Abstract
Recent studies showed that the COVID‐19 pandemic caused collateral damage in health care in terms of reduced hospital submissions or postponed treatment of other acute or chronic ill patients. An anonymous survey was sent out by mail to patients with chronic wounds in order to evaluate the impact of the pandemic on wound care. Sixty‐three patients returned the survey. In 14%, diagnostic workup or hospitalisation was cancelled or postponed. Thirty‐six percent could not seek consultation by their primary care physician as usual. The use of public transport or long travel time was not related to limited access to medical service (P = .583). In ambulatory care, there was neither a significant difference in the frequency of changing wound dressings (P = .67), nor in the person, who performed wound care (P = .39). There were no significant changes in wound‐specific quality of life (P = .505). No patient used telemedicine in order to avoid face‐to‐face contact or anticipate to pandemic‐related restrictions. The COVID‐19 pandemic impaired access to clinical management of chronic wounds in Germany. It had no significant impact on ambulatory care or wound‐related quality of life. Telemedicine still plays a negligible role in wound care.
Keywords: COVID‐19, leg ulcer, quality of life, telemedicine, wounds
1. INTRODUCTION
The coronavirus disease 2019 (COVID‐19) pandemic remains a strong challenge for health care systems around the world. The restricted access to medical service led to collateral damage to patients with other conditions but in strong need of treatment. Hospitals and emergency departments reported a decline in admissions for acute and life‐threatening conditions such as myocardial infarction, stroke, or hyperglycemic crisis. 1 , 2 , 3 Oncological patients are at risk for delayed diagnosis and treatment, which may impact their long‐term survival. 4 In addition, millions of patients with disabilities, including those who survived a severe course of COVID‐19 infection, are affected as access to rehabilitation is strongly impacted. 5 The COVID‐19 pandemic and the consequent restrictions, such as self‐quarantine or public lockdown, also limited the care of patients with chronic wounds in Italy. 6 In addition, because of higher age and multiple comorbidities, patients with chronic wounds are at higher risk for a severe course after infection with COVID‐19. However, the extent of the COVID‐19 outbreak and the public restrictions vary between regions and may influence peoples' attitude and protectoral behaviour. In Germany, a strain on the public health care system could be averted so far. However, as in most countries, German authorities implemented a nation‐wide public lockdown and restricted access to medical service for non‐urgent cases. In this survey, we sought to evaluate the impact of the COVID‐19 pandemic on chronic wound patients at our institution.
2. METHODS
Patients diagnosed with any kind of ulceration or chronic wound within the past 2 years at the outpatient clinic of the Department of Dermatology and Allergy, University Hospital, LMU (Ludwig Maximilian University) Munich, Germany, were contacted in June 2020 by mail and asked for participation in this fully anonymous questionnaire‐based cross‐sectional study. The ethics committee of the medical faculty at LMU approved the study, which was performed in accordance with the Helsinki Declaration of 1975.
A structured questionnaire was used for data collection. Information on (a) demographics (gender, age, educational background, health insurance); (b) diagnoses; (c) wound status; (d) wound dressing; and (e) medical care during the COVID‐19 pandemic were obtained. Additionally, this survey included the Wound‐QoL, a questionnaire on health‐related quality of life in patients with chronic wounds. 7
For descriptive statistics, mean with 95% confidence interval (CI) was calculated for numerical data, while proportions were calculated for categorical variables. Goodman‐Kruskal's gamma was calculated to test for a correlation between the amount of medications and hospitalisation for wound treatment. Wilcoxon's signed rank test with continuity correction was used to compare the frequency of wound dressing before and during COVID‐19. McNemar's chi‐squared test was applied to test for a difference in the person performing the wound dressing before and during COVID‐19. Pearson's chi‐squared test with Yates's continuity correction was applied to test for an association between the use of public transport and limited doctor access during COVID‐19. Whether the transportation time correlates with limited doctor access was tested by calculating Goodman‐Kruskal's gamma. The data obtained by the Wound‐QoL were analysed as suggested by Augustin et al. 8 The resulting Wound‐QoL values were compared with values obtained by Sommer et al from 2017 with two‐sample t tests. 9 All statistics were performed in R, version 3.6.0, 2010, R Foundation for Statistical Computing (Vienna, Austria) using the R packages: Hmisc, coind, vcdExtra, Mess, gmodels, and ggplot2.
