Abstract
The provision of health care in the perioperative setting has undergone significant changes due to severe respiratory distress syndrome coronavirus‐2 (SARS‐CoV‐2). Hospital facilities have been tasked with developing and implementing personal protective equipment (PPE) protocols to protect both medical providers and patients. Texas Children's Hospital has created a set of protocols for donning and doffing PPE while managing surgical pediatric patients. These requirements have undergone numerous modifications as a result of our internal infrastructural recommendations and the Centers for Disease Control and Prevention guidance, which has led to more lenient regulations. While these perioperative PPE protocols were less stringent compared to the original guidelines, we were able to create a safe surgical environment without further exposing patients and health care providers to SARS‐CoV‐2. In this article, we detail the design, distribution, implementation, and modification of our institutional surgical PPE protocols.
INTRODUCTION
Coronavirus disease 2019 (COVID‐19) has tested the resilience of health care systems on a global scale. Severe acute respiratory syndrome coronavirus‐2 (SARS‐CoV‐2), the infectious agent of COVID‐19, was first identified in Wuhan, China on December 31st, 2019. In only a few months, the virus resulted in a pandemic that was declared by the World Health Organization on March 11th, 2020. 1 As of October 21st, 2020, it has infected nearly 41 million people with over 1.12 million deaths worldwide. 2 The United States leads all countries in COVID‐19 cases with the state of Texas trailing only California. 3 Moreover, the greater Houston area ranks fourth in the nation in confirmed cases. 4
The detrimental effects of COVID‐19 are more commonly observed in adult patients, though children can also display symptoms. While uncommon, pediatric patients infected with SARS‐CoV‐2 can develop severe sequelae such as multisystem inflammatory syndrome in children and adolescents. 5 Because of COVID‐19's ubiquitous impact, hospital systems have followed strict personal protective equipment (PPE) guidelines to minimize viral transmission within the hospital for both health care staff and patients. 6 , 7 , 8
Texas Children's Hospital (TCH), the largest pediatric hospital in the nation, resides within the Texas Medical Center (TMC) in the city of Houston. With a staggering number of patients having presented with SARS‐CoV‐2 infection within the TMC, health care professionals are being challenged to maintain quality patient care while following appropriate safety measures. Medical providers are at higher risk of contracting SARS‐CoV‐2 while managing COVID‐19 patients given the prevalence of both nosocomial and asymptomatic infections. 8 , 9 , 10 , 11 , 12 , 13 It has also been reported that SARS‐CoV‐2 can remain aerosolized for up to 3 h and remain on surfaces such as stainless steel and plastic for 72 h if not properly cleaned. 14 More stringent regulations regarding use of PPE have contributed to an appreciable reduction in cases associated with hospital staff. 15 However, while it has been shown that PPE can minimize transmission of the virus, the extent to which PPE should be utilized to safely protect health care providers and patients is a topic of debate in the literature. 8
TCH has been at the forefront of the COVID‐19 pandemic, which has provided us a unique experience managing surgical patients with PPE. The process of designing and implementing PPE protocols, however, has not come without its own set of difficulties. In accordance with the Centers for Disease Control and Prevention (CDC) guidance, governmental regulations, and our internal infrastructural recommendations, we have undergone numerous modifications to provide a safe environment for all members within our institution. Consequently, in this report we will discuss the evolution of our surgical PPE protocols, describe their distribution within our institution, and delineate the major lessons learned from this experience.
PERSONAL PROTECTIVE EQUIPMENT
On April 2nd, 2020, our institution put forth its first protocols that were initially created to handle an Ebola crisis. The basic PPE requirements included donning double gloves, a gown, an N95 mask, and eye protection. In addition to these measures, surgical staff were instructed to don shoe covers and a surgical mask over the N95 respirator. If an individual who had failed fit testing was required to be in the procedure, a controlled‐air‐purifying respirator was worn prior to entering the operating room (Figure 1). The surgical team was also originally monitored through the donning and doffing process by a designated observer who was also obligated to wear full PPE. During the doffing process, the observer was responsible for dispensing hand sanitizer on the gloves before removing them to prevent contamination. Upon completion of the surgical procedure, a protective drape was placed on the floor within the operating room for all surgical personnel to dispose of their PPE. All waste was then placed in a biohazard bag following any surgical procedure. Lastly, it was mandated that the surgical team members shower after completion of each operation.
