Dear Editor,
1.
Cutaneous manifestations of COVID‐19 disease have been widely characterized. Livedo or necrosis pattern, accounting for 6% of cutaneous manifestations, is associated with more severe disease (Galván Casas et al., 2020). It has been related to vascular occlusion secondary to coagulopathy and vascular damage (Zhang et al., 2020). Ischemic lesions due to vasculitis with negative serology has been reported associated to COVID‐19 infection in two scenarios: drug‐induced vasculitis (Vanegas Ramirez et al., 2020) and secondary to COVID‐19 infection itself (Mayor‐Ibarguren et al., 2020). Although practice recommendations on the management of patients requiring microsurgery in times of COVID‐19 have been reported (Hsieh et al., 2020; Ramella et al., 2020), little is known about technical considerations of microsurgical reconstruction in a patient with tissue necrosis secondary to vasculitis COVID‐19 disease.
We describe a patient with COVID‐19 severe disease and vasculitic acro‐ischemic lesions in her right hand that required microvascular free tissue transfer. The patient was diagnosed of COVID‐19 pneumonia on March 2020, on the basis of SARS‐CoV‐2 detected at RT‐PCR testing. One week after the diagnosis, infiltrated erythematous plaque appeared in left buttock, unrelated to contact allergies or decubitus, which spontaneously solved. On April 2020, under low doses of norepinephrine, the patient manifested ischemic signs in right thumb distal phalanx and livedoid lesions in homolateral dorsum of the hand associated to pain (Figure 1(a),(b)). Autoimmunity serological analysis showed negative values for anti‐nuclear antibodies (ANAs), anti‐neutrophil cytoplasmic antibodies (ANCAs) and anticardiolipin antibodies. Component C3 was detected in serum. Biopsy of the hand lesion suggested the diagnosis of COVID‐19 vasculitis.
FIGURE 1.
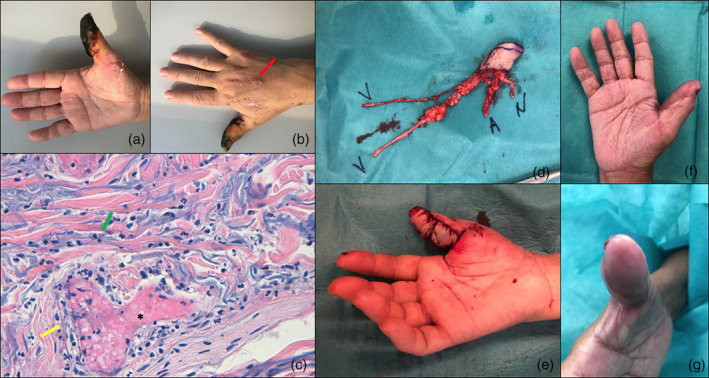
(a,b) Vasculitic lesions appeared during COVID‐19 active disease: acral‐ischemia at right thumb that progressed to necrosis and residual scar at the dorsum of the hand secondary a liveoid lesion (red arrow). (c) High magnification (×40) histologic section of hand lesion biopsy with Hematoxylin and Eosin staining showed perivascular inflammatory infiltrate at dermal vessels (green arrow), with vessel wall thickening (yellow arrow), lumen sclerosis and fibrin thrombus (*). (d,e) Intraoperatively images of the thumb‐tip reconstruction with lateral hemi‐pulp toe transfer. (f,g) Hemi‐pulp toe transfer to right thumb at 8 weeks postoperatively
Thumb lesion progressed to necrosis involving the pulp as proximal as the interphalangeal joint. On May 2020, once necrosis had delimited and patient had recovered from COVID‐19, toe pulp to hand transferred was proposed for thumb reconstruction. Thumb vessels showed no flow and dissection of radial artery at anatomical snuffbox was done to perform the anastomosis. First plantar metatarsal artery (FPMA) was dominant, thus a 6 cm interposed vein graft was required to reach donor artery. The flap was harvested with two 10 cm superficial veins that were anastomosed to superficial venous system after being tunnelized from proximal phalanx to the snuff‐box site (Figure 1(c),(d)). All anastomoses were performed termino‐terminal. The toe lateral digital collateral nerve, included in the flap, was sutured to thumb cubital digital collateral nerve. The postoperative period was uneventful. At 8 weeks postoperatively, all the wounds healed without microsurgical transfer vessel‐related complications (Figure 1(e),(f)).