3. RESULTS
This anonymous survey was sent out to 288 patients that presented with a non‐healing, chronic wound in our outpatient clinic within the last 2 years prior to the study. In total, 63 patients completed the survey, which corresponds to a return rate of 21.9%. However, not all participants answered every question.
Slightly more participants were female (55.6%). There were seven patients (11.1%) under 50 years and 28 (44.4%) over the age of 80 as shown in Table 1. Among different wound types, 19 patients (33.3%) stated to suffer from venous ulcer, followed by diabetic and arterial ulcerations in 5 patients (8.5%), respectively. Another five patients (8.8%) had a mixed aetiology of underlying venous insufficiency, arterial disease or diabetes. One suffered from pyoderma gangraenosum, 9 participants (15.8%) did not know the aetiology of their wound, and 13 (22,8%) stated other reasons, such as impaired healing of postsurgical wounds (number of replies: n = 57). Most patients (66.6%) had general education or passed middle school and 16 (33.3%) experienced higher education (n = 48). Twenty‐one participants (67.7%) have had a vocational training or specialisation, while 10 (32.3%) held a university degree (n = 31). Most patients (93.5%) were covered by public health insurance and three patients (4.8%) by private health insurance (n = 62). With regard to comorbidity and burden of the disease, around half of the participants (49.2%) took more than five drugs per day, whereas six (9.5%) denied taking any medication on daily basis (n = 63). In addition, 37 participants (59.7%) were hospitalised at least once in the previous 12 months, of these 15 (24.2%) even three times or more (n = 62). Hospitalisation because of the wound was necessary in half of the participants (49.2%) in the previous 12 months, of these 11 (18.0%) three times or more (n = 61). There was a significant correlation between the amount of medications and the frequency of hospitalisation because of the wound (Goodman‐Kruskal's gamma: 0.48, 95% CI: 0.23, 0.72, Z = 3.4, P < .001). In order to visit the physician or wound clinic, 29 patients (50.9%) depended on the help of others and needed to be transported by car or ambulance (n = 57).
TABLE 1.
Demographic and clinical characteristics of the study participants
| n | % | n = replies | |
|---|---|---|---|
| Gender | 63 | ||
| Female | 35 | 55.6 | |
| Male | 28 | 44.4 | |
| Age | 63 | ||
| <50 | 7 | 11.1 | |
| 50‐59 | 8 | 12.7 | |
| 60‐69 | 7 | 11.1 | |
| 70‐79 | 13 | 20.6 | |
| 80 or older | 28 | 44.4 | |
| School education | 38 | ||
| General education (9 years) | 16 | 33.3 | |
| Middle school (10 years) | 16 | 33.3 | |
| Higher education (12‐13 years) | 16 | 33.3 | |
| Medication per day | 63 | ||
| None | 6 | 9.5 | |
| 1‐4 | 26 | 41.3 | |
| 5‐10 | 20 | 31.7 | |
| 10 or more | 11 | 17.5 | |
| Hospitalisation within 12 months prior to study | 62 | ||
| None | 25 | 40.3 | |
| 1‐2× | 22 | 35.5 | |
| 3× or more | 15 | 24,2 | |
| Hospitalisation for wound treatment, 12 months prior to study | 61 | ||
| None | 31 | 50.8 | |
| 1‐2× | 19 | 31,1 | |
| 3× or more | 11 | 18 | |
| Wound aetiology | 57 | ||
| Venous ulcer | 19 | 33.3 | |
| Diabetic ulcer | 5 | 8.8 | |
| Arterial ulcer | 5 | 8.8 | |
| Mixed‐aetiology | 5 | 8.8 | |
| Pyoderma gangraenosum | 1 | 1.8 | |
| Pressure ulcer | 0 | 0.0 | |
| Unknown | 9 | 15.8 | |
| Other | 13 | 22.8 |
Fifty‐seven participants (90.5%) denied any delay or cancellation of planned diagnostic measures because of the COVID‐19 pandemic. In four patients (6%), diagnostic workup was postponed, in two cases (3%) the diagnostic workup was cancelled without alternative appointment (n = 63). One patient (1.6%) stated not having been hospitalised for wound treatment because of COVID‐19 restrictions, and in two patients (3.3%) the hospitalisation was postponed (n = 61).
