Abstract
Recent advances in 3D printing have provided unprecedented opportunities in bone tissue engineering applications for producing a variety of complex patient-specific implants for the treatment of critical-sized bone defects. Natural medicinal compounds (NMCs) with osteogenic potential can be incorporated into these 3D-printed parts to improve bone formation and therefore enhance implant performance. Using NMCs to treat bone-related disorders may prove to be a healthy preventive choice as they are considered safe, have lesser or no side effects, and are more suitable for prolonged use than synthetic drugs. In this review paper, the current challenges of bone tissue engineering are addressed briefly, highlighting the immense potential of NMCs integrated within tissue engineering scaffolds for orthopedic and dental applications.
Bone Tissue Engineering: Recent Advances and Challenges
In recent years, a wide variety of advanced bone tissue engineering (BTE) (see Glossary) scaffolds have been designed for the treatment of critical-sized bone defects, induced by surgery, trauma, or primary tumor resection. Bone defect repair using scaffold implantation is an unavoidable necessity, as the human body is not capable of regenerating and repairing a large bone loss. At present, more than half a million patients in the USA have received functional bone implants, with a total cost higher than $2.5 billion in 2012, which is expected to double by 2020 [1]. Autografts are considered the gold standard for bone grafts due to their excellent histocompatibility and nonimmunogenic properties. However, autografts are generally harvested from the patient’s body and therefore require a second operation. Autografts are also associated with expensive procedures, significant donor site injury, deformity, and surgical risks, including inflammation, infection, bleeding, and pain. Allografts are the second most common bone-grafting approach, in which bone tissue is transplanted from a donor, often from a cadaver [2,3]. Compared with autografts, allografts are less expensive but exhibit reduced osteoinductive properties because they lack a cellular component [4,5]. Allografts are likely to be histocompatible, but they may be immunogenic and can transmit infections. Technological advances and the clinical need for biomedical implants have led to huge progress in a short span, and various FDA-approved bone replacements have performed well over the years in many patients. However, the lifetime of an implant is often challenged in a living system, necessitating revision surgeries, especially in younger patients.
Currently, the American and global markets are experiencing an exceedingly high demand for bone grafts, unmet by the current supply [6]. Although the above-mentioned clinical techniques improve bone repair, the ideal bone scaffolds would possess the following characteristics: good osteoinductive and angiogenic potential, biocompatibility, controlled shape and size, defect-specific match, long shelf life, and low cost. To address these challenges, tissue engineering has made great strides over the past few decades in advancing scaffold design and architecture, with the fabrication of many 3D-printed constructs that mimic the biological, mechanical, and chemical characteristics of the host tissue. These 3D-printed parts, including both load-bearing hip or knee implant and low-load-bearing bioceramic scaffolds, are often incorporated with various drugs, proteins, growth factors, and biomolecules with osteogenic potential to improve bone formation and therefore enhance implant performance. BMPs, growth factors, and cell therapy can also be applied to bone cell proliferation and differentiation [7–9]. However, several challenges need to be addressed before these strategies can be clinically adopted as an alternative to the currently available therapies. These include reduced stability of encapsulated proteins for sustained release, compartmentalization of delivery materials, the release of certain hydrophobic factors, and unfavorable interaction between scaffolds and biomolecules. Prolonged delivery of these synthetic drugs and biomolecules might be effective for the treatment of musculoskeletal disorders, but at the expense of adverse side effects and tissue toxicity.
The long-lasting complications of current clinical treatments have prompted a search for safer alternatives. Natural sources and their active components, used as medicinal compounds, have stimulated increasing social and medical interest with their capability to mitigate long-lasting side effects caused by synthetic medicine and to respond competently for the treatment of acute metabolic bone disorders or osteoporosis. Such forms of medicine usually take a holistic approach that tries to work with natural healing systems, such as that of bone. Natural medicinal compounds (NMCs) have been gaining popularity for the past two decades and are now being used by two in every five adults in the USA [10]. Diverse biological activity, unmatched physiological complexity, and therapeutic simplicity are some of the unique aspects of NMCs that make them distinctive from synthetic drugs. Additionally, using these NMCs to treat bone disorders may be a healthy preventive choice as they are often more cost-effective and demonstrate fewer adverse effects compared with modern synthetic medical treatments. In this regard, we believe that the solutions to the key challenges of BTE lie in the combination of NMCs with modern technologies as well as integrating knowledge from both bone scaffolding and NMCs, which is only possible through a collaboration among clinicians, scientists, and engineers. Taking this idea further, this review explores novel strategies that involve the integration of NMCs with 3D printing techniques for improved functionality and clinical utility to overcome the challenges in current tissue engineering. Moreover, some sophisticated and advanced drug delivery techniques are also discussed to address the structural and biological complexity of the natural system.
Figure 1 (Key Figure) demonstrates various delivery vehicles that have the potential to serve as integration tools between additive manufacturing and NMCs, which can be utilized towards the clinical treatment of challenging bone defects.
Need for NMCs in BTE
Natural compounds present in common cooking spices, including curcumin, garlic, ginger, and others, have demonstrated osteogenic effects in various clinical and preclinical trials. The bioactive chemical components of these NMCs have been identified and their pharmacological effects are discussed in the following section. Table 1 presents NMCs, their active constituents, and potential role in bone health, and Table 2 gives an overview of the osteogenic potential of natural medical compounds in vitro and in vivo.
Table 1.
Natural Medicinal Compounds: Their Active Constituents and Roles in Bone Health
| Sources | Chemical structure | Active constituent | Role in bone health | Refs |
|---|---|---|---|---|
 Turmeric |
 |
Curcumin | Works by modulating osteosarcoma, osteoblast, and osteoclast cellular function and thereby controls bone tumor formation, bone resorption, and new bone formation | [15–17] |
 Garlic |
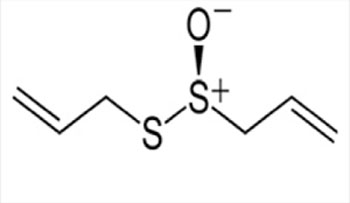 |
Allicin | Works by modulating osteoblast and osteoclast cellular function and exhibits its activity against bone resorption and oxidative stress-induced damage to bone | [18–20] |
 Aloe vera |
 |
Acemannan | Works by modulating osteoblast and osteoclast cellular function and therefore controls bone formation and resorption | [11–14] |
 Ginger |
 |
Gingerol | Works by modulating osteoblast and osteosarcoma and therefore controls bone formation and bone tumor growth | [21,22] |
 Soy |
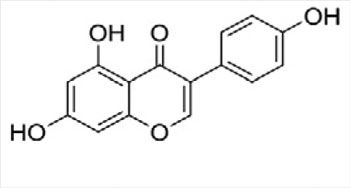 |
Isoflavones | Works by modulating osteoblast and osteosarcoma cellular function and thereby controls bone formation and chemoprevention | [28–31] |
 Green tea |
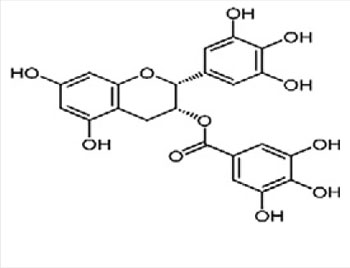 |
Epigallocatechin-gallate (EGCG) | Works by modulating osteoblast and osteoclast cellular function and thereby controls bone formation and resorption | [23–27] |
Table 2.