Figure 1.
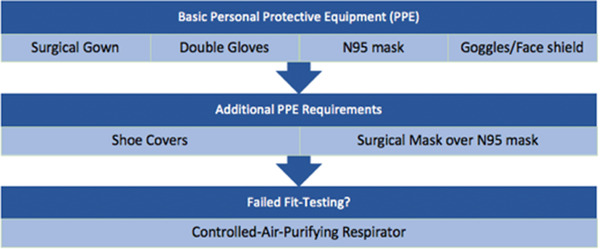
Original personal protective equipment (PPE) requirements at our institution
At the beginning of the pandemic, our institution enforced a “runner” system in which we designated an individual to help provide any additional PPE and surgical equipment that were requested by the surgical team. During the months of March and April, this runner, who had no direct patient contact, remained outside of the operating room and maintained full PPE coverage to minimize any potential risk of exposure. With new and adapted information distributed almost daily from the CDC, staff members felt compelled to follow strict PPE rules regardless of direct exposure to patients and their preoperative screening results.
While it was imperative to develop and implement PPE protocols to protect our health care workers and patients, we aimed to design a more efficient system without compromising on safety. As we looked within our internal infrastructure combined with changing guidelines from the CDC, we continued to modify our initial approach to create a more robust and efficient system while still maintaining proper precautions. Specific changes to our protocols included eliminating the mandated use of shoe covers and an additional surgical mask over an N95. It was also not required for the observer to wear full PPE, and the dispensing of hand sanitizer was no longer necessary prior to doffing gloves. Furthermore, the team did not have to discard their PPE on a protective drape nor did they have to place the disposable items within a biohazard bag at the end of the surgical procedure. Perioperative personnel were also not mandated to shower following each case. Lastly, the runner was only required to don a surgical mask and goggles. Many of these modifications have led to our current donning and doffing protocol for perioperative care designed and utilized by our providers.
Donning and doffing
The anesthesiology department at TCH has devised a performance checklist for all providers to follow to ensure proper safety precautions in donning and doffing PPE. When this checklist was originally implemented, the observer was required to examine the donning and doffing process of all members caring for this patient population including surgeons, anesthesiologists, nurses, and surgical technicians. However, as the providers became more familiar with the requirements, a collective team approach has been adopted in which members observe each other don and doff PPE.
The sequential order in which this protocol is executed is crucial to reduce the risk of intraoperative transmission (Table 1). To begin, all jewelry and personal items must be removed prior to entering the operating room. Team members then don gloves after they perform hand hygiene. Afterwards, isolation gowns are worn and tied in the back. Importantly, the gloves are placed under the sleeve of the gown. Health care providers then don an N95 mask, followed by goggles or a face shield for eye protection. To complete the donning process, a second set of gloves are placed over the sleeve of the gown. It should be noted that double gloving is standard in the operating room when at risk of contact with blood or other bodily fluids.
Table 1.
PPE donning: Special isolation practices for COVID‐19
| Donning procedure steps | Description |
|---|---|
| Remove jewelry and personal items | |
| Perform hand hygiene | Use soap and water OR hand sanitizer for at least 15 s |
| Don first set of gloves | Place under the sleeve of the gown |
| Don surgical gown | Tie in the back |
| Don N95 mask and eye protection (goggles or face shield) and adjust to fit |
Secure the two elastic bands at crown of head and base of neck Fit flexible band to bridge of nose with two fingers on each side Perform seal check to confirm mask is appropriately seated on face |
| Don second set of gloves | Place over the sleeve of the gown |
The doffing procedure outlined for health care workers at TCH occurs both within and outside of the operating room (Table 2). While still in the operating room, team members should first remove their surgical gowns and discard into the trash receptacle. The gloves should be peeled off at the same time the gown is removed. After performing hand hygiene, medical personnel can then leave the operating room with the only remaining PPE being eye protection and the N95 mask. Once outside the operating room, hand hygiene is performed again. Eye protection can then be removed, and the face shield or goggles should be placed in the designated contaminated area for future cleaning. Hand hygiene is performed prior to removal of the N95 mask. After removing the respirator, hand washing should be performed one last time to complete the doffing process.
Table 2.
