Abstract
BACKGROUND
Irritable bowel syndrome (IBS) is a common functional gastrointestinal disorder. Dysregulation of the gut–brain axis plays a central role in the pathophysiology of IBS. It is increasingly clear that the microbiome plays a key role in the development and normal functioning of the gut–brain axis.
AIM
To facilitate the identification of specific areas of focus that may be of relevance to future research. This study represents a bibliometric analysis of the literature pertaining to the microbiome in IBS to understand the development of this field.
METHODS
The data used in our bibliometric analysis were retrieved from the Scopus database. The terms related to IBS and microbiome were searched in titles or abstracts within the period of 2000–2019. VOSviewer software was used for data visualization.
RESULTS
A total of 13055 documents related to IBS were retrieved at the global level. There were 1872 scientific publications focused on the microbiome in IBS. There was a strong positive correlation between publication productivity related to IBS in all fields and productivity related to the microbiome in IBS (r = 0.951, P < 0.001). The United States was the most prolific country with 449 (24%) publications, followed by the United Kingdom (n = 176, 9.4%), China (n = 154, 8.2%), and Italy (n = 151, 8.1%). The h-index for all retrieved publications related to the microbiome in IBS was 138. The hot topics were stratified into four clusters: (1) The gut–brain axis related to IBS; (2) Clinical trials related to IBS and the microbiome; (3) Drug-mediated manipulation of the gut microbiome; and (4) The role of the altered composition of intestinal microbiota in IBS prevention.
CONCLUSION
This is the first study to evaluate and quantify global research productivity pertaining to the microbiome in IBS. The number of publications regarding the gut microbiota in IBS has continuously grown since 2013. This finding suggests that the future outlook for interventions targeting the gut microbiota in IBS remains promising.
Keywords: Irritable bowel syndrome, Bibliometric, Microbiota, Microbiome, Scopus, Brain gut axis
Core Tip: This is the first study to evaluate and quantify the global research productivity pertaining to the microbiome in irritable bowel syndrome (IBS). We present a holistic picture of this emerging topic and explore future research directions. A number of abnormalities have been described within the microbiome of patients with IBS. The relationships of these abnormalities to the causality of dysfunction and associated symptomatology have not been clearly elucidated. Our finding, while preliminary, suggests that the future outlook for interventions targeting the gut microbiota in IBS remains promising.
INTRODUCTION
Irritable bowel syndrome (IBS) is a term used to describe a group of symptoms, including abdominal pain and altered bowel habits, that arises because of disturbances of the interactions between the diet, the brain, the gut, and the microbiome. IBS poses a significant disease burden, with 20% of adults estimated to develop IBS symptoms in any given year. Symptoms arise as a consequence of abnormal visceral sensation and or motility as a result of abnormalities within the enteric or central nervous systems, or both[1]. This usually occurs in the absence of ‘organic’ disease, but the association with other gastrointestinal diseases is common. Many patients experiencing gastrointestinal inflammation due to infection or inflammatory bowel disease develop IBS symptoms[2]. Nearly a quarter of patients with IBS without identifiable ‘organic’ disease appear to have low-grade intestinal inflammation as judged by faecal inflammatory markers (calprotectin)[3]. Inflammation may lead to sensitization of peripheral nerves. Most inflammation within the gastrointestinal tract settles, but in susceptible individuals sensitization of peripheral afferents may persist. Such sensitization may be driven by ongoing mast cell activation and increased epithelial permeability associated with low-level inflammation[4].
The onset of symptoms in IBS is often associated with psychological stressors. A high proportion of people with IBS have psychological comorbidities. Chronic stress is associated with stress-induced hyperalgesia. This hyperalgesia is mediated via corticotrophin-releasing hormone and the hypothalamic–pituitary axis (HPA)[5]. Dysfunction within these systems is well documented in patients with functional gastrointestinal disorders and other chronic pain syndromes. Furthermore, many patients have histories of traumatic events in early life. These events may result in changes that profoundly affect the microbiome and brain development, predisposing patients to visceral pain syndromes[6-8]. In addition to direct effects on neurons proximal to the bowel, bacteria and their products have a profound effect on the development and activity of the central nervous system and, consequently, upon the psychological state and behaviors[9]. Within the enteric nervous system, certain bacterial strains may directly promote sensitization or downregulation of peripheral afferents. Of note, low-grade inflammation seen in a proportion of patients with IBS may result from the ability of specific bacteria to enhance the production and the effects of proinflammatory cytokines. Bacteria may also be able to transmit signals via the enteric nervous and immune systems to the central nervous system[10].
Although several bibliometric studies have been conducted to evaluate research productivity regarding various research aspects in the medical field[11-18], and some bibliometric studies have focused on microbiota science[19-25], there has not been an assessment of the research output regarding the microbiome in IBS. This study undertakes a bibliometric analysis of the literature within this field to understand the development of the literature pertaining to the microbiome in IBS and to facilitate the identification of specific areas of focus that may be of relevance to future research. This study evaluates data that will help to address the research gaps in this field. The current bibliometric study plays a significant role for researchers interested in the relationship between the microbiome and IBS, because it offers a quick reference guide for interdisciplinary researchers to know how this field has been assessed by scientific experts in previous years.
MATERIALS AND METHODS
The data used in our bibliometric analysis were retrieved from Scopus, which is a multidisciplinary database owned by Elsevier and is considered the largest and most widely used database[26-28]. Most of the publications in this field were published between 2000 and 2019. The following term combinations were searched in the title or abstract within this period: Terms related to IBS, i.e., ‘adaptive colitis’ OR ‘colon spasm’ OR ‘functional bowel disease’ OR ‘irritable bowel’ OR ‘irritable colon’ OR ‘membranous colitis’ OR ‘mucous colitis’ OR ‘spastic colitis’ OR ‘spastic colon’ OR ‘spastic bowel’ OR ‘functional colonic disease’ OR ‘colon irritable’ OR ‘colon neurosis’ OR ‘bowel neurosis’ OR ‘functional colopathy’ OR ‘functional colonopathy’ OR ‘chronic catarrhal colitis’ OR ‘colica mucosa’ OR ‘colonic enterospasm’ OR ‘dyskinesia of the colon’ OR ‘dyssynergia of the colon’ OR ‘functional enterocolonopathy’ OR ‘functional diarrhea’ OR ‘Glarry enteritis’ OR ‘glutinous diarrhea’ OR ‘intestinal croup’ OR ‘irritable gut syndrome’ OR ‘lienteric diarrhea’ OR ‘Membranous catarrh of the intestine’ OR ‘mucomembranous colic’ OR ‘myxoneurosis’ OR ‘nervous diarrhea’ OR ‘neurogenic mucous’ OR ‘nonspecific diarrhea’ OR ‘tubular diarrhea’ OR ‘unhappy colon’ OR ‘unstable colon’, and terms related to microbiome, i.e., ‘microbiome’ OR ‘microflora’ OR ‘microbiota’ OR ‘flora’ OR ‘probiotic’ OR ‘Saccharomyces’ OR ‘Lactobacillus’ OR ‘Bifidobacterium’ OR ‘Escherichia coli’. The terms were selected from related reviews on IBS[29,30] and the microbiome[19,20,31-33].
