Abstract
Objectives:
To investigate the effects of different walking aids (single cane, bilateral forearm crutch and walker) on gait parameters and kinematic analysis of pelvis in patients having adult neuromuscular diseases.
Methods:
The study design was a self-controlled study. The study was conducted in the Department of Physiotherapy and Rehabilitation, Hacettepe University in Ankara, Turkey, between 2014-2015. The study included 18 adult patients with neuromuscular disease. The manual muscle test, the Rivermead mobility index, the motor function assessment scale, and the trunk control test were used as descriptive measurements. The 2-minute walking test, the modified Borg scale and the G-Walk gait analysis system (BTS Bioenginering S.p.A., Italy) were used as the outcome measures. The outcome measures were performed randomly during normal gait without walking aids (self control group), then during walking with single point cane, bilateral forearm crutch and walker.
Results:
It was observed that the walking aids have decreased the walking speed, walking distance and cadence. When the pelvis kinematic was analyzed, there was only a significant difference in the extension of the pelvis between the groups (p<0.05). The most useful (61%), most comfortable (44.4%) and the most preferred (61%) walking aid was determined as single cane by patients and the safest (55%) one was determined as a walker.
Conclusion:
Conclusion: In the decision-making process for walking aids, the patient’s biomechanical, physiological and psychosocial needs, expectations, satisfactions and levels of independence should be considered before providing patients with aids for walking.
Neurological problems usually cause disrupting of walking and the need for assistive devices for walking.1 Basic expectations related to the rehabilitation of neurological patients are a continuation of the functional walking activities and participation.2 For this purpose, the most appropriate walking aids must be selected by taking into account the existing neurological conditions of the walking. The use of walking aids have physical, psychological and functional effects on patients such as improving the confidence, safety and patient’s activity.3,4 However, in the literature, there are studies mentioning the adverse effects of assistive devices when used incorrectly affecting the balance negatively and resulting in falling.3 Improper use of walking aids, lack of user information and education, using duration, insufficiency of the walking aids analysis are causes of problems for patients.5-7
In fact, there is not enough information and guidance concerning the use of walking aids in adult neuromuscular disease for the rehabilitation in the literature. Preferences to use walking aids in clinical use are usually made based on the experiences of other neurological disorders. On the other hand, in the neuromuscular disease, patients use gravity to compensate for their progressive weakening of the muscles to maintain functioning and for developing their compensatory postural responses. External supports such as orthotics and walking aids affect the center of gravity and also these compensatory responses, eventually result unexpectedly disadvantageous functional consequences. Therefore, it is not appropriate to generalize the walking aids decisions as based on other neurological disorders.8 Thus, there is a need to analyze the advantages and disadvantages of the use of walking aids to evaluate the impact on neuromuscular disorders.
Generally, the studies on the use of walking aids are focused on the capacity of walking and the stability. These studies do not provide adequate information about the effects of walking aids on the functional parameters and pelvic kinematics during the walking activity. Therefore, the purpose of this study is to investigate the parameters of different assistive walking aids (single-point cane, bilateral forearm crutch, walker) and to identify the selection criteria of assistive walking aids device for the adult neuromuscular disease.
Methods
Out-patients diagnosed with the neuromuscular disease by the neurologists were invited to the Center of Neuromuscular Diseases of Physical Therapy and Rehabilitation Department at Hacettepe University, Ankara, Turkey.
Cases, who were over 18 years of age, trunk and limb without having any orthopedic problem that was affecting the trunk and extremity performance, without any neurological disease other than muscle disease, who can walk 10 meters unassisted or with the help of a walking aid, who do not have cognitive problems or cooperation difficulties, who have at least 2 falling stories in 6 months and who were volunteers, were included in the study. Cases having previous spinal surgery or orthopedic procedures affecting the walking performance, having cardiac problems with chronic and acute bronchitis, diabetes, Chronic Obstructive Pulmonary Disease (COPD), pulmonary disease, pneumonia with hypertension, and the patients refusing to participate were excluded from the study. The study design was a self-controlled study.
Patients included in the study were given information about the study, and the informed consent forms were signed by them. Turgut Ozal University clinical research ethics committee and meeting No. 2015/03 in Ankara, Turkey, followed our study and found to comply with ethical and scientific principles. The study was performed according to principles of Helsinki Declaration.