Osteogenic Potential of NMCs: Preclinical, Clinical, In Vitro, and In Vivo Studies
| Natural medicinal compound | Type of study/biological system | Results | Refs |
|---|---|---|---|
| Ginger | Randomized, double-blinded, placebo-controlled, multicenter, parallel-group, 6-week study/ 261 patients with knee osteoarthritis | 63% of patients who were administered ginger extracts found relief compared with the 50% under placebo. The subjects in the ginger group showed improvement in osteoarthritis conditions in terms of standing, walking, and less frequent resorting to acetaminophen. |
[72] |
| In vivo study/ ovariectomy-induced rat | A crude extract of ginger (26 mg/kg/day) was efficient to preserve the BMD, suggesting prevention of osteoclast activity along with its anti-inflammatory effects. | [73] | |
| Garlic | In vivo study/ ovariectomized rats | Garlic oil supplementation recovered the loss in bone densities found in ovariectomized rats. Significant changes in primary and secondary markers, such as ALP, TRAP, urinary excretion of calcium, phosphate, hydroxyproline, and urinary calcium to creatinine ratio were reported. |
[74] |
| Garlic oil-supplemented diet suppressed the effect of ovariectomy in rats, such as low BMD, and low tensile strength. | [75] | ||
| Turmeric | In vivo study/ insulin-dependent diabetic rat model | Oral administration of curcumin suppressed osteoclast-induced bone resorption. | [76] |
| In vitro study/RAW 264.7 cells | Prevented RANKL-induced NF-κβ activation and osteoclastogenesis. | [77] | |
| In vivo study/ ovariectomized rats | Curcumin administration (15 mg/day) for 6 months increased the size of the femur and resulted in an increase in energy to fracture. Curcumin produces beneficial changes in bone turnover and increases in bone strength. | [78] | |
| Soy isoflavones | Randomized, double-blinded, placebo-controlled study on human patients (postmenopausal women) | Dietary genistein (54 mg/day) may be as effective as hormone replacement therapy in attenuating menopause-related bone loss without causing the associated side effects. | [79] |
| Epidemiologic study (63 257 Chinese men and women) | Consumption of soy food reduced the fracture risk in women to one-third. | [80] | |
| Blinded, randomized, crossover intervention trial in 24 postmenopausal women | A 50-day study showed daily intake of isoflavones (105 mg/day) increased bone calcium retention by 7.6% compared with that of risedronate at 15%, a bisphosphonate drug used for osteoporosis treatment. | [81] | |
| Green tea (EGCG) | Ovariectomized 14-month-old female rats | Green tea supplementation resulted in increased femur bone mineral density via an increase in antioxidant capacity and a decrease of oxidative stress damage. | [82] |
| Human bone marrow mesenchymal stem cells | EGCG can increase mRNA expression of BMP2 and subsequent osteogenic-related genes, including Runx2, ALP, osteonectin, and osteocalcin. EGCG further increased ALP activity and mineralization. | [83] |
With a long history of popular and traditional use, Aloe vera is one of the few NMCs widely used in the USA for cosmetic and pharmaceutical purposes. The pharmacological claims of Aloe vera cover a broad range of applications, including dermatological, hypoglycemic, wound healing, and bone regeneration [11]. One study showed enhanced rat bone marrow stromal cell proliferation, VEGF, and ALP activity by the treatment of acemannan, a key constituent of Aloe vera, along with higher bone mineral density (BMD) and accelerated healing [12,13].
Acemannan is believed to enhance the activity of several cytokines like interleukin 6 (IL-6) and tumor necrosis factor- (TNF- ), in turn increasing new bone formation and bone mineralization. Aloein, a glycoside isolated from Aloe vera, also helped in reducing the osteoclast activity by influencing the nuclear factor-kappa beta (NF-κβ) pathway, which is crucial for bone regeneration [14].
Curcumin is the main active component of turmeric, which is the rhizome of the herbaceous perennial plant Curcuma longa, belonging to the ginger family Zingiberaceae [15]. Curcumin is widely studied for its various biological and therapeutic properties. Numerous in vitro and in vivo studies have shown anti-inflammatory, antimicrobial, anti-arthritic, and anticancer properties of curcumin. Curcumin regulates various molecular targets, such as NF-κβ, which is associated with the bone remodeling process. Curcumin also blocks phosphorylation and degradation of NF-κβ inhibitor (Iκβ), which leads to the formation of inactive NF-κβ-Iκβ conjugate [16]. Suppression of NF-κβ positively influences osteoblast differentiation and prevents osteoclastic bone resorption. Curcumin also inhibits TNF-α, which is found in increased levels among postmenopausal women and considered to be correlated with osteoporosis [17].
Garlic (Allium sativum), a very common spice used for cooking, has attracted attention due to its multifaceted pharmacological activities, including anti-osteoporotic properties [18]. One study demonstrated that allicin, the chief active compound derived from garlic, protects osteoblasts from oxidative stress-induced mitochondrial dysfunction and apoptosis and thus inhibits osteoporosis [19]. Another study reported that garlic reduces the level of TRAP, a compound released from osteoclasts, and thereby slows the process of bone resorption [20].
Ginger (Zingiber officinale), a perennial tropical plant of the family Zingiberaceae, is a commonly used herb and food-flavoring agent. One of the major components of fresh ginger, 6-gingerol, has been shown to have antibacterial, anti-inflammatory, antihyperglycemic, antitumor, renal-protective, and cardiotonic effects [21]. The characteristic effects of 6-gingerol appear to be mediated by antioxidative action that involves inhibition of TNF- and NF-κB signaling. Because of their anti-inflammatory properties, gingerols have been implicated in the joint-protective effects in an experimental arthritis model due to their ability to inhibit joint inflammation [22].
The tea plant, an evergreen shrub (Camellia sinensis) that originated in China, is consumed and grown all over the world. Steaming freshly cut tea leaves produces green tea, which is high in polyphenolic compounds and vitamin K and potentially has anticancer and antioxidant properties [23]. Experimental and population-based studies have demonstrated the efficacy of green tea against osteoporosis [24]. Green tea has been demonstrated to inhibit bone resorption and stimulate osteoblast activity [25–27]. The efficacy of green tea in the prevention of age-related bone loss activity has also been considered in various studies.
Soy (Glycine max) and foods containing soy are excellent sources of phytoestrogens, which are considered to be very beneficial to bone health [28]. Genistein, a soy-based isoflavone, prevents osteoporotic fracture by inhibiting factors responsible for osteoclastic resorption and increasing markers like ALP, which is related to osteoblast formation [29]. Another study showed that genistein inhibits in vitro bone resorption and enhances bone formation [30]. In vivo results have also supported the evidence of improved BMD with the consumption of soybean. Various short-term studies reported a beneficial effect of isoflavones on bone turnover and BMD among postmenopausal women. The high intake of soy in the Japanese diet is correlated with low occurrences of osteoporosis and related bone fractures in Japan [31].
Key Figure
Overview of Natural Medicinal Compounds for Bone Repair
Figure 1.
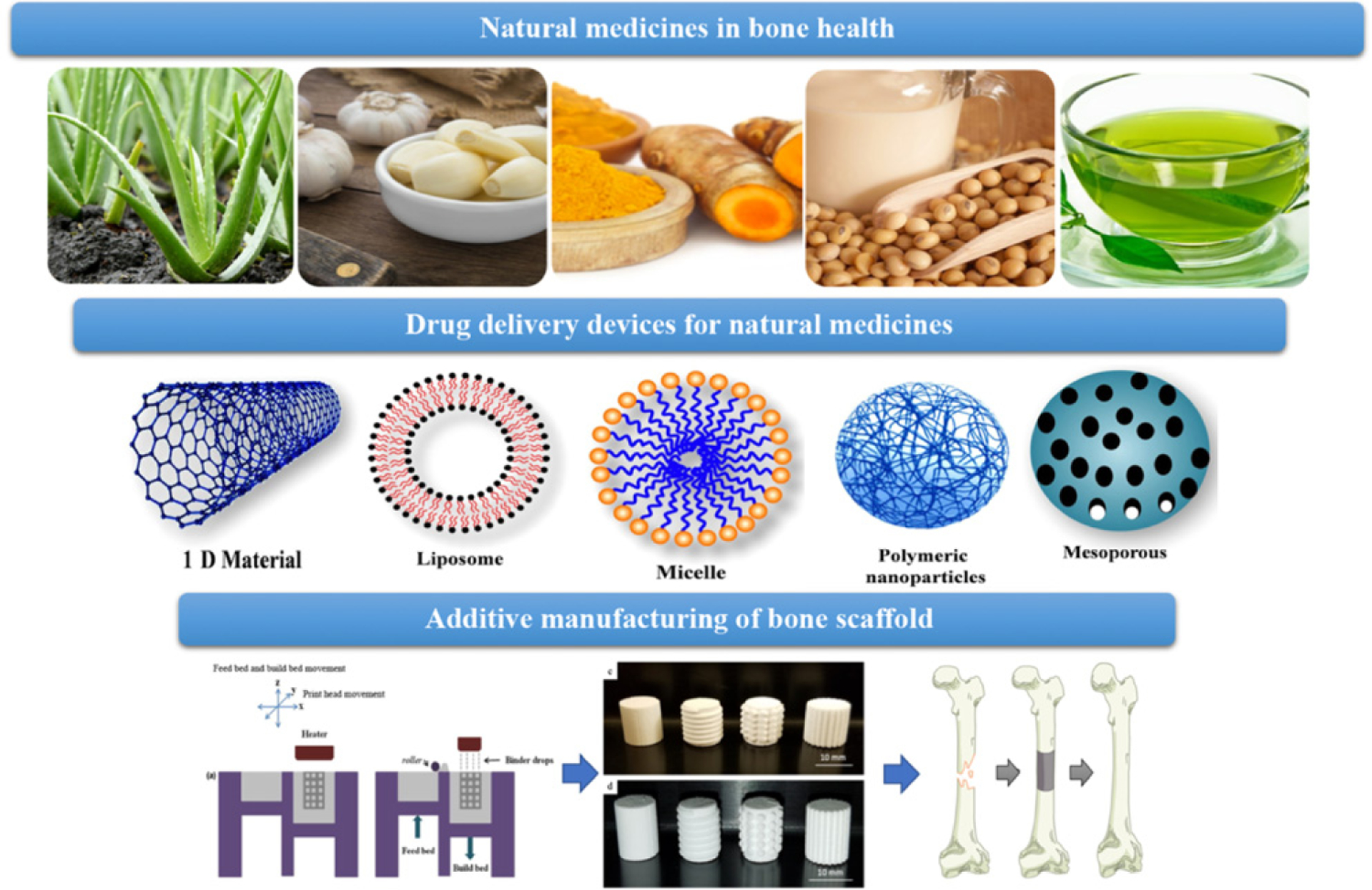
Natural medicinal compounds can be entrapped within an appropriate delivery vehicle followed by incorporation in a bone scaffold to promote bone regeneration and enhance defect repair.