PPE doffing: Special isolation practices for COVID‐19
| Doffing procedure steps | Description | |
|---|---|---|
| *Inside of operating room* | Remove surgical gown |
Break tie in the back Grasp gown in front and pull away from body Fold and roll gown inside out during removal Discard into trash receptacle *Peel off gloves at the same time as gown removal, only touching the inside of the gloves and gown |
| Doff gloves | Remove gloves using glove in glove technique if gloves are not removed with gown | |
| Perform hand hygiene | Use soap and water OR hand sanitizer for at least 15 s | |
| Leave operating room with the only remaining PPE being N95 mask and eye protection | ||
| *Outside of operating room* | Perform hand hygiene | Use soap and water OR hand sanitizer for at least 15 s |
| Remove eye protection (goggles or face shield) |
Remove by grasping only the strap in back Lean forward and do not touch face Place face shield/goggles in designated contaminated area for future cleaning |
|
| Perform hand hygiene | Use soap and water OR hand sanitizer for at least 15 s | |
| Remove N95 mask | Touch straps in back only and discard into trash receptacle | |
| Perform hand hygiene | Use soap and water OR hand sanitizer for at least 15 s |
Patient transportation
There is a risk of transmission of SARS‐CoV‐2 infection from symptomatic or confirmed cases during patient transportation within and between facilities. Few studies have proposed recommendations for health care workers to follow during patient transport, but we have designed a simple protocol to help guide those involved in this process. 16 , 17 , 18
If a patient is under investigation or has tested positive for SARS‐CoV‐2, efforts should be made to transport the patient directly to the operating room, bypassing the preoperative area and Post‐Anesthesia Care Unit (PACU) when possible to minimize any additional exposure to staff and patients. The medical team involved should don a gown, gloves, eye protection, and N95 respirator to prepare the patient for transport. Once ready for transport, the providers should remove their gloves and gown. After exiting the room, one member should replace the gloves and gown with a new pair to help with transport while a second individual should maintain the N95 respirator and eye protection to manage doors or elevators. Nonintubated patients are required to wear a surgical mask, while a high‐efficiency particulate air filter is required for intubated patients.
Cleaning protocol
Our PPE protocol had to account for operating room staff who were responsible for cleaning surfaces following a surgical procedure. If cleaning within the operating room takes place at least 30 min after patient discharge, minimum PPE requirements include gloves and an isolation gown, as air is recycled quickly within the operating room making it appropriate for working personnel to enter safely. Eye protection and a surgical mask should also be donned if there is a risk of spray or splatter. If cleaning takes place within 30 min after patient discharge, PPE that should be worn include gloves, an isolation gown, and an N95 respirator. Again, eye protection may also be necessary.
TCH has also designed a cleaning protocol for the preoperative holding area and PACU. Akin to the cleaning guidelines outlined for the operating room, all items in the patient's room should be disinfected or disposed of if unable to be disinfected. PPE requirements within negative pressure isolation or treatment rooms are similar to those within the procedural suites and are dependent on whether cleaning occurs at least 30 min after patient discharge with no aerosol‐generating procedures (AGPs) performed or if cleaning occurs within 30 min and an AGP is performed. In all other rooms, PPE requirements are analogous to those in procedural suites dependent on whether cleaning occurs at least 1 h after patient discharge or if cleaning takes place within 1 h after the patient leaves.
CONSERVATION OF PERSONAL PROTECTIVE EQUIPMENT
A fine balance is required in order to conserve PPE while also utilizing enough PPE to prevent further spread of SARS‐CoV‐2. Our institution limited the surgical procedures performed to only urgent and emergent cases and reduced the number of medical personnel allowed in the operating room. As we are a teaching institution, there are numerous learners and surgical residents who partake in educational experiences within the operating room at TCH. To minimize health care workers within the operating room while also not compromising on patient safety, a limited number of residents and no students were allowed to assist or shadow essential medical personnel. In addition to these measures, our administration assembled a supply chain designed to serve as a checks and balances system to ensure that N95 masks were readily available when operating on a COVID‐19 positive patient. N95 masks are a single‐use item, but this has been reconsidered in light of the current pandemic. Consequently, a multidisciplinary team was also formed to create a decontamination protocol to allow for the reuse of N95 masks. Our institution looked at ways to systematically process these respirators safely, and designed a protocol in the event that our institution needed to conserve N95 masks using either a STERRAD gas plasma sterilizer or germicidal ultraviolet light. 19 , 20 Though this operation was never executed due to our early efforts of conserving PPE through cancelation of surgical procedures and limited numbers of medical personnel in the operating room, we were prepared to implement our plan at any moment.