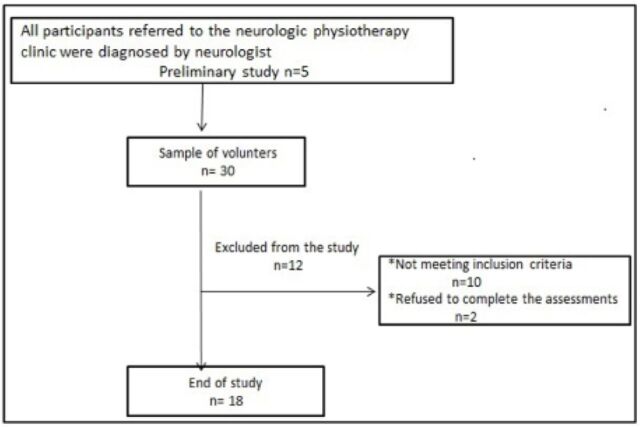
The preliminary study was conducted with 5 cases that were meeting the inclusion criteria. A sample size calculation was made with the statistical consultants by evaluating the results of the preliminary study. It was assumed that; for the walking speed which was determined as the primary parameter of the study, the least difference would be 7 m/min (which was obtained from the pilot study) between the 4 groups and having 20% standard deviation in the groups, and having 65 m/min (which was obtained from the pilot study) walking speed in normal patient group. In order to show significant statistical differences between the methods at 80% power with a 0.05 type 1 error; after the initial measurements it was found necessary to include 18 patients to whom all 3 applications, which are single point canes, bilateral forearm crutches and walkers, in the ongoing study. After preliminary study, 30 patients more were also invited to join the study, but 12 of them were excluded due to the inclusion and exclusion criteria. As a result, the study was continued along with the preliminary study and 18 patients. The flow chart of the study is shown in (Figure 1).
Figure 1.
The flow chart our the study To investigate the effects of different walking aids (single cane, bilateral forearm crutch and walker) on gait parameters and kinematic analysis of pelvis in patients having adult neuromuscular diseases.
Procedure
Descriptive and socio-demographic characteristics of the patients and their disease information were recorded. The manual muscle test (MMT) for muscle strength, the Rivermead mobility index (RMI) for levels of mobility, the motor function assessment (MFM) scale for motor function level, and the trunk control test (TCT) for trunk control of the cases were used as descriptive measurements. The 2-minute walking test (2MWT) for functional capacity, the modified Borg scale (MBS) for perceived fatigue, the G-Walk gait analysis system for the pelvis kinematic analysis and the gait parameters were used as the outcome measures. The outcome measures were performed on patients during normal gait without walking aids (self control group), then were performed on the same patients during walking with single point cane, bilateral forearm crutch and walker, randomly.
At first, the MBS was conducted to patients. If the MBS value is less than 2, the measurements of outcome are started. The patients between each measurement were absolutely rested until the MBS value fell below 2. G-Walk analysis sensors were attached to patients. Then patients started to 2MWT. The G-Walk analysis system recorded gait parameters and pelvis kinematics during the 2MWT. After expiring the 2-minute period, patients positions were marked on the walking test area. Borg fatigue assessments were conducted, and G-Walk analysis sensor were removed from the patients. The 2MWT distance was measured in walking test area and the sensor information was transferred to the computer by the physiotherapist. The other measurements were performed after the perceived borg fatigue value dropped below 2. When the measurements for self-control group were finalized; the patients were asked to repeat the 2MWT with G-Walk analysis sensor randomly by using: a single point cane, bilateral forearm crutch and walker, and the same processes applied to the self control group were repeated. Finally, our patients were asked the questions “Which walking aid was more useful for you? Which was safer? Which was more comfortable to use? If you were obliged to use one, which one would you choose?”. And their thoughts and preferences about the walking aids were recorded.
Assessment tools: muscle strength assessment
Upper limb, lower limb and trunk muscles were evaluated using manual muscle testing.9 Lower abdominal, upper abdominal and right oblique muscle, left oblique muscle, back extensors and the right and left trunk lateral flexor values and total muscle strength values were calculated between 0-35, as the total trunk muscle strength. Shoulder flexors, extensors, abductors, elbow flexors, elbow extensors, wrist flexors and extensors were evaluated, and the muscle strength values were collected from the 7 muscles and were calculated between 0-35, as the upper extremity muscle strength. Right and left upper limb muscle strength values were collected (from 0-70) and were expressed as the sum of the upper extremity muscle strength. Hip flexors, extensors, hip abductor and adductors, knee flexors and extensors, foot dorsi-flexors and plantar flexors were evaluated and their strength values were summed between a value of 0-40 as the lower limb muscle strength.
Mobility level assessment
Rivermead mobility index was applied to assess the mobility levels in the study. Rivermead mobility index, which was developed by Colleen FM et al,10 provided 15 mobility parameters. The results were evaluated on a scale between 0 as minimum, and 15 as maximum points.
Motor function level assessment
In the study, motor function levels were evaluated by MFM scale which was developed specifically for the neuromuscular disease patients. This scale was developed by Be’rard et al,11 and the validity and reliability studies have been conducted for the neuromuscular disease patients. The minimum scale was 0 and the maximum value was 96, which corresponded to a good level of motor function.