3D Printing for Bone Scaffold Fabrication and Drug Delivery
In order to repair critical-size bone defects, bone scaffolds are generally implanted in the defect size, which provides an artificial extracellular matrix environment for cell attachment, proliferation, and differentiation and therefore induces tissue regeneration. Additive manufacturing, also known as 3D printing, has demonstrated remarkable progress in the tissue engineering field due to providing patient-specific anatomic scaffolds with high structural complexity and design flexibility, overcoming the challenges of conventional fabrication methods [32]. Ideal scaffolds should mimic the hierarchical and multiscale porous architecture of bone tissue in order to optimize successful integration into the surrounding host tissue. The complex porous architecture is almost always intricately linked to biological function. For instance, macropores (100–500 μm) ensure nutrients, oxygen, and waste transport and they guide new bone tissue ingrowth through the interconnected porous channel, whereas micropores (<10 μm) increase the surface area and roughness of the scaffold, which enhances cellular attachment and osseointegration [33]. Moreover, the unique pore structure can also be tailored to achieve long-term, localized controlled delivery of NMCs for bone regeneration. Another critical challenge in designing bone scaffolds for NMC delivery lies in the selection of appropriate biomaterials. Suitable biomaterials, which can be either metal (titanium, stainless steel, and cobalt-chromium), ceramic (alumina, CaP, and bioglass), polymer (natural or synthetic), or composite, must not exhibit undesired chemical or biological interaction with the NMCs. In addition, the mechanical properties of the scaffold need to be precisely controlled to meet specific needs for clinical applications. For example, fabricated parts should possess adequate mechanical stability to serve as a platform for bone cell attachment and regeneration, but they should not cause stress-shielding, which might result in the loosening of implants [34]. These design strategies or approaches can be followed as a guideline for fabricating 3D-printed constructs with complex bone-mimicking architecture and custom-based mechanical properties.
Despite tremendous advancement in 3D printing and bone scaffold fabrication, sometimes tissue regeneration is still not guaranteed when surrounding bone around defect-site lacks the inherent potential to regenerate. In such cases, the use of osteoconductive NMCs can be considered effective as it can influence the host healing response and improve in vitro tissue formation at the defect site [35]. Oral administration of NMCs is not effective in most cases because of poor bioavailability, fast dissociation rate, and rapid elimination from the body. Therefore, natural biomolecules need to be incorporated into an appropriate delivery vehicle to achieve a controlled release of the drug molecule over an extended period. In addition to the sustained and controlled delivery, these delivery vehicles also protect the biomolecules against dissociation or deactivation and improve overall bioavailability and clinical efficacy. Figure 2 demonstrates the integration of NMCs within BTE scaffolds for enhanced osseointegration [36].
Figure 2. Integration Tools for Natural Medicinal Compounds and Bone Tissue Scaffold.
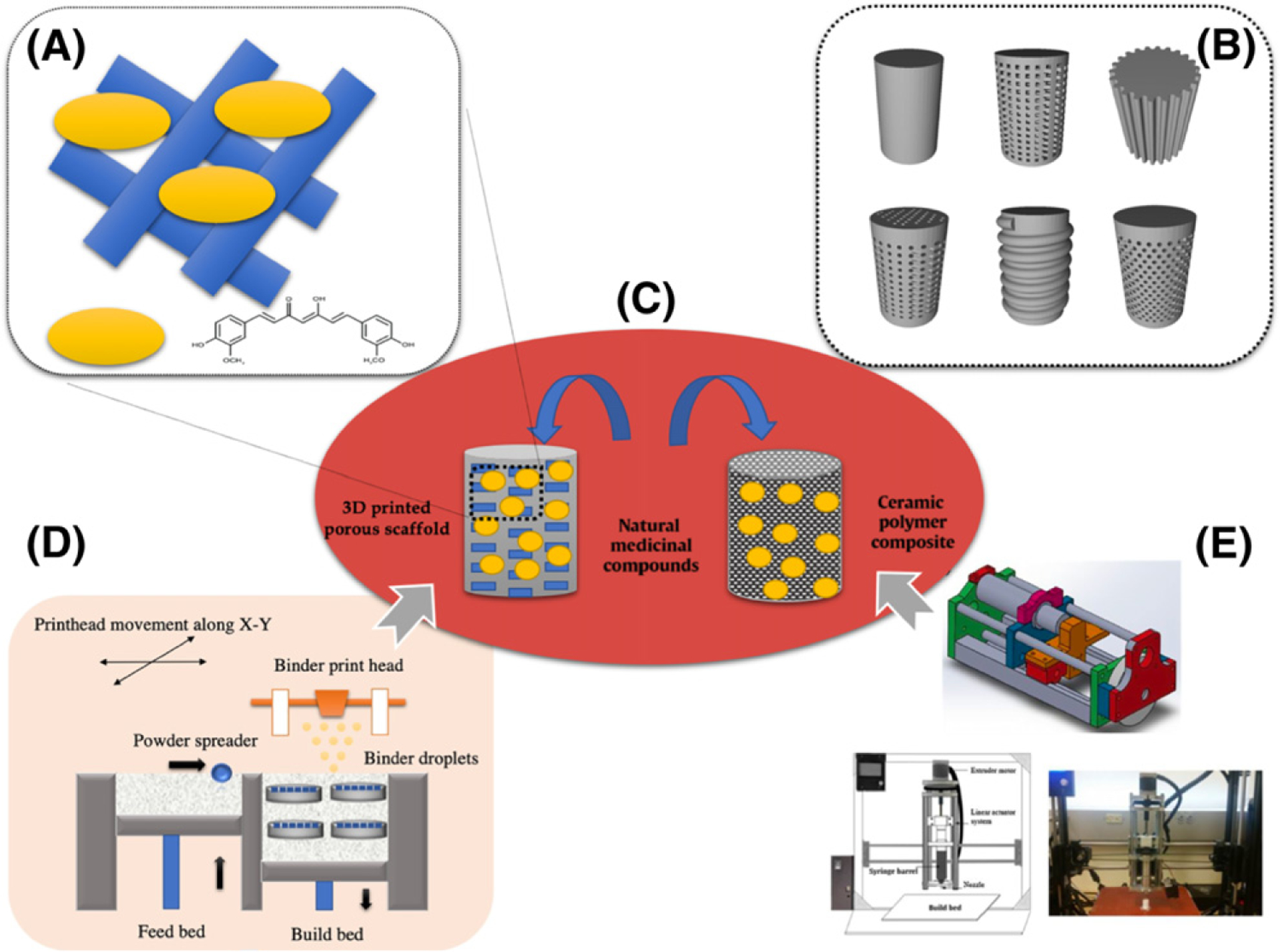
Schematic illustration showing novel integration approaches of natural medicinal compounds and additively manufactured bone scaffolds.
NMCs: Delivery Vehicles for Tissue Engineering Application
The design of the delivery system, including its chemical composition (metal, polymer, ceramics, and composites) and the geometry of the implants (nano/microparticles, porous, or bulk materials), influences the delivery of NMCs. These delivery vehicles can be designed in a wide variety of micelles, vesicles, particles, scaffolds, cements, gels, or nanotubes. CaP ceramics, particularly HA and TCP, are widely used bone graft materials that show excellent potential for localized delivery for biomolecules. Ceramic carriers easily absorb drug molecules owing to their high affinity towards them, resulting in strong retention of the drug molecule [37]. CaP nanoparticles exhibit controlled delivery of biomolecules thanks to their many advantages, such as high surface-to-volume ratio, tailored phase composition, and cell membrane permeability [38–41]. Injectable calcium phosphate cements (CPCs) are also excellent drug delivery carriers; they allow the addition of biomolecules directly into the cement with the help of liquid hardener. The biomolecules in CPC can be distributed homogeneously and can be injected to directly to repair a bone defect. Furthermore, polymeric carriers can be incorporated within the ceramic cement, scaffolds, or nanoparticles to enhance the bioavailability, obtain controlled release, and protect the biological activity of the drug molecule [42–44]. NMCs or biomolecules are incorporated utilizing noncytotoxic and biodegradable polymers such as polylactic acid, polyglycolic acid, their copolymer polylactic-co-glycolic acid (PLGA), poly-ε-caprolactone (PCL), polyethylene, polymethylmethacrylate, or natural hydrogels such as alginate, gelatin, fibrin, collagen, and chitosan. The polymeric delivery vehicle should be degraded subsequently and the degradation product should be nontoxic. In this section, we focus on various methods of incorporating biomolecules in bone scaffolds, which are extensively used for bone tissue regeneration.