During COVID‐19 pandemia, microsurgical free‐transfer in patients affected from the disease has been non‐recommended in order to simplify surgery and postoperative management, thus more conservative approach has been suggested in those patients (Ramella et al., 2020). However, surgeons continue attending cases that require microsurgical flaps and cannot be differed. No microsurgical reconstruction in patients with COVID‐19 vasculitic necrosis has been reported. Nonetheless, vasculitic necrosis secondary to other small vessel disease (understood as any pathologic process that damages small end arteries, arterioles, venules, and capillaries), although little, have been published (Battisti et al., 2019; Ikeda et al., 2012; Raurell et al., 2000). It is important to be aware that the underlying vasculitis may not only affect the zone of necrosis, but also the vessels outside this area (Raurell et al., 2000), so the risk of failure of microvascular anastomosis might be increased. The scarce available papers suggest that, although being a challenging scenario in which anticoagulant therapy as well as systemic steroid are essential, vasculitic disease it is not an absolute contraindication to perform a microsurgical reconstruction (Battisti et al., 2019). Besides systemic therapies, in specific cases of small vessel vasculitis as ours, medium‐caliber recipient vessel might provide us a more reliable anastomosis.
To our knowledge, the current case might be the first describing successful microsurgical autotransplant in a patient with COVID‐19 vasculitis‐related acral necrosis. In light of current results, microsurgical reconstructions, although challenging, may be considered in these patients, perhaps because this is a small vessel disease.
CONFLICT OF INTEREST
The authors declare no conflict of interest and no financial disclosure.
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.
REFERENCES
- Battisti, A. , Bracciolini, V. , Terenzi, V. , Cassoni, A. , Fadda, M. T. , & Valentini, V. (2019). Free flaps in head and neck reconstruction in patients affected by vasculitis: To risk or not to risk? Oral Oncology, 90, 145–146. [DOI] [PubMed] [Google Scholar]
- Galván Casas, C. , Català, A. , Carretero Hernández, G. , Rodríguez‐Jiménez, P. , Fernández‐Nieto, D. , Rodríguez‐Villa Lario, A. , Navarro Fernández, I. , Ruiz‐Villaverde, R. , Falkenhain‐López, D. , Llamas Velasco, M. , García‐Gavín, J. , Baniandrés, O. , González‐Cruz, C. , Morillas‐Lahuerta, V. , Cubiró, X. , Figueras Nart, I. , Selda‐Enriquez, G. , Romaní, J. , Fustà‐Novell, X. , … García‐Doval, I. (2020). Classification of the cutaneous manifestations of COVID‐19: A rapid prospective nationwide consensus study in Spain with 375 cases. The British Journal of Dermatology, 183, 71–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hsieh, M.‐C. W. , Lee, C.‐C. , Lu, P.‐L. , & Kuo, Y.‐R. (2020). Covid‐19 guidance algorithm for advanced head and neck cancer reconstruction. Microsurgery, 40(6), 724–725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ikeda, K. , Yotsuyanagi, T. , Arai, K. , Suda, T. , Saito, T. , & Ezoe, K. (2012). Combined revascularization and free‐tissue transfer for limb salvage in a Buerger disease patient. Annals of Vascular Surgery, 26(3), 422.e5–422.e8. [DOI] [PubMed] [Google Scholar]
- Mayor‐Ibarguren, A. , Feito‐Rodriguez, M. , Quintana Castanedo, L. , Ruiz‐Bravo, E. , Montero Vega, D. , & Herranz‐Pinto, P. (2020). Cutaneous small vessel vasculitis secondary to COVID‐19 infection: A case report. Journal of the European Academy of Dermatology and Venereology, 34, e541–e542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramella, V. , Papa, G. , Bottosso, S. , Cazzato, V. , & Arnež, Z. M. (2020). Microsurgical reconstruction in the time of COVID‐19. Microsurgery, 40, 723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raurell, A. , Austin, O. M. , & Ramakrishnan, V. (2000). Free tissue transfer in patients with systemic lupus erythematosus. British Journal of Plastic Surgery, 53(1), 77–79. [DOI] [PubMed] [Google Scholar]
- Vanegas Ramirez, A. , Efe, D. , & Fischer, M. (2020). Drug‐induced vasculitis in a patient with COVID‐19. Journal of the European Academy of Dermatology and Venereology, 34, e361–e362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang, Y. , Cao, W. , Xiao, M. , et al. (2020). Clinical and coagulation characteristics of 7 patients with critical COVID‐2019 pneumonia and acro‐ischemia. Zhonghua Xue Ye Xue Za Zhi., 41(0), E006. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.


