Abstract
Aims and objectives
To explore the impact of the COVID‐19 pandemic on alcohol and other drug nurses providing treatment for individuals presenting with problematic alcohol and other drug use.
Background
COVID‐19 has caused disruption to contemporary health service delivery, including alcohol and other drug treatment. Provisional research on drug and alcohol consumption patterns shows changes attributable to the pandemic, with implications for service delivery. Research also indicates the impact of the pandemic on healthcare staff is significant, leading to workforce challenges that threaten care provision.
Design
Qualitative descriptive study design.
Methods
Data were collected using semi‐structured, individual telephone interviews with practising alcohol and other drug nurses from Australia and New Zealand (n = 19). COREQ reporting guidelines were used.
Results
After thematic analysis, three key themes emerged: ‘No room at the inn: Changes to service delivery due to COVID‐19’, ‘We are providing care to a very vulnerable group of people: Consumer factors during COVID‐19’ and ‘Personally, we were very, very stressed: Workforce factors due to COVID‐19’.
Conclusions
The findings from this study indicate that the impact of the pandemic was felt by alcohol and other drug nurses, services and healthcare consumers alike. The experiences of alcohol and other drug nurses through the COVID‐19 pandemic need further exploration both to ensure workforce sustainability and that disruptions to alcohol and other drug services do not occur in future outbreaks of communicable disease.
Relevance to clinical practice
COVID‐19 has had a profound effect on nurses in all settings, and these effects are likely to be felt for some time after the pandemic: nursing specialties require support to ensure ongoing workforce sustainability and well‐being of nursing staff. All nurses need to be aware of changes to alcohol and other drug use during the pandemic and screen healthcare consumers accordingly.
Keywords: alcohol and other drug (AOD) nursing, COVID‐19, delivery of health care, pandemic, workforce
What does this paper contribute to the wider global clinical community?
The COVID‐19 pandemic has caused significant disruption to many areas of healthcare, including nursing.
Many nursing specialities have experienced challenges during the COVID‐19 pandemic, including nurses being redeployed to other areas considered of greater need and changes in the way services are delivered.
There is an urgent need to investigate the workforce impacts of COVID‐19 on nursing, particularly when considering older, experienced nurses who may leave the workforce due to their susceptibility to COVID‐19 infection.
1. INTRODUCTION
The COVID‐19 pandemic has caused disruption to healthcare services, including alcohol and other drug (AOD) treatment services. Social distancing, lockdown, ‘stay at home’ orders and other measures designed to reduce the spread of COVID‐19 have had a pronounced impact on the way consumers of AOD treatment services are able to access care for problematic alcohol and other drug use (Dunlop et al., 2020). The implications of post‐pandemic efforts to prevent the recurrence of widespread COVID‐19 infection will likely have wide ranging effects on AOD settings that provide services such as harm reduction (López‐Pelayo et al., 2020). Changes in the availability, supply methods and usage patterns of substances, for example due to border closure in the case of illicit substances or moves to home delivery services for alcohol, are likely to have wide‐reaching implications beyond the pandemic (Colbert et al., 2020; United Nations, 2020; Voce et al., 2020).
Generally, nurses have been portrayed as the healthcare ‘face’ of the COVID‐19 pandemic, conducting testing for the virus, providing care for those who contract COVID‐19 and at times contracting the virus themselves (Fernandez et al., 2020). AOD nurses, also known as addiction nurses, are a significant profession in the overall AOD workforce composition, performing key roles including medication administration, mental and physical health monitoring in a wide variety of settings where problematic AOD use is encountered (Searby & Burr, 2020; Skinner et al., 2020).
The aim of this study is the exploration of the impact of the COVID‐19 pandemic on AOD nurses providing treatment for individuals presenting with problematic AOD use. We sought to use qualitative description to explore the rich narratives of AOD nurses working in AOD treatment settings throughout the course of the pandemic. Little data exist on the AOD nursing workforce, and to our knowledge, this is the first study exploring solely the experiences of AOD nurses during the COVID‐19 pandemic.
2. BACKGROUND
Australia experienced initial cases of COVID‐19 in January 2020, with spread of the disease limited due to the geographic nature of the country and the fact that Australia is an island, with strict border controls limiting the intake of potentially infected individuals from other countries (Adekunle et al., 2020; Tan et al., 2020). New Zealand followed experiencing initial cases during February 2020 (Jefferies et al., 2020). COVID was initially described as a threat to intensive care units and respiratory settings, leading to concerns that, left unchecked, the COVID‐19 infection would quickly overwhelm hospitals and the availability of suitably qualified clinical staff (Litton et al., 2020). Beyond these settings, however, there has been little research conducted on the impact on healthcare settings not directly related to detecting and treating COVID‐19.
As at June 2020, Australia had recorded 7277 cases and 102 deaths; comparisons with case rates from Canada, Sweden and the United Kingdom indicate that if Australia had a similar case rate, COVID‐19 cases would be between 8–14 times higher, with between 5000–14,000 extra deaths attributable to the pandemic (Australian Institute of Health & Welfare, 2020b). However, not long after this comparison the state of Victoria experienced a ‘second wave’ of community acquired COVID‐19 infections, with Australia peaking at an average of 525 infections per day. The outbreak also reached residential aged care facilities in Melbourne and was responsible for 678 deaths to December 2020 (Australian Government Department of Health, 2020a, 2020b). Despite the second wave, Australia's COVID‐19 outbreak remains much smaller than the United States, United Kingdom and most of Europe (Sorci et al., 2020). New Zealand used a strict lockdown regime and closed borders to control the spread of the virus, with 1503 cases and 22 deaths reported to May 2020 (Jefferies et al., 2020).
A survey examining the impact of COVID‐19 on nursing and medical staff in Wuhan, China (the site of the initial mass outbreak of the virus), surveyed 994 nursing and medical staff, finding a high number reporting mental health disturbances related to working during the pandemic (Kang et al., 2020). A further study surveyed 1257 healthcare workers across several health regions in China (Lai et al., 2020), finding high rates of symptoms of depression (50.4%) and anxiety (44.6%). Studies have also found somatic disturbances related to stress associated with the pandemic, including insomnia, anxiety and headaches (Chew et al., 2020). These results indicate that the effects of the pandemic go beyond healthcare availability and have a direct impact on the well‐being of nursing staff.
As the pandemic continues, there is real concern that a ‘second pandemic’ could occur due to the psychological impact experienced by both staff and healthcare consumers, as well as family members (Choi et al., 2020). Concerns have been expressed that the mental health impact of the pandemic could also be exacerbated by job losses, extended lockdowns, isolation from family and friends in distant regions and economic downturns (Holmes et al., 2020; Torales et al., 2020). A large‐scale (n = 53,351), longitudinal cohort study conducted by Pierce et al., (2020) in the United Kingdom found an increase in mental distress in population groups most directly impacted by the lockdown, including those who lived with young children; the study reports that reduced incomes and working hours due to pandemic related shutdowns were prominent in these groups.