Trunk control assessment
In the study, trunk control assessments were performed by the TCT, which was developed in 1990 by Collin & Wade. The total score for trunk control varied between 0-100. High scores indicated better performance.10,12 The reliability and validity studies have been conducted for the neuromuscular disease patients by Parlak Demir Y et al.13
Functional capacity assessment
Functional capacity was evaluated by 2-MWT. The distance walked by the individual in 2-minutes was measured in meters. It was recorded in the walk distance meters. The validity studies have been conducted for the neuromuscular disease patients.14
Assessment of gait parameters
The gait parameters were evaluated by a G-WALK Temporo-spatial gait analysis system. In this system, the analysis results of the sensor attached to the L5-S1 level of the patient was transferred to a computer via bluetooth. This system allows gait analysis by comparing the left and right extremities with normal values; and also enables the 3-dimensional kinematic analysis of the pelvis. Thus, it provides a functional analysis of gait disorders in normal walking areas by soft tissue injuries, amputations and neuromuscular diseases.15-17
Assessment of fatigue
It was evaluated by the MBS. The Borg scale was developed to measure the effort given during physical activity by Borg in 1970. It is used to assess the severity of frequent exercise and rest dyspnea scale and consists of 10 items assessing the dyspnea severity according to the levels.18
Statistical analysis
Windows-based Statistical package for the Social Science (SPSS) Version 15.0 (SPSS Inc., Chicago, IL, USA) analysis program was used for the statistical analysis. Descriptive statistics were performed for the demographic data. Mean±standard deviation was used for the measured variables, and percentages; and the frequency values were used for the calculated variables. For the data, the distribution visual and digital methods were used. Normal data distribution was evaluated by the Kolmogorov Smirnov test and Shapiro-Wilk test values. If p-value<0.05, it was decided that there was an abnormal distribution, and the non-parametric tests were used. For the parametric test assumptions, comparison of more than 4 independent variables were performed by the repeated variance analysis. For the non-parametric (non-normal distribution) data, the Friedman test and Wilcoxon paired 2 sample test. For all assessments, the significance value was taken as p<0.05 and p<0.001.19,20
Results
The study included a total of 18 adult patient with neuromuscular disease, 10 females (55.6%) and, 8 males (44.4%). The mean patient age was 38.66±14.94 years. Descriptive assessment results and 2-MWT walking distances results were given in Table 1. Results of gait parameters with and without walk aids were showed Table 2. The results of different walking parameters with walking aids from self control group walking parameters as percentages are given in Table 3. The differences of gait parameters with walking aids from the self control group gait parameters for the normal distribution data and non-normal distribution data are shown in Table 4 & 5.
Table 1.
The results of descriptive assessments and 2-MWT distances (N=18).
| Characteristics | Mean±SD |
|---|---|
| Age (years) | 38.66±14.94 |
| Height (cm) | 169.22±8.94 |
| Weight (kg) | 66.66±16.09 |
| Duration of diseases (years) | 16.05±8.50 |
| MFM (0-96) | 71.61±9.75 |
| RMI (0-15) | 12.66±1.94 |
| TCT (0-100) | 76.33±20.95 |
| Total of upper muscle strength (0-70) | 45.63±7.23 |
| Total of lower muscle strength (0-80) | 35.47±6.54 |
| Total of trunk muscle strength (0-35) | 32.17±5.68 |
| Distances of 2-MWT normal gait without walking aids | 107.77±27.27 |
| Distances of 2-MWT with single point cane | 99.50±24.76 |
| Distances of 2-MWT with bilateral forearm cructh | 88.64±33.06 |
| Distances of 2-MWT with walker | 54.16±16.42 |
MFM - motor function measurement, RMI - rivearmead mobility index, TCT - trunk control test, 2-MWT - 2-minutes walk test, SD - standard deviation
Table 2.
Results of gait parameters with and without walk aids.
| Gait parameters | Self control group (normal gait without walk aids) | Single point cane | ||||