Data analysis
Microsoft Excel was used to analyze the retrieved data to calculate frequencies and percentages. The current bibliometric study included quantitative data about document types, language, country of the publications with their h-index and collaboration pattern, authors of the publications, journals that published papers on IBS, microbiome documents, and citation reports. In addition, we used the Statistical Package for the Social Sciences 16.0 software for Windows to assess the correlation between yearly quantitative distributions of publications related to IBS in all fields and publications related to the microbiome in IBS by using the Pearson correlation test. Analysis with P < 0.05 is considered statistically significant. In addition, the VOSviewer program[34,35] was used for mapping and clustering terms according to their occurrence in both titles and abstracts to determine hot topics in this field. Furthermore, network visualization maps for collaboration among the most productive countries and the most prolific authors in this field were prepared using VOSviewer.
RESULTS
A total of 13055 documents related to IBS in titles and abstracts were retrieved over the period of 2000–2019 at the global level. There were 1872 scientific publications focused on the microbiome in IBS. The research findings showed that English was the main research language of documents indexed in Scopus, accounting for 48.8% of the documents, followed by German (3.9%) and Chinese (2.9%). Articles were the main type of document for publications related to the microbiome and IBS, accounting for 51.9% of documents, followed by reviews (35.3%).
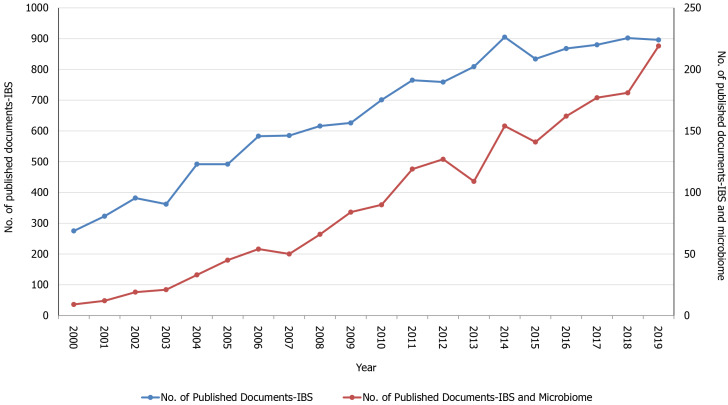
The number of publications related to the microbiome in IBS has increased year by year. The quantity of documents has increased each year, from 9 documents in 2000, to 84 documents in 2009, to 219 documents in 2019 (Figure 1). Published papers during the last 5 years (2015 to 2019) accounted for 47.0% of the total publications. There was a strong positive correlation between the publication productivity related to IBS in all fields and the productivity related to the microbiome in IBS (r = 0.951, P < 0.001).
Figure 1.
The annual number of publications related to irritable bowel syndrome and the microbiome from 2000 to 2019. IBS: Irritable bowel syndrome.
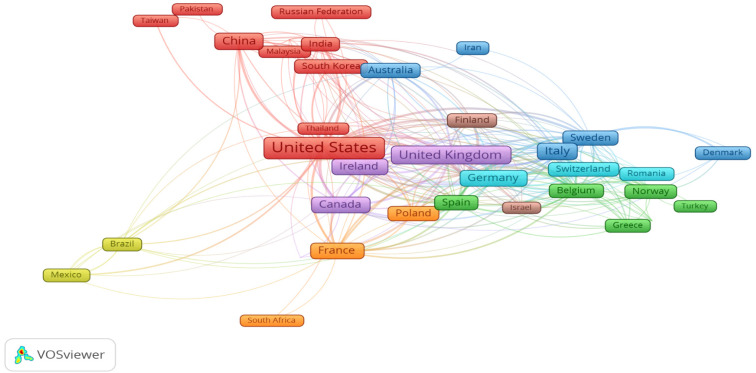
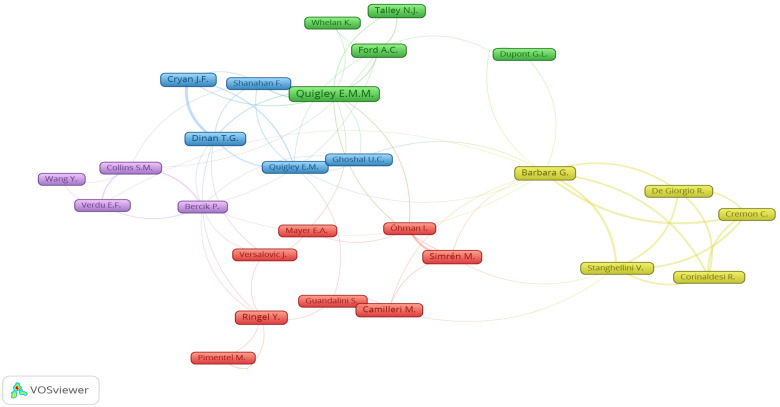
In total, authors from 105 countries published their work on the microbiome and IBS topics. Table 1 lists the top 10 most prolific countries. The United States was the most prolific country with 449 (24%) publications, followed by the United Kingdom (n = 176, 9.4%), China (n = 154, 8.2%), and Italy (n = 151, 8.1%). The h-index for all retrieved publications related to the microbiome in IBS was 138. Figure 2 shows the network visualization map for the collaboration among the 40 most productive countries. This includes countries that published more than 5 papers on microbiome and IBS research according to the number of publications in the last two decades (2000–2019). The United States and the United Kingdom can be referred to as central countries for this network because they published research in collaboration with 40 and 31 countries, respectively. In total, 5960 authors published their work on the microbiome and IBS topics. Figure 3 shows the network visualization map for the collaboration among the 32 most productive authors (authors who published more than 10 papers) on the microbiome in IBS research according to the number of publications in the last two decades (2000–2019). EMM Quigley (United States), G Barbara (Italy), JF Cryan (Ireland), and TG Dinan (Ireland) can be considered the prolific authors of this network due to the fact that they published 61, 25, 25, and 23 documents, respectively.