COMMUNICATION
A major concern recognized early during the COVID‐19 pandemic was a lack of effective communication from a centralized source, which resulted in disorganization with regards to information distribution. At our institution, one person within perioperative leadership was initially tasked with updating the PPE protocols. Updates were released almost daily via email, which contributed to further confusion. This proved to be an unsustainable method for educating teams on the evolving PPE guidelines. While email updates remained a method for communication, leadership rectified this setback by creating a central repository to which all staff employees had access. Perioperative leadership formed and implemented a version control team dedicated to updating this centralized source of information. The current documents were able to be accessed from any location within the hospital using this platform (Figure 2).
Figure 2.
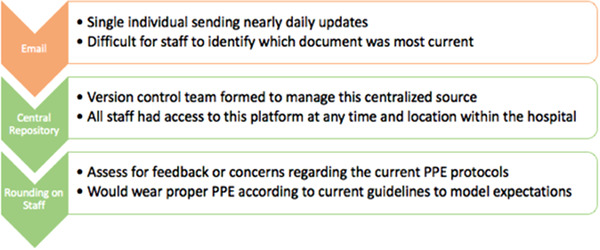
Timeline illustrating the modifications and new additions to our communication process in distributing updated information regarding PPE protocols
Perioperative leadership assumed an active role in modifying and distributing these protocols apart from technological means. At the beginning of the COVID‐19 pandemic, the hospital staff were at times understandably hesitant with the ever‐changing adjustments to the institutional PPE protocols. Perioperative leadership would round on hospital employees to evaluate for any feedback or concerns regarding present PPE regulations. Additionally, administrative leaders would speak with perioperative staff about the modifications implemented to the PPE protocols and discuss the importance of PPE in minimizing the risk of nosocomial transmission. This was particularly critical when the guidelines appeared to become more lenient compared to the original regulations. By also modeling the PPE requirements that were requested by perioperative leadership while interacting with staff, medical providers had more trust and confidence in our hospital system and the protocols proposed.
SUMMARY
Throughout the COVID‐19 pandemic, health care facilities have had to reexamine their approach to the use of personal protective equipment in the perioperative setting. TCH has remained at the forefront of innovation in this regard because of the impact that SARS‐CoV‐2 has had on the city of Houston. It was imperative to have various modes of communication to ensure that our hospital staff felt comfortable and confident with the evolving nature of our institutional PPE protocols in addition to upholding appropriate safety measures for providers and patients alike. Furthermore, by modeling the proper PPE requirements delineated through these communication pathways and by actively discussing these protocols with providers, perioperative leadership provided reassurance and trust, which has resulted in quality patient care. While our circumstances at TCH are unique, we hope that other health care facilities can benefit by learning from our experience of designing an efficient system that is also safe.
Biographies
Rami P. Dibbs, BA, is a medical student at Louisiana State University Health Science Center (LSUHSC) in New Orleans undertaking a research fellowship at Texas Children's Hospital in Houston, TX. He graduated with a bachelor's degree in chemistry from Rice University in Houston, TX. Rami is interested in pursuing a career in plastic and reconstructive surgery and is excited to continue to develop his passion in this field through his research endeavors and future clinical experience.
Andrew M. Ferry, BS, is a fourth‐year medical student at the University of Texas Medical Branch in Galveston (UTMB) undertaking a research fellowship at Texas Children's Hospital in Houston, TX. Andrew graduated with a bachelor's degree in biological sciences with honors from Louisiana State University in Baton Rouge, LA. During his third and fourth years of medical school, Andrew discovered his passion for pediatric plastic surgery with a particular interest in craniofacial surgery and plans on pursuing a career in the field.
Joyce Enochs, BSN, RN, CNOR, is the children's surgery program manager for Texas Children's Hospital in Houston, TX. Joyce is a bachelor's prepared registered nurse with over 10 years of experience in a variety of surgical settings who currently holds the Certified Nurse Operating Room Professional Certification. As children's surgery program manager for Texas Children's Hospital, she works collaboratively with the department of surgery administrators, physicians, and perioperative services leadership to ensure exceptional delivery of care by continuously improving quality processes and standards.