Beyond the mental health concerns associated with the pandemic and lockdowns, there have also been concerns regarding increased alcohol consumption, often attributed to the stresses outlined above (Callinan et al., 2020). The Australian Institute of Health and Welfare (2020a) describes an increase in spending on take away alcohol, and of those who report increasing alcohol consumption, this consumption is often attributed to boredom and isolation incurred during lockdowns. The Australian Bureau of Statistics (2020) surveyed 1022 participants early in the pandemic (late April to early May 2020), with 14.4% reporting an increase in their alcohol consumption. The Australian National Wastewater Monitoring programme reported record high drug consumption of methamphetamine and heroin in regional Australia, and capital city consumption of cocaine, cannabis and nicotine during the COVID‐19 pandemic (Australian Criminal Intelligence Commission, 2020).
3. STUDY AIM
The findings in the literature indicate a concerning situation, whereby mental ill health and alcohol and other drug consumption could increase both during the continuation of the pandemic, and for some time after COVID‐19 viral transmission has been controlled. Additionally, the stress and psychological disturbance on nursing staff is essential to explore, both for individual well‐being and workforce sustainability. Both factors have informed the aim of this study: the exploration of the impact of the COVID‐19 pandemic on AOD nurses providing treatment for individuals presenting with problematic AOD use.
4. METHOD
4.1. Design
The methodological design of this study was qualitative description, an inductive qualitative approach described as being well suited to explore participant perception and experience of phenomena, and to provide a description of events that is reflective of the participant's own language (Neergaard et al., 2009; Sandelowski, 2010). Semi‐structured interviews were conducted with 19 AOD nurses across Australia and New Zealand, and data were analysed using Braun and Clarke’s (2006) method of thematic analysis. This project was guided by the Consolidated Criteria for Reporting Qualitative Research (COREQ) checklist (Appendix S1) (Tong et al., 2007).
4.2. Ethical approval
Prior to the commencement of data collection, ethical approval for this study was obtained from the relevant University ethical review board. Participants were read a verbal consent script which required agreement before interviews commenced. All identifying information, such as names and workplaces, has been removed to protect participant confidentiality.
4.3. Data collection
Sampling for this project was conducted using purposive sampling. This methodology was used to ensure that participants had experience of the phenomenon of investigation, being the impact of COVID‐19 on their work as AOD nurses (Palinkas et al., 2015). Potential participants were invited to take part in the study by using targeted email and social media posts, distributed to the mailing list and social media connections of the national peak body for AOD nurses, the Drug and Alcohol Nurses of Australasia (DANA). Inclusion criteria, outlined on the recruitment materials, were (a) nurses currently registered with the Australian Health Practitioner Registration Agency (AHPRA) and (b) currently working in a recognised AOD nursing role.
Participants who wished to participate accessed a Qualtrics survey page where they were able to provide a contact email address to arrange an interview. This page also contained a link to download the participant information form. A trained research assistant (DB, female) contacted participants to arrange interview times via email.
Individual, in‐depth semi‐structured interviews were conducted via telephone in July and August 2020. A semi‐structured interview guide was developed from emerging literature on the healthcare response to COVID‐19 and existing literature exploring disaster preparedness in the nursing workforce (Wong et al., 2010; World Health Organisation & International Council of Nurses, 2009). The interview guide was designed to probe responses in respect to potential impacts of physical distancing or lockdowns, and how these impacts affected consumers of the AOD treatment services in question. Demographic information was also collected to enable an overview of the demographic profile of study participants. This information is summarised in Table 1.
TABLE 1.
Participant demographic profile
| Participant number | Gender | Role | Setting | State |
|---|---|---|---|---|
| 1 | Female | Clinical nurse | Pharmacotherapy clinic | New South Wales |
| 2 | Female | Clinical nurse | Residential AOD | New Zealand |
| 3 | Female | Manager | Aboriginal Medical Service | New South Wales |
| 4 | Male | Nurse practitioner | Consultation‐liaison/prison | New South Wales |
| 5 | Female | Clinical nurse consultant | Substance use in pregnancy and parenting service | New South Wales |
| 6 | Female | Clinical nurse consultant | Community health service | New South Wales |
| 7 | Female | Clinical nurse | Mental health service | ACT |
| 8 | Female | Clinical nurse | Youth health service | New South Wales |
| 9 | Female | Clinical nurse consultant | Tertiary hospital | New South Wales |
| 10 | Female | Clinical nurse | Tertiary hospital | Western Australia |
| 11 | Female | Manager | Pharmacotherapy clinic | New South Wales |
| 12 | Female | Clinical nurse consultant | Consultation‐liaison | New South Wales |
| 13 | Female | Nurse practitioner | Tertiary hospital | New South Wales |
| 14 | Female | Clinical nurse | Pharmacotherapy clinic | New South Wales |
| 15 | Male | Nurse practitioner (transitional) | Consultation‐liaison | New South Wales |
| 16 | Female | Clinical nurse | Pharmacotherapy clinic | New South Wales |
| 17 | Female | Clinical nurse | Inpatient withdrawal unit | ACT |
| 18 | Female | Clinical nurse | Youth health service | Queensland |
| 19 | Female | Clinical nurse | Medically supervised injecting facility | New South Wales |
A trained research assistant (DB, female), who has experience conducting interviews for similar qualitative projects, conducted the interviews via telephone. Interviews were recorded using a call‐recording tool to enable accurate transcription, with the interviewer making extensive notes which allowed her to capture perspectives of the interview as it occurred (Mealer & Jones, 2014). Interviews ranged between 32–47 min in duration. Interviews were conducted beyond theoretical data saturation to capture responses from a wide geographic area. Recordings were de‐identified and transcribed verbatim, with both recordings and transcripts checked regularly by the lead author (AS, male) to ensure data quality. Regular meetings were held between the research team to both discuss emergent themes and address any issues encountered in the interview process. All interviews were uploaded to the NVivo software program for analysis and coding.
4.4. Analysis
Data analysis was conducted by both members of the research team, based on Braun and Clarke's (2006) method of thematic analysis, which involves a six‐step process of finding themes in qualitative data: familiarisation with data, generating initial codes, searching for themes, reviewing themes, defining and naming themes and, finally, producing the report. Both authors independently became familiar with the data through reading transcripts and revisiting audio recordings, developing a preliminary coding matrix. To ensure inter‐rater reliability and agreement in codes developed, preliminary themes were reviewed between researchers and coding decisions explained and justified following the methods of Hemmler et al., (2020). The authors then completed the following phases (searching, reviewing, defining and naming themes, and preparing the report) cooperatively to achieve consensus and agreement of themes and subthemes. The preliminary coding matrix was regularly revised as new themes emerged during analysis of further interviews during the cooperative process. The coding tree is described in Figure 1.