Table 1.
Top 10 most productive countries on the microbiome in irritable bowel syndrome research, ranked by the total number of publications in the last two decades (2000-2019)
|
SCR
|
Country
|
Number of documents
|
%
|
| 1st | United States | 449 | 24.0 |
| 2nd | United Kingdom | 176 | 9.4 |
| 3rd | China | 154 | 8.2 |
| 4th | Italy | 151 | 8.1 |
| 5th | France | 116 | 6.2 |
| 6th | Germany | 107 | 5.7 |
| 7th | Canada | 103 | 5.5 |
| 8th | Ireland | 102 | 5.4 |
| 9th | Australia | 72 | 3.8 |
| 10th | Spain | 69 | 3.7 |
SCR: Standard competition ranking.
Figure 2.
Network visualization map for the collaboration among the 40 most productive countries on the microbiome in irritable bowel syndrome research according to the number of publications in the last two decades (2000–2019).
Figure 3.
Network visualization map for the collaboration among the 32 most productive authors on the microbiome in irritable bowel syndrome research according to the number of publications in the last two decades (2000–2019).
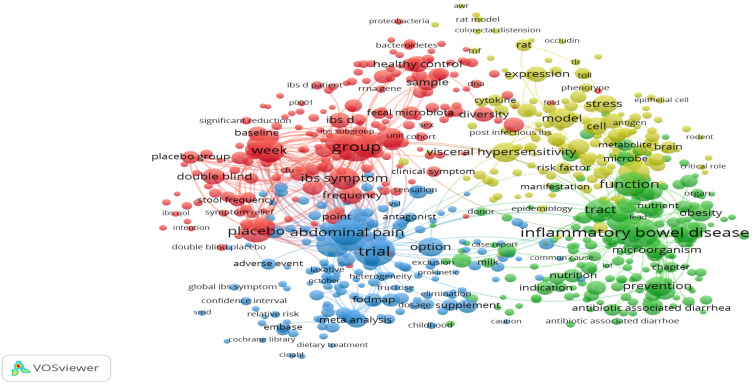
Terms were extracted from the titles and abstracts of all retrieved publications related to the microbiome in IBS and analyzed by the VOSviewer software to identify the current state and hot topics in this field. Terms appearing more than 10 times were included in the map (Figure 4) and were stratified into four clusters: IBS related to the gut–brain axis (yellow cluster), clinical trials related to IBS and the microbiome (red cluster), drug-mediated manipulation of the gut microbiome (blue cluster), and the role of the altered composition of intestinal microbiota in IBS prevention (green cluster).
Figure 4.
Network visualization map for the terms with high co-occurrence frequencies, based on the titles and abstracts of documents related to the microbiome in irritable bowel syndrome research published in the last two decades (2000–2019).
The top 10 journals accounted for 19.98% of all articles (Table 2). The four journals that published the most studies related to microbiome and IBS were World Journal of Gastroenterology (n = 70), Alimentary Pharmacology and Therapeutics (n = 54), Neurogastroenterology and Motility (n = 52), and the Journal of Clinical Gastroenterology (n = 39).
Table 2.
Top 10 most productive journals on the microbiome in irritable bowel syndrome research, ranked by the total number of publications in the last two decades (2000-2019)
|
SCR1
|
Journal
|
Frequency
|
%
|
IF2
|
| 1st | World Journal of Gastroenterology | 70 | 3.74 | 3.665 |
| 2nd | Alimentary Pharmacology and Therapeutics | 54 | 2.88 | 7.515 |
| 3rd | Neurogastroenterology and Motility | 52 | 2.78 | 2.946 |
| 4th | Journal of Clinical Gastroenterology | 39 | 2.08 | 2.973 |
| 5th | American Journal of Gastroenterology | 34 | 1.82 | 10.171 |
| 6th | Gastroenterology | 33 | 1.76 | 17.373 |
| 7th | Current Opinion in Gastroenterology | 27 | 1.44 | 3.225 |
| 8th | PLoS One | 24 | 1.28 | 2.740 |
| 9th | Nutrients | 21 | 1.12 | 4.546 |
| 10th | Gut Microbes | 20 | 1.07 | 7.740 |
Equal journals have the same ranking number, and then a gap is left in the ranking numbers.
Impact factors based on Journal Citation Reports 2019 from Clarivate Analytics.
SCR: Standard competition ranking; IF: Impact factor.
The sample presents an average citation rate of 42 citations per publication. However, 16.6% of the publications have never been cited. Table 3 lists the information on the top ranking of publications in terms of the highest number of citations[36-55]. The article ‘Prebiotic Effects: Metabolic and Health Benefits” is the most cited article with 1147 citations; it was authored by Roberfroid et al[49] and published in the British Journal of Nutrition in 2010. This study reported that a substantial number of studies about human intervention have shown that dietary intake of food products/ingredients/ supplements results in statistically important improvements in the faecal gut microbiota composition. The second most highly cited article is ‘Lactobacillus and Bifidobacterium in IBS: Symptom Responses and Relationship to Cytokine Profiles’ by O'Mahony et al[44] and published in Gastroenterology in 2005. This study showed that intake of Bifidobacterium infantis over 8 wk was associated with symptomatic improvement in IBS.
Table 3.
Top 20 most cited articles on the microbiome in irritable bowel syndrome research in the last two decades (2000-2019)
|
SCR
|
Ref.