Microparticles or nanoparticles are the most widely used drug delivery methods for controlled delivery of natural biomolecules. These microparticles or more efficient nanoparticles have large surface areas and therefore high drug loading efficiency and high reactivity towards surrounding tissues in vivo. They also have high diffusibility and mobility of drug-loaded particles [45–50]. Microcapsules are another emerging technology in which biomolecules are adsorbed or encapsulated within a polymeric vesicle. These are excellent choices for drug delivery to encapsulate labile natural molecules that need to be protected from the harsh surrounding environment. These carriers deliver the biomolecules by desorption, diffusion, or degradation processes based on the chemical composition, interaction, and geometry of the microcapsule. Microcapsule delivery can also provide sustained release kinetics, which is appropriate for long-term biomolecule delivery compared with biomolecules that are absorbed onto biomaterials surface [51,52]. Membranes are effective delivery carriers for biomolecules, which support cell adhesion and proliferation owing to the large tissue-material interface [53,54]. Hydrogels, another drug delivery method, can be integrated with biomaterials for tissue regeneration for the controlled delivery of NMCs. They have several advantages, including optimum hydrophilicity, injectability/moldability, good biological performance, mild preparation method, versatility for biomolecule encapsulation, and tunable release characteristics [55]. The 3D network of hydrogels physically or chemically immobilizes the drug particle within its polymer network by absorbing a large volume of aqueous drug solution and therefore protect the biomolecule from the harsh environment [56]. Injectable hydrogels, which undergo in situ solidification by chemical crosslinking or physical interactions such as electrostatic and hydrophobic interactions, are also suitable for carrying biomolecules [35,57]. Although hydrogels have promising properties for biomedical and tissue engineering applications, their practical applications are limited due to their poor mechanical properties.
Next Generation BTE: Integration Tools
Not much research has been dedicated to integrating synthetic medicinal approaches with herbal medicines for orthopedic applications. In this section, we consolidate the variety of outlooks towards this integration from different biomedical engineering approaches and their applications towards BTE.
One of the most important aspects of multifunctional scaffold design is developing optimal drug delivery kinetics that are suitable for a specific application. For instance, typical drug release profiles with a short-term, initial-burst release are highly desirable for fracture-fixation devices, where an early antibacterial burst prevents infection during the critical stage of postsurgical period. However, a long-term release is also preferred in some cases, where osteoconductive NMCs need to be eluted from resorbable scaffolds at a controlled rate while surrounding tissues will be integrated within time, which takes up to a few months. Controlling release kinetics tends to be more difficult in cases of NMCs with lower bioavailability, such as curcumin. A recent study used porous 3D-printed TCP scaffolds loaded with curcumin to improve the osteogenic potential of bone graft scaffolds. This work demonstrated a promising strategy, where the presence of a hydrophilic and hydrophobic polymer (PCL: PLGA at 65:35 molar ratio) in a certain ratio significantly enhanced the release of curcumin by improving its bioavailability. The results also showed that curcumin enhanced in vitro osteoblast cell viability and proliferation as well as increased in vivo mineralized bone formation compared with control [58] (Figure 3). Another promising mode of drug delivery, liposomal delivery, has been employed for enclosing curcumin to improve its cellular and tissue uptake and, subsequently, incorporation within a 3D-printed porous TCP scaffold to establish its application as a potential bone graft substitute after bone tumor resection [59]. The presence of liposomal curcumin resulted in a 96% decrease in in vitro osteosarcoma cell proliferation and viability after 11 days of incubation. Results from in vitro osteoblast cell culture demonstrate that liposomal curcumin promotes cell attachment, proliferation, viability, and differentiation (Figure 3).
Figure 3. Effects of Curcumin Incorporated 3D Printed Scaffold in Bone Tissue Engineering.
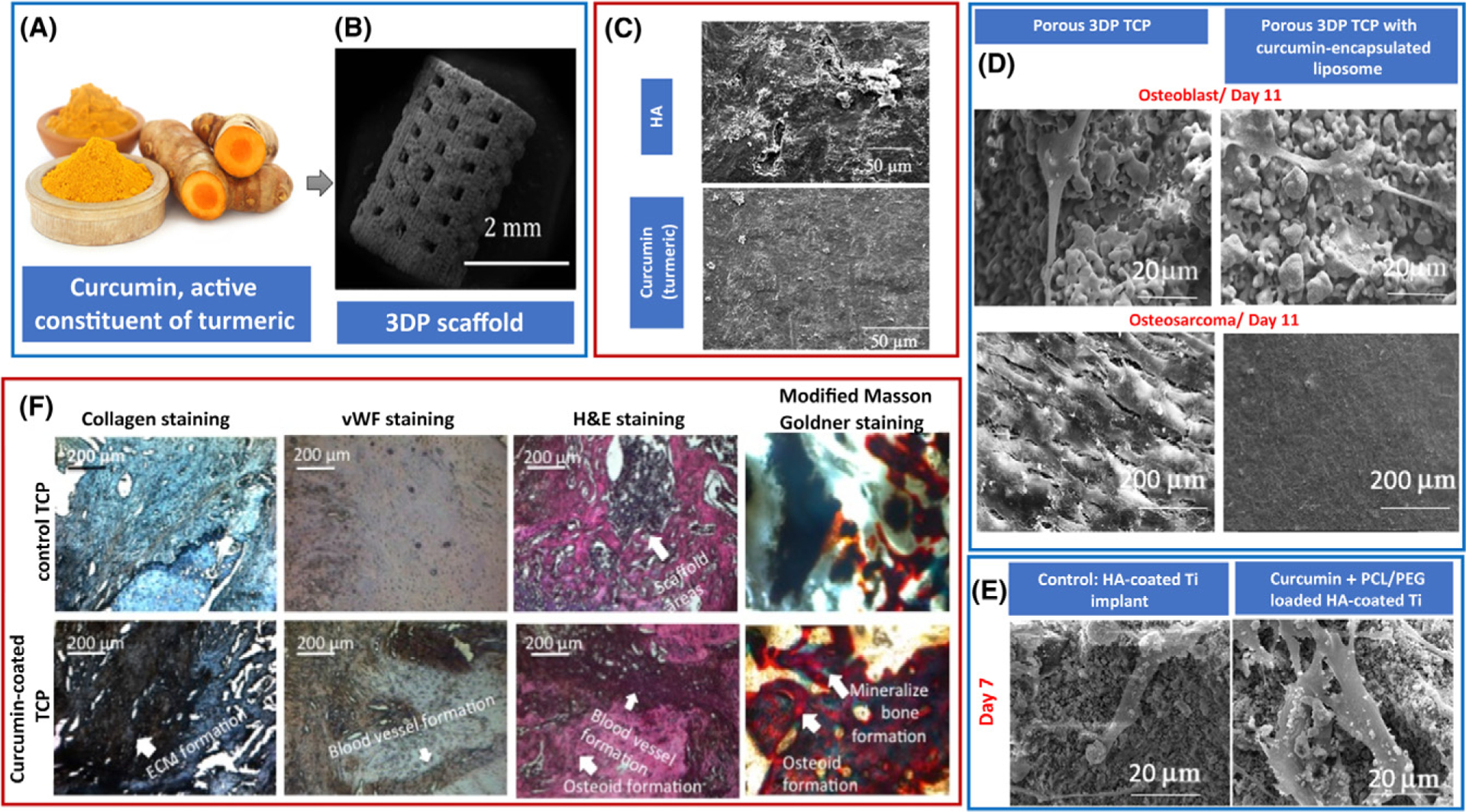
(A) Curcumin, the chief active ingredient from turmeric. (B) Curcumin-coated 3D-printed (3DP) tricalcium phosphate (TCP) scaffolds with designed pores ranging from 340 to 350 μm. (C) Much lesser resorption pits in curcumin-loaded bone implants indicating lower osteoclast activity and therefore reduced bone resorption. (D) Effects of curcumin-encapsulated liposome-coated 3DP scaffolds on osteoblast (healthy bone cell) and osteosarcoma (bone cancer) cells after 11 days of culture; curcumin showed cytotoxicity against osteosarcoma cells by inhibiting the cellular proliferation on the scaffold surface. However, presence of curcumin-encapsulated liposome promoted osteoblast cell attachment and proliferation. (E) Field emission scanning electron microscopy images showing enhanced osteoblast cell attachment and proliferation in presence of curcumin + poly-ε-caprolactone (PCL)/polyethylene glycol (PEG) samples after 7 days of culture. (F) Optical microscopy images of tissue-implant sections after von Willebrand Factor (vWF), hematoxylin and eosin (H&E), collagen, and modified Masson Goldner trichrome staining showing angiogenesis and osteoid-like new bone formation, respectively after 6 weeks of surgery in rat distal femur model. Image reproduced, with permission, from [58,59]. Abbreviations: ECM, Extracellular matrix; HA, hydroxyapatite.