FIGURE 1.
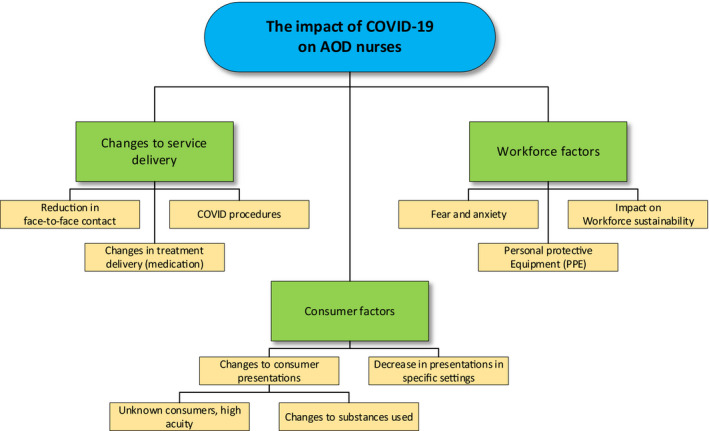
Coding tree
5. FINDINGS
A total of 19 AOD nurses took part in this study, 18 from Australia and one from New Zealand. Participants were mostly female (n = 17, 89.5%) and residing in the Australian state of New South Wales (n = 14, 74%). Participants reported a wide range of roles and settings; however, most (n = 10, 53%) worked as clinical nurses. Three parent themes emerged during the analysis of the data: changes to service delivery, factors associated with consumers and factors associated with the workforce.
5.1. ‘No room at the inn’: Changes to service delivery due to COVID‐19
As the COVID‐19 pandemic emerged as a threat to health service delivery in Australia and New Zealand, many participants reported significant changes to the delivery of AOD treatment services. Largely, these changes were described as procedures that were implemented to meet guidelines for physical distancing or the use of personal protective equipment (PPE). Participants also reported the incorporation of COVID testing procedures into their treatment service, an initiative that was said to be designed to have marginalised consumers receive testing in the service as opposed to attending a designated testing clinic:
The dosing staff [in the pharmacotherapy clinic] were doing the testing. Each patient that came in got offered the opportunity to have a test. (Participant 13)
Further procedures were incorporated to reduce the perceived risk of transmission of COVID‐19, including temperature checks and focussed questioning to ascertain whether consumers had been exposed to the virus. In addition, consumer residential locations were also considered, as indicated in this example from an inpatient unit:
We were initially restricted to [Australian Capital Territory] clients… we'd ring them the night before to check that they hadn't been in contact with anyone or had any symptoms or signs and then on admission we would wear masks and goggles, check their temperature outside, ask the questions again and then bring them down into the unit for admission. (Participant 17)
Even though participants described that these procedures were encountered over most healthcare settings in Australia and New Zealand, participants noted that it was often the nursing staff who remained on‐site to conduct these procedures. This was often due to the roles nursing staff undertook being considered essential, such as administering medication and providing care for mental and physical ill health:
The counsellors are doing pretty much all phone contact. That is not the nature of nursing, you can't really do nursing via a phone so that hasn't changed our model. But more broadly, it has changed the model of drug and alcohol services. (Participant 12)
Participants also reported a reduction in the face‐to‐face contact that had previously been the mainstay of contemporary AOD treatment services. A shift in focus was noted, where the provision of treatment for problematic AOD use made way for responding to the potential influx of healthcare consumers presenting with COVID‐19:
Our local hospitals… basically put a big ‘no room at the inn’ sign up. When you are expecting a whole influx of patients in a pandemic the capacity to accept alcohol detox patients went out the window. (Participant 15)
The lack of face‐to‐face contact had substantial impact on the delivery of AOD treatment, especially where opiate substitution therapy (OST) involving methadone and buprenorphine was concerned. Of the participants who worked in pharmacotherapy services, all reported that there had been changes made to the delivery of OST, predominantly around the provision of ‘take away’ doses. Take away dosing, where consumers effectively take pre‐prepared future doses offsite for later unsupervised administration (Ritter & Natale, 2005), marked a shift from supervised dosing that may not have been considered prior to COVID‐19:
A lot of people were given takeaway doses, even people that previously would have been too high risk. Patient contact was just wound back at every possible turn. (Participant 1)
Reports of the success of this approach from participants were mixed. Although some reported that the shift to take away doses worked well for consumers, others described consumers feeling the loss of structure that occurred with supervised dosing, and issues such as costs associated with moving dosing to a private pharmacy. Despite many participants reporting consumers moving to take away pharmacotherapy dosing, many comments reflected a perception that the risk for some consumers was too high for this approach:
Then there were the people that couldn't go anywhere, that have to daily dose here, they’re too chaotic, they’re using ice [methamphetamine] every day, they’re too unstable, the risks are too high. (Participant 11)
Takeaway dosing was also used as a strategy if consumers had to quarantine due to either waiting for test results or recording a positive COVID‐19 test. One participant reported that this approach was part of a strategy in managing confirmed COVID‐19 cases in consumers:
We had a store of takeaways ready for every single client who comes to our clinic, so that if in the event they came in and they were symptomatic, they needed to be tested and they needed to isolate, we would be able to dose them and give them a handful of takeaways. (Participant 6)
Another reported strategy was moving consumers to the long‐acting injectable buprenorphine formulation. Participants reported an urgency to implement this treatment in the wake of the initial COVID outbreak in New South Wales; it was felt that this was a key strategy to reduce face‐to‐face contact, and a way to mitigate the risks of treatment if isolation strategies were needed to prevent the spread of the virus:
We had one client who got COVID, he had been into have a look at the Ruby Princess [cruise ship] and he managed to get COVID. He had the injection [buprenorphine] two days beforehand. So, he could go into isolation… if it had been methadone, you know we would have had to home deliver. (Participant 11)
Although participants reflected that the consumers who transferred to the long‐acting injectable were largely happy with their decision to do so, there were some barriers to rapid implementation in some healthcare services, as outlined in this example:
The Department announced, ‘You need to get everybody on the [long acting injectable] as quickly as possible because then you’ll have less people coming to the clinic’. We had announced it was coming, but we had been a bit tardy around rolling it out. The reason being that we had a prescriber issue in that we didn't have one. Our prescriber had resigned, and we were utilising a prescriber through telehealth. (Participant 6)
This participant went on to describe the concern that despite the long‐acting injectable being used to reduce face‐to‐face contact, there were some reservations:
Funnily enough after having made that decision to get everybody on the [long acting injectable], one of the [service medical staff] did actually say, ‘Hang on a minute, it might actually cause us more problems if people have to isolate because then staff will have to go into their home to give the injection. It is probably easier if they’re on an oral medication because then you can just deliver it to their front door’. (Participant 6)
Overall, reactions to the reduction in face‐to‐face contact were mixed. Participants in rural areas used telehealth technologies to good effect, describing a significant reduction in travel time, meaning more appointments could be scheduled in a workday. However, most participants were concerned that telehealth appointments did not allow for an adequate therapeutic intervention and impacted on rapport and consumer engagement:
I think once you break that engagement it is very hard to get back. (Participant 5)
5.2. ‘We are providing care to a very vulnerable group of people’: Consumer factors during COVID‐19
During the interview process, participants described several factors related to the consumers of their services. These factors typically concerned changes in the AOD usage patterns of consumers seeking treatment from services during the pandemic. Despite reports of a potential shortage of certain substances (Dietze & Peacock, 2020; Voce et al., 2020), participants observed diverse patterns of use, particularly during lockdowns. Some of these observed patterns of use included shifts in substances used, placing consumers at risk:
