed my behavior with friends and family as a result of my possible excess exposure as a health care worker during the pandemic | 233 (88.9) | 242 (92.4) | 3.4% (1.6 to 8.5) |
| I have decreased … | |||
| My signs of affection (hugging, kissing) with family and friends | 192 (73.3) | 204 (77.9) | 4.6% (2.8 to 11.9) |
| My signs of affection (hugging, kissing) with romantic partner(s) | 123 (47.0) | 98 (37.4) | 9.6% (1.1 to 17.8) |
| My activities like food preparation for family and friends | 77 (29.4) | 82 (31.5) | 1.9% (–5.9 to 9.7) |
| Dependent care that involves my direct contact | 40 (15.3) | 55 (20.9) | 5.7% (–0.9 to 12.3) |
| I have discussed risks of my potential exposure as a health care worker with family and friends | 215 (82.1) | 213 (81.3) | 0.8% (–5.9 to 7.4) |
| My family and friends have expressed concerns about my health | 173 (66.0) | 176 (67.2) | 1.2% (–6.9 to 9.2) |
| My family and friends are reluctant to be in close contact with me | 108 (41.2) | 155 (59.2) | 17.9% (9.4 to 26.1) |
| My family and friends have avoided activities with me that they used to do | 73 (27.9) | 116 (44.3) | 16.4% (8.2 to 24.3) |
| My family and friends have expressed concerns about their potential exposure because of me | 113 (43.1) | 115 (44.0) | 0.8% (–7.7 to 9.2) |
| My family and friends are showing less affection toward me | 29 (11.1) | 46 (17.6) | 6.5% (0.5 to 12.5) |
| I wear gloves or a mask around the home | 5 (1.91) | 11 (4.2) | 2.3% (–0.8 to 5.6) |
Data are reported as n (%).
This article is being made freely available through PubMed Central as part of the COVID-19 public health emergency response. It can be used for unrestricted research re-use and analysis in any form or by any means with acknowledgement of the original source, for the duration of the public health emergency.
Forced‐entry binomial logistic regression was used to examine the relationship between a self‐reported PC‐PTSD‐5 score ≥ 3 with provider sex, age, level of training (faculty vs. resident/fellow), living circumstances, presence of children under 18 years in the home, location of provider institution, and self‐reported burnout. Of these, only female sex (aOR = 2.48, 95% CI = 1.28 to 4.79) and self‐reported burnout were associated with a PC‐PTSD‐5 score ≥ 3 (Table 5).
TABLE 5.
Factors associated with a PTSD score ≥3
| Factors | aOR (95% CI) |
|---|---|
| Female sex | 2.73 (1.22–6.09) |
| Feeling burned out over the past week due to severe, ongoing job stress a | 2.48 (1.86–3.30) |
| Lives with roommates | 2.80 (0.65–12.02) |
| Faculty (vs. resident/fellow) | 1.60 (0.53–4.79) |
| Age | 1.35 (0.82–2.21) |
| Lives with partner | 0.97 (0.36–2.65) |
| Lives with children < 18 years | 0.83 (0.33–2.10) |
| California (vs. other sites) | 0.69 (0.31–1.54) |
Abbreviation: aOR, adjusted odds ratio; PTSD, posttraumatic stress disorder.
The complete item is: Over the past week, to what extent are you experiencing severe, ongoing job stress where you feel emotionally exhausted, burned out, cynical about your work, and fatigued even when you wake up?
This article is being made freely available through PubMed Central as part of the COVID-19 public health emergency response. It can be used for unrestricted research re-use and analysis in any form or by any means with acknowledgement of the original source, for the duration of the public health emergency.
DISCUSSION
In this first longitudinal survey of emergency physicians during the COVID‐19 pandemic, we found that overall, stress and anxiety decreased over time and median PC‐PTSD‐5 scale scores decreased from 2 to 1 at follow‐up. In terms of ongoing concerns, physicians remained highly worried about patients with unclear diagnoses and how these patients might be exposing others in their communities. At follow‐up, physicians were predominantly worried about a potential second wave due to relaxation of social distancing, which, in retrospect, was prescient for the impending rise in COVID‐19 caseloads the United States was about to experience during the summer of 2020 (Figure 3).
FIGURE 3.