|
Title
|
Year
|
Source title
|
Cited by
|
| 1st | Roberfroid et al[49] | "Prebiotic effects: Metabolic and health benefits" | 2010 | British Journal of Nutrition | 1147 |
| 2nd | O'Mahony et al[44] | "Lactobacillus and Bifidobacterium in irritable bowel syndrome: Symptom responses and relationship to cytokine profiles" | 2005 | Gastroenterology | 1042 |
| 3rd | Claesson et al[37] | "Composition, variability, and temporal stability of the intestinal microbiota of the elderly" | 2011 | Proceedings of the National Academy of Sciences of the United States of America | 836 |
| 4th | Collins et al[38] | "The interplay between the intestinal microbiota and the brain” | 2012 | Nature Reviews Microbiology | 735 |
| 5th | Kassinen et al[40] | "The fecal microbiota of irritable bowel syndrome patients differs significantly from that of healthy subjects” | 2007 | Gastroenterology | 684 |
| 6th | Pimentel et al[46] | "Rifaximin therapy for patients with irritable bowel syndrome without constipation" | 2011 | New England Journal of Medicine | 659 |
| 7th | Rinttilä et al[48] | "Development of an extensive set of 16S rDNA-targeted primers for quantification of pathogenic and indigenous bacteria in faecal samples by real-time PCR" | 2004 | Journal of Applied Microbiology | 658 |
| 8th | O'Mahony et al[45] | "Early life stress alters behavior, immunity, and microbiota in rats: implications for irritable bowel syndrome and psychiatric illnesses " | 2009 | Biological Psychiatry | 634 |
| 9th | Rolfe[50] | “The role of probiotic cultures in the control of gastrointestinal health” | 2000 | Journal of Nutrition | 584 |
| 10h | Carabotti et al[36] | “The gut-brain axis: Interactions between enteric microbiota, central and enteric nervous systems" | 2015 | Annals of Gastroenterology | 580 |
| 11th | De Vrese and Schrezenmeir[39] | "Probiotics, prebiotics, and synbiotics" | 2008 | Advances in Biochemical Engineering/Biotechnology | 575 |
| 12th | Rajilić-Stojanović et al[47] | "Global and deep molecular analysis of microbiota signatures in fecal samples from patients with irritable bowel syndrome" | 2011 | Gastroenterology | 545 |
| 13th | Whorwell et al[55] | "Efficacy of an encapsulated probiotic Bifidobacterium infantis 35624 in women with irritable bowel syndrome" | 2006 | American Journal of Gastroenterology | 541 |
| 13th | Swidsinski et al[54] | "Spatial organization and composition of the mucosal flora in patients with inflammatory bowel disease" | 2005 | Journal of Clinical Microbiology | 541 |
| 15th | Malinen et al[41] | "Analysis of the fecal microbiota of irritable bowel syndrome patients and healthy controls with real-time PCR" | 2005 | American Journal of Gastroenterology | 523 |
| 16th | Mayer et al[42] | "Gut/brain axis and the microbiota" | 2015 | Journal of Clinical Investigation | 519 |
| 17th | Simrén et al[52] | "Intestinal microbiota in functional bowel disorders: A Rome foundation report" | 2013 | Gut | 510 |
| 18th | Spiller and Garsed[53] | "Postinfectious irritable bowel syndrome " | 2009 | Gastroenterology | 508 |
| 19th | Rousseaux et al[51] | "Lactobacillus acidophilus modulates intestinal pain and induces opioid and cannabinoid receptors" | 2007 | Nature Medicine | 500 |
| 20th | Nobaek et al[43] | "Alteration of intestinal microflora is associated with reduction in abdominal bloating and pain in patients with irritable bowel syndrome" | 2000 | American Journal of Gastroenterology | 498 |
Table 4 presents the top 10 most productive institutions on the microbiome in IBS research, ranked by the total number of publications. The four institutions that have published the most studies related to microbiome and IBS are the University College Cork (n = 87), APC Microbiome Ireland (n = 84), McMaster University (n = 45), the Mayo Clinic (n = 32), and Alma Mater Studiorum Università di Bologna (n = 38) (Table 4).
Table 4.
Top 10 most productive institutions on the microbiome in irritable bowel syndrome research, ranked by the total number of publications in the last two decades (2000-2019)
|
SCR1
|
Institute
|
Country
|
n
|
%
|
| 1st | University College Cork | Ireland | 87 | 4.65 |
| 2nd | APC Microbiome Ireland | Ireland | 84 | 4.49 |
| 3rd | McMaster University | Canada | 45 | 2.40 |
| 4th | Alma Mater Studiorum Università di Bologna | Italy | 38 | 2.03 |
| 5th | Helsingin Yliopisto | Finland | 36 | 1.92 |
| 5th | Mayo Clinic | United States | 36 | 1.92 |
| 7th | Inserm (Institut national de la santé et de la recherche médicale) | France | 30 | 1.60 |
| 8th | Baylor College of Medicine | United States | 27 | 1.44 |
| 9th | Göteborgs Universitet | Sweden | 27 | 1.44 |
| 10th | The University of North Carolina at Chapel Hill | United States | 27 | 1.44 |
Equal institutes have the same ranking number, and then a gap is left in the ranking numbers.
SCR: Standard competition ranking.
DISCUSSION
This bibliometric study was carried out using data from Scopus for the period of 2000–2019. It presents a comprehensive review of research progress on the microbiome and IBS, identifies hot topics within this field, and indicates potential directions for future research. It is apparent that the research productivity in this field has progressively increased due to the increasing recognition of the role of the gut microbiota[56,57]. In addition, this increase is probably linked to the growing number of researchers who are interested in the fields of neurology and gastroenterology [e.g., EMM Quigley (the United States), JF Cryan (Ireland), TG Dinan (Ireland), G Barbara (Italy), Y Ringel (the United States), M Simrén (Sweden), M Camilleri (the United States), A Palva (Finland), M Pimentel (Canada), NJ Talley (Australia), and others]. Over the last two decades, advances in our understanding of the enteric and central nervous systems have led to an evolving understanding of their interactions and how the gastrointestinal microbiome influences their function. Disturbances in the gastrointestinal microbiome have been identified in patients with functional gastrointestinal disease, like IBS, and it is often the case that symptoms may be triggered by events that lead to changes in the microbiome, where the emotional context and the enteric nervous system function in tandem[1].
The results of this study indicate that the United States has been the most prolific country in this field. These findings are consistent with many previous bibliometric studies[12,58]. Research productivity in the United States is likely associated with overwhelming support in terms of research, the wide range of researchers with an interest within this field, several well-resourced research environments, and greater availability of a well-trained workforce. In addition, the economic strength of the United States has led to a substantial amount of financial support for researchers and has enhanced the mobility of researchers[59,60]. Furthermore, in 2013, the United States launched an exceptional research project on the gut microbiota–brain axis[61], thus contributing to the increasing number of publications regarding the microbiome in IBS.
Our study demonstrates that the gut–brain axis has become the most prolific area for research within IBS and the microbiome globally, and several studies in a range of journals are proof of this emerging trend. According to these data, we can infer that central pain amplification occurs through a wide variety of mechanisms within the central nervous system and mediates the effects of mood, emotional context, and environmental circumstances upon our central pain perception. Functional magnetic resonance imaging (fMRI) studies have demonstrated that patients with IBS often display an exaggerated response of arousal circuits associated with the HPA and activation of endogenous pain pathways in response to visceral stimulation. Similarly, studies have shown enhanced anticipation of pain in response to conditioning stimuli in patients with functional gastrointestinal disease[62]. Neuro-immune activation within the central nervous system is associated with altered astrocyte and microglial activity that further enhances central sensitisation.