With regard to a potential impact of public lockdown or restricted access to medical services on outpatient wound care, there was no significant difference in the frequency of changing wound dressings during versus prior to the pandemic (Wilcoxon signed rank test, V = 32, P = .666; Figure 1). One patient (2.3%) stated that wound care at home was cancelled because of COVID‐19. For the other seven patients (15.9%) with ambulant care, home visits by a nurse continued as usual (n = 44). After implementation of the public lockdown, there was no significant difference which person, such as patient, relatives, or care givers performed wound dressing (McNemar's chi–squared test = 3, df = 3, P = .392; Figure 2).
FIGURE 1.
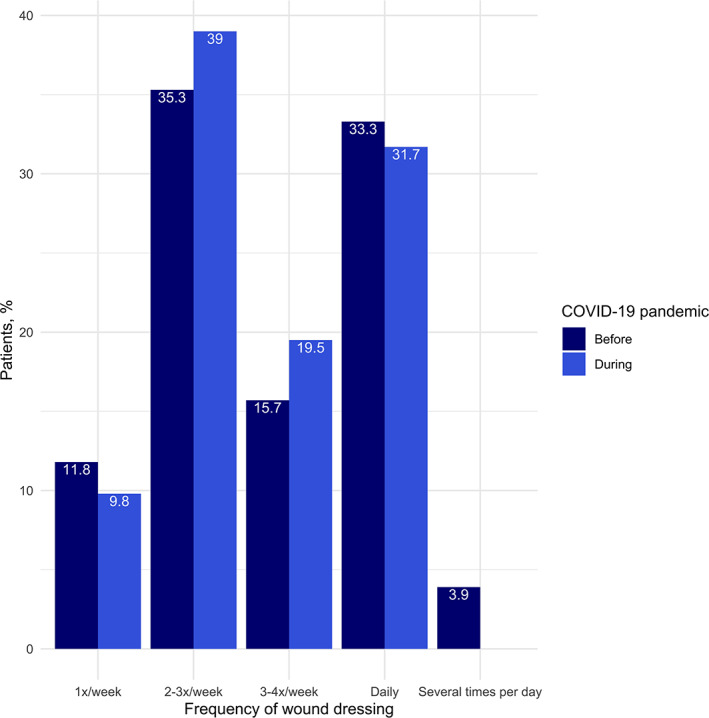
Frequency of wound dressing before versus during the COVID‐19 pandemic. There was no significant difference (P = .67)
FIGURE 2.
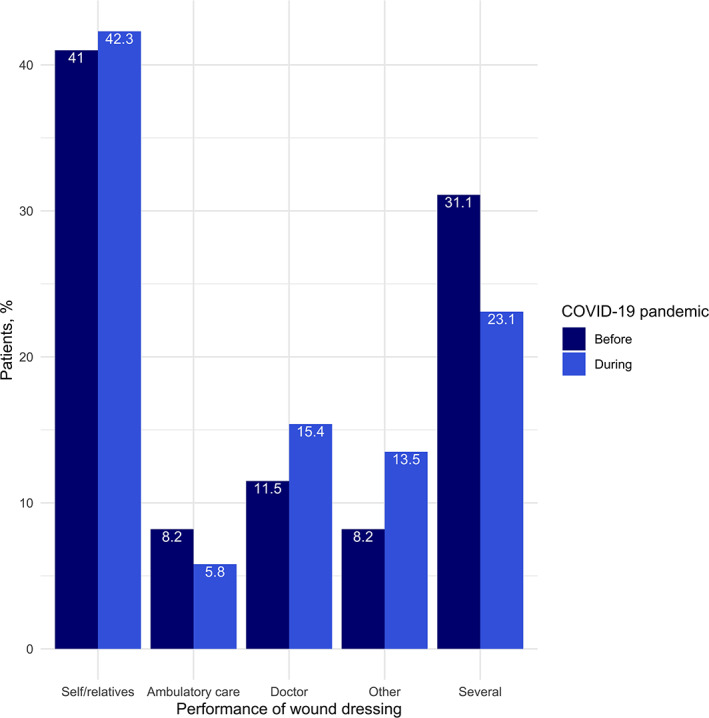
Person performing wound dressing before versus during the COVID‐19 pandemic. There was no significant difference (P = .39)
We further assessed whether the frequency of doctor consultations may have been impacted by the pandemic and if the use of public transport or travel time may have an influence. Thirty participants (63.8%) stated to see their physician as usual. Eleven patients (23%) could visit their physician, but less frequently as usual. Only one patient (2%) could not consult his doctor because of COVID‐19‐related restrictions. Five patients (10.6%) avoided doctor visits because of fear of COVID‐19 (n = 47). It had no significant influence on medical care, if patients depended on public transport (Pearson's chi‐squared test, χ 2 = 0.41, df = 1, P = .521). Longer travel duration did not limit patients' access to his or her physician, neither (Goodman‐Kruskal's gamma: 0.15, 95% CI: −037 to 0.66, Z = 0.6, P = .583).