|---|---|---|---|---|---|---|
| Mean±SD | M | IQR 25-75 | Mean±SD | M | IQR 25-75 | |
| Speed | 65.57±15.29 | 64.70 | 48.37-74.75 | 54.35±10.75 | 52.40 | 45.67-61.85 |
| Cadence | 50.47±5.47 | 50.40 | 45.05-55.47 | 45.19±5.73 | 45.80 | 42.52-49.12 |
| Stride length | 1.27±0.21 | 1.26 | 1.13-1.41 | 1.21±0.20 | 1.19 | 1.05-1.28 |
| Gait cycle duration | 1.20±0.13 | 1.19 | 1.08-1.19 | 1.36±0.18 | 1.31 | 1.25-1.41 |
| Left step time | 0.60±0.06 | 0.59 | 0.51-0.67 | 0.67±0.09 | 0.66 | 0.62-0.71 |
| Right step time | 0.59±0.06 | 0.58 | 0.54-0.67 | 0.68±0.10 | 0.66 | 0.63-0.71 |
| Left step percentage | 50.21±0.81 | 50.20 | 49.87-50.75 | 49.43±1.72 | 49.80 | 48.75-50.30 |
| Right step percentage | 49.86±0.78 | 49.95 | 49.52-50.20 | 50.66±1.79 | 50.50 | 49.62-51.35 |
| Stance phase | 62.72±5.39 | 61.55 | 59.62-63.37 | 61.88±3.52 | 61.75 | 60.25-62.70 |
| Swing phase | 35.55±5.49 | 37.05 | 34.90-38.40 | 36.67±3.49 | 36.95 | 35.92-38.32 |
| Double support duration | 12.69±2.86 | 12.25 | 10.57-14.22 | 12.60±3.42 | 12.45 | 10.95-13.35 |
| Single support duration | 36.41 | 37.05 | 34.67-38.40 | 36.67±3.49 | 36.95 | 35.92-38.32 |
|
| ||||||
| Gait parameters | Bilateral forearm crutch | Walker | ||||
| X±SD | M | IQR 25-75 | X±SD | M | IQR 25-75 | |
|
| ||||||
| Speed | 48.48±8.19 | 47.80 | 42.75-56.52 | 40.46±12.36 | 44.35 | 32.15-47.25 |
| Cadence | 38.12±10.55 | 41.70 | 36.67-43.27 | 32.36±11.24 | 35.05 | 21.82-40.97 |
| Stride length | 1.17±0.24 | 1.12 | 1.04-1.38 | 1.28±0.19 | 1.24 | 1.15-1.51 |
| Gait cycle duration | 1.50±0.24 | 1.42 | 1.36-1.55 | 2.91±1.10 | 1.71 | 1.46-2.78 |
| Left step time | 0.77±0.15 | 0.72 | 0.68-0.78 | 1.09±0.54 | 0.86 | 0.74-1.40 |
| Right step time | 0.74±0.12 | 0.71 | 0.67-0.76 | 1.06±0.51 | 0.85 | 0.71-1.31 |
| Left step percentage | 50.82±1.54 | 50.55 | 49.82-51.62 | 50.28±1.47 | 50.15 | 49.35-50.95 |
| Right step percentage | 49.40±1.03 | 49.60 | 48.45-50.20 | 49.30±2.09 | 49.85 | 48.10-50.67 |
| Stance phase | 63.05±5.97 | 61.10 | 60.32-63.17 | 64.85±6.09 | 63.30 | 60.30-67.62 |
| Swing phase | 36.37±5.05 | 37.30 | 35.87-38.32 | 33.92±6.19 | 36.20 | 31.70-38.35 |
| Double support duration | 13.35±5.22 | 11.95 | 11.00-14.05 | 15.41±6.14 | 13.25 | 10.87-17.60 |
| Single support duration | 36.37±5.05 | 37.30 | 35.87-38.32 | 33.92±6.19 | 36.20 | 31.70-38.35 |
SD - standard deviation, M - median, IQR - interquartile range
Table 3.
The results of different walking parameters with walking aids from self control group walking parameters as percentages.
| Gait parameters | Single point cane % | Bilateral forearm crutch % | Walker % |
|---|---|---|---|
| Speed | 20.64 decrease | 35.25 decrease | 62.06 decrease |
| Cadence | 11.68 decrease | 32.39 decrease | 55.96 decrease |
| Stride length | 4.95 decrease | 8.54 decrease | 0.78 decrease |
| Gait cycle duration | 11.76 increase | 20.00 increase | 58.76 increase |
| Left step time | 10.44 increase | 22.07 increase | 44.95 increase |
| Right step time | 13.23 increase | 20.27 increase | 44.33 increase |
| Double support duration | 0.71 decrease | 4.94 increase | 17.65 increase |
| Single support duration | 0.70 increase | 0.10 decrease | 7.34 decrease |
| Distances of 2-MWT | 8.30 decrease | 21.58 decrease | 98.98 decrease |
2-MWT - 2-minutes walk test
Table 4.
Comparison of gait parameters between groups for data with normal distribution.
| Parameters | Self control group | The differences of groups | |||||
|---|---|---|---|---|---|---|---|
| Single point cane group | Bilateral forearm crutch | Walker | P-value | ||||
| F | P-value | F | P-value | F | P-value | ||
| Speed | 6.298 | 0.023* | 20.409 | <0.001* | 25.263 | <0.001* | <0.001* |
| Cadence | 18.183 | 0.001* | 24.193 | <0.001* | 41.118 | <0.001* | <0.001* |
| Stride length | 2.650 | 0.122 | 2.466 | 0.149 | 0.020 | 0.135 | 0.889 |
| Left step percentage | 3.193 | 0.092 | 4.137 | 0.040* | 0.36 | 0.058 | 0.851 |
| Right step percentage | 3.107 | 0.096 | 2.481 | 0.051* | 1.125 | 0.134 | 0.304 |
| Distances of 2-MWT (m) | 2.437 | 0.137 | 5.661 | 0.002* | 74.968 | <0.001* | <0.001* |
Variance analysis, p-values are significant (p<0.0027), benferoni correction p/18. 2-MWT - 2-minute walk test, F - variance ratio test.
Table 5.