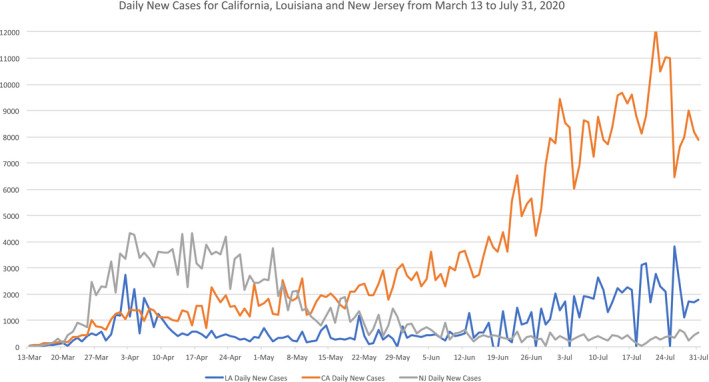
Daily New Cases in California, Louisiana, and New Jersey from March 13 to July 31, 2020
The reduction in stress levels, we believe, was in part due to improvements in PPE and COVID‐19 testing availability, both of which were major concerns in the initial survey. By April 2020, PPE shortages were well documented worldwide, with over 50% of health care workers reporting at least one standard item of PPE unavailable and 30% reporting reuse of single‐use PPE. 11 In the United States, nurses reported that only 24% of employers had sufficient PPE stock on hand to protect staff in case of a rapid surge in patients with possible coronavirus infections. 12 By May, the peaks in caseloads on the east coast had passed and only a few areas in the United States were dealing with COVID‐19 surges.
Overall, stressors at the workplace improved; however, the effects of social distancing measures intensified. Most respondents (~90%) reported that they had decreased signs of affection with family and friends at both study periods. In follow‐up, more physicians reported that family and friends were reluctant to be in close contact with them and were avoiding activities that they used to do together. These findings are concerning, because prior literature has shown that health care workers with increased levels of social support show lower levels of depression, anxiety, stress, and burnout. 13 Adequate social support has also been linked with resilience—an individual's capacity to deal with significant adversity and respond with quick recovery. In a study of Chinese health care workers during the COVID‐19 pandemic, Hou et al. 14 demonstrated that the relationship between resilience and mental health is stronger among young adults compared to older adults. In younger adults, mental health is more influenced by social interactions and relationships with others, whereas the mental health of older adults is thought to be more dependent on generativity, i.e., contributions to society and the next generation via work and child‐rearing. 14 , 15 These findings should raise concerns for the mental health of our trainees and younger physicians, because they may be more likely to suffer negative effects from social isolation than more senior practitioners. Practical solutions to address these concerns may include practitioner bereavement rounds, strict protection of “off time” where providers remain free from patient care and administrative duties, and encouragement for practitioners to provide honest feedback about the stressors they face. 16 The latter could be achieved through an anonymous hotline system within the health care system, where physicians can voice concerns without the fear of reprisal. To maximize effectiveness, leadership needs to respond proactively to feedback in a timely manner. 17
High levels of perceived stress, anxiety, posttraumatic stress symptoms, and depression during infectious outbreaks have been well documented in health care workers. 1 , 5 , 6 , 18 , 19 , 20 , 21 Our findings mirror these results. Almost one‐third of respondents met risk levels for PTSD, both at initial survey and at follow‐up (33% and 26%, respectively). A greater proportion of women had PC‐PTSD‐5 scores ≥ 3 compared to men at both the initial (43% vs. 23%) and the follow‐up surveys (35% vs. 17%). Even after we controlled for other demographic and social factors, female sex and burnout were the only factors associated with a PC‐PTSD‐5 score ≥ 3. Others have documented similar associations between female sex and depression, anxiety, and distress in studies of health care workers during the COVID‐19 pandemic. 3 , 5 , 6
In developing our follow‐up survey, we attempted to elucidate potential stressors that may disproportionately affect women. At both time points, a greater proportion of women emergency physicians self‐reported PTSD level symptoms compared to men. Yet, a critical question remains: why? We suspect that women may bear more of the burden of childcare, at‐home schooling, and dependent care while maintaining active careers. The health care sector has some of the highest childcare obligations in the United States, with 29% of the health care workforce needing to provide care for children age 3 to 12 years. 22 Concerns have already been raised about how school closures could lead to more female health care worker absenteeism, with one model estimating that a 4‐week closure of all schools in the United States would lead to a reduction of 6% to 19% of key health care personnel. 23
In a similar vein, others have postulated that the COVID‐19 pandemic will further exacerbate the gender gap found in academic medicine. Prior to the pandemic, women in academic medicine spent 8.5 more hours per week on parenting and domestic tasks than their male peers. 24 Early examination of manuscript submissions during the pandemic reveal a marked gender gap, with a decrease in female first authorship. 25 , 26 The investigators surmised that increased demands on women, many of which were unanticipated or quickly evolved, forced them to place their academic careers on hold while attending to more pressing domestic needs. While these findings are specific to academic physicians and their scholarly productivity, one can easily extend these findings to all female physicians who experienced a similar explosion of responsibilities at home. 27 By recognizing the mental health sequelae, as well as the clear gender gap as pertains to PTSD and decreased productivity, potential solutions to these challenges may be developed.