Early deprivation in patients with IBS can have profound effects on the microbiome, and researchers recognise that these factors may predispose susceptible individuals to more severe IBS[8,63-66]. Changes in central nervous system function arise as a result of microbial products, which then influence astrocyte, microglial, and central nervous system inflammatory responses[67]. Certain bacterial strains, possibly as a result of being able to modulate these effects, may influence behaviour. Offspring of mice fed a high-fat diet display disordered behaviour and socialisation. These behavioural changes appear to be manifested by alterations in the microbiome. Correction of ‘bacterial deficits’ or their metabolic sequelae leads to improvements in behaviour. Specific bacterial strains have been demonstrated to increase resilience in individuals with anxiety, and these behavioural changes have neurological correlates in fMRI studies. Those factors known to provoke IBS have profound effects on the microbiome function; gastroenteritis can deplete the microbiome, and psychological stress can lead to significant changes in the representation of different phyla within the microbial flora. These potentially detrimental changes may facilitate feedback from the gut and, consequently, permit the gut to have effects on mood, behaviour, and cognitive functions.
Limitations
There are some limitations in our study that are similar to previous bibliometric studies. First, although Scopus is the most recognized and the largest database for peer-reviewed literature, our study is restricted to only the Scopus database as a source of data collection. Second, some authors or institutions have different name formats in the Scopus database, and their research count might be scattered; therefore, their names might not show in the active list. Despite these limitations, we still consider that the findings of our analysis were adequate to characterize accurately the state of IBS and microbiome research at the global level.
CONCLUSION
This is the first study to evaluate and quantify the global research productivity pertaining to the microbiome in IBS to present a holistic picture of this emerging topic and explore future research directions. The number of publications regarding the gut microbiota in IBS has continuously grown since 2013. The United States, the United Kingdom, Italy, and Ireland have been the most productive regions. Currently, the main hot topics regarding the gut microbiota in IBS are the gut–brain axis related to IBS, clinical trials related to IBS and the microbiome, drug-mediated manipulation of the gut microbiome, and the role of the altered composition of intestinal microbiota in IBS prevention. A number of abnormalities have been described within the microbiome of patients with IBS. The relationship between these abnormalities and the causality of dysfunction and associated symptomatology have yet to be clearly elucidated. Our findings, while preliminary, suggest that the future outlook for interventions targeting the gut microbiota in IBS remains promising.
ARTICLE HIGHLIGHTS
Research background
The ability of specific bacteria to boost the development and the effects of proinflammatory cytokines can result in low-grade inflammation seen in a proportion of patients with irritable bowel syndrome (IBS).
Research motivation
The current bibliometric analysis plays an important role for researchers interested in the relationship between the microbiome and IBS. It provides a simple reference guide for interdisciplinary researchers to learn how scientific experts have examined this area in previous years.
Research objectives
This study aimed to carry out a bibliometric review of the IBS and the microbiome literature to explain the growth of this field and assist the identification of unique focus areas that may be important for future research.
Research methods
The information used in our bibliometric research was derived from the Scopus database. Terms related to IBS and the microbiome were searched in titles or abstracts during the period of 2000–2019. For data visualization, VOSviewer software was used.
Research results
Since 2013, the number of publications on gut microbiota in IBS has continuously increased. This result indicates that the future outlook remains optimistic for treatments targeting the gut microbiota in IBS.
Research conclusions
This is the first study to analyze and measure the global research productivity of IBS and microbiome research to provide a holistic view of this evolving subject and explore future research directions. It is evident that, due to the growing understanding of the role of the gut microbiota, research productivity in this area has steadily increased. Currently, the key hot topics are the gut–brain axis related to IBS, clinical trials related to IBS and the microbiome, drug-mediated modulation of the gut microbiome, and the role of the altered composition of the intestinal microbiome in the prevention of IBS.
Research perspectives
Our results indicate that the future outlook for IBS therapies targeting the intestinal microbiota remains promising.
Footnotes
Conflict-of-interest statement: The authors have no financial disclosures or conflicts of interest to declare.
PRISMA 2009 Checklist statement: The authors have read the PRISMA 2009 Checklist, and the manuscript was prepared and revised according to the PRISMA 2009 Checklist.
Manuscript source: Invited manuscript
Peer-review started: November 18, 2020
First decision: December 27, 2020
Article in press: March 16, 2021
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: Palestine
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Gazouli M S-Editor: Fan JR L-Editor: A P-Editor: Li JH
Contributor Information
Sa'ed H Zyoud, Poison Control and Drug Information Center (PCDIC), College of Medicine and Health Sciences, An-Najah National University, Nablus 44839, West Bank, Palestine. saedzyoud@yahoo.com; Department of Clinical and Community Pharmacy, College of Medicine and Health Sciences, An-Najah National University, Nablus 44839, West Bank, Palestine; Department of Clinical Research Centre, An-Najah National University Hospital, Nablus 44839, West Bank, Palestine.
Simon Smale, Department of Gastroenterology, York Hospital, York Teaching Hospital NHS Foundation Trust, York YO31 8HE, United Kingdom.
W Stephen Waring, Acute Medical Unit, York Teaching Hospitals NHS Foundation Trust, York YO31 8HE, United Kingdom.
Waleed Sweileh, Department of Pharmacology and Toxicology, College of Medicine and Health Sciences, An-Najah National University, Nablus 44839, West Bank, Palestine.
Samah W Al-Jabi, Department of Clinical and Community Pharmacy, College of Medicine and Health Sciences, An-Najah National University, Nablus 44839, West Bank, Palestine.