There's more overdosing on GHB [gamma hydroxybutyrate]. Methadone overdoses. [Methamphetamine] supply has dropped off and GHB has arisen from that. I've seen clients drinking and then taking GHB on top of that and it's just causing them to be unconscious and needing to be intubated. I have concerns for our cohort. (Participant 1)
Further, participants noted a change in AOD purchasing behaviours related to government financial stimulus provided at the commencement of lockdowns associated with the pandemic:
The government gave handouts… $750, so all of a sudden, it's like, oh wow, you know, not a problem in terms of finances. Some [consumers] used that money and got on the ice [methamphetamine] and there was an increase in ice use, but that seems to have settled down a bit now. (Participant 11)
Alternative methods of obtaining alcohol and other drugs were also noted, particularly concerning alcohol. For example, one participant described an increase in home delivered alcohol, which again caused concern when linked to the government stimulus payments:
We are providing care to a very vulnerable group of people… their drinking or drug use had not ceased but could have possibly increased because now they were getting extra money from the government. And possibly having home delivery straight to their door knowing that alcohol is the number one danger. (Participant 4)
A participant who worked with youth also reported that consumers had been using home delivery to obtain alcohol:
Ordering bottles of alcohol over the internet has become a problem. That is probably the biggest change that I've seen in COVID, is that all of a sudden you can buy alcohol online and you don't need ID. (Participant 9)
In addition to changes in usage patterns observed during the COVID‐19 pandemic, many participants also reported a perceived change in the consumers that were requesting assistance from AOD services. Mostly, participants related this back to the impact of lockdowns, job losses and additional stresses associated with the pandemic, such as home schooling:
We have seen people showing up that we have never seen before, and they're sick. They are having alcohol withdrawal seizures… because with COVID, there has been a whole month of people staying home, they're not working, they’re stressed about money. (Participant 9)
There was a fella who came in just a little bit upset and wanted to see somebody. He'd lost his job as a bricklayer, couldn't pay his mortgage, wife kicks him out and he ended up at a refuge… He came up to the ED and wanted to see someone to talk about it, ended up having a seizure in the waiting room and ended up intubated in ICU for three or four days. He probably would’ve been a little bit upset anyway but because of the pandemic and losing his job and the money, all that has kicked him over the edge and those sorts of really extreme drug and alcohol presentations seem to have really increased in the last couple of months. (Participant 15)
However, some participants did note that AOD use and presentations decreased over the course of the pandemic in specific treatment areas. One participant related this back to a government initiative to provide housing for consumers who were homeless, noting that several ‘regular’ consumers of the service had either ceased or reduced their use:
Probably the biggest change is our numbers have decreased dramatically and a lot of that is because a lot of our clients were homeless and they've all been housed, they’ve all been put up in hotels by the government to prevent the spread of COVID amongst homeless people. (Participant 19)
Additionally, participants described consumers who had effectively gone into an ‘involuntary abstinence’ due to a lack of substances, often leading to a need to purchase substances from unknown sources. This was described as a concern for participants, particularly in respect of the quality or potency of substances and the potential for these to cause harm:
Yeah just some [consumers] were reducing. I think they didn't want to go out so that was their reasoning behind it. Or they’d say the market had closed down so, yeah, they just didn't get enough in town. For us it wasn't so much that that was a choice they made, it was more that, you know, they just couldn't get it. (Participant 8)
For those consumers who did reduce or cease their substance use, positive benefits were noted, as illustrated in the following anecdote:
Some clients did use more and yet other clients found it actually really helped their substance use because they were self‐isolating and they stayed at home and they weren't out and about getting on and everything, they actually did a lot of the repair of their relationships and a lot of work on themselves and their family and a lot of goal setting and things like that. (Participant 8)
5.3. ‘Personally, we were very, very stressed’: Workforce factors due to COVID‐19
The final theme emerging from the qualitative interview process concerned workforce factors, which were mainly related to changes in the workplace necessary to incorporate social distancing, personal protective equipment or a repurposing of services to meet the expected influx of COVID‐19 positive individuals. Several responses around workforce factors also mentioned a degree of fear:
We were attending Emergency Department meetings and they were talking about what they were expecting to see, and that was unnerving for us. We had a few tough days about that. Personally, we were very, very stressed. (Participant 10)
This fear often related to the perceptions of worst‐case scenarios eventuating, which were driven by fear of the unknown and an uncertainty of the duration of the pandemic:
Originally, we were told that this would just be for a couple of weeks and it turned into three months. It is getting to the point that we need to have some stability and we need to start returning to as normal a service as we possibly can. (Participant 5)
Several participants also described a fear of contracting the virus in the workplace, with some going on to report factors that they felt put their consumers, and themselves, at greater risk:
When it first started, I was anxious… a significant proportion of our clients come from a high‐density public housing, and therefore their risk is not insignificant. I was quite worried about that cohort of people, for themselves being infected, but also for us as staff being infected. (Participant 14)
In addition to fear of uncertainty in relation to the pandemic and procedures associated with the prevention of the spread of the COVID‐19 virus, participants also reported ambiguity around the messaging concerning personal protective equipment (PPE). In the early stages of the pandemic, this was often described as confusion around wearing PPE items, such as masks; as the following participant describes, there was an overarching feeling that masks should be preserved for areas considered more important than AOD treatment settings:
PPE was in a significant shortage and they didn't want you to use a lot of PPE because they were really concerned… at that state level, we didn't have adequate supplies. Some nurses were putting on masks and being told no, you’re not allowed to wear that mask here at the moment. If you do, you have to leave. And several of them were sent home for wearing them. (Participant 4)
The perception that PPE needed to be stockpiled also meant participants reported feeling that AOD treatment services were of a lesser need than other healthcare settings:
You're not considered essential like general health is, therefore if this ramps up another level, the only service that will be available is the daily opioid treatment program dosing. The detox facility and everything else will cease to exist and the nurses will be probably be redeployed. (Participant 4)
Redeployment was frequently mentioned during the interview process and was also reported as a key driver of fear in participants. Like many clinicians working in AOD settings, nurses are highly specialised. However, many participants reported that the overarching concept of nurses being generalised and able to work in any setting was communicated to them during the pandemic, leading to much anxiety:
There was some talk that some of our [registered nurses] might get seconded up to the testing clinics but that never eventuated, thankfully. I don't think anyone was very keen on doing that. (Participant 15)
Many participants reinforced this view of redeployment, with interview narratives describing nurses being asked to move to COVID‐19 testing or respiratory settings. The underlying theme of these responses is to discount AOD experience and move nurses to ‘real nursing’ settings, in this case, responding to the pandemic:
They're thinking half the staff are going to go down with COVID and they're looking at you going okay, what can you do, do you have any children, do you have any dependants, where can you go kind of thing. (Participant 7)
As one participant reflected, this is an ongoing issue with AOD nursing roles:
I guess this just this feeling that we are, I don't know, not as respected within the nursing profession and so we're just easy to just move on. (Participant 16)
Finally, one participant reported that an older nurse was deemed high risk and taken indefinite leave from work. Given the older age of the AOD nursing cohort (Searby & Burr, 2020), this is a significant concern and could lead to a loss of AOD nurses as the pandemic subsides:
There was one staff member who was currently undergoing cancer treatment who was allowed to stay home. She never returned. She hasn't returned to work. (Participant 13)
6. DISCUSSION
This study explored of the impact of the COVID‐19 pandemic on AOD nurses providing treatment for individuals presenting with problematic AOD use. Our findings demonstrate that nurses are a key profession in the AOD treatment workforce, and their experiences during COVID‐19 show unique narratives given they were often the last workers ‘left at the coalface’. Despite many healthcare settings mandating work from home to attempt to prevent the spread of the virus, this was often not achievable for nurses due to the nature of the role they perform; other studies echo our findings, showing the high level of stress and anxiety nursing staff experience in these situations (Liu et al., 2020; Mo et al., 2020).
In our study, stress and anxiety among nurses was increased due to the constant threat of redeployment. Often, this redeployment was away from AOD treatment settings to COVID‐19 specific areas, such as testing centres and respiratory medical environments. The notion that nurses are generalised and able to work readily in any setting discounts the specialist skills held by nurses such as those working in AOD treatment. Further, our participants also reported that the threat of relocation and redeployment had some nurses considering leaving the nursing profession, a significant threat to the ongoing sustainability of the AOD nursing role.
Many of the AOD usage patterns observed by participants in this study are beginning to be shown through research, particularly around alcohol consumption (Huckle et al., 2020; Sutherland et al., 2020), although these results seem to be region specific with some areas observing decreases in weekend consumption (Bade et al., 2020). These findings were reflected by participants who reported seeing more complex presentations for AOD treatment, as opposed to those they would usually see because of emergency department presentations for intoxication, primarily on weekends. Participants described consumers reporting a decrease in substance use due to availability, and although this was often spoken of as a positive aspect of the pandemic, there were also accounts provided of consumers moving to different substances or overdosing due to reduced tolerance or obtaining drugs of greater purity. These findings emphasise the importance of clinicians, including nurses, providing harm reduction education on tolerance and the risk of overdose, in addition to naloxone (Dion et al., 2020; Mullennix et al., 2020).
A reduction in face‐to‐face contact was described as a threat to maintaining rapport with consumers of AOD treatment services. Participants felt that engagement suffered when telehealth was used as a substitute for face‐to‐face appointments. There is limited research on the efficacy of telehealth methods used during COVID‐19 in AOD services, with urgent need to ensure that this service delivery modality is appropriate for consumers who seek AOD treatment (Uscher‐Pines et al., 2020). Additionally, participants reported concern at the perceived level of risk they believed telehealth carried, particularly when they could not observe clinical interactions or situations. Similar responses have been observed in other qualitative studies exploring the shift to telemedicine for AOD treatment (Uscher‐Pines et al., 2020).
Finally, the physical distancing and isolation requirements did see an increase in the use of long‐acting injectable buprenorphine formulations and take‐home methadone doses. Early evaluation research of similar flexibility in dosing conducted in Spain notes that this practice is largely a success and should continue beyond the pandemic (Trujols et al., 2020); however, local research needs to be conducted to evaluate the ongoing efficacy of this approach. What is clear, however, is that the role of the nurse is essential in administering and monitoring the effects of both flexible dosing regimens and long‐acting injectable preparations (Go et al., 2011). These treatments provide a clear mandate for the inclusion of the AOD nurse in all treatment services.
6.1. Strengths and weaknesses
To our knowledge, this study is the first in Australia and New Zealand exploring the experiences of AOD nurses during the COVID‐19 pandemic. Despite this strength of the study, there are limitations that need to be considered. Primarily, the sampling methodology used to recruit participants for this study meant that most Australian participants were from the state of New South Wales, with no representation from Victoria, South Australia, Tasmania or the Northern Territory. Workforce data show that New South Wales employs the majority of AOD nurses across Australia (Searby & Burr, 2020); however, the lack of representation from other states in conjunction with the qualitative approach of this study means the findings may not be representative of the wider AOD nursing workforce across Australia and New Zealand. Additionally, only one participant was from New Zealand despite our efforts to increase recruitment there. There are several speculative reasons for the lack of participation from other Australian states and New Zealand which may be associated with increased COVID numbers in regions such as the state of Victoria, lockdowns in Auckland or simply a lack of AOD nurses connected with the professional organisation (DANA) and therefore not seeing invitations to participate in the study. Future research should endeavour to recruit participants from these areas to provide a greater overview of the experiences of AOD nurses across the country.
The design of the study is cross‐sectional and represents the experiences of nurses at a specific point in time; as the COVID‐19 situation progresses, workforce impacts on nursing may change and future research should consider a longitudinal approach to explore changes over time (Nevedal et al., 2019).
7. CONCLUSION
The COVID‐19 pandemic has caused several fundamental changes to the way AOD treatment services were delivered, and the nursing workforce was not immune from these challenges. Further longitudinal research is required to determine the overall impact of COVID‐19 pandemic on workforce sustainability; the potential to lose many highly experienced, highly qualified AOD nurses is high given the findings of this study indicate that nurses simply stopped working in AOD treatment due to the perceived risk. Future research exploring the change in AOD use due to lack of supply or changes in availability should consider providing education on harm reduction to clinicians providing care to those seeking treatment. It is also imperative that the specialty of AOD nursing is protected from the notion that nurses can work in any setting. AOD treatment is a field employing highly specialised clinicians, including nursing staff.