Comparison of gait parameters between groups for data with non-normal distribution.
| Parameters | Self control group (Wilcoxon test) | The differences of groups (Friedman test) | |||||
|---|---|---|---|---|---|---|---|
| Single point cane | Bilateral forearm crutch | Walker | |||||
| Z | P-value | Z | P-value | Z | P-value | P-value | |
| Gait cycle duration | -3.530 | <0.001** | -3.726 | <0.001* | -3.622 | <0.001* | <0.001* |
| Left step time | -3.322 | 0.001** | -3.725 | <0.001** | -3.623 | <0.001** | <0.001** |
| Right step time | -3.534 | <0.001** | -3.729 | <0.001** | -3.621 | <0.001** | <0.001** |
| Stance phase | -0.588 | 0.556 | -0.240 | 0.811 | -1.810 | 0.070* | 0.042* |
| Swing phase | -1.279 | 0.201 | -1.113 | 0.266 | -1.752 | 0.080* | 0.032* |
| Single support duration | -1.184 | 0.236 | -1.018 | 0.309 | -2.083 | 0.037* | 0.032* |
| Double support duration | - | - | - | - | - | - | 0.060 |
| Pelvic extansion | -1.635 | 0.102 | -2.506 | 0.012* | -1.166 | 0.244 | 0.040* |
Friedman test (*p<0.05) and Wilcoxon test (**p<0.0018), Benferroni correction p/27.
Results on the kinematic analysis of pelvis
When assessing the impact of the pelvis on kinematics, only in pelvis extension, there was a significant difference between the single point cane and the bilateral forearm crutch use. The extension of the pelvis was decreased by the use of each 3 walking aids and the maximum reduction (approximately 25%) was seen in the bilateral forearm crutch use. The results of differences the kinematic analysis of pelvis during walking with walking aids from the kinematic analysis of pelvis during unassisted walking as percentages are shown in Table 6.
Table 6.
The results of different kinematic analysis of pelvis during walking with walking aids from the kinematic analysis of pelvis during normal walking (unassisted walking) as percentages.
| Kinematic analysis of pelvis | Self control group | Single point cane | Bilateral forearm crutch | Walker | Comparison with self control group (%) | ||
|---|---|---|---|---|---|---|---|
| Mean±SD | Single point cane | Bilateral forearm crutch | Walker | ||||
| Flexion of pelvis | 1.08±0.90 | 1.29±1.11 | 1.78±1.62 | 1.71±1.16 | 20.00 increase | 39.32 increase | 36.84 increase |
| Extansion of pelvis | 3.08±1.57 | 2.73±1.53 | 2.47±1.47 | 2.61±1.84 | 12.82 decrease | 24.69decrease | 18.00 decrease |
| Total range of fleksiyon-extansiyon of pelvis | 4.15±1.71 | 3.94±1.30 | 4.26±2.31 | 4.31±2.37 | 5.32 decrease | 2.58 increase | 3.71 increase |
| Right lateral flexion of pelvis | 3.72±3.15 | 3.17±1.80 | 4.30±3.05 | 2.56±2.00 | 17.35 decrease | 13.48 increase | 45.31 decrease |
| Left lateral flexion of pelvis | 3.67±3.34 | 2.89±2.09 | 3.82±3.39 | 2.99±2.00 | 29.98 decrease | 3.92 increase | 22.74 decrease |
| Total range of lateral flexion of pelvis | 7.42±6.42 | 5.76±3.17 | 8.12±6.22 | 5.57±3.85 | 28.81 decrease | 8.62 increase | 33.21 decrease |
| Right rotation of pelvis | 2.42±2.41 | 2.58±2.81 | 3.20±2.71 | 2.37±1.77 | 6.20 increase | 24.37 increase | 2.10 decrease |
| Left rotation of pelvis | 2.59±2.00 | 1.77±1.11 | 2.61±2.21 | 2.19±1.76 | 46.32 decrease | 0.76 increase | 18.26 decrease |
| Total range of rotation of pelvis | 4.97±4.18 | 4.36±3.40 | 5.70±4.18 | 4.58±2.91 | 13.99 decrease | 12.80 increase | 8.51 decrease |
SD - standard deviation.
Results on walking aid preferences of the patients
Walking single point canes were expressed as the most convenient and comfortable walking aid by the patients. The walker was found to be the most reliable but non-preferred walking aid by the patients. The distribution of preferences related to walking aid of patients is shown in Table 7.
Table 7.
Patients preferences of walk aid.
| The questions of patients preferences | Single point cane | Bilateral forearm cructh | Walker | Nothing |
|---|---|---|---|---|
| (%) | ||||
| Which walk aid was useful for you? | (61.1) | (27.8) | (0.0) | (11.1) |
| Which walk aid was comfortable for you? | (44.4) | (27.8) | (16.7) | (11.1) |
| Which walk aid did you feel more confident? | (16.7) | (22.2) | (55.6) | (5.6) |
| Which walk aid would you prefer if you had to use it? | (61.1) | (22.2) | (0.0) | (16.7) |
Discussion
The most important result of our study is the decreasing of the walking speed, walking distance and cadence (the number of steps per minute) by the use of walking aids in adult neuromuscular diseases. Also, when the impact of walking aids on the kinematics of the pelvis, which is the most important key point for the lower part of the body, is assessed, there is only a significant difference between the use of the single point cane and the bilateral forearm crutch for the pelvis extension.