The total mean score of the wound‐specific quality of life assessment was 1.46 (95% CI: 1.15‐1.78, SD = 1.11, n = 50). There was no significant difference compared with quality of life values of the referential study of Sommer et al (two‐sample t test: t(67) = 0.67, P = .505). There were also no significant differences with regard to the three subscales “body” (two‐sample t test: t(76) = 1.09, P = .280), “psychology” (two‐sample t test: t(85) = 1.17, P = .244), and “everyday life” (two‐sample t test: t(81) = 0.13, P = .896).
When asked about the option of using telemedicine as digital alternative to physical doctor visits, two patients (4.3%) already used telemedicine, but none newly initiated digital consultations in order to avoid face‐to‐face contact. However, 19 participants (41.3%) showed interest in telemedicine, whereas 12 (26.1%) refused it and 13 (28.3%) did not know what telemedicine is (n = 46; Figure 3).
FIGURE 3.
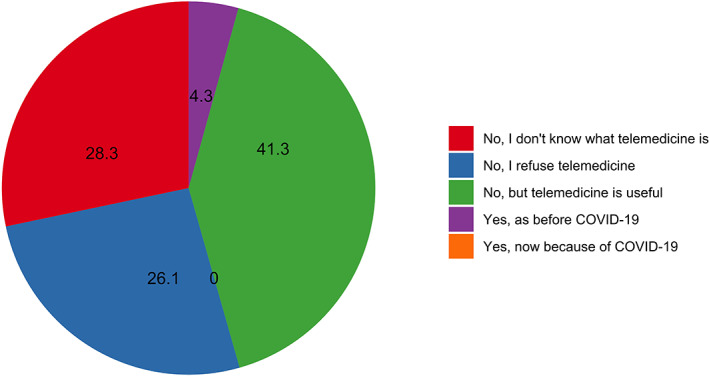
Use of telemedicine during the COVID‐19 pandemic. No patient newly initiated digital consultations during the COVID‐19 pandemic. Numbers represent proportion in percent
4. DISCUSSION
This cross‐sectional survey provides evidence on the impact of the COVID‐19 pandemic on patients with chronic wounds in Germany. The study population was comparable to those of previous clinical trials on chronic wounds. 9 , 10 Most patients were disabled and suffered multiple comorbidities given the high percentage of geriatric patients, polypharmacy, immobility and high hospitalisation rate within 12 months prior to the study. The obtained data show that the COVID‐19 pandemic had negative impact on wound care in terms of diagnostic workup, hospitalisation, and access to the primary care physician. However, the pandemic‐related restrictions did not significantly impair wound care at home. The use of public transport or longer travel time did not appear to be related to limited access to the physician. There were no significant changes in wound‐specific quality of life during the pandemic. Only few patients used telemedicine before, and none initiated digital consultation because of the pandemic.