LIMITATIONS
The two main limitations are our response rate of 61.5% in this follow‐up sample and the differing phases of the pandemic for the various sites during the study period. For the former, we attribute our lower response rate due to typical factors including the use of email for the survey, potentially increased clinical workload or other duties of health care providers, and our inability to provide an incentive in this unfunded study. Despite these limitations, our physician enrollment was among the highest and our response rate was on par with or higher than other COVID‐19 investigations of health care workers. 1 , 3 , 11 , 28 Furthermore, numerous articles omit response rates or note that they are lacking because of an unknown baseline population N. 5 , 6 The other limitation may have been driven by the multicenter nature of this investigation, normally considered a strength. By early May, New Jersey's peak was waning and Louisiana's first, less severe peak was also resolving. California sites experienced a minor hump in new COVID‐19 cases in March (the time of the initial survey) but these continued to increase throughout May, with a rapid rise in June. Thus, it is possible that our follow‐up survey assessed health care workers at three different pandemic periods: post peak (NJ), interim peak (LA), and pre–second peak of COVID‐19 cases (CA; Figure 3). Finally, 18 respondents did not provide a viable follow‐up email address. If these 18 respondents are excluded, our response rate was 262/408 (64.2%). In spite of these limitations, we believe that our real‐time assessments remain superior to postpandemic stress assessments due to the high potential for recall bias.
A lack of baseline stress, burnout and PTSD measures from before the pandemic is also problematic. There are little data about prepandemic stress levels of health care providers—even with other, prior pandemics, where increased stress levels of men and women are reported. 18 , 19 We attempted to overcome this limitation by asking respondents what they believe their stress and burnout levels were prior to the COVID‐19 pandemic in our initial survey, but fully acknowledge that these responses may have been affected by recall bias. Finally, we noted a discrepancy between our median burnout stress scores and PC‐PTSD‐5 screener ≥ 3 scores. At follow‐up, female physicians had higher stress/anxiety scores and median PC‐PTSD‐5 scores than men, but there was no difference in median burnout scores. We are unsure why this discrepancy exists. It is possible that our burnout question was too limited in scope, focusing only on “severe, ongoing job stress” as opposed to all stressors, including those at home. We believe that there were factors that may have affected women to a greater degree than men that we were unable to capture in our follow‐up survey. To address this, we a priori made our follow‐up stress question more open‐ended by not specifying work‐ versus home‐related stress. The higher self‐reported stress level for women at follow‐up was subtle as demonstrated in Table 3.
The PC‐PTSD‐5 screener appeared to be more sensitive in assessing distress symptoms in our cohort, with higher median scores and a greater proportion of high scores (≥3) in women when compared to men. The reason for this difference may be an actual increase in trauma symptoms, due to COVID‐19, in women, or possible limitations in the PC‐PTSD‐5 screener scale. The screener may be too sensitive in women, overestimating PTSD levels, possibly due to measurement error induced by a scale validated on a mostly male veteran sample. 9 Alternatively, the screener may be performing appropriately, because sex differences in PTSD are well established, with a 2:1 sex ratio favoring women. 29 The original, four‐item PC‐PTSD screener was noted as one of the best‐performing screeners in a systemic review of 15 PTSD screening instruments and has been used in diverse populations. 30 , 31 Because of its brevity and ease in administration, the revised PC‐PTSD‐5 was used in our investigation and has been used by others during the COVID‐19 pandemic. 32 , 33 , 34 In a recently published study conducted on the general public from 20 countries 16.4% of women and 17.7% of men screened positive on the PC‐PTSD‐5. 32 Currently, a cohort study of stressors, coping, and symptoms of adjustment disorder in the course of the COVID‐19 pandemic is being undertaken in 10 European countries utilizing the PC‐PTSD‐5. 34 We anticipate that these findings will contribute to ours in the assessment of stressors during the COVID‐19 pandemic.
CONCLUSIONS
We demonstrated an improvement in stress and PC‐PTSD‐5 scores over time in the first longitudinal study of emergency physicians during the COVID‐19 pandemic. A greater proportion of female emergency medicine physicians had PC‐PTSD‐5 screener scores ≥ 3 compared to men; however, our findings did not clearly delineate the cause. Given the ongoing pandemic, further attention should be given to elucidate why and how some physicians are more impacted by the pandemic stressors than others, particularly women and residents. Additional study may play an increasing role in maintaining physician mental health, particularly if the COVID‐19 pandemic fails to abate in the United States.