In an alternative approach, curcumin has been coordinated with zinc ions to improve its bioavailability, and ultimately incorporated within a core-shell nanofiber scaffold to achieve controlled release kinetics. This scaffold showed enhanced osteoblast cell viability, proliferation, and ALP activity, as well as good antibacterial activity against Escherichia coli and Staphylococcus aureus [60]. Another interesting and effective method of curcumin drug delivery was reported, where cerium (1–2 mol%), gallium (1–2 mol%), and zinc (2–4 mol%) substituted mesoporous bioactive glass was synthesized to facilitate curcumin uptake and release for BTE application. While unsubstituted and least-substituted cerium, gallium, and zinc (1%, 1%, and 2%, respectively) glass released curcumin within the therapeutic range, higher amounts of these trace metals (2%, 2%, and 4%, respectively) indicated greater retention and lower release of drug [61]. Mesoporous nanostructures were also explored by Chen and colleagues, who designed curcumin-loaded calcium silicate cements to investigate anti-inflammatory properties at the early postimplantation stage. Their results showed the formation of a bone-like apatite layer induced by calcium silicate cements, whereas curcumin inhibited the expression of anti-inflammatory markers such as TNF-α and interleukin-1 [62].
Similarly, electrospun PCL nanofibers were also fabricated for curcumin drug delivery applications due to their ability to balance high drug loading and delivery capability. Their results showed that the presence of 1% curcumin demonstrated enhanced osteogenesis by ALP activity as well as increased gene and protein expression of osteogenic markers [63]. While synthetic electrospun polymeric nanofibers have shown a promising biological effect as potential drug delivery carriers, natural options have been considered as an encouraging alternative, especially for optimum biodegradability and limited toxicity. Electrospun honey nanofibers enriched with garlic, edible mushrooms, and mint showed potential for repair and regenerating bone and damaged skin tissues, indicating its efficacy to be utilized as a biomaterial [64].
A significant amount of research has been performed to incorporate NMCs within a natural polymer-based scaffold such as gelatin and/or chitosan for improved skin tissue regeneration. For example, incorporating Aloe vera and snail (Helix aspersa) secretions into chitosan and gelatin-based scaffold improved the biocompatibility and biodegradability of the natural ingredients and enhanced tissue regeneration [65].
An unconventional approach is the use of acemannan sponges, which have been explored as a natural scaffold to enhance alveolar bone, cementum, and ligament formation for canine periodontal tissue regeneration. These acemannan sponges showed elevated levels of growth factor 5, runt-related transcription factor 2, and BMPs in human periodontal ligament cells model and demonstrated augmented bone formation 2 months after implantation [66]. Another study also reported enhanced osteopontin and ALP expression in vitro and higher BMD in vivo in male Sprague Dawley rats after 4 weeks of treatment with a similar type of acemannan sponge scaffolds [12]. Freeze-dried acemannan sponge has been further proposed in a recent study as a potent biomaterial for bone regeneration. The micro-computed tomography result demonstrated a significant increase in bone volume and tissue mineral density in the acemannan-treated group compared with the control, as revealed by the 4 weeks in vivo study performed in female Sprague Dawley rats. The presence of acemannan also showed denser bone matrix formation with no presence of inflammation in the defect area compared with the control group, as shown by histological analysis [67].
In a recent study, the novel concept of integrating NMCs with a load-bearing tissue engineering scaffold has been successfully realized by developing acemannan-loaded surface-modified titanium alloys for BTE application. The implant, as shown in Figure 4, has demonstrated improved bone formation with a seamless implant interface in a rat distal femur model 5 weeks after implantation. Moreover, the presence of hydrophobic polymer coating of chitosan enhanced bone mineralization and prevented infection, leading to accelerated healing [68].
Figure 4. Effects of Aloe vera Extract on In Vivo and In Vitro Biological Properties of HA-coated Ti Load-Bearing Implants.
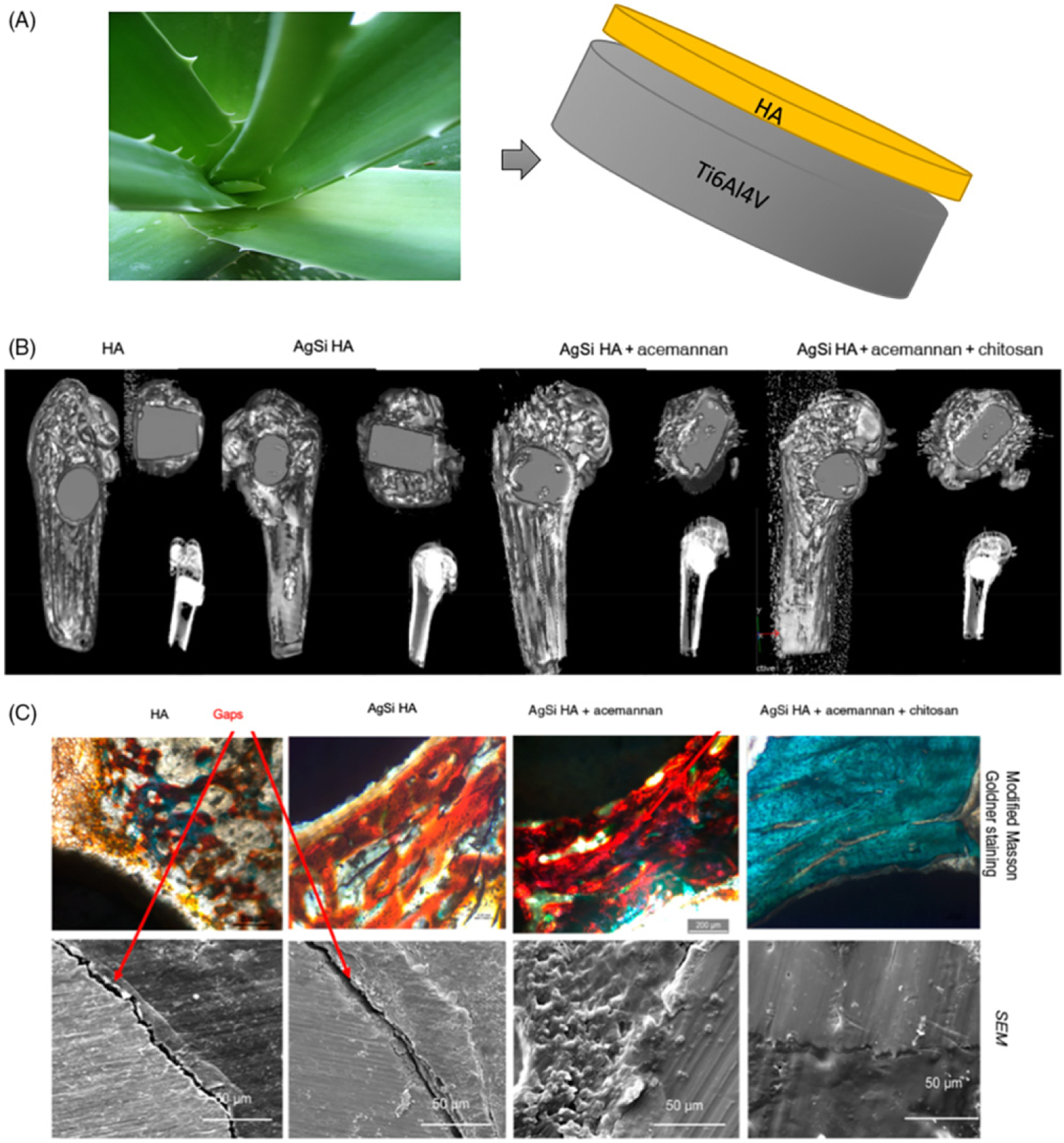
. (A) Acemannan, key component of Aloe vera incorporated hydroxyapatite (HA)-coated Ti implant. (B) Computed tomography scan, (B) histology and scanning electron microscopy (SEM) micrographs of HA-coated Ti64 implants with or without dopants and acemannan. The presence of acemannan improved the osteoid formation, which is evident from the enhanced reddish orange color around the vicinity of the implant. SEM micrographs also showed no gaps at the interface of the acemannan implants. The combined presence of chitosan with acemannan further mineralized the new osteoid formation around the implant, shown by the greenish blue color, leading to improved early stage osseointegration. Osseous tissue had been observed to interlock with the implant in the SEM micrographs, leaving no visible gaps. Image adapted, with permission, from [68].