The walking speed is an indicator showing the change in physical performance of the patient, the recovery and social inclusion, the patient’s disorder, balance and physical performance as a reliable method. It is often preferred in order to assess the success of the walking performance and rehabilitation during the rehabilitation applications.21 Tyson SF,22 conducted a study and showed that the speed of walking decreased with mobility aids. However, Polese et al,23 have indicated that walking aids that are provided by considering the patient’s functional status increased walking speed, while these aids were provided not suitable to the patient’s functional status they decreased walking speed of the patient.
According to our study results; using walking aids in adult neuromuscular disease was observed to decrease walking speed, walking distance and cadence (the number of steps per minute). The walking distance showed a significant decrease with the use of bilateral forearm crutch and walker compared to self control group, while no significant difference was found between walking with single point cane and unassisted walking. If the aim is to provide the best walking aid, for the best walking speed and the longest walk, single point cane is suggested as the best assistive device. Indeed, increasing the walking speed was associated with quality of life.24,25
It has been shown in the literature that falls are caused by reduced walking speed, decreased step length, increase step time.26 In our study, the differences in step length have been found. The walker was seen having the highest increase in step duration as the walking aid. In our study, considering the step duration is a variable parameter depending on the speed, the changes in walking speed of all walking aids explain the difference.
In our study, significant differences have been found between groups in terms of using different walking aids in the single support period, and in pairwise comparisons, and it has also been observed that this difference is between self control group and walking with a walker. The walker usage in the adult neuromuscular diseases has increased the single support period. This result shows the parallel result with the walker to be the most reducing walking aid for the walking speed. As a result, while the speed was reducing, the single support period was increasing, and the double support period was decreasing. Based on this result; we can consider the cases having trunk influences, the walker could be considered as a viable option in cases where trunk impairment is high, and to increase the transfer of weight to the extremity in case there is an atrophy of not using due to inactivity, and in case there is the need for limitation of the walking speed in cardiomyopathy patients.
Kinematic analysis of the pelvis
When the effects of walking aids on the pelvis kinematics, the most important key point for the lower trunk, were evaluated in our study, it has been found out that; significant statistical difference exists between the groups only in the pelvis extension; and these differences has arisen from the use of a single point cane and bilateral forearm crutch. Literature has shown that using a cane has not affected the angular kinematics of the pelvis and the functional performance of the chronic stroke patients. Researchers have stated that the dorsi flexion in swing phase and the pelvic tilt in stance phase are the most important components of the gait impairment.27 In our study, the angular changes occurred in the pelvis with the walking aids; pelvis flexion in all walking aids has been increased. The maximum increase has appeared with the bilateral forearm crutch at approximately 40%. These results have given us the following idea; when there is a preference between single point cane and bilateral forearm crutch in the clinic, the bilateral forearm crutch forms an influence as reducing effect of the extension of the pelvis angular movement, and the influence might make it difficult for patients to walk, which is performed by the patient with compensatory mechanisms in adult neuromuscular patients.
In addition to taking into consideration the 25% loss, which was observed in the patient trunk control test, it was observed that the trunk control of patients was influenced. This influence leads to inadequate power transfer to the lower extremities of the trunk and responding by reducing the pelvis movement to this changing situation. The mobility of pelvis in normal walking is an advantage, but it is desirable together with a good trunk control. The situation is different in the walker. It was observed that reasons such as 4-point support provided by walkers, increased propriocepive and sensory feedback due to both hands and arms resulting in the reduction of postural sway and the patient’s reliance on the walker, an increase lateral flexion of the pelvis in patients.28,29 It was thought that, achieved lower trunk control improved with stabilization training, patients can be progressed to a single point cane from walker in the rehabilitation practice. However, when the patient’s trunk control and lower extremity strength were inadequate, the walker achieved the result that sensory feedback from the upper extremity could be favored for reducing postural sway. The therapists can consider walkers as a suitable option for trunk control and lower extremity weakness.
In the literature it has been shown that; the use of cane in 25 patients with peripheral vestibular balance disorders has been shown to reduce the lateral flexion of pelvis and the rotation of the pelvis ahead in 4-5 degrees contributed to the acceleration of the thigh.28,30 In our study, when compared to the percentage of the total angular change in the pelvis lateral flexion, it appeared that; the lateral pelvic tilt has decreased 29% with a single point cane and has decreased 33% with a walker and has increased with a bilateral forearm crutch, and it appeared as increase in 8.62% when compared with normal walking. When the effect of changes in the pelvis rotation range by walking aids were evaluated, it was found that; it decreased 14% with a single point cane, and decreased 8.5 % with a walker, and increased approximately 13% with a bilateral forearm crutch. These results have shown us that the single point canes and walkers have made impact on lateral flexion and medio-lateral movement of the pelvis, but suggested that the bilateral forearm crutch has contributed to the reciprocal walking by increasing the rotation. If the aim is having reciprocal and symmetrical gait, it may be a suitable alternative to use a bilateral forearm crutch, but it should not be forgotten that a good upper limb strength is required for use of the bilateral forearm crutch.