Amanda Ward, BSN, MBA, CNOR, serves as the director of perioperative services at Texas Children's Hospital in Houston, TX. She received her bachelor's of science in nursing from Prairie View A&M University and her master's of business administration from Texas Woman's University where she was inducted into Phi Kappa Phi for her academic excellence. Among her many accolades, she received the 2017 Mark A. Wallace Catalyst Leader of the Year at Texas Children's Hospital in 2017, Bronze Nursing Excellence Award in 2018, and was the commencement address speaker for Texas Women's University in 2018.
Chris D. Glover MD, FAAP, is division director for anesthesia services at both Texas Children's Hospital Katy campus and Texas Children's Hospital Woodlands Campus. These campuses are part of the Texas Children's department of anesthesiology, which is a national leader in clinical care, quality, and safety outcomes. Dr. Glover practices and preaches multimodal pain control centered on a philosophy that pain in children should be minimized or eliminated if possible. His research's focus centers on pediatric pain control with a specific emphasis on pediatric regional anesthesia and multicenter large data warehousing to determine best methods of care for the pediatric patient undergoing complex pediatric surgery. Nationally, Dr. Glover sits on the communications committee for the Society of Pediatric Anesthesiology. He is also a delegate for the Texas Society of Anesthesiologists and sits on the practice advisory committee for that organization.
Nakeisha Archer, MBA, RN, NE‐BC, CNOR, CSSM, has over 23 years of nursing and formal leadership experience in various progressive roles and has led several hospital teams successfully. Nakeisha has a master's degree in business and health care management, and is in the process of obtaining her DNP. She is currently in an organization that has many change initiatives underway at which she is leading teams to integrate perioperative services policies, procedures, and standards in everyday practice. She is a member of the national board of directors for the Association of periOperative Registered Nurses, and works to be on the cusp of change and innovation in all that she does.
Kimberly D. Taylor, RN, BSN, MBA, works as the quality improvement specialist for the department of anesthesiology, perioperative, and pain management at Texas Children's Hospital in Houston, TX. Prior to this role, she has overseen nursing care in the post anesthesia care unit at Texas Children's Hospital, where she received, “2017 Excellence in Nursing, Bronze Award.” She earned her bachelor of science degree from Old Dominion University and her master of business degree from the University of Phoenix.
Judy Almaguer‐Bravo, MBA, currently serves as the manager of the anesthesia support staff at Texas Children's Hospital in Houston, TX. Her responsibilities include oversight of the pediatric anesthetizing locations within the operating room and nonoperating room units. Prior to this role, she led the perioperative care technician staff in the daily support operations in the main operating room at Texas Children's Hospital. She earned her bachelor of science degree from the University of Houston (Main); and master of business/health care administration degree from Texas Woman's University, where she was inducted to the Golden Key International Honour Society.
Larry H. Hollier, Jr., MD, FACS, FAAP, is a board‐certified plastic surgeon who specializes in plastic and reconstructive surgery, including cleft lip and palate, pediatric craniofacial, and hand surgery. Dr. Hollier is a professor of plastic surgery, orthopedic surgery, and pediatrics at Baylor College of Medicine and is the surgeon‐in‐chief at Texas Children's Hospital and chief of plastic surgery at Baylor College of Medicine. He serves on the board of the Duke Global Health Institute and as chairman of the medical advisory board for Smile Train. He has authored more than 250 articles for scholarly and professional publications, written 37 book chapters, and made dozens of presentations to professional audiences worldwide on a full range of topics related to plastic and reconstructive surgery. Dr. Hollier is on the editorial boards of numerous scientific journals including serving as the section editor for pediatric and craniofacial surgery for Plastic and Reconstructive Surgery. In 2016, Dr. Hollier was named the Press Ganey Physician of the Year for his leadership in improving the patient experience at Texas Children's Hospital.
REFERENCES
- 1. WHO . WHO Director‐General's opening remarks at the media briefing on COVID‐19, 11 March 2020. https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020. Accessed October 21, 2020.
- 2. WHO . WHO coronavirus disease (COVID‐19) dashboard. https://covid19.who.int/table Accessed October 21, 2020.
- 3. Johns Hopkins University and Medicine. Texas ‐ COVID‐19 overview—Johns Hopkins. https://coronavirus.jhu.edu/region/us/texas Accessed October 21, 2020.