8. RELEVANCE TO CLINICAL PRACTICE
The COVID‐19 pandemic has had a profound influence on healthcare services in Australia, and although we may not face another pandemic in the future, the effects of COVID are likely to continue to be felt by health service providers and nurses for some time. The need to ensure that nurses are prepared and supported in their role is essential, both to reduce anxiety that may impact on work performance and to ensure that the nursing workforce does not face insurmountable challenge in respect of many highly experienced nurses leaving the profession. This is an especially relevant factor for small, highly specialised branches of nursing, such as alcohol and other drug nursing.
The switch to new and novel treatments, such as the injectable buprenorphine depot, has shown the utility and value of nurses in alcohol and other drug treatment services. Further, nurses hold specific skills useful in times of pandemics, such as infection control and the ability to provide holistic physical healthcare to an often‐marginalised consumer population who use AOD treatment services. The role of the nurse should be promoted and protected in AOD treatment, and there is an urgent need to ensure the sustainability of this highly specialised nursing workforce.
Beyond AOD treatment, all nurses should hold skills in assessing and responding to problematic AOD use. As indicated in our research and supported by emerging data on alcohol and drug consumption patterns, the COVID‐19 pandemic has not only seen increases of alcohol and drug use in certain areas of Australia, but may also see individuals presenting to healthcare services for assistance who have never received treatment for problematic AOD use before (Callinan et al., 2020; Neill et al., 2020). Often, the first point of contact for these individuals is not AOD treatment, but other healthcare services such as the emergency department (Butler et al., 2016). Therefore, it is essential for all nurses to be able to assess for problematic AOD use in the wake of the COVID‐19 pandemic.
CONFLICT OF INTEREST
The authors have no competing interests to declare.
Supporting information
Supplementary Material
ACKNOWLEDGEMENTS
The authors acknowledge the Drug and Alcohol Nurses of Australasia (DANA) for their financial support to conduct this study. We would also like to thank the AOD nurses who volunteered their time to take part in this study.
Funding information
This project was funded by the Drug and Alcohol Nurses of Australasia (DANA), the peak body for nurses with an interest in alcohol and other drug issues in Australia and New Zealand.
REFERENCES
- Adekunle, A. , Meehan, M. , Rojas‐Alvarez, D. , Trauer, J. , & McBryde, E. (2020). Delaying the COVID‐19 epidemic in Australia: Evaluating the effectiveness of international travel bans. Australian and New Zealand Journal of Public Health, 44(4), 257–259. 10.1111/1753-6405.13016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Australian Bureau of Statistics (2020). Household Impacts of COVID‐19 Survey. Retrieved from https://www.abs.gov.au/statistics/people/people‐and‐communities/household‐impacts‐covid‐19‐survey/24‐29‐june‐2020 [Google Scholar]
- Australian Criminal Intelligence Commission (2020). National Wastewater Drug Monitoring Program Report 11, 2020. Commonwealth of Australia. Retrieved from https://www.acic.gov.au/sites/default/files/2020‐10/NWDMP_R11%20‐%20FINAL.pdf [Google Scholar]
- Australian Government Department of Health (2020a). COVID‐19 Australia: Epidemiology Report 23. Retrieved from https://www1.health.gov.au/internet/main/publishing.nsf/Content/novel_coronavirus_2019_ncov_weekly_epidemiology_reports_australia_2020.htm [Google Scholar]
- Australian Government Department of Health (2020b). COVID‐19 outbreaks in Australian residential aged care facilities. AIHW. Retrieved from https://www.health.gov.au/sites/default/files/documents/2020/12/covid‐19‐outbreaks‐in‐australian‐residential‐aged‐care‐facilities‐4‐december‐2020.pdf [Google Scholar]
- Australian Institute of Health and Welfare (2020b). Australia's health: 2020 data insights. AIHW. Retrieved from https://www.aihw.gov.au/reports/australias‐health/australias‐health‐2020‐data‐insights/contents/summary [Google Scholar]
- Australian Institute of Health and Welfare (2020a). Alcohol, tobacco and other drugs in Australia . Retrieved from https://www.aihw.gov.au/reports/alcohol/alcohol‐tobacco‐other‐drugs‐australia/contents/interactive‐data/tobacco
- Bade, R. , Simpson, B. S. , Ghetia, M. , Nguyen, L. , White, J. M. , & Gerber, C. (2020). Changes in alcohol consumption associated with social distancing and self‐isolation policies triggered by COVID‐19 in South Australia: a wastewater analysis study. Addiction. 10.1111/add.15256. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Braun, V. , & Clarke, V. (2006). Using thematic analysis in psychology. Qualitative Research in Psychology, 3(2), 77–101. 10.1191/1478088706qp063oa [DOI] [Google Scholar]
- Butler, K. , Reeve, R. , Arora, S. , Viney, R. , Goodall, S. , van Gool, K. , & Burns, L. (2016). The hidden costs of drug and alcohol use in hospital emergency departments. Drug and Alcohol Review, 35(3), 359–366. 10.1111/dar.12302 [DOI] [PubMed] [Google Scholar]
- Callinan, S. , Mojica‐Perez, Y. , Wright, C. J. C. , Livingston, M. , Kuntsche, S. , Laslett, A.‐M. , Room, R. , & Kuntsche, E. (2020). Purchasing, consumption, demographic and socioeconomic variables associated with shifts in alcohol consumption during the COVID‐19 pandemic. Drug and Alcohol Review. 10.1111/dar.13200 [DOI] [PubMed] [Google Scholar]
- Chew, N. W. S. , Lee, G. K. H. , Tan, B. Y. Q. , Jing, M. , Goh, Y. , Ngiam, N. J. H. , Yeo, L. L. L. , Ahmad, A. , Ahmed Khan, F. , Napolean Shanmugam, G. , Sharma, A. K. , Komalkumar, R. N. , Meenakshi, P. V. , Shah, K. , Patel, B. , Chan, B. P. L. , Sunny, S. , Chandra, B. , Ong, J. J. Y. , … Sharma, V. K. (2020). A multinational, multicentre study on the psychological outcomes and associated physical symptoms amongst healthcare workers during COVID‐19 outbreak. Brain, Behavior, and Immunity, 88, 559–565. 10.1016/j.bbi.2020.04.049 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choi, K. R. , Heilemann, M. V. , Fauer, A. , & Mead, M. (2020). A second pandemic: Mental health spillover from the novel coronavirus (COVID‐19). Journal of the American Psychiatric Nurses Association, 26(4), 340–343. 10.1177/1078390320919803 [DOI] [PubMed] [Google Scholar]