In the rehabilitation during the selection of walking aids; patient-centered approach, people’s expectations and personal factors should be taken into account. In a study, the abondanment rate of walking aids was reported to be 29%, as patients did not feel safe and independent of themselves. Also, patients may refuse the use of walking aids by aesthetic concerns.30 When our patients’ walking aids preferences were evaluated, it was observed that the single point cane was selected as the most useful (61%), most comfortable (44.4%) and most preferred (61%) walking aid by the patients. But, 17% replied as “nothing” and the safest walking aid was chosen walker by the patients (55%). Even if the most suitable walking aid is selected for a patient; the patient may refuse to use it, if the patient has a feeling that it is unsafe and not proper for him/her or not noticing the functional decline.
The most important limitation of our study was that the level of fatigue is determined based on the expression of the patients. Another limitation of our study, despite performing kinematic analysis of the pelvis during gait, was the lack of assessment of the effect of the walking aids on postural sway and stability limit. The assessment of the impact on postural sway and stability limit of using walking aids for the future studies will make the results more powerful.
In conclusion, in clinical decision-making process of the present rehabilitation applications in which bio-psychosocial treatment models are emphasized our study proposes that the provision of a walking aid to the patient must be performed after the realization of the following, not merely with the personal experience of health professionals; the performance of overall muscle strength profile of the patients, motor performances, balance, functional status, trunk control, falling story, mobility level assessments, and by taking the patient’s biomechanical, physiological and psychosocial needs, expectations, satisfaction and the level of independence providing to the patient into account.
Acknowledgment
The authors would like to thank Yerel Tercüme translation office for English language editing
Footnotes
Copyright
Whenever a manuscript contains material (tables, figures, etc.) which is protected by copyright (previously published), it is the obligation of the author to obtain written permission from the holder of the copyright (usually the publisher) to reproduce the material in Saudi Medical Journal. This also applies if the material is the authors own work. Please submit copies of the material from the source in which it was first published.
References
- 1.D'Angelo MG, Berti M, Piccinini L, Romei M, Guglieri M, Bonato S, et al. Gait pattern in Duchenne muscular dystrophy. Gait Posture. 2009;29:36–41. doi: 10.1016/j.gaitpost.2008.06.002. [DOI] [PubMed] [Google Scholar]
- 2.Armand S, Mercier M, Watelain E, Patte K, Pelissier J, Rivier F. A comparison of gait in spinal muscular atrophy, type II and Duchenne muscular dystrophy. Gait Posture. 2005;21:369–378. doi: 10.1016/j.gaitpost.2004.04.006. [DOI] [PubMed] [Google Scholar]
- 3.Bateni H, Maki BE. Assistive devices for balance and mobility:benefits, demands, and adverse consequences. Arch Phys Med Rehabil. 2005;86:134–145. doi: 10.1016/j.apmr.2004.04.023. [DOI] [PubMed] [Google Scholar]
- 4.Zecevic AA, Salmoni AW, Speechley M, Vandervoort AA. Defining a fall and reasons for falling:comparisons among the views of seniors, health care providers, and the research literature. Gerontologist. 2006;46:367–376. doi: 10.1093/geront/46.3.367. [DOI] [PubMed] [Google Scholar]
- 5.samuelsson K, Wressle E. User satisfaction with mobility assistive devices:an important element in the rehabilitation process. Disabil Rehabil. 2008;30:551–558. doi: 10.1080/09638280701355777. [DOI] [PubMed] [Google Scholar]
- 6.Grundstrom AC, Guse CE, Layde PM. Risk factors for falls and fall-related injuries in adults 85 years of age and older. Arch Gerontol Geriatr. 2012;54:421–428. doi: 10.1016/j.archger.2011.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bertrand K, Raymond MH, Miller WC, Martin Ginis KA, Demers L. Walking Aids for Enabling Activity and Participation:A Systematic Review. Am J Phys Med Rehabil. 2017;96:894–903. doi: 10.1097/PHM.0000000000000836. [DOI] [PubMed] [Google Scholar]
- 8.McCrory MA, Kim HR, Wright NC, Lovelady CA, Aitkens S, Kilmer DD. Energy expenditure, physical activity, and body composition of ambulatory adults with hereditary neuromuscular disease. Am J Clin Nutr. 1998;67:1162–1169. doi: 10.1093/ajcn/67.6.1162. [DOI] [PubMed] [Google Scholar]