- 4. Johns Hopkins University and Medicine. COVID‐19 United States cases by county—Johns Hopkins Coronavirus Resource Center. Accessed October 21, 2020. https://coronavirus.jhu.edu/us-map
- 5. Whittaker E, Bamford A, Kenny J, et al. Clinical characteristics of 58 children with a pediatric inflammatory multisystem syndrome temporally associated with SARS‐CoV‐2. JAMA ‐ J Am Med Assoc. 2020;324(3):259‐269. 10.1001/jama.2020.10369 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Baker TL, Greiner J V., Maxwell‐Schmidt E, Lamothe PH, Vesonder M. Guidelines for frontline health care staff safety for COVID‐19. J Prim Care Community Heal. 2020;11. 10.1177/2150132720938046 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Parikh SR, Avansino JR, Dick AA, et al. Collaborative multidisciplinary incident command at Seattle children's hospital for rapid preparatory pediatric surgery countermeasures to the COVID‐19 pandemic. J Am Coll Surg. 2020;231(2):269‐274.e1. 10.1016/j.jamcollsurg.2020.04.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Stewart CL, Thornblade LW, Diamond DJ, Fong Y, Melstrom LG. Personal protective equipment and COVID‐19: a review for surgeons. Ann Surg. 2020;272(2):e132‐e138. 10.1097/SLA.0000000000003991 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Wang D, Hu B, Hu C, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus‐infected pneumonia in Wuhan, China. JAMA ‐ J Am Med Assoc. 2020;323(11):1061‐1069. 10.1001/jama.2020.1585 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Nguyen LH, Drew DA, Graham MS, et al. Risk of COVID‐19 among front‐line health‐care workers and the general community: a prospective cohort study. 2020; 5(9):E475‐E483 10.1016/S2468-2667(20)30164-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Rickman HM, Rampling T, Shaw K, et al. Nosocomial transmission of coronavirus disease 2019: a retrospective study of 66 hospital‐acquired cases in a London teaching hospital. Clin Infect Dis. 2020. 10.1093/cid/ciaa816 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Carter B, Collins JT, Barlow‐Pay F, et al. Nosocomial COVID‐19 infection: examining the risk of mortality. The COPE‐Nosocomial study (COVID in older people). J Hosp Infect. 2020;106(2):376‐384. 10.1016/j.jhin.2020.07.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Wang Y, Kang H, Liu X, Tong Z. Asymptomatic cases with SARS‐CoV‐2 infection. J Med Virol. 2020;92(9):1401‐1403. 10.1002/jmv.25990 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Van Doremalen N, Bushmaker T, Morris DH, et al. Aerosol and surface stability of SARS‐CoV‐2 as compared with SARS‐CoV‐1. N Engl J Med. 2020;382(16):1564‐1567. 10.1056/NEJMc2004973 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Wang X, Pan Z, Cheng Z. Association between 2019‐nCoV transmission and N95 respirator use. J Hosp Infect. 2020;105(1):104‐105. 10.1016/j.jhin.2020.02.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Evans HL, Thomas CS, Bell LH, et al. Development of a sterile personal protective equipment donning and doffing procedure to protect surgical teams from SARS‐CoV‐2 exposure during the COVID‐19 pandemic. Surg Infect (Larchmt). 2020;21(8):671‐676. 10.1089/sur.2020.140 [DOI] [PubMed] [Google Scholar]
- 17. Liew MF, Siow WT, MacLaren G, See KC. Preparing for CovID‐19: early experience from an intensive care unit in Singapore. Crit Care. 2020;24(1). 10.1186/s13054-020-2814-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Yousuf B, Sujatha KS, alfoudri H, Mansurov V. Transport of critically ill COVID‐19 patients. Intensive Care Med. 2020;46(8):1663‐1664. 10.1007/s00134-020-06115-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Lindsley WG, Martin SB, Thewlis RE, et al. Effects of ultraviolet germicidal irradiation (UVGI) on N95 respirator filtration performance and structural integrity. J Occup Environ Hyg. 2015;12(8):509‐517. 10.1080/15459624.2015.1018518 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Jatta M, Kiefer C, Patolia H, et al. N95 reprocessing by low temperature sterilization with 59% vaporized hydrogen peroxide during the 2020 COVID‐19 pandemic. Am J Infect Control. 2020. 10.1016/j.ajic.2020.06.194 [DOI] [PMC free article] [PubMed] [Google Scholar]