References
- 1.Foster JA, Rinaman L, Cryan JF. Stress & the gut-brain axis: Regulation by the microbiome. Neurobiol Stress. 2017;7:124–136. doi: 10.1016/j.ynstr.2017.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hoekman DR, Zeevenhooven J, D'Haens GR, Benninga MA. The prevalence of irritable bowel syndrome-type symptoms in inflammatory bowel disease patients in remission. Eur J Gastroenterol Hepatol. 2017;29:1086–1090. doi: 10.1097/MEG.0000000000000921. [DOI] [PubMed] [Google Scholar]
- 3.Holtmann GJ, Ford AC, Talley NJ. Pathophysiology of irritable bowel syndrome. Lancet Gastroenterol Hepatol. 2016;1:133–146. doi: 10.1016/S2468-1253(16)30023-1. [DOI] [PubMed] [Google Scholar]
- 4.Boeckxstaens GE, Wouters MM. Neuroimmune factors in functional gastrointestinal disorders: A focus on irritable bowel syndrome. Neurogastroenterol Motil. 2017;29 doi: 10.1111/nmo.13007. [DOI] [PubMed] [Google Scholar]
- 5.Park SH, Naliboff BD, Shih W, Presson AP, Videlock EJ, Ju T, Kilpatrick L, Gupta A, Mayer EA, Chang L. Resilience is decreased in irritable bowel syndrome and associated with symptoms and cortisol response. Neurogastroenterol Motil. 2018;30 doi: 10.1111/nmo.13155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Stern EK, Brenner DM. Gut Microbiota-Based Therapies for Irritable Bowel Syndrome. Clin Transl Gastroenterol. 2018;9:e134. doi: 10.1038/ctg.2018.2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rodiño-Janeiro BK, Vicario M, Alonso-Cotoner C, Pascua-García R, Santos J. A Review of Microbiota and Irritable Bowel Syndrome: Future in Therapies. Adv Ther. 2018;35:289–310. doi: 10.1007/s12325-018-0673-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Salem AE, Singh R, Ayoub YK, Khairy AM, Mullin GE. The gut microbiome and irritable bowel syndrome: State of art review. Arab J Gastroenterol. 2018;19:136–141. doi: 10.1016/j.ajg.2018.02.008. [DOI] [PubMed] [Google Scholar]
- 9.Dinan TG, Cryan JF. Mood by microbe: towards clinical translation. Genome Med. 2016;8:36. doi: 10.1186/s13073-016-0292-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Menees S, Chey W. The gut microbiome and irritable bowel syndrome. F1000Res. 2018;7 doi: 10.12688/f1000research.14592.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hernández-Vásquez A, Alarcon-Ruiz CA, Bendezu-Quispe G, Comandé D, Rosselli D. A bibliometric analysis of the global research on biosimilars. J Pharm Policy Pract. 2018;11:6. doi: 10.1186/s40545-018-0133-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Liu H, Yu Z, Chen C, Hong R, Jin K, Yang C. Visualization and Bibliometric Analysis of Research Trends on Human Fatigue Assessment. J Med Syst. 2018;42:179. doi: 10.1007/s10916-018-1033-3. [DOI] [PubMed] [Google Scholar]
- 13.Ozsoy Z, Demir E. The Evolution of Bariatric Surgery Publications and Global Productivity: A Bibliometric Analysis. Obes Surg. 2018;28:1117–1129. doi: 10.1007/s11695-017-2982-1. [DOI] [PubMed] [Google Scholar]
- 14.Schwimmer MH, Sawh MC, Heskett KM, Goyal NP, Newton KP, Schwimmer JB. A Bibliometric Analysis of Clinical and Translational Research in Pediatric Gastroenterology from 1970 to 2017. J Pediatr Gastroenterol Nutr. 2018;67:564–569. doi: 10.1097/MPG.0000000000002056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wang B, Zhao P. Worldwide research productivity in the field of back pain: A bibliometric analysis. Medicine (Baltimore) 2018;97:e11566. doi: 10.1097/MD.0000000000011566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Yeung AWK, Heinrich M, Atanasov AG. Ethnopharmacology-A Bibliometric Analysis of a Field of Research Meandering Between Medicine and Food Science? Front Pharmacol. 2018;9:215. doi: 10.3389/fphar.2018.00215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zyoud SH, Waring WS, Al-Jabi SW, Sweileh WM. Global cocaine intoxication research trends during 1975-2015: a bibliometric analysis of Web of Science publications. Subst Abuse Treat Prev Policy. 2017;12:6. doi: 10.1186/s13011-017-0090-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zyoud SH, Waring WS, Sweileh WM, Al-Jabi SW. Global Research Trends in Lithium Toxicity from 1913 to 2015: A Bibliometric Analysis. Basic Clin Pharmacol Toxicol. 2017;121:67–73. doi: 10.1111/bcpt.12755. [DOI] [PubMed] [Google Scholar]
- 19.Tian J, Li M, Lian F, Tong X. The hundred most-cited publications in microbiota of diabetes research: A bibliometric analysis. Medicine (Baltimore) 2017;96:e7338. doi: 10.1097/MD.0000000000007338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Yao H, Wan JY, Wang CZ, Li L, Wang J, Li Y, Huang WH, Zeng J, Wang Q, Yuan CS. Bibliometric analysis of research on the role of intestinal microbiota in obesity. PeerJ. 2018;6:e5091. doi: 10.7717/peerj.5091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zyoud SH, Smale S, Waring WS, Sweileh WM, Al-Jabi SW. Global research trends in microbiome-gut-brain axis during 2009-2018: a bibliometric and visualized study. BMC Gastroenterol. 2019;19:158. doi: 10.1186/s12876-019-1076-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ejtahed HS, Tabatabaei-Malazy O, Soroush AR, Hasani-Ranjbar S, Siadat SD, Raes J, Larijani B. Worldwide trends in scientific publications on association of gut microbiota with obesity. Iran J Basic Med Sci. 2019;22:65–71. doi: 10.22038/ijbms.2018.30203.7281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Huang X, Fan X, Ying J, Chen S. Emerging trends and research foci in gastrointestinal microbiome. J Transl Med. 2019;17:67. doi: 10.1186/s12967-019-1810-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Li Y, Zou Z, Bian X, Huang Y, Wang Y, Yang C, Zhao J, Xie L. Fecal microbiota transplantation research output from 2004 to 2017: a bibliometric analysis. PeerJ. 2019;7:e6411. doi: 10.7717/peerj.6411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ding-Qi B, Hui-Bo C, Xin-Yang L, Yi Z, Lan-Hua L, Yun-Hai G. [Analysis of research status and hotspots of snail intestinal flora based on bibliometrics] Zhongguo Xue Xi Chong Bing Fang Zhi Za Zhi. 2018;30:571–574. doi: 10.16250/j.32.1374.2018189. [DOI] [PubMed] [Google Scholar]