Recent studies discussed the collateral damage of overburdened health care systems and restricted access to non‐essential health services during the COVID‐19 pandemic with regard to patients with chronic leg ulcers. 6 , 11 , 12 For example, an Italian survey asked medical doctors, nurses, caregivers, and 28 patients with chronic leg ulcers about their perception of the impact of COVID‐19 on wound care. This study showed that over 75% of the patients discontinued their consultations at the wound clinic. Most patients or their relatives continued to change wound dressings at home, and almost 13% of the patients did not change the wound dressing at all during the pandemic. Finally, over 15% stated that their wound had worsened. 6 Our findings show that the COVID‐19 pandemic had a considerable impact on wound care in Germany as well, but to a lesser extent. Obvious reasons may be the higher incidence of COVID‐19 cases and, subsequently, the higher exposure risk in Italy. Public lockdown and restricted access to medical services were more stringently implemented compared with Germany, where outbreak severity was relatively limited. However, collateral damage in health care was also seen in Germany, for example, in a significant decline of admissions to the emergency departments. 13 In addition, in order to cope with a potential rapid increase of COVID‐19 cases, as seen in neighbouring countries, non‐essential medical services in Germany were reduced. Many outpatient wound clinics, such as ours, were closed for several weeks during the pandemic. However, in Germany, the rising curve of COVID‐19 cases could be flattened and, so far, an overburden of the health care system could be averted. This may have affected patients' perception of the pandemic and reduce their fear of infection with COVID‐19. This might explain why only 10% refused to visit the doctor in order to avoid potential exposure to the virus. Furthermore, already prior to the pandemic, many patients of this sample changed wound dressings either alone or with help of family members. Thus, restrictions to medical services might not have led to a significant impact on daily wound care.
Finally, the pandemic had no significant impact on the wound‐specific quality of life. We compared our findings with data of Sommer and colleagues from 2017 as reference values. 9 A statistical comparison of two different patient cohorts is associated with bias. Hence, this finding should be interpreted with caution. However, both study populations were comparable in terms of gender, age, educational level, and distribution of wound aetiologies. Sommer et al assessed the quality of life in German patients, who had local nursing service. In our sample, only 18.2% had ambulant care. Thus, comorbidities or severity of the wound might have been more significant compared with our sample. However, because the pandemic nearly caused no disruption in local nursing service in our population, the impact of this difference might be limited.
Telemedicine is an increasing popular alternative that provides health care via digital communication between medical staff and patients using smartphones, email, or videoconference. 14 During the pandemic, the interest in telemedicine increased significantly among patients in the United States. 15 As response to public restrictions and constraints to the health care system, some wound clinics anticipated their strategy and increasingly used photograph‐ and video‐based communication to maintain professional wound care. 16 , 17 However, our data yield that telemedicine in wound care remains very uncommon in Germany. Most of all, this may be due to the lack of established telemedicine systems or even technical resources and know‐how. In addition, more than half of the included patients did not know of the existence of telemedicine or even refused it. The latter may be conditioned by scepticism concerning the protection of personal data and lack of knowledge about the advantages of telemedicine. Furthermore, because of the impact of the COVID‐19 pandemic on our patient sample was limited, a shift towards digital wound consultation might not have been considered as necessary. However, the COVID‐19 pandemic remains a challenge for months and probably years to come. Wound care through telecommunication would be a reasonable strategy in order to prevent the spread of COVID‐19 and protect medical workers and the major‐at‐risk patients with chronic wounds.
The main limitation of this survey is the limited sample size of 63 patients at a single‐centre site. In addition, not all participants answered every question. However, the return rate of this survey (22%) was remarkably high. To our knowledge, this is the largest survey to assess the impact of the COVID‐19 pandemic on patients with chronic wounds and the first to focus on the patients' perspective.
5. CONCLUSION
This survey provides evidence that the COVID‐19 pandemic impaired access to clinical management of chronic wounds in Germany. However, the restrictions had no significant impact on home care or wound‐related quality of life. Despite its clear advantages in wound care, especially with respect to the pandemic, telemedicine plays a negligible role in Germany. However, these findings are based on data of only one institution and generalizability may be limited. Collateral damage of the COVID‐19 pandemic on patients with chronic wounds may depend on regional outbreak severity. The final impact depends on the ongoing course of the pandemic and remains subject of future research.
CONFLICT OF INTEREST
The authors declared no potential conflicts of interest.
ACKNOWLEDGMENTS
Open access funding enabled and organized by Projekt DEAL.
Schlager JG, Kendziora B, Patzak L, et al. Impact of COVID‐19 on wound care in Germany. Int Wound J. 2021;18:536–542. 10.1111/iwj.13553
Markus Reinholz and Daniela Hartmann contributed equally to this study.