- 9.Cuthbert SC, Goodheart GJ., Jr On the reliability and validity of manual muscle testing:a literature review. Chiropr Osteopat. 2007;15:4. doi: 10.1186/1746-1340-15-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Collen FM, Wade DT, Robb GF, Bradshaw CM. The Rivermead Mobility Index:a further development of the Rivermead Motor Assessment. Int Disabil Stud. 1991;13:50–54. doi: 10.3109/03790799109166684. [DOI] [PubMed] [Google Scholar]
- 11.Bérard C, Payan C, Hodgkinson I, Fermanian J. A motor function measure for neuromuscular diseases Construction and validation study. Neuromuscul Disord. 2005;15:463–470. doi: 10.1016/j.nmd.2005.03.004. [DOI] [PubMed] [Google Scholar]
- 12.Collin C, Wade D. Assessing Motor Impairment after Stroke:A Pilot Reliability Study. J Neurol Neurosurg Psychiatry. 1990;53:576–579. doi: 10.1136/jnnp.53.7.576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Parlak Demir Y, Yıldırım SA. Reliability and validity of Trunk Control Test in patients with neuromuscular diseases. Physiother Theory Pract. 2015;31:39–44. doi: 10.3109/09593985.2014.945673. [DOI] [PubMed] [Google Scholar]
- 14.Jain M, Logaraj R, Waite M, Shieh CY, Dastgir J, Donkervoort S, Leach M, Bonnemann C. Validity of 2 Min Walk Test as an Outcome Measure in Individuals with Cmd and Other Neuromuscular Diseases. Neuromuscul Disord. 2013;23:738–852. [Google Scholar]
- 15.Li Q, Young M, Naing V, Donelan J. Walking speed estimation using shank-mounted inertial measurement units. J Biomech. 2010;43:1640–1643. doi: 10.1016/j.jbiomech.2010.01.031. [DOI] [PubMed] [Google Scholar]
- 16.Kotiadis D, Hermens HJ, Veltink PH. Inertial Gait Phase Detection for control of a drop foot stimulator Inertial sensing for gait phase detection. Med Eng Phys. 2010;32:287–297. doi: 10.1016/j.medengphy.2009.10.014. [DOI] [PubMed] [Google Scholar]
- 17.Wren TA, Gorton GE, 3rd, Ounpuu S, Tucker CA. Efficacy of clinical gait analysis:A systematic review. Gait Posture. 2011;34:149–153. doi: 10.1016/j.gaitpost.2011.03.027. [DOI] [PubMed] [Google Scholar]
- 18.Borg GA. Psychophysical bases of perceived exertion. Med Sci Sports Exerc. 1982;14:377–381. [PubMed] [Google Scholar]
- 19.Hayran M, Hayran M, editors. Basic statistics for health research. Ankara (TR): 2011. pp. 30–35. [Google Scholar]
- 20.Green SB, Salkind NJ, editors. Using SPSS for Windows and Macintosh, Books a la Carte. 8th Edition. TX (USA): Pearson; 2016. [Google Scholar]
- 21.Bohannon RW, Glenney SS. Minimal clinically important difference for change in comfortable gait speed of adults with pathology:a systematic review. J Eval Clin Pract. 2014;20:295–300. doi: 10.1111/jep.12158. [DOI] [PubMed] [Google Scholar]
- 22.Tyson SF. Trunk kinematics in hemiplegic gait and the effect of walking aids. Clin Rehabil. 1999;13:295–300. doi: 10.1191/026921599666307333. [DOI] [PubMed] [Google Scholar]
- 23.Polese JC, Teixeira-Salmela LF, Nascimento LR, Faria CD, Kirkwood RN, Laurentino GC, et al. The effects of walking sticks on gait kinematics and kinetics with chronic stroke survivors. Clin Biomech (Bristol, Avon) 2012;27:131–137. doi: 10.1016/j.clinbiomech.2011.08.003. [DOI] [PubMed] [Google Scholar]
- 24.Wiles CM, Busse ME, Sampson CM, Rogers MT, Fenton-May J, van Deursen R. Falls and stumbles in myotonic dystrophy. J Neurol Neurosurg Psychiatry. 2006;77:393–396. doi: 10.1136/jnnp.2005.066258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Constantinescu R, Leonard C, Deeley C, Kurlan R. Assistive devices for gait in Parkinson's disease. Parkinsonism Relat Disord. 2007;13:133–138. doi: 10.1016/j.parkreldis.2006.05.034. [DOI] [PubMed] [Google Scholar]
- 26.Kuan TS, Tsou JY, Su FC. Hemiplegic gait of stroke patients:the effect of using a cane. Arch Phys Med Rehabil. 1999;80:777–784. doi: 10.1016/s0003-9993(99)90227-7. [DOI] [PubMed] [Google Scholar]
- 27.Baetens T, De Kegel A, Palmans T, Oostra K, Vanderstraeten G, Cambier D. Gait analysis with cognitive-motor dual tasks to distinguish fallers from nonfallers among rehabilitating stroke patients. Arch Phys Med Rehabil. 2013;94:680–686. doi: 10.1016/j.apmr.2012.11.023. [DOI] [PubMed] [Google Scholar]
- 28.Whittle MW, editor. Gait analysis: An introduction. 4th edition. OH (USA): Butterworth-Heinemann; 2014. pp. 124–130. [Google Scholar]
- 29.Wressle E, Oberg B, Henriksson C. The rehabilitation process for the geriatric stroke patient--an exploratory study of goal setting and interventions. Disabil Rehabil. 1999;21:80–87. doi: 10.1080/096382899298016. [DOI] [PubMed] [Google Scholar]
- 30.Leach E, Cornwell P, Fleming J, Haines T. Patient centered goal-setting in a subacute rehabilitation setting. Disabil Rehabil. 2010;32:159–172. doi: 10.3109/09638280903036605. [DOI] [PubMed] [Google Scholar]