CONFLICT OF INTEREST
Richelle J. Cooper receives grant support from PCORI as site PI for a multicenter EM palliative care study and receives support from the American College of Emergency Physicians for her role as Deputy Editor and Methodology and Statistics Editor for Annals of Emergency Medicine. Brian W. Roberts reports grant money to Rowan University from NHLBI for investigator‐initiated research titled “Post‐resuscitation PaCO2 and Neurological Outcome after Cardiac Arrest.” The other authors have no potential conflicts to disclose.
AUTHOR CONTRIBUTIONS
Robert M. Rodriguez and Elissa S. Epel conceived the study, and all authors contributed to the survey instrument design and content and assisted with data collection. Robert M. Rodriguez, Brigitte M. Baumann, and Remi Frazier managed the data, including quality control. Brigitte M. Baumann, Robert M. Rodriguez, Richelle J. Cooper, Brian W. Roberts, and Elissa S. Epel provided statistical advice on study design and analyzed the data. Brigitte M. Baumann, Richelle J. Cooper, and Robert M. Rodriguez drafted the manuscript and all authors contributed substantially to its revision. Brigitte M. Baumann takes responsibility for the paper as a whole.
Supporting information
Data Supplement S1. Supplemental material.
ACKNOWLEDGMENTS
We thank Ashley Mason, PhD, and the UCSF Stress Network for their assistance with development of the survey instrument.
REFERENCES
- 1. Du J, Dong LU, Wang T, et al. Psychological symptoms among frontline healthcare workers during COVID‐19 outbreak in Wuhan. Gen Hosp Psychiatry 2020;67:144‐145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Zhang W‐R, Wang K, Yin LU, et al. Mental health and psychosocial problems of medical health workers during the COVID‐19 epidemic in China. Psychother Psychosom. 2020;89:242‐250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Lai J, Ma S, Wang Y, et al. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw Open. 2020;3(3):e203976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Chew NW, Lee GK, Tan BY, et al. A multinational, multicentre study on the psychological outcomes and associated physical symptoms amongst healthcare workers during COVID‐19 outbreak. Brain Behav Immun. 2020;88:559‐565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Rossi R, Socci V, Pacitti F, et al. Mental health outcomes among frontline and second‐line health care workers during the coronavirus disease 2019 (COVID‐19) pandemic in Italy. JAMA Netw Open. 2020;3:e2010185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Elbay RY, Kurtulmuş A, Arpacıoğlu S, Karadere E. Depression, anxiety, stress levels of physicians and associated factors in Covid‐19 pandemics. Psychiatry Res. 2020;290:113130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Rodriguez RM, Medak AJ, Baumann BM, et al. Academic emergency medicine physicians’ anxiety levels, stressors, and potential stress mitigation measures during the acceleration phase of the COVID‐19 pandemic. Acad Emerg Med. 2020;27(8):700‐707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Shanafelt T, Ripp J, Trockel M. Understanding and addressing sources of anxiety among health care professionals during the COVID‐19 pandemic. JAMA. 2020;323(21):2133‐2134. [DOI] [PubMed] [Google Scholar]
- 9. Prins A, Bovin MJ, Smolenski DJ, et al. The Primary Care PTSD Screen for DSM‐5 (PC‐PTSD‐5): development and evaluation within a Veteran primary care sample. J Gen Intern Med. 2016;31:1206‐1211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. von Elm E, Altman DG, Egger M, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Ann Intern Med. 2007;147(8):573‐577. [DOI] [PubMed] [Google Scholar]
- 11. Tabah A, Ramanan M, Laupland KB, et al. Personal protective equipment and intensive care unit healthcare worker safety in the COVID‐19 era (PPE‐SAFE): an international survey. J Crit Care. 2020;59:70‐75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. National Nurses United COVID‐19 survey . 2020. Accessed April 29, 2020. https://act.nationalnursesunited.org/page/‐/files/graphics/0320_NNU_COVID‐19_SurveyResults_Updated_031920.pdf
- 13. Jenkins R, Elliott P. Stressors, burnout and social support: nurses in acute mental health settings. J Adv Nurs. 2004;48(6):622‐631. [DOI] [PubMed] [Google Scholar]
- 14. Hou T, Zhang T, Cai W, et al. Social support and mental health among health care workers during coronavirus disease 2019 outbreak: a moderated mediation model. PLoS One. 2020;15(5):e0233831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Slater CL. Generativity versus stagnation: an elaboration of Erikson's adult stage of human development. J Adult Dev. 2003;10(1):53‐65. [Google Scholar]