- Colbert, S. , Wilkinson, C. , Thornton, L. , & Richmond, R. (2020). COVID‐19 and alcohol in Australia: Industry changes and public health impacts. Drug and Alcohol Review, 39(5), 435–440. 10.1111/dar.13092 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dietze, P. M. , & Peacock, A. (2020). Illicit drug use and harms in Australia in the context of COVID‐19 and associated restrictions: Anticipated consequences and initial responses. Drug and Alcohol Review, 39(4), 297–300. 10.1111/dar.13079 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dion, K. , Chiodo, L. , Whynott, L. , Loftus, B. , Alvarez, P. , Shanahan, J. , Quaglia, G. , Roman, A. , Sorbi, E. , & Wilkins‐Carmody, D. (2020). Exploration of the unmet health care needs of people who inject drugs. Journal of the American Association of Nurse Practitioners, 32(1), 60–69. 10.1097/JXX.0000000000000201 [DOI] [PubMed] [Google Scholar]
- Dunlop, A. , Lokuge, B. , Masters, D. , Sequeira, M. , Saul, P. , Dunlop, G. , Ryan, J. , Hall, M. , Ezard, N. , Haber, P. , Lintzeris, N. , & Maher, L. (2020). Challenges in maintaining treatment services for people who use drugs during the COVID‐19 pandemic. Harm Reduction Journal, 17(1), 26. 10.1186/s12954-020-00370-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fernandez, R. , Lord, H. , Halcomb, E. , Moxham, L. , Middleton, R. , Alananzeh, I. , & Ellwood, L. (2020). Implications for COVID‐19: A systematic review of nurses’ experiences of working in acute care hospital settings during a respiratory pandemic. International Journal of Nursing Studies, 111, 103637. 10.1016/j.ijnurstu.2020.103637 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Go, F. , Dykeman, M. , Santos, J. , & Muxlow, J. (2011). Supporting clients on methadone maintenance treatment: A systematic review of nurse's role. Journal of Psychiatric and Mental Health Nursing, 18(1), 17–27. 10.1111/j.1365-2850.2010.01628.x [DOI] [PubMed] [Google Scholar]
- Hemmler, V. L. , Kenney, A. W. , Langley, S. D. , Callahan, C. M. , Gubbins, E. J. , & Holder, S. (2020). Beyond a coefficient: An interactive process for achieving inter‐rater consistency in qualitative coding. Qualitative Research. 10.1177/1468794120976072. [Epub ahead of print] [DOI] [Google Scholar]
- Holmes, E. A. , O'Connor, R. C. , Perry, V. H. , Tracey, I. , Wessely, S. , Arseneault, L. , Ballard, C. , Christensen, H. , Cohen Silver, R. , Everall, I. , Ford, T. , John, A. , Kabir, T. , King, K. , Madan, I. , Michie, S. , Przybylski, A. K. , Shafran, R. , Sweeney, A. , … Bullmore, E. (2020). Multidisciplinary research priorities for the COVID‐19 pandemic: A call for action for mental health science. The Lancet Psychiatry, 7(6), 547–560. 10.1016/S2215-0366(20)30168-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huckle, T. , Parker, K. , Romeo, J. S. , & Casswell, S. (2020). Online alcohol delivery is associated with heavier drinking during the first New Zealand COVID‐19 pandemic restrictions. Drug and Alcohol Review. 10.1111/dar.13222. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jefferies, S. , French, N. , Gilkison, C. , Graham, G. , Hope, V. , Marshall, J. , McElnay, C. , McNeill, A. , Muellner, P. , Paine, S. , Prasad, N. , Scott, J. , Sherwood, J. , Yang, L. , & Priest, P. (2020). COVID‐19 in New Zealand and the impact of the national response: A descriptive epidemiological study. The Lancet Public Health, 5(11), e612–e623. 10.1016/S2468-2667(20)30225-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kang, L. , Ma, S. , Chen, M. , Yang, J. , Wang, Y. , Li, R. , Yao, L. , Bai, H. , Cai, Z. , Xiang Yang, B. , Hu, S. , Zhang, K. , Wang, G. , Ma, C. , & Liu, Z. (2020). Impact on mental health and perceptions of psychological care among medical and nursing staff in Wuhan during the 2019 novel coronavirus disease outbreak: A cross‐sectional study. Brain, Behavior, and Immunity, 87, 11–17. 10.1016/j.bbi.2020.03.028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lai, J. , Ma, S. , Wang, Y. , Cai, Z. , Hu, J. , Wei, N. , Wu, J. , Du, H. , Chen, T. , Li, R. , Tan, H. , Kang, L. , Yao, L. , Huang, M. , Wang, H. , Wang, G. , Liu, Z. , & Hu, S. (2020). Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Network Open, 3(3), e203976. 10.1001/jamanetworkopen.2020.3976 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Litton, E. , Bucci, T. , Chavan, S. , Ho, Y. Y. , Holley, A. , Howard, G. , Huckson, S. , Kwong, P. , Millar, J. , Nguyen, N. , Secombe, P. , Ziegenfuss, M. , & Pilcher, D. (2020). Surge capacity of intensive care units in case of acute increase in demand caused by COVID‐19 in Australia. Medical Journal of Australia, 212(10), 463–467. 10.5694/mja2.50596 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu, Q. , Luo, D. , Haase, J. E. , Guo, Q. , Wang, X. Q. , Liu, S. , Xia, L. , Liu, Z. , Yang, J. , & Yang, B. X. (2020). The experiences of health‐care providers during the COVID‐19 crisis in China: A qualitative study. Lancet Glob Health, 8(6), e790–e798. 10.1016/s2214-109x(20)30204-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- López‐Pelayo, H. , Aubin, H.‐J. , Drummond, C. , Dom, G. , Pascual, F. , Rehm, J. , Saitz, R. , Scafato, E. , & Gual, A. (2020). “The post‐COVID era”: Challenges in the treatment of substance use disorder (SUD) after the pandemic. BMC Medicine, 18(1), 241. 10.1186/s12916-020-01693-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mealer, M. , & Jones, J. (2014). Methodological and ethical issues related to qualitative telephone interviews on sensitive topics. Nurse Researcher (2014+), 21(4), 32–37. 10.7748/nr2014.03.21.4.32.e1229 [DOI] [PubMed] [Google Scholar]
- Mo, Y. , Deng, L. , Zhang, L. , Lang, Q. , Liao, C. , Wang, N. , Qin, M. , & Huang, H. (2020). Work stress among Chinese nurses to support Wuhan in fighting against COVID‐19 epidemic. Journal of Nursing Management, 28(5), 1002–1009. 10.1111/jonm.13014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mullennix, S. C. , Iseler, J. , Kwiatkowski, G. M. , McCann‐Spry, L. , Skinner, J. , Kuhl, N. , VanDePol, E. K. , & Poland, C. A. (2020). A clinical nurse specialist‐led emergency department naloxone distribution program. Clinical Nurse Specialist, 34(3), 116–123. 10.1097/NUR.0000000000000515 [DOI] [PubMed] [Google Scholar]