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.
REFERENCES
- 1. Lange SJ, Ritchey MD, Goodman AB, et al. Potential indirect effects of the COVID‐19 pandemic on use of emergency departments for acute life‐threatening conditions—United States, January–May 2020. MMWR Morb Mortal Wkly Rep. 2020;69(25):795‐800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Reinstadler SJ, Reindl M, Lechner I, et al. Effect of the COVID‐19 pandemic on treatment delays in patients with ST‐segment elevation myocardial infarction. JCM. 2183;9(7):2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Diegoli H, Magalhães PSC, Martins SCO, et al. Decrease in hospital admissions for transient ischemic attack, mild, and moderate stroke during the COVID‐19 era. Stroke. 2020;51(8):2315‐2321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Sud A, Jones ME, Broggio J, et al. Collateral damage: the impact on outcomes from cancer surgery of the COVID‐19 pandemic. Ann Oncol. 2020;31(8):1065‐1074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Negrini S, Grabljevec K, Boldrini P, et al. Up to 2.2 million people experiencing disability suffer collateral damage each day of COVID‐19 lockdown in Europe. Eur J Phys Rehabil Med. 2020;56(3):361‐365. [DOI] [PubMed] [Google Scholar]
- 6. Tinelli G, Sica S, Guarnera G, Pitocco D, Tshomba Y. Wound care during COVID‐19 pandemic. Ann Vasc Surg. 2020;68:93‐94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Blome C, Baade K, Debus ES, Price P, Augustin M. The “Wound‐QoL”: a short questionnaire measuring quality of life in patients with chronic wounds based on three established disease‐specific instruments. Wound Repair Regen. 2014;22(4):504‐514. [DOI] [PubMed] [Google Scholar]
- 8. Augustin M, Baade K, Herberger K, et al. Use of the WoundQoL instrument in routine practice: feasibility, validity and development of an implementation tool. Wound Med. 2014;5:4‐8. [Google Scholar]
- 9. Sommer R, Augustin M, Hampel‐Kalthoff C, Blome C. The wound‐QoL questionnaire on quality of life in chronic wounds is highly reliable: wound‐QoL retest reliability. Wound Repair Regain. 2017;25(4):730‐732. [DOI] [PubMed] [Google Scholar]
- 10. Augustin M, Conde Montero E, Zander N, et al. Validity and feasibility of the wound‐QoL questionnaire on health‐related quality of life in chronic wounds. Wound Repair Regen. 2017;25(5):852‐857. [DOI] [PubMed] [Google Scholar]
- 11. Rogers LC, Armstrong DG, Capotorto J, et al. Wound center without walls: the new model of providing care during the COVID‐19 pandemic. Wounds. 2020;9. [PMC free article] [PubMed] [Google Scholar]
- 12. Rogers LC, Lavery LA, Joseph WS, Armstrong DG. All feet on deck—the role of podiatry during the COVID‐19 pandemic: preventing hospitalizations in an overburdened healthcare system, reducing amputation and death in people with diabetes. J Am Podiatr Med Assoc. 2020. 10.7547/20-051. [DOI] [PubMed] [Google Scholar]
- 13. Slagman A, Behringer W, Greiner F, et al. Medical emergencies during the COVID‐19 pandemic—an analysis of emergency department data in Germany. Deutsches Ärzteblatt. 2020;117:545‐552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Barnett ML, Ray KN, Souza J, Mehrotra A. Trends in telemedicine use in a large commercially insured population, 2005‐2017. JAMA. 2018;320(20):2147‐2149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Hong Y‐R, Lawrence J, Williams D, Mainous A III. Population‐level interest and telehealth capacity of US hospitals in response to COVID‐19: cross‐sectional analysis of Google search and National Hospital Survey Data. JMIR Public Health Surveill. 2020;6(2):e18961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Hsieh MW, Lee C, Ou S, Kuo Y. Telemedicine algorithm for chronic wound care during covid‐19. Int Wound J. 2020;17(5):1535‐1537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Shin L, Bowling FL, Armstrong DG, Boulton AJM. Saving the diabetic foot during the COVID‐19 pandemic: a tale of two cities. Dia Care. 2020;43(8):1704‐1709. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.