Concluding Remarks and Future Perspectives
Integrating BTE scaffolds with natural medicinal drug delivery is gaining increased attention due to several advantages over conventional bone grafts, including the ability to design a sustained and controlled release system, improved bone regeneration with reduced side effects, and lowered toxicity compared with systemic drug administration. However, much research is still needed; particularly, there is an unmet demand for a detailed investigation of NMCs integrated with additively manufactured scaffolds to design multifunctional parts, which can find use in a range of BTE applications. This review illustrates some of the primary signs of progress in the tissue engineering field that demonstrate 3D-printed BTE parts can serve as a scaffold to control NMC delivery for new bone tissue formation and regeneration in critical-sized defect repair.
Although major advances have been made recently for the design of ceramic, polymer, or metal bone tissue implants that allow controlled release of NMCs, there remain a number of challenges that need to be addressed in the future (see Outstanding Questions). For effective utilization of NMCs with the combination of modern treatments like 3D-printed prosthesis or bone scaffolds, research needs to be done to optimize the drug-scaffold interaction mechanism, along with the sustained release of the drug molecule from the scaffold to uphold the therapeutic needs in the patient’s body. Other challenges include enhancing the stability of NMCs by encapsulating them to allow extended-release (e.g., weeks to months) and determining the suitable delivery vehicle to allow multiple NMCs to be released with distinct kinetics. Also, improving the release of certain NMCs owing to their hydrophobic nature or strong charge-charge interactions between scaffolds and the NMCs would be an important step towards more validity and comparability in this field. A further major challenge is the adaptation of these approaches for clinical use. Most of the work that has been done involves in vitro or animal models and it is unclear how well much of this work will translate to use in human patients.
Outstanding Questions.
After considering the scaffoldprocessing conditions and sterilization techniques, how can the homogeneous loading/incorporation of the drug throughout the matrix be ensured? What are some other novel drug-loading techniques to ensure that they retain their chemical stability?
How can the drug-release time be accurately controlled and specific quantities of drugs for different bone tissue engineering applications be delivered? How can the release patterns of the drug be engineered, and how are they related to the interaction between the drug and the scaffold? Is it possible to develop a chemical interaction between the scaffold material and biomolecule to better understand the matrix degradation or drug diffusion through the matrix?
Is it possible to incorporate two or more NMCs within a scaffold, which may offer multipronged approaches towards bone tissue regeneration and defect repair? In that case, how can their biphasic release kinetics be tailored in such a way so that one drug can release rapidly during the initial time points followed by the other, which will exhibit a more sustained and controlled release for specific clinical need?
Given the concerns related to the stability and bioavailability of NMCs, what are the other novel drug-delivery approaches that can be utilized to improve their efficacy in bone tissue engineering or in treatment of bone disorder?
How can we optimize a specific concentration of drug needed in relation to the particular local microenvironment and how is this affected by the tissue-material interaction? How can a toxicology profile and safety data for NMCs be developed to ensure proper dosage is being delivered from the scaffold based on specific clinical needs?
How can the mechanism of action of NMCs in relation to a specific tissue engineering application be understood?
The general perception that NMCs are safe and devoid of adverse effects is not only untrue but also misleading. Self-medication, nonexpert consultation, and lack of risk awareness are potentially harmful, and NMCs have been shown to be capable of producing a wide range of undesirable effects in these cases [69]. Other than the safety concerns, risk related to adulteration, contamination, and misidentification is also notable, which may cause serious harm to patients. The extensive range of harmful chemicals associated with NMCs are heavy metals, toxic minerals, pesticides, microbes, and mycotoxins, just to name a few. Deliberate and fraudulent contamination by adding or substituting foreign materials during the production of NMCs constitutes another risk. Furthermore, ensuring effective extraction and quality control of NMCs are more challenging since the composition of active constituents varies with geographic region, environmental changes, and cultivating conditions [70,71]. Hence, scientists developing the scaffolds must establish a certain level of awareness regarding the active concentration, toxic limits, side effects, and possible interaction to prevent serious adverse reactions in the site of implantation. It is equally important that health-related decision-makers such as government bodies, doctors, and pharmaceutical companies are aware of the dissatisfaction with the current clinical application of bone tissue implants, which is the most important reason to consider integrating NMCs and additively manufactured scaffolds. In a broader perspective, further advances in this field will rely on multidisciplinary approaches that combine medicine, chemistry, engineering, and pathology to develop effective strategies to repair critical-sized bone defects. Looking ahead, the combination of NMCs for enhancing bone growth with the advancement of modern BTE technologies opens up a whole new era of research envisioning novel treatment opportunities and solutions.
Highlights.
Bone tissue engineering is a promising approach for secondary reconstruction after severe trauma and bone defects. Their importance led to the establishment of 3D-printed bone graft substitutes, including both load bearing and low-load bearing parts, which offer patient-specific defect repair and bone regeneration.
Current obstacles in the clinical success of bone graft substitutes led to the establishment of multifunctional grafts, where natural medicinal compounds with osteogenic potential were incorporated in additively manufactured grafts for enhanced osseointegration.
Natural medicinal compounds have immense potential towards bone tissue regeneration. Careful investigation of chemical and pharmacological aspects of natural medicinal compounds and their interaction with biomaterials may provide potential directions for researchers in designing scaffolds for bone defect repair.
Acknowledgments
The authors would like to acknowledge financial support from the National Institutes of Health under grant numbers R01 AR066361.