- Neergaard, M. A. , Olesen, F. , Andersen, R. S. , & Sondergaard, J. (2009). Qualitative description – The poor cousin of health research? BMC Medical Research Methodology, 9(1), 52. 10.1186/1471-2288-9-52 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neill, E. , Meyer, D. , Toh, W. L. , van Rheenen, T. E. , Phillipou, A. , Tan, E. J. , & Rossell, S. L. (2020). Alcohol use in Australia during the early days of the COVID‐19 pandemic: Initial results from the COLLATE project. Psychiatry and Clinical Neurosciences, 74(10), 542–549. 10.1111/pcn.13099 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nevedal, A. L. , Ayalon, L. , & Briller, S. H. (2019). A qualitative evidence synthesis review of longitudinal qualitative research in gerontology. The Gerontologist, 59(6), e791–e801. 10.1093/geront/gny134 [DOI] [PubMed] [Google Scholar]
- Palinkas, L. A. , Horwitz, S. M. , Green, C. A. , Wisdom, J. P. , Duan, N. , & Hoagwood, K. (2015). Purposeful sampling for qualitative data collection and analysis in mixed method implementation research. Administration and Policy in Mental Health, 42(5), 533–544. 10.1007/s10488-013-0528-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pierce, M. , Hope, H. , Ford, T. , Hatch, S. , Hotopf, M. , John, A. , Kontopantelis, E. , Webb, R. , Wessely, S. , McManus, S. , & Abel, K. M. (2020). Mental health before and during the COVID‐19 pandemic: A longitudinal probability sample survey of the UK population. The Lancet Psychiatry, 7(10), 883–892. 10.1016/S2215-0366(20)30308-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ritter, A. , & Natale, R. D. I. (2005). The relationship between take‐away methadone policies and methadone diversion. Drug and Alcohol Review, 24(4), 347–352. 10.1080/09595230500263939 [DOI] [PubMed] [Google Scholar]
- Sandelowski, M. (2010). What's in a name? Qualitative description revisited. Research in Nursing and Health, 33(1), 77–84. 10.1002/nur.20362 [DOI] [PubMed] [Google Scholar]
- Searby, A. , & Burr, D. (2020). State of the workforce 2020: Mapping the alcohol and other drug (AOD) nursing workforce in Australia and New Zealand. Woolloongabba, Queensland: Drug and Alcohol Nurses of Australasia (DANA). Retrieved from https://www.danaonline.org/wp‐content/uploads/2020/12/DANA‐workforce‐2020‐final‐report.pdf [Google Scholar]
- Skinner, N. , McEntee, A. , & Roche, A. (2020). Australia's Alcohol and Other Drug Workforce: National Survey Results 2019–2020. Adelaide, South Australia: National Centre For Education and Training on Addiction (NCETA). Retrieved from http://nceta.flinders.edu.au/workforce/national‐alcohol‐other‐drugs‐workforce‐survey‐2019/ [Google Scholar]
- Sorci, G. , Faivre, B. , & Morand, S. (2020). Explaining among‐country variation in COVID‐19 case fatality rate. Scientific Reports, 10(1), 18909. 10.1038/s41598-020-75848-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sutherland, R. , Baillie, G. , Memedovic, S. , Hammoud, M. , Barratt, M. , Bruno, R. , Dietze, P. , Ezard, N. , Salom, C. , Degenhardt, L. , Hughes, C. , & Peacock, A. (2020). Key findings from the ‘Australians’ Drug Use: Adapting to Pandemic Threats (ADAPT)’ Study. ADAPT Bulletin no. 1. In National Drug and Alcohol Research Centre. UNSW Sydney. [Google Scholar]
- Tan, E. J. , Meyer, D. , Neill, E. , Phillipou, A. , Toh, W. L. , Van Rheenen, T. E. , & Rossell, S. L. (2020). Considerations for assessing the impact of the COVID‐19 pandemic on mental health in Australia. Australian & New Zealand Journal of Psychiatry, 54(11), 1067–1071. 10.1177/0004867420947815 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tong, A. , Sainsbury, P. , & Craig, J. (2007). Consolidated criteria for reporting qualitative research (COREQ): a 32‐item checklist for interviews and focus groups. International Journal for Quality in Health Care, 19(6), 349–357. 10.1093/intqhc/mzm042 [DOI] [PubMed] [Google Scholar]
- Torales, J. , O’Higgins, M. , Castaldelli‐Maia, J. M. , & Ventriglio, A. (2020). The outbreak of COVID‐19 coronavirus and its impact on global mental health. International Journal of Social Psychiatry, 66(4), 317–320. 10.1177/0020764020915212 [DOI] [PubMed] [Google Scholar]
- Trujols, J. , Larrabeiti, A. , Sànchez, O. , Madrid, M. , De Andrés, S. , & Duran‐Sindreu, S. (2020). Increased flexibility in methadone take‐home scheduling during the COVID‐19 pandemic: Should this practice be incorporated into routine clinical care? Journal of Substance Abuse Treatment, 119, 108154. 10.1016/j.jsat.2020.108154 [DOI] [PMC free article] [PubMed] [Google Scholar]
- United Nations . (2020). World Drug Report 2020. Vienna, Austria: United Nations Office on Drugs and Crime. www.unodc.org/wdr2020 [Google Scholar]
- Uscher‐Pines, L. , Sousa, J. , Raja, P. , Mehrotra, A. , Barnett, M. , & Huskamp, H. A. (2020). Treatment of opioid use disorder during COVID‐19: Experiences of clinicians transitioning to telemedicine. Journal of Substance Abuse Treatment, 118, 108124. 10.1016/j.jsat.2020.108124 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Voce, A. , Finney, J. , Gately, N. , & Sullivan, T. (2020). Statistical Bulletin 29: COVID‐19 pandemic constricts methamphetamine supply in Perth. Australian Institute of Criminology. Retrieved from https://www.aic.gov.au/sites/default/files/2020‐09/sb29_covid‐19_pandemic_constricts_methamphetamine_supply_in_perth.pdf [Google Scholar]
- Wong, E. L. Y. , Wong, S. Y. S. , Kung, K. , Cheung, A. W. L. , Gao, T. T. , & Griffiths, S. (2010). Will the community nurse continue to function during H1N1 influenza pandemic: A cross‐sectional study of Hong Kong community nurses? BMC Health Services Research, 10(1), 107. 10.1186/1472-6963-10-107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organisation and International Council of Nurses (2009). ICN Framework of Disaster Nursing Competencies. Geneva, Switzerland: International Council of Nurses. Retrieved from http://www.apednn.org/doc/resourcespublications/ICN%20Framework%20of%20Disaster%20Nursing%20Competencies%20ICN%202009.pdf [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Material