- 26.Padilla FM, Gallardo M, Manzano-Agugliaro F. Global trends in nitrate leaching research in the 1960-2017 period. Sci Total Environ. 2018;643:400–413. doi: 10.1016/j.scitotenv.2018.06.215. [DOI] [PubMed] [Google Scholar]
- 27.Teles RHG, Moralles HF, Cominetti MR. Global trends in nanomedicine research on triple negative breast cancer: a bibliometric analysis. Int J Nanomedicine. 2018;13:2321–2336. doi: 10.2147/IJN.S164355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Cash-Gibson L, Rojas-Gualdrón DF, Pericàs JM, Benach J. Inequalities in global health inequalities research: A 50-year bibliometric analysis (1966-2015) PLoS One. 2018;13:e0191901. doi: 10.1371/journal.pone.0191901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ford AC, Quigley EM, Lacy BE, Lembo AJ, Saito YA, Schiller LR, Soffer EE, Spiegel BM, Moayyedi P. Effect of antidepressants and psychological therapies, including hypnotherapy, in irritable bowel syndrome: systematic review and meta-analysis. Am J Gastroenterol. 2014;109:1350–65; quiz 1366. doi: 10.1038/ajg.2014.148. [DOI] [PubMed] [Google Scholar]
- 30.Latimer PR. Irritable bowel syndrome. Psychosomatics. 1983;24:205–218. doi: 10.1016/S0033-3182(83)73223-8. [DOI] [PubMed] [Google Scholar]
- 31.John GK, Wang L, Nanavati J, Twose C, Singh R, Mullin G. Dietary Alteration of the Gut Microbiome and Its Impact on Weight and Fat Mass: A Systematic Review and Meta-Analysis. Genes (Basel) 2018;9 doi: 10.3390/genes9030167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Memba R, Duggan SN, Ni Chonchubhair HM, Griffin OM, Bashir Y, O'Connor DB, Murphy A, McMahon J, Volcov Y, Ryan BM, Conlon KC. The potential role of gut microbiota in pancreatic disease: A systematic review. Pancreatology. 2017;17:867–874. doi: 10.1016/j.pan.2017.09.002. [DOI] [PubMed] [Google Scholar]
- 33.Linares DM, Ross P, Stanton C. Beneficial Microbes: The pharmacy in the gut. Bioengineered. 2016;7:11–20. doi: 10.1080/21655979.2015.1126015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.van Eck NJ, Waltman L. Software survey: VOSviewer, a computer program for bibliometric mapping. Scientometrics. 2010;84:523–538. doi: 10.1007/s11192-009-0146-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.van Eck NJ, Waltman L. Citation-based clustering of publications using CitNetExplorer and VOSviewer. Scientometrics. 2017;111:1053–1070. doi: 10.1007/s11192-017-2300-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Carabotti M, Scirocco A, Maselli MA, Severi C. The gut-brain axis: interactions between enteric microbiota, central and enteric nervous systems. Ann Gastroenterol. 2015;28:203–209. [PMC free article] [PubMed] [Google Scholar]
- 37.Claesson MJ, Cusack S, O'Sullivan O, Greene-Diniz R, de Weerd H, Flannery E, Marchesi JR, Falush D, Dinan T, Fitzgerald G, Stanton C, van Sinderen D, O'Connor M, Harnedy N, O'Connor K, Henry C, O'Mahony D, Fitzgerald AP, Shanahan F, Twomey C, Hill C, Ross RP, O'Toole PW. Composition, variability, and temporal stability of the intestinal microbiota of the elderly. Proc Natl Acad Sci USA. 2011;108 Suppl 1:4586–4591. doi: 10.1073/pnas.1000097107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Collins SM, Surette M, Bercik P. The interplay between the intestinal microbiota and the brain. Nat Rev Microbiol. 2012;10:735–742. doi: 10.1038/nrmicro2876. [DOI] [PubMed] [Google Scholar]
- 39.de Vrese M, Schrezenmeir J. Probiotics, prebiotics, and synbiotics. Adv Biochem Eng Biotechnol. 2008;111:1–66. doi: 10.1007/10_2008_097. [DOI] [PubMed] [Google Scholar]
- 40.Kassinen A, Krogius-Kurikka L, Mäkivuokko H, Rinttilä T, Paulin L, Corander J, Malinen E, Apajalahti J, Palva A. The fecal microbiota of irritable bowel syndrome patients differs significantly from that of healthy subjects. Gastroenterology. 2007;133:24–33. doi: 10.1053/j.gastro.2007.04.005. [DOI] [PubMed] [Google Scholar]
- 41.Malinen E, Rinttilä T, Kajander K, Mättö J, Kassinen A, Krogius L, Saarela M, Korpela R, Palva A. Analysis of the fecal microbiota of irritable bowel syndrome patients and healthy controls with real-time PCR. Am J Gastroenterol. 2005;100:373–382. doi: 10.1111/j.1572-0241.2005.40312.x. [DOI] [PubMed] [Google Scholar]
- 42.Mayer EA, Tillisch K, Gupta A. Gut/brain axis and the microbiota. J Clin Invest. 2015;125:926–938. doi: 10.1172/JCI76304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Nobaek S, Johansson ML, Molin G, Ahrné S, Jeppsson B. Alteration of intestinal microflora is associated with reduction in abdominal bloating and pain in patients with irritable bowel syndrome. Am J Gastroenterol. 2000;95:1231–1238. doi: 10.1111/j.1572-0241.2000.02015.x. [DOI] [PubMed] [Google Scholar]
- 44.O'Mahony L, McCarthy J, Kelly P, Hurley G, Luo F, Chen K, O'Sullivan GC, Kiely B, Collins JK, Shanahan F, Quigley EM. Lactobacillus and bifidobacterium in irritable bowel syndrome: symptom responses and relationship to cytokine profiles. Gastroenterology. 2005;128:541–551. doi: 10.1053/j.gastro.2004.11.050. [DOI] [PubMed] [Google Scholar]
- 45.O'Mahony SM, Marchesi JR, Scully P, Codling C, Ceolho AM, Quigley EM, Cryan JF, Dinan TG. Early life stress alters behavior, immunity, and microbiota in rats: implications for irritable bowel syndrome and psychiatric illnesses. Biol Psychiatry. 2009;65:263–267. doi: 10.1016/j.biopsych.2008.06.026. [DOI] [PubMed] [Google Scholar]