Glossary
- ALP
alkaline phosphatase is generally released from osteoblasts and has a role in the mineralization of newly formed bone
- Angiogenesis
physiological process through which new blood vessel forms. A normal and vital stage during wound healing and tissue formation
- Biocompatibility
ability to be in contact with a living system without having toxic or injurious effects and by performing an appropriate host response in a specific situation
- Biodegradability
ability of materials to be chemically dissolved by bacteria, fungi, or biological means
- BMPs
bone morphogenetic proteins are a group of growth factors with an ability to induce bone formation and stimulate bone growth naturally in the body
- Bone mineral density (BMD)
a measure of mineral amount (calcium and phosphorous) contained in a certain volume of bone. BMD measurements are utilized to diagnose osteoporosis, a condition marked by reduced bone mass
- Bone tissue engineering (BTE)
an interdisciplinary field that applies the use of a combination of cells, engineering materials, and suitable biochemical factors toward the development of biological substitutes that restore, maintain, or improve bone tissue function
- CaP
calcium phosphate
- Critical-sized bone defect
the smallest bone defect that will not heal spontaneously over a long period
- FDA
Food and Drug Administration; a federal agency of the United States Health and Human Services
- Growth factors
naturally occurring substances capable of stimulating cellular growth, proliferation, and differentiation
- HA
hydroxyapatite
- In vitro
(Latin: in glass); studies performed with microorganisms, cells, or biomolecules in a test tube, culture tube, or elsewhere outside a living system
- In vivo
studies performed in a living organism, usually animals
- Osteoblast
mononuclear bone cells, differentiated from mesenchymal stem cells, responsible for bone matrix formation by producing collagen and glycoproteins
- Osteoclast
multinucleated bone cells associated with bone resorption through secretion of acid and collagenase enzyme
- Osteoconductivity
property of a biomaterial by which new bone is directed to conform to a material’s surface. Osteoconductive materials permit attachment, proliferation, and migration of bone cells, leading to bone growth
- Osteogenesis
process of bone formation and regeneration
- Osteoinductive
the recruitment and stimulation of immature cells to develop into bone-forming cells, such as preosteoblasts, osteoblasts, and finally osteocytes
- Osseointegration
direct anchorage of an implant by the formation of bony tissue around the implant without the growth of fibrous tissue at the bone-implant interface
- Revision surgery
surgery performed to remove and replace a failed implant with a new prosthesis (e.g., hip revision surgery)
- Sustained release
a designed release of drug at a predetermined rate in order to maintain a constant effective drug concentration for a specific period
- TCP
tricalcium phosphate
- TRAP
concentration of tartrate-resistant acid phosphatase activity in serum is utilized as a biochemical marker of osteoclast function and degree of bone resorption
- VEGF
vascular endothelial growth factor is a signal protein produced by cells that induces blood vessel formation
References
- 1.Amini AR et al. (2012) Bone tissue engineering: recent advances and challenges. Crit. Rev. Biomed. Eng 40, 363–408 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Younger EM and Chapman MW (1989) Morbidity at bone graft donor sites. J. Orthop. Trauma 3, 192–195 [DOI] [PubMed] [Google Scholar]
- 3.Banwart J et al. (1995) Iliac crest bone graft harvest donor site morbidity. A statistical evaluation. Spine 20, 1055–1060 [DOI] [PubMed] [Google Scholar]
- 4.Delloye C et al. (2007) Bone allografts: what they can offer and what they cannot. J. Bone Joint Surg. Br 89, 574–580 [DOI] [PubMed] [Google Scholar]
- 5.Lord CF et al. (1988) Infection in bone allografts. Incidence, nature, and treatment. J. Bone Joint Surg. Am 70, 369–376 [PubMed] [Google Scholar]
- 6.American Academy of Orthopaedic Surgeons (2003) Bone Graft Substitutes: Facts, Fictions & Applications, American Academy of Orthopedic Surgeons 70th Annual Meeting [Google Scholar]
- 7.Lee K et al. (2010) Growth factor delivery-based tissue engineering: general approaches and a review of recent developments. J. R. Soc. Interface 8, 153–170 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bose S et al. (2018) Enhanced in vivo bone and blood vessel formation by iron oxide and silica doped 3D printed tricalcium phosphate scaffolds. Ann. Biomed. Eng 46, 1241–1253 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bose S et al. (2019) Enhanced bone remodeling on human osteoblast-osteoclast co-culture system using doped hydroxyapatite plasma coatings for musculoskeletal applications. Mater. Today Commun 10.1016/j.mtcomm.2019.05.010 Published online May 17, 2019 [DOI] [Google Scholar]
- 10.Barnes PM et al. (2008) Complementary and alternative medicine use among adults and children: United States, 2007. Natl. Health Stat. Report 10, 1–23 [PubMed] [Google Scholar]
- 11.Foster M et al. (2011) Evaluation of the nutritional and metabolic effects of Aloe vera (Vol. 3). In Herbal Medicine: Biomolecular and Clinical Aspects (Benzie IFF and Wachtel-Galor S, eds), CRC Press [Google Scholar]
- 12.Boonyagul S et al. (2014) Effect of acemannan, an extracted polysaccharide from Aloe vera, on BMSCs proliferation, differentiation, extracellular matrix synthesis, mineralization, and bone formation in a tooth extraction model. Odontology 102, 310–317 [DOI] [PubMed] [Google Scholar]
- 13.Songsiripradubboon S et al. (2017) Stimulation of dentin regeneration by using acemannan in teeth with lipopolysaccharide-induced pulp inflammation. J. Endod 43, 1097–1103 [DOI] [PubMed] [Google Scholar]
- 14.Pengjam Y et al. (2016) NF-κB pathway inhibition by anthrocyclic glycoside aloin is key event in preventing osteoclastogenesis in RAW264. 7 cells. Phytomedicine 23, 417–428 [DOI] [PubMed] [Google Scholar]
- 15.Rohanizadeh R et al. (2016) Therapeutic actions of curcumin in bone disorders. Bonekey Rep. 5, 793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tong W et al. (2016) Curcumin suppresses colon cancer cell invasion via AMPK-induced inhibition of NF-κB, uPA activator and MMP9. Oncol. Lett 12, 4139–4146 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sahebkar A et al. (2016) Curcumin downregulates human tumor necrosis factor-α levels: a systematic review and meta-analysis of randomized controlled trials. Pharmacol. Res 107, 234–242 [DOI] [PubMed] [Google Scholar]
- 18.Bayan L et al. (2014) Garlic: a review of potential therapeutic effects. Avicenna J. Phytomed 4, 1. [PMC free article] [PubMed] [Google Scholar]
- 19.Ding G et al. (2016) Allicin inhibits oxidative stress-induced mitochondrial dysfunction and apoptosis by promoting PI3K/AKT and CREB/ERK signaling in osteoblast cells. Exp. Ther. Med 11, 2553–2560 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chen Y et al. (2016) Alliin attenuated RANKL-induced osteoclastogenesis by scavenging reactive oxygen species through inhibiting Nox1. Int. J. Mol. Sci 17, 1516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mashhadi NS et al. (2013) Anti-oxidative and anti-inflammatory effects of ginger in health and physical activity: review of current evidence. Int. J. Prev. Med 4, S36. [PMC free article] [PubMed] [Google Scholar]
- 22.Funk JL et al. (2016) Anti-inflammatory effects of the essential oils of ginger (Zingiber officinale Roscoe) in experimental rheumatoid arthritis. PharmaNutrition 4, 123–131 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Suzuki Y et al. (2012) Health-promoting effects of green tea. Proc. Jpn. Acad. Ser. B 88, 88–101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Muraki S et al. (2007) Diet and lifestyle associated with increased bone mineral density: cross-sectional study of Japanese elderly women at an osteoporosis outpatient clinic. J. Orthop. Sci 12, 317–320 [DOI] [PubMed] [Google Scholar]
- 25.Shen C-L et al. (2011) Green tea and bone health: evidence from laboratory studies. Pharmacol. Res 64, 155–161 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Shen CL et al. (2011) Supplementation with green tea polyphenols improves bone microstructure and quality in aged, orchidectomized rats. Calcif. Tissue Int 88, 455–463 [DOI] [PubMed] [Google Scholar]
- 27.Shen CL et al. (2009) Green tea and bone metabolism. Nutr. Res 29, 437–456 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Messina M (2016) Soy and health update: evaluation of the clinical and epidemiologic literature. Nutrients 8, 754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Li B and Shifeng Y (2003) Genistein prevents bone resorption diseases by inhibiting bone resorption and stimulating bone formation. Biol. Pharm. Bull 26, 780–786 [DOI] [PubMed] [Google Scholar]
- 30.Yamaguchi M and Gao YH (1998) Inhibitory effect of genistein on bone resorption in tissue culture. Biochem. Pharmacol 55, 71–76 [DOI] [PubMed] [Google Scholar]
- 31.Putnam SE et al. (2007) Natural products as alternative treatments for metabolic bone disorders and for maintenance of bone health. Phytother. Res 21, 99–112 [DOI] [PubMed] [Google Scholar]