- 16. Kiser SB, Bernacki RE. When the dust settles: preventing a mental health crisis in COVID‐19 clinicians. Ann Intern Med. 2020;173(7):578‐579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Dzau VJ, Kirch D, Nasca T. Preventing a parallel pandemic ‐ a national strategy to protect clinicians’ well‐being. N Engl J Med. 2020;383(6):513‐515. [DOI] [PubMed] [Google Scholar]
- 18. Lin CY, Peng Y, Wu YH, et al. The psychological effect of severe acute respiratory syndrome on emergency department staff. Emerg Med J. 2007;24:12‐17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Chan AO, Huak CY. Psychological impact of the 2003 severe acute respiratory syndrome outbreak on health care workers in a medium size regional general hospital in Singapore. Occup Med. 2004;54(3):190‐196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Luo M, Guo L, Yu M, Jiang W, Wang H. The psychological and mental impact of coronavirus disease 2019 (COVID‐19) on medical staff and general public – A systematic review and meta‐analysis. Psychiat Res. 2020;291:113190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Johnson SU, Ebrahimi OV, Hoffart A. PTSD symptoms among health workers and public service providers during the COVID‐19 outbreak. PLoS One. 2020;15(10):e0241032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Bayham J, Fenichel EP. Impact of school closures for COVID‐19 on the US health‐care workforce and net mortality: a modelling study. Lancet Public Health. 2020;5(5):e271‐e278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Lempel H, Epstein JM, Hammond RA. Economic cost and health care workforce effects of school closures in the U.S. PLoS Curr. 2009;1:RRN1051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Jolly S, Griffith KA, DeCastro R, Stewart A, Ubel P, Jagsi R. Gender differences in time spent on parenting and domestic responsibilities by high‐achieving young physician‐researchers. Ann Intern Med. 2014;160:344‐353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Vincent‐Lamarre P, Sugimoto CR, Larivière V.The Decline of Women’s Research Production During the Coronavirus Pandemic. Nature Index. 2020. Accessed August 9, 2020. https://www.natureindex.com/news‐blog/decline‐women‐scientist‐research‐publishing‐production‐coronavirus‐pandemic.
- 26. Andersen JP, Nielsen MW, Simone NL, Lewiss RE, Jagsi R. COVID‐19 medical papers have fewer women first authors than expected. Elife. 2020;9:e58807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Madsen TE, Dobiesz V, Das D, et al. Unique Risks and Solutions for Equitable Advancement during the Covid‐19 Pandemic: Early Experience from Frontline Physicians in Academic Medicine. NEJM Catal Innov Care Deliv. 2020. 10.1056/CAT.20.0268. [DOI] [Google Scholar]
- 28. Shechter A, Diaz F, Moise N, et al. Psychological distress, coping behaviors, and preferences for support among New York healthcare workers during the COVID‐19 pandemic. Gen Hosp Psychiatry. 2020;66:1‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Christiansen DM, Berke ET. Gender‐ and sex‐based contributors to sex differences in PTSD. Curr Psychiatry Rep. 2020;22(4):19. [DOI] [PubMed] [Google Scholar]
- 30. Spoont MR, Williams JW, Kehle‐Forbes S, et al. Does this patient have posttraumatic stress disorder?: Rational clinical examination systematic review. JAMA. 2015;314(5):501‐510. [DOI] [PubMed] [Google Scholar]
- 31. Freedy JR, Steenkamp MM, Magruder KM, et al. Post‐traumatic stress disorder screening test performance in civilian primary care. Fam Pract. 2010;27(6):615‐624. [DOI] [PubMed] [Google Scholar]
- 32. Kar N, Kar B, Kar S. Stress and coping during COVID‐19 pandemic: Result of an online survey Psychiatry Res. 2020;295:113598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Feng Z, Xu L, Cheng P, et al. The psychological impact of COVID‐19 on the families of first‐line rescuers. Indian J Psychiatry. 2020;62(Suppl 3):S438‐S444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Lotzin A, Acquarini E, Ajdukovic D, et al. Stressors, coping and symptoms of adjustment disorder in the course of the COVID‐19 pandemic ‐ study protocol of the European Society for Traumatic Stress Studies (ESTSS) pan‐European study. Eur J Psychotraumatol. 2020;11(1):1780832. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Supplement S1. Supplemental material.