- 46.Pimentel M, Lembo A, Chey WD, Zakko S, Ringel Y, Yu J, Mareya SM, Shaw AL, Bortey E, Forbes WP TARGET Study Group. Rifaximin therapy for patients with irritable bowel syndrome without constipation. N Engl J Med. 2011;364:22–32. doi: 10.1056/NEJMoa1004409. [DOI] [PubMed] [Google Scholar]
- 47.Rajilić-Stojanović M, Biagi E, Heilig HG, Kajander K, Kekkonen RA, Tims S, de Vos WM. Global and deep molecular analysis of microbiota signatures in fecal samples from patients with irritable bowel syndrome. Gastroenterology. 2011;141:1792–1801. doi: 10.1053/j.gastro.2011.07.043. [DOI] [PubMed] [Google Scholar]
- 48.Rinttilä T, Kassinen A, Malinen E, Krogius L, Palva A. Development of an extensive set of 16S rDNA-targeted primers for quantification of pathogenic and indigenous bacteria in faecal samples by real-time PCR. J Appl Microbiol. 2004;97:1166–1177. doi: 10.1111/j.1365-2672.2004.02409.x. [DOI] [PubMed] [Google Scholar]
- 49.Roberfroid M, Gibson GR, Hoyles L, McCartney AL, Rastall R, Rowland I, Wolvers D, Watzl B, Szajewska H, Stahl B, Guarner F, Respondek F, Whelan K, Coxam V, Davicco MJ, Léotoing L, Wittrant Y, Delzenne NM, Cani PD, Neyrinck AM, Meheust A. Prebiotic effects: metabolic and health benefits. Br J Nutr. 2010;104 Suppl 2:S1–63. doi: 10.1017/S0007114510003363. [DOI] [PubMed] [Google Scholar]
- 50.Rolfe RD. The role of probiotic cultures in the control of gastrointestinal health. J Nutr. 2000;130:396S–402S. doi: 10.1093/jn/130.2.396S. [DOI] [PubMed] [Google Scholar]
- 51.Rousseaux C, Thuru X, Gelot A, Barnich N, Neut C, Dubuquoy L, Dubuquoy C, Merour E, Geboes K, Chamaillard M, Ouwehand A, Leyer G, Carcano D, Colombel JF, Ardid D, Desreumaux P. Lactobacillus acidophilus modulates intestinal pain and induces opioid and cannabinoid receptors. Nat Med. 2007;13:35–37. doi: 10.1038/nm1521. [DOI] [PubMed] [Google Scholar]
- 52.Simrén M, Barbara G, Flint HJ, Spiegel BM, Spiller RC, Vanner S, Verdu EF, Whorwell PJ, Zoetendal EG Rome Foundation Committee. Intestinal microbiota in functional bowel disorders: a Rome foundation report. Gut. 2013;62:159–176. doi: 10.1136/gutjnl-2012-302167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Spiller R, Garsed K. Postinfectious irritable bowel syndrome. Gastroenterology. 2009;136:1979–1988. doi: 10.1053/j.gastro.2009.02.074. [DOI] [PubMed] [Google Scholar]
- 54.Swidsinski A, Weber J, Loening-Baucke V, Hale LP, Lochs H. Spatial organization and composition of the mucosal flora in patients with inflammatory bowel disease. J Clin Microbiol. 2005;43:3380–3389. doi: 10.1128/JCM.43.7.3380-3389.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Whorwell PJ, Altringer L, Morel J, Bond Y, Charbonneau D, O'Mahony L, Kiely B, Shanahan F, Quigley EM. Efficacy of an encapsulated probiotic Bifidobacterium infantis 35624 in women with irritable bowel syndrome. Am J Gastroenterol. 2006;101:1581–1590. doi: 10.1111/j.1572-0241.2006.00734.x. [DOI] [PubMed] [Google Scholar]
- 56.Distrutti E, Monaldi L, Ricci P, Fiorucci S. Gut microbiota role in irritable bowel syndrome: New therapeutic strategies. World J Gastroenterol. 2016;22:2219–2241. doi: 10.3748/wjg.v22.i7.2219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.König J, Brummer RJ. Alteration of the intestinal microbiota as a cause of and a potential therapeutic option in irritable bowel syndrome. Benef Microbes. 2014;5:247–261. doi: 10.3920/BM2013.0033. [DOI] [PubMed] [Google Scholar]
- 58.Mo Z, Fu HZ, Ho YS. Global development and trend of wind tunnel research from 1991 to 2014: a bibliometric analysis. Environ Sci Pollut Res Int. 2018;25:30257–30270. doi: 10.1007/s11356-018-3019-6. [DOI] [PubMed] [Google Scholar]
- 59.Philipson L. Medical research activities, funding, and creativity in Europe: comparison with research in the United States. JAMA. 2005;294:1394–1398. doi: 10.1001/jama.294.11.1394. [DOI] [PubMed] [Google Scholar]
- 60.Fontanarosa PB, DeAngelis CD, Hunt N. Medical research--state of the science. JAMA. 2005;294:1424–1425. doi: 10.1001/jama.294.11.1424. [DOI] [PubMed] [Google Scholar]
- 61.Wang HX, Wang YP. Gut Microbiota-brain Axis. Chin Med J (Engl) 2016;129:2373–2380. doi: 10.4103/0366-6999.190667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Kano M, Dupont P, Aziz Q, Fukudo S. Understanding Neurogastroenterology From Neuroimaging Perspective: A Comprehensive Review of Functional and Structural Brain Imaging in Functional Gastrointestinal Disorders. J Neurogastroenterol Motil. 2018;24:512–527. doi: 10.5056/jnm18072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Tanaka Y, Kanazawa M, Fukudo S, Drossman DA. Biopsychosocial model of irritable bowel syndrome. J Neurogastroenterol Motil. 2011;17:131–139. doi: 10.5056/jnm.2011.17.2.131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Vuong HE, Yano JM, Fung TC, Hsiao EY. The Microbiome and Host Behavior. Annu Rev Neurosci. 2017;40:21–49. doi: 10.1146/annurev-neuro-072116-031347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Dinan TG, Cryan JF. The Microbiome-Gut-Brain Axis in Health and Disease. Gastroenterol Clin North Am. 2017;46:77–89. doi: 10.1016/j.gtc.2016.09.007. [DOI] [PubMed] [Google Scholar]
- 66.Chong PP, Chin VK, Looi CY, Wong WF, Madhavan P, Yong VC. The Microbiome and Irritable Bowel Syndrome - A Review on the Pathophysiology, Current Research and Future Therapy. Front Microbiol. 2019;10:1136. doi: 10.3389/fmicb.2019.01136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Fung TC, Olson CA, Hsiao EY. Interactions between the microbiota, immune and nervous systems in health and disease. Nat Neurosci. 2017;20:145–155. doi: 10.1038/nn.4476. [DOI] [PMC free article] [PubMed] [Google Scholar]