- 32.Bose S et al. (2012) Recent advances in bone tissue engineering scaffolds. Trends Biotechnol. 30, 546–554 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bose S et al. (2018) Additive manufacturing of biomaterials. Prog. Mater. Sci 93, 45–111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bose S et al. (2018) Surface modification of biomaterials and biomedical devices using additive manufacturing. Acta Biomater. 66, 6–22 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Tarafder S and Bose S (2014) Polycaprolactone-coated 3D printed tricalcium phosphate scaffolds for bone tissue engineering: in vitro alendronate release behavior and local delivery effect on in vivo osteogenesis. ACS Appl. Mater. Interfaces 6, 9955–9965 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Koski C et al. (2018) Starch-hydroxyapatite composite bone scaffold fabrication utilizing a slurry extrusion-based solid freeform fabricator. Addit. Manuf 24, 47–59 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bose S and Tarafder S (2012) Calcium phosphate ceramic systems in growth factor and drug delivery for bone tissue engineering: a review. Acta Biomater. 8, 1401–1421 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Uskoković V and Uskoković DP (2011) Nanosized hydroxyapatite and other calcium phosphates: chemistry of formation and application as drug and gene delivery agents. J. Biomed. Mater. Res. B Appl. Biomater 96, 152–191 [DOI] [PubMed] [Google Scholar]
- 39.Habraken WJEM et al. (2007) Ceramic composites as matrices and scaffolds for drug delivery in tissue engineering. Adv. Drug Deliv. Rev 59, 234–248 [DOI] [PubMed] [Google Scholar]
- 40.Bose S et al. (2018) Effects of polycaprolactone on alendronate drug release from Mg-doped hydroxyapatite coating on titanium. Mater. Sci. Eng C 88, 166–171 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Epple M et al. (2010) Application of calcium phosphate nanoparticles in biomedicine. J. Mater. Chem 20, 18–23 [Google Scholar]
- 42.Tarafder S et al. (2013) Lovastatin release from polycaprolactone coated β-tricalcium phosphate: effects of pH, concentration and drug–polymer interactions. Mater. Sci. Eng C 33, 3121–3128 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Bose S et al. (2019) Sustained release of vitamin C from PCL coated TCP induces proliferation and differentiation of osteoblast cells and suppresses osteosarcoma cell growth. Mat. Sci. Eng. C 105, 110096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Li M et al. (2009) Creation of macroporous calcium phosphate cements as bone substitutes by using genipin-crosslinked gelatin microspheres. J. Mater. Sci. Mater. Med 20, 925–934 [DOI] [PubMed] [Google Scholar]
- 45.Biondi M et al. (2008) Controlled drug delivery in tissue engineering. Adv. Drug Deliv. Rev 60, 229–242 [DOI] [PubMed] [Google Scholar]
- 46.Mouriño V and Boccaccini AR (2009) Bone tissue engineering therapeutics: controlled drug delivery in three-dimensional scaffolds. J. R. Soc. Interface 7, 209–227 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Bose S et al. (2017) Effect of chemistry on osteogenesis and angiogenesis towards bone tissue engineering using 3D printed scaffolds. Ann. Biomed. Eng 45, 261–272 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Freiberg S and Zhu XX (2004) Polymer microspheres for controlled drug release. Int. J. Pharm 282, 1–18 [DOI] [PubMed] [Google Scholar]
- 49.Yang L and Webster TJ (2009) Nanotechnology controlled drug delivery for treating bone diseases. Expert Opin. Drug Deliv 6, 851–864 [DOI] [PubMed] [Google Scholar]
- 50.Tabata Y (2003) Tissue regeneration based on growth factor release. Tissue Eng. 9, 5–15 [DOI] [PubMed] [Google Scholar]
- 51.Habraken WJEM et al. (2008) PLGA microsphere/calcium phosphate cement composites for tissue engineering: in vitro release and degradation characteristics. J. Biomat. Sci. Polym. Ed 19, 1171–1188 [DOI] [PubMed] [Google Scholar]
- 52.Eley JG and Mathew P (2007) Preparation and release characteristics of insulin and insulin-like growth factor-one from polymer nanoparticles. J. Microencapsul 24, 225–234 [DOI] [PubMed] [Google Scholar]
- 53.Needleman I et al. (2002) A systematic review of guided tissue regeneration for periodontal infrabony defects. J. Periodontal Res 37, 380–388 [DOI] [PubMed] [Google Scholar]
- 54.Retzepi M and Donos N (2010) Guided bone regeneration: biological principle and therapeutic applications. Clin. Oral Implants Res 21, 567–576 [DOI] [PubMed] [Google Scholar]
- 55.Slaughter BV et al. (2009) Hydrogels in regenerative medicine. Adv. Mater 21, 3307–3329 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Yamamoto M et al. (2001) Controlled release of growth factors based on biodegradation of gelatin hydrogel. J. Biomater. Sci. Polym. Ed 12, 77–88 [DOI] [PubMed] [Google Scholar]
- 57.Kretlow JD et al. (2009) Injectable biomaterials for regenerating complex craniofacial tissues. Adv. Mater 21, 3368–3393 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Bose S et al. (2018) Effects of PCL, PEG and PLGA polymers on curcumin release from calcium phosphate matrix for in vitro and in vivo bone regeneration. Mater. Today Chem 8, 110–120 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Sarkar N and Bose S (2019) Liposome-encapsulated curcumin-loaded 3D printed scaffold for bone tissue engineering. ACS Appl. Mater. Interfaces 11, 17184–17192 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Sedghi R et al. (2018) Novel biocompatible zinc-curcumin loaded coaxial nanofibers for bone tissue engineering application. Polymer 142, 244–255 [Google Scholar]
- 61.Shruti S et al. (2013) Curcumin release from cerium, gallium and zinc containing mesoporous bioactive glasses. Microporous Mesoporous Mater. 180, 92–101 [Google Scholar]
- 62.Chen Y-C et al. (2017) Anti-inflammation performance of curcumin-loaded mesoporous calcium silicate cement. J. Formos. Med. Assoc 116, 679–688 [DOI] [PubMed] [Google Scholar]
- 63.Jain S et al. (2016) Curcumin eluting nanofibers augment osteogenesis toward phytochemical based bone tissue engineering. Biomed. Mater 11, 055007. [DOI] [PubMed] [Google Scholar]
- 64.Shahbazi E and Bahrami K (2019) Production and properties analysis of honey nanofibers enriched with antibacterial herbal extracts for repair and regeneration of skin and bone tissues. J. Pharm. Pharmacol 7, 37–50 [Google Scholar]
- 65.Angulo DEL and do Amaral Sobral PJ (2016) Characterization of gelatin/chitosan scaffold blended with Aloe vera and snail mucus for biomedical purpose. Int. J. Biol. Macromol 92, 645–653 [DOI] [PubMed] [Google Scholar]
- 66.Chantarawaratit P et al. (2014) Acemannan sponges stimulate alveolar bone, cementum and periodontal ligament regeneration in a canine class II furcation defect model. J. Periodontal Res 49, 164–178 [DOI] [PubMed] [Google Scholar]
- 67.Godoy DJD et al. (2018) Acemannan increased bone surface, bone volume, and bone density in a calvarial defect model in skeletally-mature rats. J. Dent. Sci 13, 334–341 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Banerjee D and Bose S (2019) Effects of Aloe vera gel extract in doped hydroxyapatite coated titanium implants on in vivo and in vitro biological properties. ACS Appl. Bio Mater 2, 3194–3202 [DOI] [PubMed] [Google Scholar]
- 69.White A et al. (2014) Reducing the risk of complementary and alternative medicine (CAM): challenges and priorities. Eur. J. Integr. Med 6, 404–408 [Google Scholar]
- 70.Zhang J et al. (2012) Quality of herbal medicines: challenges and solutions. Complement. Ther. Med 20, 100–106 [DOI] [PubMed] [Google Scholar]
- 71.Ekor M (2014) The growing use of herbal medicines: issues relating to adverse reactions and challenges in monitoring safety. Front. Pharmacol 4, 177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Altman RD and Marcussen KC (2001) Effects of a ginger extract on knee pain in patients with osteoarthritis. Arthritis Rheumatol. 44, 2531–2538 [DOI] [PubMed] [Google Scholar]
- 73.Funk JL et al. (2012) Effects of ginger (Zingiber officialis L) on inflammation-induced bone loss. FASEB J. 26, 263–265 [Google Scholar]
- 74.Mukherjee M et al. (2004) Prevention of bone loss by oil extract of garlic (Allium sativum Linn.) in an ovariectomized rat model of osteoporosis. Phytother. Res 18, 389–394 [DOI] [PubMed] [Google Scholar]
- 75.Mukherjee M et al. (2006) Role of oil extract of garlic (Allium sativum Linn.) on intestinal transference of calcium and its possible correlation with preservation of skeletal health in an ovariectomized rat model of osteoporosis. Phytother. Res 20, 408–415 [DOI] [PubMed] [Google Scholar]
- 76.Hie M et al. (2009) Curcumin suppresses increased bone resorption by inhibiting osteoclastogenesis in rats with streptozotocin-induced diabetes. Eur. J. Pharmacol 621, 1–9 [DOI] [PubMed] [Google Scholar]
- 77.Bharti AC et al. (2004) Curcumin (diferuloylmethane) inhibits receptor activator of NF-κB ligand-induced NF-κB activation in osteoclast precursors and suppresses osteoclastogenesis. J. Immunol 172, 5940–5947 [DOI] [PubMed] [Google Scholar]
- 78.French DL et al. (2008) The ovariectomized, mature rat model of postmenopausal osteoporosis: an assessment of the bone sparing effects of curcumin. Phytomedicine 15, 1069–1078 [DOI] [PubMed] [Google Scholar]
- 79.Cotter A and Cashman KD (2003) Genistein appears to prevent early postmenopausal bone loss as effectively as hormone replacement therapy. Nutr. Rev 61, 346–351 [DOI] [PubMed] [Google Scholar]
- 80.Koh W-P et al. (2009) Gender-specific associations between soy and risk of hip fracture in the Singapore Chinese Health Study. Am. J. Epidemiol 170, 901–909 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Pawlowski JW et al. (2015) Impact of equol-producing capacity and soy-isoflavone profiles of supplements on bone calcium retention in postmenopausal women: a randomized crossover trial. Am. J. Clin. Nutr 102, 695–703 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Shen CL et al. (2008) Protective effect of green tea polyphenols on bone loss in middle-aged female rats. Osteoporosis Int. 19, 979–990 [DOI] [PubMed] [Google Scholar]
- 83.Lin SY et al. (2018) (−)-Epigallocatechin-3-gallate (EGCG) enhances osteogenic differentiation of human bone marrow mesenchymal stem cells. Molecules 23, 3221. [DOI] [PMC free article] [PubMed] [Google Scholar]


